Abstract
Background
Anal intercourse (AI) is not uncommon among U.S. women and, when condomless, confers a far greater likelihood of HIV transmission than condomless vaginal intercourse. We aim to identify determinants preceding AI, among women with, and women without HIV.
Methods
3708 women living with (73%), and without HIV (27%) participating in the Women’s Interagency HIV Study provided sexual behavior and other data at 6-monthly visits over a median of 9 years (1994–2014). We used generalized estimating equation models to examine sociodemographic, structural and behavioral determinants reported in the visit preceding (1) AI, and (2) condomless AI.
Results
AI was reported at least once over follow-up by 31% of women without, and 21% with HIV. AI was commonly condomless; reported at 76% and 51% of visits among women living without HIV, and with HIV, respectively. Women reporting AI were more likely to be younger (continuous variable, adjusted odds ratio (aOR) = 0.97, 95% confidence interval (CI):0.96–0.98), Hispanic (aOR = 1.88, CI:1.47–2.41) or White (aOR = 1.62, CI:1.15–2.30) compared to Black, and have at least high school education (aOR = 1.33, CI:1.08–1.65). AI was more likely following the reporting of either (aOR = 1.35, CI:1.10–1.62), or both (aOR = 1.77, CI:1.13–2.82) physical and sexual violence, excessive drinking (aOR = 1.27, CI:1.05–1.66) or any drug use (aOR = 1.34, CI:1.09–1.66), multiple male partners (aOR = 2.64, CI:2.23–3.11), exchange sex (aOR = 3.45, CI:2.53–4.71), one or more female sex partners (aOR = 1.32, CI:1.01–1.75), condomless vaginal intercourse (aOR = 1.80, CI:1.53–2.09), and high depressive symptoms (aOR = 1.23, CI:1.08–1.39).
Conclusion
AI disproportionally follows periods of violence victimization, substance use, multiple sex partners and depression. Better prevention messaging and biomedical interventions that reduce acquisition or transmission risk are needed, but when AI occurs in the context of violence against women, as our findings indicate, focusing on gender-based violence reduction and immediate treatment to reduce HIV transmission risk is important.
Similar content being viewed by others
Background
Anal intercourse (AI) is practiced by women in the U.S. with an estimated 25% of sexually active young women and girls (aged < 25 years) in North America reporting having ever practiced AI [1], and 30% of sexually active women living in 20 US cities with high HIV prevalence reported AI within the past year [2]. The likelihood of HIV transmission during condomless receptive AI may be up to 18-fold higher than during condomless receptive vaginal intercourse (VI) [3]. Given this elevated transmission risk, AI among women may substantially shape the HIV epidemic in the U.S. A mathematical modeling study suggested that four in ten new HIV infections among urban U.S. women may be attributed to condomless AI [4].
Numerous cross-sectional studies have identified correlates of AI among women in the U.S., finding that women who report AI are more likely to report multiple sexual partners [2, 5, 6], transactional sex [2, 5, 7,8,9,10], lower condom use [11,12,13] and sex with both men and women [2, 14]. Substance use has also frequently been found to be positively associated with AI, with AI being more common among U.S. women who report using any type of illegal drug [6, 7, 9, 11, 15, 16], or binge drinking [2, 10, 17]. Although some women do report finding AI pleasurable [18], it does seem that it may often occur under coercion or in the context of violent relationships, with women reporting AI more likely to also report rape or coerced sex [19, 20], and to have experienced intimate partner physical violence [15, 21].
While we have a fair understanding from prior studies of current behaviors and exposures associated with AI among women, cross-sectional studies are limited by the lack of clear temporality between exposures, such as violence victimization, and AI. Prospective analysis should be conducted to better understand determinants of AI and condomless AI over time among women living with or at risk for HIV infection. Using 23 years of data from the Women’s Interagency HIV Study (WIHS) cohort, we aimed to identify time-varying determinants of AI and condomless AI over follow-up, among both women living with and without HIV.
Methods
The WIHS Cohort
The WIHS was the largest, and longest prospective cohort study of HIV infection among U.S. cisgender women, comprising 3677 women living with HIV (WLHIV) and 1305 demographically similar women without HIV. Initial recruitment occurred in 1994, with further recruitment waves in 2001–02 and 2011–12 at six urban sites (Bronx, NY; Washington, DC; San Francisco, CA; Los Angeles, CA; Chicago, IL; and Brooklyn, NY). In 2013, a fourth wave expanded recruitment to sites in the Southern U.S. (Chapel Hill, NC; Atlanta, GA; Miami, FL; Birmingham, AL; and Jackson, MS [22]. Briefly, WLHIV were recruited from HIV and other clinics and the community, as were demographically-similar women without HIV. Women without HIV were eligible for inclusion if they reported recent high-risk sexual or substance use behavior, or a diagnosis of a sexually transmitted infection (STI), although eligibility criteria varied slightly for each wave (Additional file 1: Table S1). Data were collected at approximately 6-month intervals, using structured face-to-face interviews or occasionally phone interviews when necessary. Local ethical approval for collection of data on violence victimization was granted at most sites from the first round, but was first granted to the San Francisco site in 2006, and was never granted for the Los Angeles site. All other data relevant to this analysis were collected at all sites, although data on violence and depression were not collected at all visits.
All cohort participants provided written informed consent. Ethical approval for data collection was granted by review boards at each study site.
Data analysis
We first described the proportion of visits at which AI and condomless AI were reported over follow-up. We then used bivariate and multivariable logistic regression models to examine sociodemographic, structural and behavioral determinants of our two outcomes of interest: (1) AI and (2) condomless AI. As observations were not independent, we used generalized estimating equations (GEE) to cluster standard errors at the participant level (with an exchangeable correlation structure) [23]. Visits with and without reported (1) AI and (2) condomless AI were compared using determinants measured during the prior visit. Condomless AI was defined as reporting that condoms were used ‘sometimes’ or ‘never’ during AI since the last visit, versus ‘always’.
The recall period for the outcomes of interest and the time-varying covariates was ‘since the last visit’, which was approximately six months prior if no study visits had been skipped. Our analysis was restricted to visits where the recall period of the outcome was up to approximately one year (i.e., a maximum of one skipped prior visit).
Guided by a literature-based conceptual framework, covariates of interest available in the WIHS dataset were identified and selected a priori (Additional file 1: Figure S1) [24]. Multicollinearity between covariates was assessed using the variance inflation factor [25]. Collinear variables were combined where reasonable, otherwise one was selected based on quasi information criteria (QIC) values measuring model fit [26]. If QIC varied little, the variable with fewest missing values was retained. Thus, the highly collinear variables for number of male partners and exchange sex (defined as practicing sex in exchange for money or drugs) were combined into one variable, as were sexual and physical violence victimization. Household income was chosen over the collinear housing and employment status variables based on QIC values, while crack, cocaine or heroin use was chosen over injection drug use based on number of missing values.
Time-varying covariates of interest were: HIV status (n = 23 women sero-converted during follow-up), age (continuous), marital status (married or living with a partner / not), annual household income (< $12,000/$12,000 +), physical (experienced serious physical violence) and sexual (pressured or forced to have sex) violence victimization (none/either physical or sexual/both physical and sexual), alcohol use (dichotomized at seven drinks per week, the limit above which alcohol use among women is considered to be problematic drinking per National Institute on Alcohol Abuse and Alcoholism [27]), any crack, cocaine or heroin use, the number of male partners and exchange sex (one partner and no exchange sex/multiple partners and no exchange sex/exchange sex), any female sexual partners, condomless VI (‘never’ or ‘sometimes’ using condoms during VI), and high depressive symptoms (defined as scoring 16 + on the Center for Epidemiologic Studies Depression Scale [28]).Models were additionally controlled for non-time-varying covariates measured at baseline: educational level (< high school/ high school +) and race and ethnicity (Non-Hispanic Black/Hispanic or Latina/White/Other). The small number of women who seroconverted during follow-up (n = 23) were considered as not living with HIV until documentation of seroconversion; for visits after this point their status was changed. The same covariates apart from condomless VI were used to examine determinants of condomless AI. WIHS participants with at least two follow-up visits, and for whom data on AI and each time-varying covariate were available at least once, were included in our analysis.
Ten of the 13 included covariates had missing data (all missing at < 8% of visits except for the violence covariates, missing at 39% of visits, and depressive symptoms, missing at 12%). In this context, a complete case analysis would have dropped 52% of all study visits; we therefore dealt with missing covariate values using multiple imputation. Outcome variables were not imputed. We used a joint modelling approach which uses a multivariate normal model fitted by Markov Chain Monte Carlo [29]. Along with the covariates of interest, the imputation model additionally controlled for recruitment wave and baseline study site, as missingness differed by these variables. Twenty imputed datasets were produced and combined using Rubin’s rule [30]. As a sensitivity analysis, we also performed the analysis on the subset of complete cases.
All analyses were conducted using the R statistical software [31], with “mitml” and “jomo” packages [32, 33] used for multiple imputation and the “geepack” package [34] used for GEE regression models.
Results
Study participants and visits
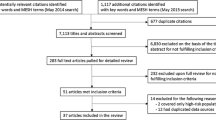
Of the 4982 total women recruited, 3708 women (74%) met the inclusion criteria for this analysis (Additional file 1: Figure S2). Baseline characteristics are presented in Table 1. Participants were followed for a median of 9 years (inter quartile range (IQR) = 3.0–16.5). Over a quarter (27%) of women (n = 1004) were not living with HIV at baseline; the remaining 73% of women were living with HIV at enrollment. Median baseline age was 37 years (IQR = 31–44). Over two-thirds of women described themselves as non-Hispanic Black (69%) and over a sixth as Hispanic or Latina (16%). The remainder identified as non-Hispanic White (12%) and other ethnicities and races (3%). Median income was low, with 56% having an annual household income of less than $12,000/year, and less than a third were employed (29%). Experience of violence victimization was common, with 55% reporting ever having been victims of physical, and 40% of sexual violence. The median number of lifetime male sex partners was 10 (IQR = 5–40). 43% of women reporting ever having had AI, 36% reported ever having practiced exchange sex. Most baseline characteristics did not vary by HIV status.
AI over follow-up
AI was reported at least once over follow-up by nearly a quarter of women (24%) and was more commonly reported by women without HIV (31%) than by WLHIV (21%). Reporting condomless AI at least once was twice as common among women without HIV (28%) as among WLHIV (14%).
Across the whole sample, AI was reported at 5% of all visits. A male sexual partner was reported at two-thirds of visits (64%) with AI reported at 8% of those visits. At visits when a male sex partner was reported, women without HIV reported AI at 10% of visits and condomless AI at 8% of visits, compared to 7% and 4%, respectively, reported by WLHIV. AI was more often condomless among women without AI; reporting that three-quarters (76%) of AI acts were condomless while HIV-infected women reported that nearly half (51%) of AI acts were condomless. Table 2 details the proportions of visits at which time-varying covariates of interest were reported, as well as the proportions of visits at which AI was reported at the subsequent visit, among the whole sample (with proportions by HIV status reported in Additional file 1: Table S2).
Determinants of AI, and condomless AI over follow-up
Although the unadjusted odds of AI were substantially lower among WLHIV than among women without HIV (odds ratio (OR) = 0.67; 95% confidence interval (CI): 0.54–0.83), the association did not remain after multivariable adjustment (Table 3). Adjusted odds of condomless AI, however, were lower among WLHIV (adjusted odds ratio (aOR) = 0.61; 95% CI: 0.46–0.74). AI decreased substantially with age (aOR = 0.94; 95% CI: 0.94–0.95 per one-year increase in age). After multivariable adjustment, Hispanic and White women had over 1.5 times the odds of reporting AI than Black women (e.g., aOR = 1.62; 95% CI: 1.25–2.30 among White women), while condomless AI was more likely to be reported by Hispanic women (aOR = 1.65; 95% CI: 1.25–2.20), but not by White women, relative to Black women. After multivariable adjustment, AI was slightly more likely among women who had finished high school (aOR = 1.33; 95% CI:1.08–1.65).
Odds of AI as well as condomless AI increased with violence victimization. Odds of AI were higher when both physical and sexual violence were reported (aOR = 2.50; 95% CI: 1.44–4.12), compared to one form of violence (aOR = 1.62; 95% CI: 1.28–2.08). Relative to non-substance users, odds of AI and condomless AI were slightly higher following periods of problematic alcohol use (AI, aOR = 1.27; 95% CI:1.05–1.51) and use of crack, cocaine, or heroin (AI, aOR = 1.34; 95% CI:1.09–1.66). Compared to women reporting one male sex partner and no exchange sex, women reporting multiple partners and no exchange sex, as well as those reporting exchange sex, had approximately two-fold adjusted odds of both AI and condomless AI. Women reporting a recent female sex partner had a slightly elevated adjusted odds of subsequent AI (aOR = 1.32; 95% CI: 1.00–1.75) but not higher adjusted odds of condomless AI, while women reporting condomless VI had nearly two-fold the odds (aOR = 1.80; 95% CI:1.53–2.09) of subsequently reporting AI. Having high depressive symptoms slightly increased the odds of both subsequent AI (aOR = 1.23; 95% CI:1.08–1.39) and condomless AI (aOR = 1.25; 95% CI:1.03–1.48).
Results were similar when the analysis was restricted to complete cases (Additional file 1: Tables S3 and S5), although 95% CIs were narrower in models using multiple imputation. Models stratified by HIV status at baseline also found similar results (Additional file 1: Tables S4, S5).
Discussion
Using more than two decades of data from the WIHS cohort, we found that AI decreased with age and is more commonly practiced by White and Hispanic women (compared to Black women) and more educated women. We found AI to be associated with previous violence victimization, excessive drinking, drug use, likely depression, and more varied or risky sexual behaviours: multiple male partners, any female partners, transactional sex, and condomless VI. These findings concur with observations from numerous cross-sectional studies [24], but our longitudinal analysis supports the temporal order of these associations; strengthening the evidence by avoiding potential reverse causality issues.
The associations of AI which we identified here are similar to findings of other papers, including to our previous analysis which used group-based trajectory modelling to identify groups with distinct AI behaviors among WIHS participants living without HIV [35]. We found that the trajectory group reporting AI most consistently over the life course were, at baseline, more likely to identify as bisexual or lesbian, to report more male sex partners, and to report ever having experienced physical or sexual violence, compared to the group who rarely or never reported AI.
Determinants of AI and condomless AI were largely similar, although there were some interesting differences. Adjusted estimates of AI did not differ by HIV status, but condomless AI was much less commonly practiced among WLHIV. Further, while White women (compared to Black women) and women with at least a high school education were more likely to report AI, they were not more likely to practice condomless AI, implying that these women tend to use condoms more consistently. Women experiencing violence were more likely to report AI and condomless AI, but the magnitude of association with condomless AI was 1.5 times greater. This could imply that when AI occurs in the context of violence, it is more likely to be unprotected by condoms. This conjecture is supported by other studies which examined intimate partner violence directly, and found it to be associated with condomless AI [15, 19], while others have found that intimate partner violence is associated with using condoms inconsistently, regardless of sex act type [36]. Further research, ideally taking a qualitative approach, should be conducted to more thoroughly explore the relationships between violence, coercion, condom use and AI.
A main limitation of this analysis is the use of face-to-face interviews to collect data, and AI as well as condomless sex may be underreported due to social-desirability bias. Meta-analyses have found that the reporting of AI increases with confidentiality of interview method [1, 37, 38]. As reported elsewhere [6, 8], we found AI to be more common among women with higher educational attainment. We did not assess whether AI is less stigmatized among women with higher educational attainment who may therefore more accurately report AI. Second, the lack of data on violence perpetrators was a limitation, as we were unable to directly assess whether intimate partner violence predicted AI. Third, high proportions of values were missing for some indicators. The use of multiple imputation helped avoid some biases and allowed us to retain the large sample size, but also incorporated additional uncertainty in the results.
Policy implications
As AI has been found to be fairly common among US women, clinicians should routinely include question on AI practice when assessing patients’ HIV and STI risk. In addition, in order to anal STIs, women should be offered both rectal and vaginal tests, rather than solely vaginal tests, as is currently the norm in routine STI screening [39].The determinants of AI identified in this paper can be used to improve targeting of safe sex messaging and of prevention services such as both HIV pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP). However, when AI occurs in the context of violence, as these findings indicate it often might, women are unlikely to be able to insist on condom use, and may also be unable to safely access and take PrEP. As such, gender-based violence reduction interventions, may offer an additional path to reducing HIV transmission among women. These could range from individual-level approaches such as teaching teens healthy relationship skills, teaching parenting skills and engaging with families in early childhood, to structural interventions such as improving school climate and safety, and strengthening economic support for families [40].
Availability of data and materials
Access to individual-level data from the MACS/WIHS Combined Cohort Study Data (MWCCS) may be obtained upon review and approval of a MWCCS concept sheet. Links and instructions for online concept sheet submission can be found on the study website: https://statepi.jhsph.edu/mwccs/work-with-us/. Upon request, we will share the code used for this analysis with anyone with access to the relevant WIHS data.
References
Owen BN, Brock PM, Butler AR, Pickles M, Brisson M, Baggaley RF, et al. Prevalence and frequency of heterosexual anal intercourse among young people: a systematic review and meta-analysis. AIDS Behav. 2015;19:1338–60.
Hess KL, DiNenno E, Sionean C, Ivy W, Paz-Bailey G. Prevalence and correlates of heterosexual anal intercourse among men and women, 20 U.S. Cities. AIDS Behav. 2016;20(12):2966–75. https://doi.org/10.1007/s10461-016-1295-z.
Baggaley RF, Owen BN, Silhol R, Elmes J, Anton P, McGowan I, et al. Does per-act HIV-1 transmission risk through anal sex vary by gender? An updated systematic review and meta-analysis. Am J Reprod Immunol. 2018;80: e13039.
Elmes J, Silhol R, Hess KL, Gedge LM, Nordsletten A, Staunton R, et al. Receptive anal sex contributes substantially to heterosexually acquired HIV infections among at‐risk women in twenty US cities: results from a modelling analysis. Am J Reprod Immunol. 2020. https://doi.org/10.1111/aji.13263.
Gorbach PM, Manhart LE, Hess KL, Stoner BP, Martin DH, Holmes KK. Anal intercourse among young heterosexuals in three sexually transmitted disease clinics in the United States. Sex Transm Dis. 2009;36:193–8.
Benson LS, Martins SL, Whitaker AK. Correlates of heterosexual anal intercourse among women in the 2006–2010 National survey of family growth. J Sex Med. 2015;12:1746–52.
Champion JD, Roye CF. Toward an understanding of the context of anal sex behavior in ethnic minority adolescent women. Issues Ment Health Nurs. 2014;35:509–16.
Misegades L, Page-Shafer K, Halperin D, McFarland W. Anal intercourse among young low-income women in California: an overlooked risk factor for HIV? AIDS. 2001;15:534–5.
Javanbakht M, Guerry S, Gorbach PM, Stirland A, Chien M, Anton P, et al. Prevalence and correlates of heterosexual anal intercourse among clients attending public sexually transmitted disease clinics in Los Angeles County. Sex Transm Dis. 2010;37:369–76.
McLellan-Lemal E, O’Daniels CM, Marks G, Villar-Loubet O, Doherty IA, Simpson C, et al. Sexual risk behaviors among African-American and Hispanic women in five counties in the Southeastern United States: 2008–2009. Womens Health Issues. 2012;22:e9-18.
Gross M, Holte SE, Marmor M, Mwatha A, Koblin BA, Mayer KH. Anal sex among HIV-seronegative women at high risk of HIV exposure: the HIVNET vaccine preparedness study 2 protocol team. J Acquir Immune Defic Syndr. 2000;24(4):393–8. https://doi.org/10.1097/00042560-200008010-00015.
D’Anna LH, Warner L, Margolis AD, Korosteleva OA, O’Donnell L, Rietmeijer CA, Klausner JD, Kevin Malotte C. Consistency of condom use during receptive anal intercourse among women and men who have sex with men: findings from the safe in the city behavioral study. Sex Transm Dis. 2015;42(7):393–9. https://doi.org/10.1097/OLQ.0000000000000306.
Hebert LE, Lilleston PS, Jennings JM, Sherman SG. Individual, partner, and partnership level correlates of anal sex among youth in Baltimore City. Arch Sex Behav. 2015;44:619–29.
Roye CF, Krauss BJ, Silverman PL. Prevalence and correlates of heterosexual anal intercourse among Black and Latina female adolescents. J Assoc Nurses AIDS Care. 2010;21:291–301.
Koblin BA, Hoover DR, Xu G, Frye V, Latka MH, Lucy D, et al. Correlates of anal intercourse vary by partner type among substance-using women: baseline data from the UNITY study. AIDS Behav. 2010;14:132–40.
Reynolds GL, Fisher DG, Napper LE, Fremming BW, Jansen MA. Heterosexual anal sex reported by women receiving HIV prevention services in Los Angeles County. Women’s Health Issues. 2010;20:414–9.
Hutton HE, McCaul ME, Chander G, Jenckes MW, Nollen C, Sharp VL, et al. Alcohol use, anal sex, and other risky sexual behaviors among HIV-infected women and men. AIDS Behav. 2013;17:1694–704.
Reynolds GL, Fisher DG, Rogala B. Why women engage in anal intercourse: results from a qualitative study. Arch Sex Behav. 2015;44:983–95.
Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, Gorbach PM. Intimate partner violence and anal intercourse in young adult heterosexual relationships. Perspect Sex Reprod Health. 2013;45:6–12.
Fahs B, Swank E, Clevenger L. Troubling anal sex: gender, power, and sexual compliance in heterosexual experiences of anal intercourse. Gend Issues. 2015;32:19–38.
Hess KL, Reynolds GL, Fisher DG. Heterosexual anal intercourse among men in Long Beach. California J Sex Res. 2014;51:874–81.
Adimora AA, Ramirez C, Benning L, Greenblatt RM, Kempf M-C, Tien PC, et al. Cohort profile: the women’s interagency HIV study (WIHS). Int J Epidemiol. 2018;47:393–394i.
Hanley JA. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–75. https://doi.org/10.1093/aje/kwf215.
Owen BN. A neglected risk factor in HIV prevention and implications for prevention. Imperial College London; 2019.
Midi H, Sarkar SK, Rana S. Collinearity diagnostics of binary logistic regression model. J Interdisc Math. 2010;13:253–67.
Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001;57:120–5.
NIH: National Institute on Alcohol Abuse and Alcoholism. Drinking levels defined. www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed 7 Apr 2016.
Cook JA, Grey DD, Burke-Miller JK, Cohen MH, Vlahov D, Kapadia F, et al. Illicit drug use, depression and their association with highly active antiretroviral therapy in HIV-positive women. Drug Alcohol Depend. 2007;89:74–81.
Quartagno M, Carpenter JR. Multiple imputation for discrete data: evaluation of the joint latent normal model. Biom J. 2019;61:1003–19.
Rubin D. Multiple Imputation for Nonresponse in Surveys. Hoboken: John Wiley & Sons; 1987.
Team RC. R: A language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria. ISBN 3-900051-07-0, URL. 2018. http://www.R-project.org/.
Halekoh U, Højsgaard S, Yan J. The R package geepack for generalized estimating equations. J Stat Softw. 2006. https://doi.org/10.18637/jss.v015.i02.
Quartagno M, Carpenter J. JOMO: Multilevel Joint Modelling Multiple Imputation. 2019.
Hojsgaard S, Halekoh U, Yan J. The R package geepack for generalized estimating equations journal of statistical software. J Statis. 2006;15:1–11.
Owen BN, Baggaley RF, Maheu-Giroux M, Elmes J, Adimora AA, Ramirez C, et al. Patterns and trajectories of anal intercourse practice over the life course among us women at risk of HIV. J Sex Med. 2020;17:1629–42.
Coker AL. Does physical intimate partner violence affect sexual health? Trauma Violence Abuse. 2007;8:149–77.
Owen BN, Elmes J, Silhol R, Dang Q, McGowan I, Shacklett B, et al. How common and frequent is heterosexual anal intercourse among South Africans? A systematic review and meta-analysis. J Int AIDS Soc. 2017;19:1–14.
Owen BN, Baggaley RF, Elmes J, Harvey A, Shubber Z, Butler AR, et al. What proportion of female sex workers practise anal intercourse and how frequently? A systematic review and meta-analysis. AIDS Behav. 2019. https://doi.org/10.1007/s10461-019-02477-w.
Tao G, Hoover KW, Nye MB, Peters PJ, Gift TL, Body BA. Infrequent testing of women for rectal chlamydia and gonorrhea in the United States. Clin Infect Dis. 2018;66:570–5.
Niolon PH, Kearns M, Dills J, Rambo K, Irving S, Armstead T, et al. Preventing intimate partner violence across the lifespan: a technical package of programs, policies and practices. Atlanta; 2017.
Acknowledgements
Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS), now the MACS/WIHS Combined Cohort Study (MWCCS). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). MWCCS (Principal Investigators): Atlanta CRS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-HL146241; Bronx CRS (Kathryn Anastos and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01-HL146202; Data Analysis and Coordination Center (Gypsyamber D’Souza, Stephen Gange and Elizabeth Golub), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Northern California CRS (Bradley Aouizerat, Jennifer Price, and Phyllis Tien), U01-HL146242; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-HL146203; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom, and Deborah Konkle-Parker), U01-HL146192; UNC CRS (Adaora Adimora), U01-HL146194. The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute Of Child Health and Human Development (NICHD), National Institute On Aging (NIA), National Institute Of Dental and Craniofacial Research (NIDCR), National Institute Of Allergy And Infectious Diseases (NIAID), National Institute Of Neurological Disorders And Stroke (NINDS), National Institute Of Mental Health (NIMH), National Institute On Drug Abuse (NIDA), National Institute Of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute on Minority Health and Health Disparities (NIMHD), and in coordination and alignment with the research priorities of the National Institutes of Health, Office of AIDS Research (OAR). MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), P30-AI-050409 (Atlanta CFAR), P30-AI-073961 (Miami CFAR), P30-AI-050410 (UNC CFAR), P30-AI-027767 (UAB CFAR), and P30-MH-116867 (Miami CHARM). The authors gratefully acknowledge the contributions of the study participants and dedication of the staff at the MWCCS sites.
Funding
The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute of Mental Health (NIMH). Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Cranio-facial Research (NIDCR), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and Other Communication Disorders (NIDCD), and the NIH Office of Research on Women’s Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA), P30-AI-050409 (Atlanta CFAR), P30-AI-050410 (UNCCFAR), and P30-AI-027767 (UAB CFAR). Rebecca F. Baggaley is supported by a Wellcome Trust Institutional Strategic Support Fund Fellowship (204801/Z/16/Z). Mathieu Maheu-Giroux’s research program is funded by a career award from the Fonds de Recherche du Québec—Santé. Tonya N. Taylor’s work is supported by HRSA-19–008 (Cohen and Reinhardt, mPI 7/1/19–6/30/24and 1R21NR018348-01 (Wilson) 7/1/18–6/30/20. Dominika Seidman’s work is supported by grant 5K12HD001262-18 from the National Institutes of Health. We acknowledge joint-centre funding from the UK Medical Research Council and Department for International Development (Grant reference MR/R015600/1). This award is jointly funded by the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement and is also part of the EDCTP2 programme supported by the European Union. The funders played no role in the design of the study, the data collection, analysis or interpretation, or the writing.
Author information
Authors and Affiliations
Contributions
Conception and Design: BNO, MCB, RFB, MMG, JE, CR, AAA, AE. Acquisition of Data: AAA, KS, TTT, MP, DS, KMW, ETG, JW, HB, DKP, JC, AE. Analysis and Interpretation of Data: BNO and GP. Drafting the Article: BNO. Revising it for Intellectual Content: BNO, MCB, RFB, MMG, JE, CR, AAA, AE, GP, KS, TTT, MP, DS, KMW, ETG, JW, HB, DKP, JC. Final Approval of the Completed Article: BNO, MCB, RFB, MMG, JE, CR, AAA, AE, GP, KS, TTT, MP, DS, KMW, ETG, JW, HB, DKP, JC. All the authors read and approved final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent to participate was obtained from all participants. Review boards at each of individual study sites granted ethical approval for the data collection. After submission of a concept note which included an analysis plan, and once ethical approval for this analysis was granted, the WIHS Executive Committee granted access to anonymized individual level data. Ethical approval for this secondary analysis was granted by review boards at the National Institute of Health and Imperial College London.
Consent for publication
Not Applicable.
Competing interests
The authors declare no financial or non-financial competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Eligibility criteria of women without HIV recruited to the WIHS cohort. Table S2. Percentage of visits at which time-varying covariates reported, and percentage of visits at which anal intercourse and condomless anal intercourse reported at subsequent visit. Table S3. Predictors of anal intercourse and condomless anal intercourse using a complete case analysis. Table S4. Predictors of any anal intercourse over follow-up, by HIV status, using a complete case analysis. Figure S1. A conceptual framework of anal intercourse among women in the U.S. Figure S2. Selection process of analysis sample.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Owen, B.N., Baggaley, R.F., Maheu-Giroux, M. et al. Longitudinal determinants of anal intercourse among women with, and without HIV in the United States. BMC Women's Health 22, 291 (2022). https://doi.org/10.1186/s12905-022-01849-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01849-0