Abstract
Objectives
Little direction exists on how to effectively implement palliative care for patients with COPD. In the COMPASSION study, we developed, executed, and evaluated a multifaceted implementation strategy to improve the uptake of region-tailored palliative care intervention components into routine COPD care. We evaluated the implementation strategy and assessed the implementation process, barriers, and facilitators.
Methods
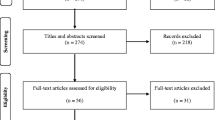
A mixed methods process evaluation was performed. Primary and secondary healthcare providers in four hospital regions in the Netherlands were trained. Patients identified during hospitalisation for an acute exacerbation received palliative care and were followed for a year. Various sources were used: process data, questionnaires including the End-of-life Professional Caregiver Survey (EPCS), medical records, monitoring meetings, and interviews. The Consolidated Framework of Implementation Research (CFIR) was used to categorize implementation determinants.
Results
The training sessions with roleplay were positively evaluated and increased professionals’ self-efficacy in providing palliative care statistically significantly. Of 98 patients identified, 44 (44.9%) received one or more palliative care conversations at the outpatient clinic. Having those conversations was highly valued by healthcare providers because it led to clarity and peace of mind for the patient and higher job satisfaction. Coordination and continuity remained suboptimal. Most important barriers to implementation were time constraints, the COVID-19 pandemic, and barriers related to transmural and interdisciplinary collaboration. Facilitators were the systematic screening of patients for palliative care needs, adapting to the patient’s readiness, conducting palliative care conversations with a pulmonologist and a COPD nurse together, and meeting regularly with a small team led by a dedicated implementation leader.
Conclusions
Providing integrated palliative care for patients with COPD is highly valued by healthcare providers but remains challenging. Our findings will guide future implementation efforts. Future research should focus on how to optimize transmural and interdisciplinary collaboration.
Trial registration
The COMPASSION study is registered in the Netherlands Trial Register (NTR): NL7644. Registration date: 07/04/2019.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Patients with advanced Chronic Obstructive Pulmonary Disease (COPD) suffer from a high symptom burden and low quality of life, emphasizing the need for palliative care [1]. Palliative care is an approach that aims to optimize the quality of life of patients with a life-limiting illness through assessment and treatment of physical, psychological, social and spiritual problems [2]. It includes advance care planning, allowing care to be tailored to the patient’s goals and preferences [3]. Despite guideline recommendations, [4, 5] palliative care is only provided to a limited number of patients with COPD, and often, advance care planning is discussed in an acute care setting (e.g., when a patient visits the emergency department for an acute exacerbation) rather than proactively (e.g., during an outpatient visit to their regular doctor) [6, 7]. Also, the involvement of specialist palliative care is limited and restricted to the terminal phase [8]. As a result, many symptoms, such as dyspnoea, fatigue, and depression, remain undertreated, [9] and care preferences are not timely discussed [7].
Although the need for palliative care has been widely acknowledged, little direction exists on successfully implementing it into routine COPD care [10]. The key barriers to timely initiating palliative care in COPD are the prognostic uncertainty due to the unpredictable illness trajectory and the lack of training of healthcare providers (HCPs) to discuss end-of-life topics [11, 12]. These barriers may be addressed by using transition points, such as hospitalisation, to screen for palliative care needs [13] and communication training to increase HCPs’ self-efficacy in discussing palliative care topics [14]. However, the empirical evidence on effective implementation strategies is still limited [10].
Therefore, as part of the COMPASSION study, a multifaceted implementation strategy was developed, executed and evaluated [15]. HCPs across four hospital regions were trained to implement palliative care components into routine COPD care. Also, they were provided with access to an online toolbox, including a screening tool to identify palliative patients during hospitalisation, and implementation guidance. The aim of this study was 1) to evaluate the implementation strategy and its effect on reach and dose delivered of palliative care components and 2) to identify barriers and facilitators to successful implementation of integrated palliative care in COPD.
Methods
Design and setting
A comprehensive, mixed-method process evaluation was performed in four intervention hospital regions of the COMPASSION study. Each region was asked to form an intervention team consisting of primary and secondary care providers working in respiratory and palliative care (Table 1). We followed the Standards for Reporting Implementation Studies (StaRi) for reporting [16].
Intervention and implementation strategy
The intervention and multifaceted implementation strategy were developed in collaboration with many stakeholders and have previously been described in detail in the COMPASSION study protocol [15]. The intervention was based on national guidelines [2, 5] and consisted of the following core components (Fig. 1A): 1) identification of palliative patients with COPD during hospitalisation, 2) one or more palliative care conversations consisting of advance care planning, multidimensional assessment, and symptom management, 3) coordination and continuity of care, and 4) if a patient died, aftercare comprising bereavement care and care evaluation with involved HCPs. According to the national guideline, palliative care was performed primarily by respiratory HCPs, whereas specialist palliative care team consultants could be involved in case of complex needs [2]. Regions were allowed to tailor the intervention to regional and individual patients’ needs and preferences. The ProPal-COPD tool was used to facilitate providers to identify palliative patients admitted to the hospital for an exacerbation of COPD [17]. It consists of the surprise question (“Would you be surprised if your patient were to die in the next 12 months?”) and six COPD-specific clinical indicators, which together produce a total score. Initially, the cut-off value as previously published was used [17]. After six months, in monitoring meetings it became clear that the rate of positive scores was lower than expected by HCPs and researchers. Therefore, the research group deemed it necessary to lower the cut-off value.
To facilitate uptake of the intervention components, a multifaceted implementation strategy was developed (Fig. 1B). Between April and September 2019, HCPs from the intervention team received two 3-hour training sessions on 1) content of palliative care in COPD, including communication training with roleplay and non-pharmacological dyspnoea management, and 2) implementation of palliative care. At the end of the second training session, HCPs were asked to complete a regional action plan detailing how, when and by whom different intervention components had to be performed. They received access to an online toolbox (www.palliatievezorgcopd.nl), comprising information on the content and practice of the intervention components, the ProPal-COPD tool, and other tools for facultative use. Furthermore, implementation leaders were guided for two years through four monitoring meetings per region and two project meetings, where regions exchanged experiences and best practices.
Data collection
The multifaceted implementation strategy was evaluated using process data (attendance rate of the training and use of regional action plans) and evaluation questionnaires administered at the end of each training session (appreciation of the training) and three and fifteen months later (use and appreciation of the toolbox). Also, HCPs’ level of self-efficacy in providing palliative care was assessed using the End-of-life Professional Caregiver Survey (EPCS) before and 3 and 15 months after the training [18]. This scale is a validated questionnaire comprising 28 items on three domains: patient- and family-centred communication, cultural and ethical values, and effective care delivery. The total score ranges from 0 to 112, with higher scores reflecting better knowledge and comfort in providing end-of-life communication.
To determine reach and dose delivered, we assessed the medical records of patients participating in the COMPASSION study one year after inclusion. Reach was defined as the number of patients participating in the intervention. Dose was defined as the extent to which each component was delivered [19]. Information on the number, timing, and content of palliative care conversations, treatments started, referrals made, and life-sustaining treatment preferences documented were extracted. For each included patient, HCPs were asked to indicate the duration of palliative care conversations, who was present, and the reason if no conversation had taken place.
Barriers and facilitators to implementation were identified using transcripts of monitoring meetings with implementation leaders (held by EV and JB) and semi-structured interviews with implementation leaders and trained HCPs less actively involved in implementation (held by JB). Between fifteen to twenty months after the training, per region, six HCPs (n = 24), were interviewed about care practices and work agreements, experiences with the implementation process, barriers and facilitators encountered, and experiences with the intervention. Interview duration varied between 20 and 85 minutes (mean 49 minutes). Monitoring meetings and interviews were audio-recorded and transcribed verbatim. All participants gave written informed consent, except for one GP due to time constraints, and this transcript was therefore excluded from analysis.
Data analyses
Quantitative data were analysed using descriptive statistics with IMB SPSS (Statistical Package for Social Science) version 25. EPCS total scores were calculated, and pre-post scores of HCPs with complete EPCS data were compared using Wilcoxon signed rank tests. Qualitative data were analysed using thematic analysis with a phenomenological approach [20]. Transcripts were first inductively coded via open and axial coding (JB). Initial codes and summaries were discussed with the research group multiple times, and codes were merged, split, and renamed until consensus was reached. Subsequently, the Consolidated Framework of Implementation Research (CFIR) was used to further categorize possible barriers and facilitators to implementation [21]. The CFIR contains 39 constructs across five domains: intervention characteristics, outer setting, inner setting, characteristics of the individuals involved, and the process of implementation. Each code was mapped to one of the constructs by JB and checked by RK, who has extensive expertise in implementation research. Differences between and within regions were compared. Finally, the interpretation of findings was discussed with the research group.
Results
Evaluation of implementation strategy
The first and second training session attendance rates were 38/46 (82.6%) and 36/46 (78.3%), respectively. HCPs evaluated the first training session high with a mean score of 8.4 out of 10 and the second training session with 7.9. The highest rated training elements were interactive communication training and dyspnoea management. After three months, 18/29 responding providers (62.1%) reported to have visited the online toolbox at least once, and 20/28 responding providers (71.4%) after fifteen months. The online toolbox was evaluated with a score of 7.1 for design and 7.8 for content. A draft of a regional action plan was completed by two regions, but not actively used in practice.
A statistically significant increase in EPCS total scores was observed three and fifteen months after the training (Table 2).
Reach and dose of intervention components
Component 1. Identification
All 198 hospitalised patients eligible and consenting to participate in the COMPASSION study (100%) were screened with the ProPal-COPD tool (Table 3). Of these, 98 had a positive ProPal-score. HCPs also screened outpatients on their initiative, but as these patients did not participate in the COMPASSION study, they were not included in the numbers.
Component 2. Palliative care conversations
A palliative care conversation at the outpatient clinic within 1-year follow-up occurred in 44/98 patients with a positive ProPal-score (44.9%). The timing, duration, and content of the conversations are presented in Table 4. In some cases, a conversation was waived due to organisational factors: transferral to a different care setting (primary care, rehabilitation centre, or nursing home) (n = 9) or postponement of outpatient visits due to the COVID-19 pandemic (n = 6). In other cases, the patient had died (n = 9), was reluctant (n = 7), or was psychiatrically ill (n = 1).
Twenty-two of 98 patients (22.4%) received a specialist palliative care team consultation and were subsequently discussed in the multidisciplinary team meeting; the percentage varied between regions from 0 to 45% (Table 3).
Component 3. Coordination and continuity
In half (22/44) of patients receiving an outpatient palliative care conversation, a letter was sent to the GP to report the conversation, in which nine agreements about future care coordination were included. None of the regions noted creating an individual care plan.
Component 4. Aftercare
Of all 98 patients, 21 patients died within one year of follow-up. An aftercare conversation was occasionally offered to bereaved families but never occurred in practice, and an evaluation of HCPs involved took place once.
Barriers and facilitators to successful implementation
Characteristics of interview participants are described in Table 5. For each domain of the CFIR, the facilitators and barriers identified are summarised in Table 6. In the outer setting domain, no determinants were identified.
Intervention characteristics
Relative advantage
All HCPs highly appreciated the palliative care intervention because its implementation resulted in more clarity and peace of mind for patients, improved the relationship with patients, and provided HCPs with a sense of contributing in a meaningful way.
“It also gives a lot of satisfaction in your work, that you can help people in that way too, those patients. So I also personally really enjoy it because of that.” Pulmonologist 6.
Pulmonologists and COPD nurses across all regions indicated that systematic screening of patients had enhanced their awareness of palliative care needs.
“[…] in the past, I often thought, oh, it’ll be fine, he’ll still have years. And now I’m more alert to it, so I think that’s a really important factor, which makes me think more quickly that we need to have a conversation.” Pulmonologist 2.
Perceived difficulties of the intervention
HCPs across all regions experienced that most patients were open to discussing palliative care topics. However, reactions differed, and adapting to the patient’s level of readiness was found essential.
“Um, at the beginning of the project, I did it quite abruptly […]. I also noticed that people were a bit frightened, [...] that I thought, oh yes, this has to be done more gradually.” COPD nurse 7.
Across all regions, the collaboration between the hospital and primary care was perceived inadequate due to time constraints and lack of an appropriate communication tool. Also, some pulmonologists had doubts about what to communicate to GPs, as the level of palliative care expertise varied greatly between GPs. COPD nurses in primary care were found to be important for adequate transmural communication, but they were not always available due to staff shortages and budget cuts.
Inner setting
Tension for change
Almost all HCPs felt that improvement in palliative care was highly needed and they were willing to improve care.
Available resources
Busy schedules made planning palliative care conversations challenging, particularly when both a pulmonologist and COPD nurse were involved. In one region, this was solved by reserving a weekly set time in the pulmonologist’s agenda. Whether conversations were scheduled depended greatly on clear working arrangements and staff continuity.
Relative priority
When the COVID-19 pandemic broke out in March 2019, HCPs experienced that priorities changed. Multidisciplinary meetings were cancelled, and palliative care conversations were postponed to keep patients out of the hospital.
Networks and communications
In each region, a COPD nurse became part of the specialist palliative care team to exchange knowledge. However, the extent of and satisfaction with collaboration between pulmonary and palliative care providers varied between regions. In one region, friction arose because palliative care providers had expected to become involved more often, but pulmonary care providers found them too direct in their approach to patients with COPD.
Characteristics of the individuals
Knowledge and beliefs about the intervention
Experiencing the positive effects on the patient motivated HCPs across all regions to continue implementing the intervention.
“Because you do the questionnaire [ProPal-score] with the patient, is it positive or not? And you also schedule appointments with the patient in a really clear way, it gives it all structure and clarity and by doing it you gain self-confidence and the reaction of the patient is generally very positive and yes, that also gives us a reason to continue, well, the way we took is just the right way.” COPD nurse 5.
Also, sharing experiences with other regions during the project meetings was reported by four HCPs to be very helpful.
Self-efficacy
Most pulmonologists and two COPD nurses reported initially feeling uncomfortable starting a palliative care conversation, but their confidence increased the more they did it. The communication training and example phrases were perceived as helpful. Most pulmonologists and COPD nurses preferred to hold the conversations partly together because it was more efficient and made it easier to start the conversation.
“That actually really helped me, I think, it also supported me a bit, that I found it a little less scary. Because it is quite difficult to start a conversation like that.” Pulmonologist 2.
“Because […] I do the introductory talk, it’s easier for the pulmonologist to continue the conversation in that half hour. Um, and in this way it’s a bit more structured, the pulmonologist doesn’t have to block a full hour for it, and in this way, we complement each other well.” COPD nurse 2.
Implementation process
Planning, Reflecting and Evaluating
Regional action plans were not used to guide implementation, but HCPs of three regions indicated that they made verbal work agreements. Working together in a small team helped to make those agreements and keep them. HCPs of one region noticed that it worked well to schedule weekly meetings at a fixed time.
“The big stick is that you just get together every week, [...] to implement the actions that each person is assigned.” COPD nurse 2.
Engaging
In all regions, implementation was primarily focused on identification and palliative care conversations. As a result, transmural collaboration only came into focus later in the project. To the disappointment of some, team members from primary care and specialist palliative care were not actively involved in the implementation process because their potential contribution was unclear.
“I didn’t notice so much here the role of the specialised general practitioner. I had a different expectation.” General Practitioner 2.
Implementation leader
A dedicated implementation leader feeling responsible for the implementation and keeping everyone engaged was deemed essential by HCPs across all regions. In one region, no one was explicitly made responsible, which hampered implementation.
Discussion
Main findings
This mixed-method study provides a detailed understanding of the implementation process of palliative care components into routine COPD care, how a multifaceted strategy can influence this process, and essential factors for successful implementation. Training sessions with roleplay were positively evaluated and increased the self-efficacy in providing palliative care. Of all patients screened, around half received an outpatient palliative care conversation, on average six weeks after inclusion and mostly held by a pulmonologist and COPD nurse together. Continuity and coordination of care remained limited, and aftercare was not done at all. The most important implementation barriers were time constraints, the COVID-19 pandemic, and barriers related to interdisciplinary and transmural collaboration. Factors facilitating implementation were: the systematic screening of palliative patients, adapting to the patient’s readiness, conducting palliative care conversations together with a pulmonologist and COPD nurse, and meeting regularly with a small team led by a dedicated implementation leader. Our findings will guide future implementation efforts to integrate a palliative care approach into COPD care and provide insights into the most effective components.
Implementation strategies
A multifaceted implementation strategy was used to optimize uptake of the intervention, [22] but the appropriateness varied per individual strategy. In line with previous research, communication training with roleplay by actors was positively evaluated by HCPs and increased their self-efficacy in providing palliative care [14, 23, 24]. Also, sharing best practices between regions during project meetings was positively evaluated and perceived as inspiring to continue implementation. However, the online toolbox and regional action plans were less used than anticipated. Filling in the plans proved too abstract and time-consuming for busy HCPs. As a result, implementation proceeded largely unstructured and depended greatly on the implementation leader’s enthusiasm. For future implementation efforts, we recommend providing HCPs with clear instructions and practical ready-to-use tools and scheduling frequent team meetings led by a dedicated implementation leader.
Palliative care conversations
Systematic screening of patients appeared to be an essential intervention component. It raised HCPs’ awareness and made them more ready to initiating palliative care conversations. However, the ProPal-COPD tool’s performance appeared to be unsatisfactory. External validation results and user experiences will be discussed in a separate publication. With 45% of patients identified, a palliative care conversation was held. Despite of the COVID-19 pandemic, this percentage is comparable to previous studies. In the systematic review of Houben et al. on advance care planning interventions, [25] the occurrence of palliative care conversations in intervention groups of included studies ranged from 18 to 64% [26,27,28,29,30]. HCPs were very positive about the palliative care discussions, but alignment with patient readiness was deemed important as COPD is not considered as ‘potentially lethal’ by most patients [31]. It is less confronting to patients if advance care planning is initiated gradually with topics related to dying and death introduced step-by-step over multiple conversations. In our study, using a dual-track approach (“hope for the best, and prepare for the worst”), [32] it was possible to introduce such topics already in an earlier stage. Pulmonologists highly valued collaboration with a COPD nurse as it helped them discuss sensitive topics and saved time. Indeed, blocking enough time for the palliative care conversations was challenging. Therefore, scheduling conversations at the end of the consultation hour to allow for possible extension or scheduling a fixed time in the week is recommended.
Interdisciplinary collaboration
In line with guideline recommendations and care practices in the Netherlands, [4, 5, 33, 34] our intervention was delivered by respiratory HCPs (so-called generalist care providers), while specialist palliative care providers were only involved in the case of complex care needs. In our study, the level of involvement varied across regions. Respiratory HCPs were reluctant to involve the specialist palliative care team because they lacked COPD-specific knowledge regarding treatment and communication practices. Specialist palliative care providers are mainly involved with oncology patients, [35] whereas patients with COPD require a different approach [36]. Therefore, it should be further explored how respiratory and palliative care HCPs optimally collaborate and learn from each other’s expertise.
Transmural collaboration
The intervention component coordination & continuity was less well implemented across all regions. Although providers from primary care and the hospital were involved in the training, implementation leaders first focused on organizing outpatient palliative care conversations. Consequently, transmural collaboration received insufficient attention, as reflected by the low number of letters sent from hospital to the GP. Although HCPs expressed that contact by phone is preferred to optimize care coordination and continuity after a patient was identified, this was not always done due to time constraints and lack of a shared electronic medical record. Therefore, a communication tool to facilitate bidirectional communication (ideally digital, linked to medical files, and always accessible) is needed. Further, COPD nurses in primary care play an essential role in linking primary and secondary care and should be available in every region. Moreover, to optimize coordination and guarantee continuity of care, financial structures that allow flexibility and ‘shared care’ are warranted.
Strengths & limitations
This is the first comprehensive study assessing palliative care implementation in a real-world outpatient COPD care setting. We used different data sources to provide a broad and in-depth understanding of the implementation process. Furthermore, the intervention and implementation strategy were designed using theory, guidelines, and input of many stakeholders, ensuring that barriers from the field were addressed [15]. However, our study also has some limitations. First, the COVID-19 pandemic had severe implications that may have biased our findings. HCPs had less time for implementation activities, multidisciplinary meetings were put on hold, and palliative care conversations were cancelled to prevent contamination. Second, our implementation results were somewhat constrained because it was performed alongside a cluster randomised controlled trial (as part of a hybrid type 2 effectiveness-implementation study) [15]. Next to the positive aspects of combining these two study objectives, such as faster knowledge development, [37] it limited our flexibility to adapt to new insights that emerged during the study. For example, the fixed inclusion criteria required for effectiveness evaluation limited the measured reach because palliative patients identified at the outpatient clinic could not be included. Also, HCPs were focused on enrolling patients for sufficient power of the effectiveness study, limiting their time for implementation activities. Finally, we did not assess the quality of implementation, e.g. the quality of palliative care conversations. In future studies, this could be assessed using conversation analysis, as was found to be a viable method by Otte et al. [38].
Conclusion
Implementation is a complex process, and dedicated action is needed to ensure theoretically promising and highly needed interventions, such as palliative care for patients with COPD, are delivered as intended. The multifaceted implementation strategy evaluated in the COMPASSION study demonstrated the importance of communication training in discussing palliative care topics with patients with COPD in a sensitive way, systematic screening of patients with palliative care needs, and a structured implementation process led by a dedicated implementation leader. It also highlighted that we are not there yet; future research should focus on optimizing transmural and interdisciplinary collaboration, to ensure optimal integration and continuity of palliative COPD care.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to the confidentiality and the traceability of the data but are available from the corresponding author on reasonable request.
Abbreviations
- CFIR:
-
Consolidated Framework of Implementation Research
- COPD:
-
chronic obstructive pulmonary disease
- EPCS:
-
End-of-life Professional Caregiver Survey
- HCP:
-
healthcare provider
References
Habraken JM, ter Riet G, Gore JM, Greenstone MA, Weersink EJ, Bindels PJ, et al. Health-related quality of life in end-stage COPD and lung cancer patients. J Pain Symptom Manag. 2009;37(6):973–81.
Boddaert M, Douma J, Dijxhoorn F, Bijkerk M. Netherlands quality framework for palliative care. Utrecht: IKNL/Palliatief; 2017.
Rietjens JAC, Sudore RL, Connolly M, van Delden JJ, Drickamer MA, Droger M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–51.
Lanken PN, Terry PB, Delisser HM, Fahy BF, Hansen-Flaschen J, Heffner JE, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177(8):912–27.
Netherlands Comprehensive Cancer Organisation & Lung Alliance Netherlands. National guideline Palliative care in patients with COPD, version 2.0. Utrecht: IKNL/LAN; 2021.
Broese JMC, van der Kleij R, Verschuur EML, Kerstjens HAM, Engels Y, Chavannes NH. Provision of palliative Care in Patients with COPD: a survey among pulmonologists and general practitioners. Int J Chron Obstruct Pulmon Dis. 2021;16:783–94.
Jabbarian LJ, Zwakman M, van der Heide A, Kars MC, Janssen DJA, van Delden JJ, et al. Advance care planning for patients with chronic respiratory diseases: a systematic review of preferences and practices. Thorax. 2018;73(3):222–30.
Reipas KM, Grossman DL, Lock K, Caraiscos VB. Examining the characteristics of patients with non-malignant lung disease at the time of referral to an inter-professional supportive care clinic. Am J Hosp Palliat Care. 2021;38(11):1329–35.
Janssen DJ, Spruit MA, Uszko-Lencer NH, Schols JM, Wouters EF. Symptoms, comorbidities, and health care in advanced chronic obstructive pulmonary disease or chronic heart failure. J Palliat Med. 2011;14(6):735–43.
Broese JM, de Heij AH, Janssen DJ, Skora JA, Kerstjens HA, Chavannes NH, et al. Effectiveness and implementation of palliative care interventions for patients with chronic obstructive pulmonary disease: a systematic review. Palliat Med. 2021;35(3):486–502.
Tavares N, Jarrett N, Hunt K, Wilkinson T. Palliative and end-of-life care conversations in COPD: a systematic literature review. ERJ Open Res. 2017;3(2).
Aldridge MD, Hasselaar J, Garralda E, van der Eerden M, Stevenson D, McKendrick K, et al. Education, implementation, and policy barriers to greater integration of palliative care: a literature review. Palliat Med. 2016;30(3):224–39.
Meehan E, Foley T, Kelly C, Burgess Kelleher A, Sweeney C, Hally RM, et al. Advance care planning for individuals with chronic obstructive pulmonary disease: a scoping review of the literature. J Pain Symptom Manag. 2020;59(6):1344–61.
Chung HO, Oczkowski SJ, Hanvey L, Mbuagbaw L, You JJ. Educational interventions to train healthcare professionals in end-of-life communication: a systematic review and meta-analysis. BMC Med Educ. 2016;16:131.
Broese JMC, van der Kleij R, Kerstjens HAM, Verschuur EML, Engels Y, Chavannes NH. A cluster randomized controlled trial on a multifaceted implementation strategy to promote integrated palliative care in COPD: study protocol of the COMPASSION study. BMC Palliat Care. 2020;19(1):155.
Pinnock H, Barwick M, Carpenter CR, Eldridge S, Grandes G, Griffiths CJ, et al. Standards for reporting implementation studies (StaRI) statement. BMJ (Clinical research ed). 2017;356:i6795.
Duenk RG, Verhagen C, Bronkhorst EM, Djamin RS, Bosman GJ, Lammers E, et al. Development of the ProPal-COPD tool to identify patients with COPD for proactive palliative care. Int J Chron Obstruct Pulmon Dis. 2017;12:2121–8.
Lazenby M, Ercolano E, Schulman-Green D, McCorkle R. Validity of the end-of-life professional caregiver survey to assess for multidisciplinary educational needs. J Palliat Med. 2012;15(4):427–31.
Steckler A, Linnan L. Process evaluation for public health interventions and research. San Francisco: Jossey-Bass; 2002.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50.
van Riet PJ, Vernooij-Dassen M, Sommerbakk R, Moyle W, Hjermstad MJ, Leppert W, et al. Implementation of improvement strategies in palliative care: an integrative review. Implement Sci. 2015;10:103.
Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167(5):453–60.
Tilburgs B, Koopmans R, Vernooij-Dassen M, Adang E, Schers H, Teerenstra S, et al. Educating Dutch general practitioners in dementia advance care planning: a cluster randomized controlled trial. J Am Med Dir Assoc. 2020;21(6):837–842.e834.
Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(7):477–89.
Au DH, Udris EM, Engelberg RA, Diehr PH, Bryson CL, Reinke LF, et al. A randomized trial to improve communication about end-of-life care among patients with COPD. Chest. 2012;141(3):726–35.
Clayton JM, Butow PN, Tattersall MH, Devine RJ, Simpson JM, Aggarwal G, et al. Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol. 2007;25(6):715–23.
Heffner JE, Barbieri C. Effects of advance care education in cardiovascular rehabilitation programs: a prospective randomized study. J Cardpulm Rehabil. 2001;21(6):387–91.
Jacobsen J, Robinson E, Jackson VA, Meigs JB, Billings JA. Development of a cognitive model for advance care planning discussions: results from a quality improvement initiative. J Palliat Med. 2011;14(3):331–6.
Pearlman RA, Starks H, Cain KC, Cole WG. Improvements in advance care planning in the veterans affairs system: results of a multifaceted intervention. Arch Intern Med. 2005;165(6):667–74.
Knauft E, Nielsen EL, Engelberg RA, Patrick DL, Curtis JR. Barriers and facilitators to end-of-life care communication for patients with COPD. Chest. 2005;127(6):2188–96.
Back AL, Arnold RM, Quill TE. Hope for the best, and prepare for the worst. Ann Intern Med. 2003;138(5):439–43.
Quill TE, Abernethy AP. Generalist plus specialist palliative care--creating a more sustainable model. N Engl J Med. 2013;368(13):1173–5.
Henderson JD, Boyle A, Herx L, Alexiadis A, Barwich D, Connidis S, et al. Staffing a specialist palliative care service, a team-based approach: expert consensus white paper. J Palliat Med. 2019;22(11):1318–23.
Beernaert K, Cohen J, Deliens L, Devroey D, Vanthomme K, Pardon K, et al. Referral to palliative care in COPD and other chronic diseases: a population-based study. Respir Med. 2013;107(11):1731–9.
Ngwenya N, Crang C, Farquhar M, Rintoul RC, Mahadeva R, Calvert LD, et al. Communicating uncertainty: contrasting the communication experiences of patients with advanced COPD and incurable lung cancer. Fam Pract. 2021;38(5):637–43.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–26.
Otte R, Roodbeen R, Boland G, Noordman J, van Dulmen S. Affective communication with patients with limited health literacy in the palliative phase of COPD or lung cancer: analysis of video-recorded consultations in outpatient care. PLoS One. 2022;17(2):e0263433.
Acknowledgements
We thank all patients, informal caregivers, and healthcare providers who participated in the COMPASSION study. We are very grateful for the enthusiasm, effort, and dedication of all involved primary and secondary healthcare providers of the four intervention regions: Langeland Hospital in Zoetermeer, Martini Hospital in Groningen, Slingeland Hospital in Doetinchem, and Zaans Medisch Centrum in Zaandam. In particular, we would like to thank Sandra Been-Buck, Gerrit Bosman, Linda Brandjes, Leonie Bruil, Karin Eikenaar, Ellen Jacobs-Taag, Titia Klemmeier, Martijn Kross, Sarah van Oord, Carla van de Spek, and Maritha Spekschoor. We thank Noortje van Vliet for her help in collecting data from medical records.
Funding
This research project has been financially supported by The Netherlands Organization for Health Research and Development (ZonMw) (project no. 844001401).
Author information
Authors and Affiliations
Contributions
J.B., R.K, H.K., Y.E. and N.H. designed the study protocol; E.V. and J.B. led the development and implementation of the training and toolbox and held monitoring meetings; Y.E. led project meetings; J.B. and E.V. collected data; J.B. and R.K. performed data analyses, and the research group discussed preliminary and definitive findings; J.B. wrote the first draft; All authors contributed to critical revision and agreed with the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed according to the Dutch law, the principles outlined in the Declaration of Helsinki, and Good Clinical Practice guidelines. The Medical Ethics Committee of the Radboud University Medical Centre approved the study protocol and concluded that the study was not subject to the Medical Research Involving Human Subjects act (number 2018–4833). All participating patients gave their written informed consent to use their medical data.
Competing interests
The authors declared no potential conflicts of interest concerning the research, authorship, or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Broese, J.M.C., van der Kleij, R.M.J.J., Verschuur, E.M.L. et al. Implementation of a palliative care intervention for patients with COPD – a mixed methods process evaluation of the COMPASSION study. BMC Palliat Care 21, 219 (2022). https://doi.org/10.1186/s12904-022-01110-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-022-01110-3