Abstract
Background
Those experiencing socioeconomic deprivation have poorer quality of health throughout their life course which can result in poorer quality of death – with decreased access to palliative care services, greater use of acute care, and reduced access to preferred place of care compared with patients from less deprived populations.
Aim
To summarise the current global evidence from developed countries on end-of-life experience for those living with socio-economic deprivation.
Design
Integrative review in accordance with PRISMA. A thorough search of major databases from 2010–2020, using clear definitions of end-of-life care and well-established proxy indicators of socio-economic deprivation. Empirical research describing experience of adult patients in the last year of life care were included.
Results
Forty studies were included from a total of 3508 after screening and selection. These were deemed to be of high quality; from a wide range of countries with varying healthcare systems; and encompassed all palliative care settings for patients with malignant and non-malignant diagnoses. Three global themes were identified: 1) multi-dimensional symptom burden, 2) preferences and planning and 3) health and social care interactions at the end of life.
Conclusions
Current models of healthcare services are not meeting the needs of those experiencing socioeconomic deprivation at the end-of-life. Further work is needed to understand the disparity in care, particularly around ensuring patients voices are heard and can influence service development and delivery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
On a global scale, it is now recognized that people experiencing socioeconomic deprivation (SED) are spending more of their shorter lives in ill health and are carrying a higher burden of chronic disease, multimorbidity and symptom burden than more affluent neighbours [1,2,3]. Socioeconomic deprivation is an independent risk factor for higher mortality in both cancer and non-cancer populations [4,5,6] and is associated with higher use and cost of healthcare in the last year of life [7, 8].
Given that people living with SED are carrying this inequitably high burden of poor health outcomes, equal access to palliative care would be expected when compared with those in more affluent areas. However, it is now recognised that people with lower incomes have a potentially poorer experience at end-of-life (EOL) [6], with reduced referral and access to specialist palliative care services in and out of hours [9,10,11], are more likely to use ambulance and A&E and to be admitted to and die in hospital [7, 12, 13], rather than at home or in a hospice [9, 10, 14,15,16,17]. People with lower wealth have recently been found to have had more hospital admissions in the last two years of life [18] and this is often a substitute for elective, community-based healthcare services [19]. Families living in poverty may need to compromise on food and heating and incur significant debts when someone dies [20] and report significantly less support and satisfaction with care received at the EOL [6]. A qualitative evidence synthesis, undertaken in 2019, identified that access to preferred place of death was limited by human factors, such as social support, personal and cultural beliefs, poor communication, and environmental factors, such as suitability of the home environment, and availability of resources within health and care services [21]. An earlier review highlighted barriers such as accessibility, availability, affordability and acceptability [22].
As quantitative evidence describing the disparity in access and delivery of palliative care services between socioeconomic groups continues to grow, there is still little understanding of how people with SED experience living and dying with a life-limiting illness. This review feeds directly into ongoing empirical work to understand the experiences of home death for people at the EOL who are living with poverty [23] and complements a recently published paper by Rowley and colleagues [24] by providing a comprehensive and systematic description of the issues experienced at EOL. This manuscript provides further justification for Rowley et al.’s call to action for researchers, policy-makers and clinicians working with people experiencing socioeconomic deprivation at EOL [24]. By understanding what inequalities and disparities persist, practitioners and policy makers can meaningfully address the issue at individual, institutional and societal levels and progress can be made to narrow the gap. The aim of this review is to describe current global evidence from high income countries on the experiences of people at the EOL who are living with SED.
Methods
Design
An integrative literature review approach was chosen to facilitate synthesising and concept building given the multiple evidence sources and methodologies. We conducted our review according to the methods described by Whittemore and Knafl [25]. This study was registered on PROSPERO (CRD42019151906) [26] and reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27].
Definitions
We used the NICE definition for EOL which includes people who are likely to die within 12 months, with advanced, progressive, or incurable diseases or acute life-threatening conditions [28]. We also referred to Rietjens recent article to develop our search terms related to palliative care; these were developed from the World Health Organisation broad and accepted definition of palliative care – “Palliative care is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” [29, 30]. The definitions available for socioeconomic status are less distinct. Clear definitions are rare (i.e. the United Kingdom Index of Multiple Deprivation), do not encompass the complex nature of SED and are particularly poor at capturing rural SED [31]. We therefore reviewed the evidence on proxy indicators of SED in addition to systematic reviews of the same topic to devise the evidence-based list of search terms related to SED which are presented in Table 1 [7, 32, 33]. This review did not include papers from developing countries given their unique challenges to resources and the delivery of healthcare.
There have been multiple recently published reviews focussing on the interaction of socioeconomic inequities and place of death and access [13, 34,35,36]. Such studies have utilised different approaches in their definitions of the dynamic concept of access including the Levesque’s five domains [34] and the candidacy model [36]. The similarity in such concepts of access is the identification of patients both by self and professionals as needing a particular healthcare service, the initial contact and subsequent uptake of that service and to actually have a need for the services fulfilled. With this in mind, our criteria (Table 2) excluded papers which solely focused on initial contact with or referral to palliative care services, patient and professional perceptions of palliative care need and availability of resources.
Search strategy
Key search terms were agreed between SB and EC, with support from a librarian based at NHS Greater Glasgow & Clyde, and these were combined with standard Boolean operators (Table 1). The following databases were searched to capture the wide range of research and disciplines involved in SED at the EOL – Medline, Embase, CINAHL, ASSIA and PsychInfo. The most relevant systematic review to describe palliative care in the context of SED was reported in 2010 [22] and thus we limited our search from January 2010 to March 2020. Inclusion and exclusion criteria were agreed to ensure we obtained relevant, original research (Table 2).
Study selection
Initial screening by title and abstract was conducted by SB and MC. Both authors screened the first 20 papers for inclusion to ensure consistency. Full texts were then reviewed according to the inclusion and exclusion criteria. Where there was uncertainty, papers were read by EC and a decision was made as a team.
Quality appraisal
Given the breadth of research designs obtained by integrative reviews, there is no gold standard for quality appraisal [25]. However, a research critique framework developed by Caldwell et al. [38] was considered suitable to assess quality in both qualitative and quantitative papers. Bloomer et al. used the Caldwell criteria in a recent integrative review and shared the flowchart they had developed [39]. The methodological strengths and weaknesses of each included study were assessed independently with SB and MC using the Caldwell 11 point criteria. Final scores were corroborated and differences discussed.
Data abstraction and synthesis
We followed the four steps as described by Whittemore and Knafl: 1) data reduction, 2) data display, 3) data comparison, 4) conclusion drawing [25]. The papers were reviewed and data extracted on: full reference, continent, language, how SED was defined, how EOL was defined, aim, objectives or research questions, design, setting for data collection, participants, diagnosis, sample size, tools, key findings, limitations as described, author conclusions, references to other relevant studies.
With the aim of the review in mind, SB and MC thoroughly read each of the included papers independently and extracted the relevant findings. These were then categorised into 15 broad themes which were assimilated into an excel database. Using the constant comparison method outlined by Whittemore and Knafl [25], extracted data were compared item by item to allowing grouping and categorization allowing varied data from diverse methodology to be collated. The final 3 global themes, and 9 subthemes, were then created based on the above groupings of the findings with corroboration from all authors.
Findings
Included studies
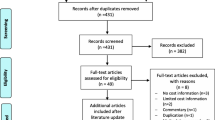
In total, 2458 studies were found after removal of duplicates as illustrated in Fig. 1. Initial screening of titles and abstracts resulted in 236 papers for full-text review. Ultimately, 40 studies were included in the analysis. A list of these papers is included in Table 3. In total, 38 out of 40 papers were of high quality with a score of 9/11 or higher, the remaining 2 papers scored 8/11. Given the experiences of people living in SED have not been well described in detail in the literature, we did not exclude on the basis of quality.
Most studies originated in North America (23/40); 8 in Europe (one of these was UK based); 7 in Asia; 1 Australia and 1 was cross-continent between USA and Europe. The studies were conducted in different healthcare settings including community, hospital and hospice. Some [9] were population studies. Most studies (28/40) recruited patients with cancer diagnoses; 11 did not specify a particular diagnosis and only one looked exclusively at patients with a non-malignant diagnosis – Chronic Obstructive Pulmonary Disease (COPD). Quantitative designs were most commonly used (34/40). There were 3 qualitative studies and the remaining 3 using mixed methodologies. The total sample size of the included studies was 439,423 (range = 18 – 307,188).
The studies included used a variety of definitions to define SED. Twenty-two studies used only one marker in their analysis: education status (n = 7); household income (n = 4); insurance status (n = 3 from the USA); subgroups of employment (n = 2); specifically designed SED scores as the single marker of SED (n = 2) i.e. the Carstairs SED score and the Index of Relative Disadvantage; decedent postal code linked to nationally available data on poverty rates and estimated income (n = 2); patient self-reported financial strain (n = 1); structurally vulnerable (n = 1). The remaining 18 studies used multifactorial markers of SED.
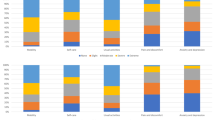
The amalgamated findings of our research are presented below in 3 global themes (Fig. 2):
-
Multidimensional Symptom Burden at the EOL: This encapsulates the broad physical, psychological, social and financial issues that patients experience in the last year of life under the subthemes of: physical symptoms, psychological symptoms and social and financial stress.
-
Preferences and Planning at the EOL: This describes the patient-reported favoured modalities of care in the last year of life and activities taken to plan for such outcomes.
-
Health and Social Care Interactions at the EOL: This shows how patients use different healthcare services and what their reported satisfaction is with such encounters.
Multidimensional symptom burden at the EOL
Physical symptoms
There were 3 studies exploring physical symptom burden [42, 44, 69, 72].Lower income and education levels were generally associated with higher physical symptom burden, with pain being widely reported [42, 69]. Poverty was also found to be associated with increased receipt of medication for pain, dyspnoea and emotional distress [72]. However, the association between higher physical symptom burden and SED was not sustained in one study [44] where no difference was found in symptom burden between insured and uninsured patients.
Psychological symptoms
The evidence on the relationship between SED and psychological wellbeing is conflicting and was described across 6 of the included studies [50, 56, 64, 67, 68, 74]. While one study found that financial difficulty was associated with lower functional, emotional and spiritual wellbeing [74] another found that unemployed patients with cancer had less anxiety and depression [67]. Similarly, Dhingra et al. found that patients living in impoverished neighbourhoods reported very low illness burden (defined as physical functioning, symptom distress, unmet needs and quality of life) [50]. One study showed that lower education was associated with higher hopelessness and depression rates [64] but education levels generally did not impact on levels of psychological distress, anxiety or depression scores [67, 74].
There is no consistent evidence regarding coping ability. Tang et al. showed that higher education was associated with higher post-traumatic growth scores, showing positive personal development and adjustment to trauma [56]. However, Chochinov et al. reported that patients with higher education were more likely to report feelings of having lost control, unfinished business, and poorer coping with activities of daily living [68].
Social and financial stress
Only 2 studies described the social support available to patients, from government agencies and more informal routes [60, 70]. Lewis et al. described limited family support, often a sole caregiver, and sometimes fragile relationships in situations that could be compounded by violence and alcohol in their studied population in a lower socioeconomic area in Western Sydney, Australia. There was a heavy reliance on other sources of support, but welfare support and government housing agencies were described as difficult to navigate and community support (including informal support from neighbours and formalised primary care and community nursing support) was described as inconsistent, unpredictable and inadequate to meet patient need [60]. Once a connection was able to be established, patients who had previously engaged with government agencies prior to their illness described subsequent interactions as a positive experience. However, for those who had no prior connection, the experience, particularly around negotiating benefits was challenging [60].
In one study, women with breast cancer in the US expressed a desire to maintain social connections, describing this as a key aspect of a meaningful life, alongside creative outlets and spirituality. For those living alone, in lower socioeconomic populations, neighbourhood networks were essential to sustain care and social needs [70].
Four studies in countries with both publicly funded and private healthcare systems described the impact of ill-health on finances when living with pre-existing poverty [40, 70, 73, 75]. Financial distress was common prior to diagnosis but worsened after due to medical costs and inability to work. Patients who had low income or who were in financial poverty allocated a larger proportion of family income to health expenses and were more likely to report catastrophic health expenditure and higher health costs at the EOL [73, 75].
Similarly, a qualitative study of low-income patients with breast cancer in America found that most patients had difficulty meeting basic needs, inadequate financial resources, and were unable to work, resulting in them feeling burdensome and useless [70].
Drug reimbursement due to terminal illness (DRTI) is a scheme available in Denmark for patients with incurable disease and a short life expectancy allowing for prescription medicines to be obtained free of charge. However, the authors noted that patients with lower income were less likely to use the DRTI scheme [40].
Preferences and planning at the EOL
Preferences
Preferences for EOL care were described in 5 studies [49, 54, 61, 76, 78]. Overall, patients with higher education level were more likely to choose supportive care. Tang et al. reported that patients with higher education level were more likely to accurately know their prognosis, which was in turn associated with greater odds of preferring comfort-orientated and hospice-based care at the EOL [61]. Carlucci et al. provided patients with advanced COPD theoretical scenarios and found those with a higher education level were more likely not to choose EOL sustaining treatments such as intubation and non-invasive ventilation. Of note, the study also suggested that all participants’ understanding of choices were suboptimal, with over 40% of participants being unable to correctly define the comfort/supportive option [49]. Saeed et al. found that education did not affect participants’ preference to receive comfort/supportive care [76], however the sample consisted of mainly highly educated participants.
Future care planning
Future care planning, including designation of power of attorney, EOL discussions, and completion of written instructions for care at EOL, was described in 3 studies [52, 69, 76]. Khosla et al. found that although higher household income increased the odds of having a legally designated power of attorney for healthcare, this did not impact on EOL discussions or written instructions. They also showed that education level did not impact advanced care planning behaviour [52]. Carr et al. found that having assets significantly increased the likelihood of participants having a living will or legal power of attorney but did not impact on informal EOL discussions [69]. In contrast, another study looking at a sample of lower income patients found that education level and financial strain did not affect completion of advanced care directives [76].
Health and social care interactions at EOL
Service use
Nine studies described what and how palliative care services were used [40,41,42, 46, 51, 55, 58, 63, 71]. The evidence shows that even when patients had equal access to palliative care services, differences in the uptake of these persisted across different indicators of socioeconomic status. For example, those with higher income or living in a neighbourhood with a higher socioeconomic status, were significantly more likely to have inpatient hospice admissions [51].
The literature points to a distinction between which services are desired or used by patients based on their socioeconomic status. Ankuda et al. showed that patients with financial strain described the connection to social services offered by an at home palliative care service including transportation, help with navigating insurance policies or benefits and food stamps as what mattered most due to self-perceived poverty, disability and high medication cost [41]. Another reason for reliance on practical or social support may be explained by the availability of informal caregivers. For example, Bijnsdorp et al. described a positive correlation between educational attainment and availability of partner care-networks, defined as care provided primarily by a partner in the last year of life, particularly for patients younger than 77.9 years [71]. Similarly, a home-based palliative care service in Canada found a difference in unpaid caregiving hours provided for those with the highest socioeconomic status and the lowest socioeconomic status of 6.18 h and 2.66 h, respectively [46].
When those experiencing SED have accessed specialist palliative care services, there is some evidence that they use them more thereafter. The literature shows that this is the case for both routine and non-routine care and across the different services offered by palliative care. For example, patients with either limited insurance (Medicaid) or no health insurance had more follow up appointments with a hospital palliative care service [42]. This finding persisted for universal, publicly funded health insurance systems. Two Canadian home-based palliative care services showed that patients with higher levels of SED and lower levels of educational attainment had increased propensity and intensity of support worker and nurse visits [46, 63]. The type of support from General Practitioners may also show some slight variation for patients in the last year of life. For example, patients with cancer in the last year of life were more likely to have GP face-to-face visits if they had a lower income [55].
Treatment intensity
Treatment intensity at EOL was described in 8 studies [43, 45, 47, 48, 51, 57, 59, 65]. In most of the studies included, patients with lower income, lower education levels, or no insurance, were generally more likely to receive intensive treatment at the EOL [43, 45, 57, 59]. Such treatments included chemotherapy, attendance at emergency departments or > 14 days hospitalisation prior to death, intensive care admission, use of mechanical ventilation and cardiopulmonary resuscitation. Lower income and lower education level also led to increased rate of transfer from home or nursing home to secondary care in the last months of life [48]. Having an inpatient hospice admission during the last 6 months of life reduced hospital admissions by almost half. However, patients with lower income and lower education were less likely to utilise hospice [51].
A few studies were contradictory. A Taiwanese study showed that whilst low income was associated with increased likelihood of hospital admission beyond 14 days and death in an acute hospital, higher income patients were more likely to attend the emergency department and be admitted to intensive care units [45]. One study of cancer patients showed that those with higher education levels were more likely to receive diagnostic and therapeutic procedures at the EOL [47]. Bergman et al. described an analysis of a dedicated programme for men with low income and prostate cancer, and found rates of chemotherapy use, emergency and intensive care admissions and inpatient stays for those in the programme were comparable to the general population [65].
Patient satisfaction
There is limited and conflicting evidence relating socioeconomic status to patient satisfaction with palliative care services as described in six of the included studies [41, 53, 62, 66, 70, 77]. Lower levels of education were linked in one study to higher satisfaction with care [62] whilst another showed no association with ratings on quality of death and dying for patients or family [79]. Patients with financial strain rated a home palliative care programme the highest of all socioeconomic groups [41].
The available qualitative research pointed to concerns from patients experiencing SED around the use of palliative care services. For example, patients described that having reduced financial means and lack of private insurance meant they did not receive the same high quality care [79]. Patients living in poverty felt a negative bias and stigmatization from healthcare professionals towards them due to their lower socioeconomic class and this impacted on perception of the care received [79]. One general practitioner out-of-hours service in a deprived area in Scotland was found to be stressful and cumbersome to use with patients describing bad experiences or feeling their care needs were too complex for this service [66]. A Canadian study of those who were homeless, or at risk of such, described that patients often had their care needs unidentified and unmet. However, when patients were linked to palliative care services, they reported feeling listened to and reported that services were extremely accommodating and attentive to their needs [77].
Discussion
We reviewed, integrated and summarised evidence on the EOL experiences of people living with SED in high income countries. Forty heterogenous studies were identified from a wide range of countries with varying healthcare systems and encompassed both malignant and non-malignant diseases. Three global themes were identified relating to the multi-dimensional EOL experience, preferences and planning and service uptake and utilization. The following key findings were identified—those living with SED have: increased symptom burden; difficulty navigating complex healthcare systems at the EOL and increased intensity of use of these once a link is established; a preference for, and are more likely to have, intensive treatment at the EOL; limited formal and informal social support; a greater propensity to experience financial distress; and, less participation in advanced care planning.
Previous research has shown that people experiencing SED use palliative care services differently and that current universally available models often fail to meet patients’ needs [7, 9,10,11,12, 14,15,16,17,18, 40]. Navigating and negotiating multiple and complex systems in order to access essential support may be overwhelming. For example, social service support with transport, navigating insurance, benefits and food stamps mattered most in Ankuda et al. [51], particularly when compounded by unpredictable community support [60, 70] and a lack of unpaid family caregiving [46, 71]. Our work lends further argument to the call for proportionate universalism, where marginalised groups need systems to be designed to incorporate their needs, rather than needing them to adapt to a universal healthcare system, and for time and resources to be proportionate to the level of disadvantage [80, 81].
Dying can be expensive, for both patients and the people caring for them. In addition to existing financial constraint, further loss of income, changes to benefits and treatment-related costs can be catastrophic [70, 75, 82]. Interestingly, even when a drug reimbursement system was available in Denmark, patients from poorer backgrounds were less likely to claim it [40]. This supports what we already know – that financial benefits do not always reach those who need them most. In the UK alone, up to £6.2billion of income-related benefits went unclaimed in 2018–2019 [83]. Ultimately, patients and families may not get access to the financial support they need to mitigate the costs associated with EOL, including fees for diagnostic interventions, hospice or home care and reduced household income as relatives become unemployed unpaid caregivers. This financial distress can leave patients and caregivers feeling devalued, and financially burdensome [70]. Our findings highlight that in order to tackle the systemic issues of social justice which impact on EOL experience, we must adopt multidisciplinary and multi-agency approaches to support families to navigate health and social care and benefits systems. Our review suggests that people experiencing SED valued the non-medical support from palliative care services most, particularly around use of social and supportive services and were less likely to have informal caregivers [46, 60].
Our findings showed that people living in SED absorbed palliative care services when they could gain access to them, with demonstrable higher intensity of use, particularly with regards to outpatient and community-based services [13, 42, 46, 63]. Additionally, our review suggests that patients also have a greater physical symptom burden [42, 69, 84], thus making the greater use of palliative care services unsurprising. However, an alternative explanation could be that services and existing resources are failing to meet the complex needs of people experiencing SED, thus leading to repeated consultations. Barriers to quality care identified in this review have been multifactorial, complex, and difficult to address on a single level. Without significant changes to the way we deliver healthcare, the complexity of these barriers will only serve to widen the quality-of-care gap between deprived and affluent populations yet again, proving the inverse care law true.
Our review demonstrated that people living with SED had both a preference for, and tendency to receive intensive treatments at the EOL [43, 45, 47, 48, 51, 57, 59, 65] and recent research from Scotland added weight to these findings, with Mason et al. demonstrating that for those in the last year of life, living in SED used more unscheduled care (unplanned use of healthcare services) [11]. People living with SED may have more interaction with health and social care professionals and thus potentially more opportunity to engage with future care planning, yet this is not translating to the actual experience at the EOL. Whilst Davies et al. have demonstrated that part of the increased uptake of hospital-based services may be due to poorer health and function for those living in SED [18], until we start asking people about their EOL care experiences and preferences at the right time, in the right way, with consideration given to their limited opportunities to make choices throughout the life course, we will fail to understand the potentially complex nature of future planning for this group.
Strengths & limitations
This review summarises a thorough analysis of the literature from the developed world about the experience of those dying in SED. We include high quality studies from a variety of settings, healthcare systems and countries thus allowing our work to be transferable and applicable across high income countries. Excluding papers prior to 2010 and addressing well-explored issues of access and preferred place of death has allowed us to focus on the patient voice and experience. In doing so, we acknowledge that this has narrowed the scope of our manuscript but together with the recent reviews on access to palliative care and studies about place of death, there is now a comprehensive and contemporary body of research on how people die and the experiences they have.
Although we included a wide variety of different healthcare settings and systems in various countries, this also meant that there were a wide variety of cultural and societal differences which may limit the generalisability across settings. Indeed the majority of studies (45%, n = 18) originated in the United States, which is a similar geographical bias reflected in a previous literature review on access to palliative care services for socioeconomically deprived groups by Lewis et al., 2011 (49%, n = 33) [22]. Similar to that group, we acknowledge that the intersection of race with SED and impact of insurance-based health services could have had an impact on our findings. It is significant to note that the magnitude of US research remains persistent ten years later and perhaps reflects differences in availability of funding for palliative care research globally. Whilst we had intended to draw out the patient voice, only 3 studies using a qualitative design and a further 3 studies using mixed quantitative and qualitative research methods. As our findings show, the evidence was heterogenous and often contradictory, which can be challenging to analyse and synthesise. The lack of a standard definition for SED may have contributed to the heterogenous evidence and led researchers of the included papers seeking measures that could be easily obtained.
Implications for policy, practice and research
The voices of people experiencing SED at the EOL are underrepresented. The COVID-19 pandemic has disproportionately affected people living with poverty [85, 86], forced more families into poverty and has highlighted the fragility of health systems across the globe. Health inequalities are now a stark focus for policymakers globally [87]. Inclusive and participatory research, which enables patients and families to feed directly into this policy making and service design is a priority. We need to actively and broadly engage with policies beyond those of palliative care services at the end of life, to consider the complex needs of this group in societies and systems.
Our review highlighted a dearth of research on spirituality at the EOL for people living with poverty. Further exploration into this important but neglected area is recommended. We also need to understand why people are more likely to experience pain and receive intensive treatment at EOL. In general, patients with lower income were less likely to complete advanced care planning. Further exploration into the link between these two things is important but it is vital that health and social care professionals understand attitudes, experiences and preferences for future care discussions. Further research/implementation science to test specific initiatives in practice is required to better support people living with socio-economic deprivation.
The generalisability of SED research would be improved if standard markers could be agreed upon, at least in similar healthcare systems. Whilst this is not a critique of any particular SED marker, it may be that using a combination of SED markers, or a specifically designed SED score such as the Carstairs SED score would be more appropriate [88]. This echoes the work of social epidemiologists who advocate that valid measurements of socioeconomic status are required and propose the use of multidimensional, composite models which allow for capturing more context [89].
Conclusion
As a consequence of the COVID-19 pandemic, it is estimated that somewhere between 88 and 115 million people worldwide will be forced into extreme poverty, and issues of inequity have been exacerbated [37]. In the UK, this is happening on the background of a decade of stalling life expectancy, austerity and rising health inequalities between socioeconomic groups and regions [3]. Our comprehensive review shows that SED needs to be a key facilitator in identifying those who are likely to have a greater health burden and thus requiring specialist care at the end of life. Ultimately, future palliative care services cannot adopt a ‘one size fits all’ approach, shaped by our majority populations, rather they should be adaptable and flexible to provide different levels of support based on individualised need. Multidisciplinary and multi-agency approaches are needed to navigate healthcare and benefits systems and tackle the systemic issues associated with socioeconomic deprivation, which impact on EOL experience.
Availability of data and materials
All data analysed are included in published literature that were identified through the following bibliographic databases: Medline, Embase, CINAHL, ASSIA and PsychInfo. A list of included studies can be found in Table 3. For further information about the availability of these data, please contact the corresponding author.
Abbreviations
- SED:
-
Socio-economic deprivation
- EOL:
-
End of life
References
Mair FS, Jani BD. Emerging trends and future research on the role of socioeconomic status in chronic illness and multimorbidity. Lancet Public Health. 2020;5(3):e128–9.
Santos Salas A, Watanabe SM, Tarumi Y, Wildeman T, Hermosa García AM, Adewale B, et al. Social disparities and symptom burden in populations with advanced cancer: specialist palliative care providers’ perspectives. Support Care Cancer. 2019;27(12):4733–44.
Marmot M. Health equity in England: the Marmot review 10 years on. BMJ. 2020;368:m693.
Singh GK, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017;2017:2819372.
Hastert TA, Beresford SA, Sheppard L, White E. Disparities in cancer incidence and mortality by area-level socioeconomic status: a multilevel analysis. J Epidemiol Community Health. 2015;69(2):168–76.
Office for National Statistics. National Survey of Bereaved People (VOICES) 2015: quality of care delivered in the last 3 months of life for adults who died in England. 2016.
Davies JM, Sleeman KE, Leniz J, Wilson R, Higginson IJ, Verne J, et al. Socioeconomic position and use of healthcare in the last year of life: a systematic review and meta-analysis. PLoS Med. 2019;16(4):e1002782.
Asaria M, Doran T, Cookson R. The costs of inequality: whole-population modelling study of lifetime inpatient hospital costs in the English National Health Service by level of neighbourhood deprivation. J Epidemiol Community Health. 2016;70(10):990–6.
Macfarlane M, Carduff E. Does place of death vary by deprivation for patients known to specialist palliative care services? BMJ Support Palliat Care. 2018;8(4):428–30.
Buck J, Webb L, Moth L, Morgan L, Barclay S. Persistent inequalities in Hospice at Home provision. BMJ Support Palliat Care. 2020;10(3):e23.
Mason B, Kerssens JJ, Stoddart A, Murray SA, Moine S, Finucane AM, et al. Unscheduled and out-of-hours care for people in their last year of life: a retrospective cohort analysis of national datasets. BMJ Open. 2020;10(11):e041888.
Barratt H, Asaria M, Sheringham J, Stone P, Raine R, Cookson R. Dying in hospital: socioeconomic inequality trends in England. J Health Serv Res Policy. 2017;22(3):149–54.
Neergaard MA, Brunoe AH, Skorstengaard MH, Nielsen MK. What socio-economic factors determine place of death for people with life-limiting illness? A systematic review and appraisal of methodological rigour. Palliat Med. 2019;33(8):900–25.
Sleeman KE, Davies JM, Verne J, Gao W, Higginson IJ. The changing demographics of inpatient hospice death: population-based cross-sectional study in England, 1993–2012. Palliat Med. 2016;30(1):45–53.
Gao W, Ho YK, Verne J, Glickman M, Higginson IJ. Changing patterns in place of cancer death in England: a population-based study. PLoS Med. 2013;10(3):e1001410.
Koffman J, Burke G, Dias A, Raval B, Byrne J, Gonzales J, et al. Demographic factors and awareness of palliative care and related services. Palliat Med. 2007;21(2):145–53.
Dixon J, King D, Matosevic T, Clark C, Knapp K. Equity in the provision of palliative care in the UK: review of evidence. London: Personal Social Services Research Unit, London School of Economics and Political Science; 2015.
Davies JM, Maddocks M, Chua KC, Demakakos P, Sleeman KE, Murtagh FEM. Socioeconomic position and use of hospital-based care towards the end of life: a mediation analysis using the English Longitudinal Study of Ageing. Lancet Public health. 2021;6(3):e155–63.
Walsh B, Laudicella M. Disparities in cancer care and costs at the end of life: evidence from England’s National Health Service. Health Aff (Project Hope). 2017;36(7):1218–26.
Gold R, Hartung HP, Hohlfeld R, Wiendl H, Kieseier BC, Linker RA, et al. Therapy of multiple sclerosis with monoclonal antibodies: Results and recommendations of a symposium of the medical advisory board of the german MS society. Aktuelle Neurologie. 2009;36(7):334–44.
Turner V, Flemming K. Socioeconomic factors affecting access to preferred place of death: a qualitative evidence synthesis. Palliat Med. 2019;33(6):607–17.
Lewis JM, DiGiacomo M, Currow DC, Davidson PM. Dying in the margins: understanding palliative care and socioeconomic deprivation in the developed world. J Pain Symptom Manage. 2011;42(1):105–18.
Glasgow GEoLSGUo. Dying in the Margins. 2020. Available from: https://www.gla.ac.uk/research/az/endoflifestudies/projects/dyinginthemargins/.
Rowley J, Richards N, Carduff E, Gott M. The impact of poverty and deprivation at the end of life: a critical review. Palliat Care Soc Pract. 2021;15:26323524211033870.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Carduff E, Bowers S, Chin M, O'Riordan M. The experiences of people living with socio-economic deprivation who are approaching the end of life: an integrative review [updated October 201926/11/2021]. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019151906.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89.
National Institute for Health and Care Excellence. End of life care for adults: service delivery NICE guideline [NG142]. 2017. Available from: https://www.nice.org.uk/guidance/ng142. Accessed 17 Jan 2022.
Rietjens JA, Bramer WM, Geijteman EC, van der Heide A, Oldenmenger WH. Development and validation of search filters to find articles on palliative care in bibliographic databases. Palliat Med. 2019;33(4):470–4.
World Health Organisation. Palliative Care. 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/palliative-care.
Martin D, Brigham P, Roderick P, Barnett S, Diamond I. The (mis)Representation of Rural Deprivation. Environ Plan A. 2000;32(4):735–51.
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey SG. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12.
Galobardes B, Shaw M, Lawlor DA, Lynch JW. Indicators of socioeconomic position (part 2). J Epidemiol Community Health. 2006;60(2):95.
Nelson KE, Wright R, Peeler A, Brockie T, Davidson PM. Sociodemographic disparities in access to hospice and palliative care: an integrative review. Am J Hosp Palliat Care. 2021;38(11):1378–90.
Mondor L, Wodchis WP, Tanuseputro P. Persistent socioeconomic inequalities in location of death and receipt of palliative care: a population-based cohort study. Palliat Med. 2020;34(10):1393–401.
French M, Keegan T, Anestis E, Preston N. Exploring socioeconomic inequities in access to palliative and end-of-life care in the UK: a narrative synthesis. BMC Palliat Care. 2021;20(1):179.
World Bank. World Bank list of economies. 2020. Available from: https://databank.worldbank.org/data/download/site-content/CLASS.xls. Last accessed 21 Jan 2022.
Caldwell K, Henshaw L, Taylor G. Developing a framework for critiquing health research: an early evaluation. Nurse Educ Today. 2011;31(8):e1-7.
Bloomer MJ, Hutchinson AM, Brooks L, Botti M. Dying persons’ perspectives on, or experiences of, participating in research: an integrative review. Palliat Med. 2018;32(4):851–60.
Daugaard C, Neergaard MA, Vestergaard AHS, Nielsen MK, Johnsen SP. Socioeconomic inequality in drug reimbursement during end-of-life care: a nationwide study. J Epidemiol Community Health. 2019;73(5):435–42.
Ankuda CK, Kersting K, Guetterman TC, Haefner J, Fonger E, Paletta M, et al. What matters most? A mixed methods study of critical aspects of a home-based palliative program. Am J Hosp Palliat Care. 2018;35(2):236–43.
Azhar A, Yennurajalingam S, Ramu A, Zhang H, Haider A, Williams JL, et al. timing of referral and characteristics of uninsured, medicaid, and insured patients referred to the outpatient supportive care center at a comprehensive cancer center. J Pain Symptom Manage. 2018;55(3):973–8.
Brown CE, Engelberg RA, Sharma R, Downey L, Fausto JA, Sibley J, et al. Race/ethnicity, socioeconomic status, and healthcare intensity at the end of life. J Palliat Med. 2018;21(9):1308–16.
Cervantez SR, Tenner LL, Schmidt S, Aduba IO, Jones JT, Ali N, et al. Symptom burden and palliative referral disparities in an Ambulatory South Texas Cancer Center. Front Oncol. 2018;8:443.
Huang CY, Hung YT, Chang CM, Juang SY, Lee CC. The association between individual income and aggressive end-of-life treatment in older cancer decedents in Taiwan. PLoS ONE. 2015;10(1):e0116913. https://doi.org/10.1371/journal.pone.0116913.
Cai J, Guerriere DN, Zhao H, Coyte PC. Socioeconomic differences in and predictors of home-based palliative care health service use in Ontario, Canada. Int J Environ Res Public Health. 2017;14(7):802.
Koroukian SM, Schiltz NK, Warner DF, Given CW, Schluchter M, Owusu C, et al. Social determinants, multimorbidity, and patterns of end-of-life care in older adults dying from cancer. J Geriatr Oncol. 2017;8(2):117–24.
Krishnan P, Thompson G, McClement S. Predicting hospital transfers among nursing home residents in the last months of life. Int J Palliat Nurs. 2017;23(11):535–42.
Carlucci A, Vitacca M, Malovini A, Pierucci P, Guerrieri A, Barbano L, et al. End-of-life discussion, patient understanding and determinants of preferences in very severe COPD patients: a multicentric study. COPD. 2016;13(5):632–8.
Dhingra L, Dieckmann NF, Knotkova H, Chen J, Riggs A, Breuer B, et al. A high-touch model of community-based specialist palliative care: latent class analysis identifies distinct patient subgroups. J Pain Symptom Manage. 2016;52(2):178–86.
Karikari-Martin P, McCann JJ, Farran CJ, Hebert LE, Haffer SC, Phillips M. Race, any cancer, income, or cognitive function: what inf luences hospice or aggressive services use at the end of life among community-dwelling medicare beneficiaries? Am J Hosp Palliat Care. 2016;33(6):537–45.
Khosla N, Curl AL, Washington KT. Trends in engagement in advance care planning behaviors and the role of socioeconomic status. Am J Hosp Palliat Care. 2016;33(7):651–7.
Lee JJ, Long AC, Curtis JR, Engelberg RA. The influence of race/ethnicity and education on family ratings of the quality of dying in the ICU. J Pain Symptom Manage. 2016;51(1):9–16.
Schou-Andersen M, Ullersted MP, Jensen AB, Neergaard MA. Factors associated with preference for dying at home among terminally ill patients with cancer. Scand J Caring Sci. 2016;30(3):466–76.
Neergaard MA, Olesen F, Sondergaard J, Vedsted P, Jensen AB. Are cancer patients’ socioeconomic and cultural factors associated with contact to general practitioners in the last phase of life? Int J Family Med. 2015;2015:952314.
Tang ST, Lin KC, Chen JS, Chang WC, Hsieh CH, Chou WC. Threatened with death but growing: changes in and determinants of posttraumatic growth over the dying process for Taiwanese terminally ill cancer patients. Psychooncology. 2015;24(2):147–54.
Tucker-Seeley RD, Abel GA, Uno H, Prigerson H. Financial hardship and the intensity of medical care received near death. Psychooncology. 2015;24(5):572–8.
Bhatraju P, Friedenberg AS, Uppal A, Evans L. Factors associated with utilization of an inpatient palliative care consultation service in an urban public hospital. Am J Hosp Palliat Care. 2014;31(6):641–4.
Chang CM, Wu CC, Yin WY, Juang SY, Yu CH, Lee CC. Low socioeconomic status is associated with more aggressive end-of-life care for working-age terminal cancer patients. Oncologist. 2014;19(12):1241–8.
Lewis JM, DiGiacomo M, Currow DC, Davidson PM. Social capital in a lower socioeconomic palliative care population: a qualitative investigation of individual, community and civic networks and relations. BMC Palliat Care. 2014;13(1):30.
Tang ST, Liu TW, Chow JM, Chiu CF, Hsieh RK, Chen CH, et al. Associations between accurate prognostic understanding and end-of-life care preferences and its correlates among Taiwanese terminally ill cancer patients surveyed in 2011–2012. Psychooncology. 2014;23(7):780–7.
Chang YJ, Kwon YC, Lee WJ, Do YR, Seok LK, Kim HT, et al. Burdens, needs and satisfaction of terminal cancer patients and their caregivers. Asian Pac J Cancer Prev. 2013;14(1):209–16.
Masucci L, Guerriere DN, Zagorski B, Coyte PC. Predictors of health service use over the palliative care trajectory. J Palliat Med. 2013;16(5):524–30.
Sahin ZA, Tan M, Polat H. Hopelessness, depression and social support with end of life Turkish cancer patients. Asian Pac J Cancer Prev. 2013;14(5):2823–8.
Bergman J, Chi AC, Litwin MS. Quality of end-of-life care in low-income, uninsured men dying of prostate cancer. Cancer. 2010;116(9):2126–31.
Fergus C, Chinn D, Murray S. Assessing and improving out-of-hours palliative care in a deprived community: a rapid appraisal study. Palliat Med. 2010;24(5):493–500.
Maric DM, Jovanovic DM, Golubicic IV, Nagorni-Obradovic LJ, Stojsic JM, Pekmezovic TD. Psychological well-being in advanced NSCLC patients in Serbia: impact of sociodemographic and clinical factors. Neoplasma. 2010;57(1):1–7.
Chochinov HM, Hassard T, McClement S, Hack T, Kristjanson LJ, Harlos M, et al. The landscape of distress in the terminally ill. J Pain Symptom Manage. 2009;38(5):641–9.
Carr D. Is death “The Great Equalizer”? The social stratification of death quality in the United States. Ann Am Acad Pol Soc Sci. 2016;663(1):331–54.
Adler SR, Coulter YZ, Stone K, Glaser J, Duerr M, Enochty S. End-of-life concerns and experiences of living with advanced breast cancer among medically underserved women. J Pain Symptom Manage. 2019;58(6):959–67.
Bijnsdorp FM, Pasman HRW, Francke AL, Evans N, Peeters CF, van Groenou MIB. Who provides care in the last year of life? A description of care networks of community-dwelling older adults in the Netherlands. BMC Palliat Care. 2019;18(1):41.
Saphire ML, Prsic EH, Canavan ME, Wang SJ, Presley CJ, Davidoff AJ. Patterns of symptom management medication receipt at end-of-life among medicare beneficiaries with lung cancer. J Pain Symptom Manage. 2020;59(4):767-77.e1.
Yi D, Johnston BM, Ryan K, Daveson BA, Meier DE, Smith M, et al. Drivers of care costs and quality in the last 3 months of life among older people receiving palliative care: a multinational mortality follow-back survey across England, Ireland and the United States. Palliat Med. 2020;34(4):513–23.
Jacob J, Palat G, Verghese N, Chandran P, Rapelli V, Kumari S, et al. Health-related quality of life and its socio-economic and cultural predictors among advanced cancer patients: evidence from the APPROACH cross-sectional survey in Hyderabad-India. BMC Palliat Care. 2019;18(1):94.
Leng A, Jing J, Nicholas S, Wang J. Catastrophic health expenditure of cancer patients at the end-of-life: a retrospective observational study in China. BMC Palliat Care. 2019;18(1):43.
Saeed F, Hoerger M, Norton SA, Guancial E, Epstein RM, Duberstein PR. Preference for Palliative Care in Cancer Patients: Are Men and Women Alike? J Pain Symptom Manage. 2018;56(1):1-6.e1. https://doi.org/10.1016/j.jpainsymman.2018.03.014. Epub 2018 Mar 23. PMID: 29581034.
Stajduhar KI, Mollison A, Giesbrecht M, McNeil R, Pauly B, Reimer-Kirkham S, et al. “Just too busy living in the moment and surviving”: barriers to accessing health care for structurally vulnerable populations at end-of-life. BMC Palliat Care. 2019;18(1):1–14.
Wales J, Kalia S, Moineddin R, Husain A. The impact of socioeconomic status on place of death among patients receiving home palliative care in Toronto, Canada: a retrospective cohort study. J Palliat Care. 2020;35(3):167–73.
Aoun S, Bentley B, Funk L, Toye C, Grande G, Stajduhar KJ. A 10-year literature review of family caregiving for motor neurone disease: moving from caregiver burden studies to palliative care interventions. Palliat Med. 2013;27(5):437–46.
McFadden A, Siebelt L, Gavine A, Atkin K, Bell K, Innes N, et al. Gypsy, Roma and Traveller access to and engagement with health services: a systematic review. Eur J Pub Health. 2018;28(1):74–81.
Scotland PH. Proportionate Universalism Briefing. 2014.
Sadler E, McKevitt C. “Expert carers”: An emergent normative model of the caregiver. Soc Theory Health. 2012;11(1):40–58.
Gov.uk. Income-related benefits: estimates of take-up [updated 29/10/202026/11/2021]. Available from: https://www.gov.uk/government/collections/income-related-benefits-estimates-of-take-up--2.
Williams C. Chronic illness and informal carers: “Non-persons” in the health system, neither carers, workers or citizens. Health Sociol Rev. 2012;21(1):58–68.
Government S. Coronavirus (COVID-19): impact on equality (research). 2020.
Carmody P, McCan G, Colleran C, O’Halloran C. COVID-19 in the Global South: impacts and responses. 2020.
Organisation for Economic Co-operation and Development. A systemic resilience approach to dealing with Covid-19 and future shocks. Available from: https://www.oecd.org/coronavirus/policy-responses/a-systemic-resilience-approach-to-dealing-with-covid-19-and-future-shocks-36a5bdfb/ . Last accessed 21 Jan 2022.
Public Health Scotland. The Carstairs and Morris Index. Available from: https://www.isdscotland.org/Products-and-services/Gpd-support/Deprivation/Carstairs/ . Last accessed 17 Jan 2022.
Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56(4):769–84.
Acknowledgements
- Dr Anne Finucane for commenting on the protocol.
- Dr Melissa Bloomer advised us on use of the Caldwell criteria for assessing the quality of the articles included in this study.
- Shona MacNeilage at the NHS Greater Glasgow and Clyde library service helped develop the search strategies.
Funding
The roles of Emma Carduff and Maire O'Riordan are funded by Marie Curie. Emma Carduff is Co-Applicant on an Economic and Social Research Council grant (ES/S014373/1) entitled Dying in the Margins: uncovering the reasons for unequal access to home dying for the socio-economically deprived.
Author information
Authors and Affiliations
Contributions
EC, SB and MOR conceptualised the review. SB and EC conducted the literature searches. SB and MC conducted the screening of abstracts. All authors were involved in reviewing the final set of papers, analysing the data. All authors made major contributions to preparing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bowers, S.P., Chin, M., O’Riordan, M. et al. The end of life experiences of people living with socio-economic deprivation in the developed world: an integrative review. BMC Palliat Care 21, 193 (2022). https://doi.org/10.1186/s12904-022-01080-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-022-01080-6