Abstract
Objective
The benefits of palliative care for cancer patients were well developed; however, the characteristics of receiving palliative care and the utilization patterns among lung cancer patients have not been explored using a large-scale representative population-based sample.
Methods
The National Inpatient Sample of the United States was used to identify deceased metastatic lung cancer patients (n = 5,068, weighted n = 25,121) from 2010 to 2014. We examined the characteristics of receiving palliative care use and the association between palliative care and healthcare utilization, measured by discounted hospital charges and LOS (length of stay). The multivariate survey logistic regression model (to identify predictors for receipts of palliative care) and the survey linear regression model (to measure how palliative care is associated with healthcare utilization) were used.
Results
Among 25,121 patients, 50.1% had palliative care during the study period. Survey logistic results showed that patients with higher household income were more likely to receive palliative care than those in lower-income groups. In addition, during hospitalization, receiving palliative care was associated with11.2% lower LOS and 28.4% lower discounted total charges than the non-receiving group.
Conclusion
Clinical evidence demonstrates the benefits of palliative care as it is associated with efficient end-of-life healthcare utilization. Health policymakers must become aware of the characteristics of receiving the care and the importance of limited healthcare resource allocation as palliative care continues to grow in cancer treatment.
Similar content being viewed by others
Background
Lung cancer is one of the leading causes of cancer-related deaths worldwide. Approximately 1.7 million deaths occur annually, accounting for about 20% of all cancer-related deaths [1]. In 2018, estimated new cases of lung cancer were 234,030 (121,680 men and 112,350 for women) and accounting for 14% of new cancers in men and 13% of new cancers in women in the U.S [2]. Lung cancer is also associated with 154,050 deaths (83,550 for men/70,500 for women) in 2018, which accounted for 25% of all cancer fatalities in the U.S. [2].
Palliative care is medical care aimed at improving the quality of life of seriously ill cancer patients and their families through comprehensive assessment and treatment of the physical, psychosocial, and spiritual areas, including relief of pain and symptoms [3]. Previous research has investigated the benefit of palliative care on lung cancer patients and confirmed that palliative care improves patient and caregiver outcomes, and is also associated with less medical interventions near the end of life [4,5,6,7,8]. With that in mind, the American Association of Clinical Oncology suggested that palliative care should be considered for managing advanced cancer patients [9, 10]. Moreover, cancer patients' healthcare costs and utilization were markedly increased, creating a "U" shape at the first stage of diagnosis and end of life. Especially during the last months of life, hospital charges are known to increase rapidly, a trend confirmed by studies in USS Medicare patients [11,12,13] and lung cancer patients in Korea, where a single health insurance payer system is also utilized [14].
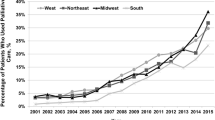
Palliative care is associated with decreased cost, and as the clinical and economic benefits of palliative care for metastatic cancer patients become evident, more patients are seeking the treatment [15, 16]. A study suggested that the share of palliative care use among all deaths varied by country: the United States (52.0%), the United Kingdom (46.6%), Canada (40.8%), Korea (24.3%), and Taiwan (39.0%) [17]. However, data lagged far behind, and lung cancer-specific results were not well documented. The rapid growth in the number of cancer patients highlights the importance of better understanding the characteristics of palliative care utilization. However, evidence on the use of palliative care with lung cancer has not been reviewed well [18], despite lung cancer being one of the cancer types with a poor prognosis, with meager 5-years survival rates. A recent study investigated the utilization of palliative care using Surveillance, Epidemiology, and End Results-Medicare linked database (2001–2013) and suggested that receipt of palliative care varied significantly by sex, race, and region [15]. Although this study sample is limited to older Medicare population (> 65 years old), it addressed important issues of palliative care 'recipients' characteristics among aged lung cancer patients. Since there is a lack of studies on the aspects of palliative care use by a population representative sample [19, 20] and its association with healthcare utilization among deceased metastatic lung cancer patients, it is crucial to examine the issue.
To address these research gaps, the aim of this study is two specific objectives: 1) to investigate the temporal trend of receiving palliative care and its association with patient characteristics, and 2) to examine how palliative care is associated with efficient healthcare utilization among end life of deceased metastatic lung cancer patients using a representative population sample.
Methods
Data collection
The 2010–2014 National Inpatient Sample (NIS) data, by Healthcare Cost and Utilization Project.
(HCUP) of Agency for Healthcare Research and Quality (AHRQ), were utilized to obtain patients with metastatic lung cancers. NIS is one of the largest publicly available dataset which include all-payer US hospital inpatients records. Among all 2010–2014 NIS samples (N = 37,312,324), as shown in Fig. 1, we first verified a primary diagnosis of lung cancer (total n = 156,180) using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for lung cancer. Then we obtained patients that were deceased (N = 13,620) and were at a metastatic stage (N = 5,068) (Fig. 1).
Variables
The main outcomes of this study was to investigate the characteristics of palliative care use by LOS (length of stay) and hospital charges. The main interesting variable was the receipt of palliative care consultation by year. To identify palliative care for hospitalized patients, this study used the ICD-9-CM code of V66.7. Total hospital charges was determined after reflecting for the annual inflation rate using Centers for Medicare and Medicaid Services estimates [21]. Due to the skewness of distribution for hospital charges and length of stay, we conducted the natural log of those variables.
In this study, we adjusted various patient-level confounders. Patient characteristics included age, race, annual median household income, primary payer (Private insurance, Medicare, Medicaid, Self-Pay/No Charge, and Others), number of comorbidities, the severity of illness, and whether the patient received surgery, radiation, or chemotherapy.
Statistical analysis
In this study, we used sampling weights for statistical analyses to represent deceased metastatic lung cancer patients. First, we examined the characteristics of the final dataset, which include patient characteristics by palliative care use. The patient characteristics were presented as mean or weighted frequency (percentage) with SD (standard deviation). Rao-Scott Chi-Square tests were employed to examine categorical variables for their group differences (whether receiving palliative care).
Using the survey logistic regression analysis, the odds ratios and 95% confidence interval (ORs and 95% CI) for receiving palliative care for deceased metastatic lung cancer patients were calculated. We also investigated how palliative care was associated with discounted hospital charges and length of stay using the multivariate survey linear regression analysis. This study used SAS statistical software (SAS Institute Inc., Cary, NC, USA, Version 9.4) for all statistical analyses. All methods were carried out in accordance with relevant guidelines and regulations in the method section.
Results
Patient characteristics
A total of 5,068 deceased metastatic lung cancer were identified in the 2010–2014 NIS data (weighted n = 25,121, Table 1). Among them, 2,544 (weighted n = 12,588, 50.1%) had palliative care. The general characteristics of patient characteristics are presented in Table 1. The mean LOS and discounted hospital charges were 7.05 days (SD = 7.37 days) and $53,514 (SD = $88,566) for those with palliative care and 8.94 days (SD = 9.15 days) and $81,213 (SD = $114,368) for those without palliative care (Table 1).
Patterns of palliative care use
Table 2 shows the temporal trends in palliative care use and healthcare utilization among hospitalized patients with metastatic lung cancer between 2010 and 2014. The rate of receiving palliative care consultations increased from 42.8% to 56.2% during the study period (p < 0.001). LOS and discounted total charges were not volatile during the study period.
The ORs of receiving palliative care from the survey logistic regression model are shown in Table 3. After controlling for all other variables, age, sex, and race 'didn't play important roles in receiving palliative care. However, the higher household income group was more likely to receive palliative care than the lower household income groups. (Reference group of 76th to 100th percentile, 0-25th percentile OR = 0.639 95% CI = 0.542–0.754, 26th to 50th percentile OR = 0.724 95% CI = 0.613–0.855, 51st to 75th percentile OR = 0.733 95% CI = 0.620–0.866). Additionally, palliative care was significantly less likely to be used in patients receiving surgery (OR = 0.519, 95% CI = 0.341–0.791) or chemotherapy (OR = 0.713, 95% CI = 0.563–0.903) during the same hospitalization.
Association of palliative care with discounted hospital charges and LOS
Table 4 shows the palliative care associations with discounted total hospital charges and LOS. After controlling for other variables, receiving palliative care during hospitalization was associated with statistically significant decreased LOS (β = -0.112, p < 0.001), which means 11.2% lower LOS than the not receiving group. Additionally, the use of palliative care was significantly associated with decreased hospital charges (β = -0.284, p < 0.001), which means 28.4% lower discounted total costs than the not receiving group after controlling for other variables.
Discussion
Through a large-scale national inpatient sample dataset, this study found an increase in palliative care services and a clear association between reduced healthcare utilization and deceased metastatic lung cancer patients who received palliative care. Furthermore, we observed different patient characteristics of those receiving palliative care in the study sample.
Our study results indicate that palliative care use grew during the study periods, which aligns with other studies investigating palliative care utilization among various chronic diseases. For instance, a study reported an increase of 0.45% to 2.56% between 2006 and 2012 among end-stage chronic obstructive pulmonary disease patients [22]. Another study using the National Inpatient Sample reported that chronic obstructive pulmonary disease patients receiving palliative care increased from 8.5% to 57.2% between 2005 and 2014 [23]. In studies using cancer patients, similar trends were also reported. In 'Dev's study, outpatient consultations tripled, and inpatient consultations increased 25 fold from 2000 to 2010 [24]. A recent study investigated palliative care use in metastatic non-small cell lung cancer patients using the Surveillance, Epidemiology, and End Results-Medicare linked database and reported that between 2001 to 2013, the temporal trend of palliative care use drastically increased from 3.6% to 31.9% in the study population [15]. Comparatively, our study revealed that almost 50% of lung cancer patients received palliative care. In the United States, the number of palliative care facilities has significantly grown with pediatric palliative programs and more than 1000 new palliative programs during the past decades [25, 26]. The escalation of cancer and other chronic disease incidences and an increase in life expectancy, promises that the need for palliative care services will continue to grow in the United States and worldwide.
Our study also found new insights on who receives palliative care and how it is associated with efficient healthcare spending and utilization. A recent study also reported that income was significantly associated with palliative care- especially in the top quartile compared to the bottom quartile using NIS data [27]. Economic factors may play an essential role in receiving palliative care, so more research should be conducted on this topic. Health policymakers must learn to promote access to the service which may reduce unnecessary interventions at 'patients' end of life. Other studies also suggested palliative care reduces healthcare cost for seriously ill lung cancer patients [15, 28,29,30]. However, the datasets of those studies were limited to certain population groups. One strength of our study was using NIS data which contains all age groups, races, and many other socio-economic statuses, representing a broader population; hence this study’s results may be generalized to all patients with lung cancer in the United States.
Although this study has several insights and strengths, there are some limitations worth noting. First, we used a national inpatient dataset which, depending on ICD-9-CM codes, may have a limited capture of palliative care. It is possible that terminal patients were coded with palliative care and were discharged to hospice, thus receiving less interventions. Second, the dataset does not have detailed clinical information such as stage or pharmacologic treatments. However, this study contained control variables, including APR-DRG, surgery, radiation, and chemotherapy, which may play a proxy role in 'patients' status. Third, the dataset of this study may not fully capture whether they are receiving care in an outpatient or inpatient setting and 'patients' or 'physicians' preferences toward palliative care. Further study should be conducted on how this may affect palliative care delivery and its association with spending and utilization. Finally, we were unable to capture the timing of palliative care delivery to patients due to a lack of information in the dataset. This could be another critical issue in seriously ill lung cancer patients. However, given that we conducted research with a well-sampled dataset with multiple study periods, we believe that the findings in our study are generalizable to most US deceased lung cancer patients and promote the benefits of palliative care.
Conclusion
Clinical evidence has demonstrated the benefits of palliative care. Palliative care is associated with efficient end-of-life healthcare utilization. Health policymakers should be aware of the characteristics of receiving the care and the importance of limited healthcare resource allocation as palliative care will continue to grow in cancer treatment.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2016;388:1459–544.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Clark D. From margins to centre: a review of the history of palliative care in cancer. Lancet Oncol. 2007;8(5):430–8.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2010;363:733–42.
Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, Moore M, Rydall A, Rodin G, Tannock I, Donner A, Lo C. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–30.
Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, Hull JG, Li Z, Tosteson TD, Byock IR, Ahles TA. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009;302(7):741–9.
Vanbutsele G, Pardon K, Van Belle S, Surmont V, De Laat M, Colman R, Eecloo K, Cocquyt V, Geboes K, Deliens L. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol. 2018;19(3):394–404.
Kavalieratos D, Corbelli J, Zhang D, Dionne-Odom JN, Ernecoff NC, Hanmer J, Hoydich ZP, Ikejiani DZ, Klein-Fedyshin M, Zimmermann C, Morton SC, Arnold RM, Heller L, Schenker Y. Association Between Palliative Care and Patient and Caregiver Outcomes: A Systematic Review and Meta-analysis. JAMA. 2016;316(20):2104–14.
Schnipper LE, Smith TJ, Raghavan D, Blayney DW, Ganz PA, Mulvey TM, Wollins DS. American Society of Clinical Oncology identifies five key opportunities to improve care and reduce costs: the top five list for oncology. J Clin Oncol. 2012;30(14):1715–24.
Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, Basch EM, Ferrell BR, Loscalzo M, Meier DE, Paice JA, Peppercorn JM, Somerfield M, Stovall E, Von Roenn JH. American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol. 2012;30(8):880–7.
Lubitz J, Prihoda R. The use and costs of Medicare services in the last 2 years of life. Health Care Financ Rev. 1984;5(3):117–31.
McCall N. Utilization and costs of Medicare services by beneficiaries in their last year of life. Med Care. 1984;22(4):329–42.
Lubitz JD, Riley GF. Trends in Medicare payments in the last year of life. N Engl J Med. 1993;328(15):1092–6.
Kim SJ, Han KT, Park EC, Park S, Kim TH. Copayment policy effects on healthcare spending and utilization by Korean lung cancer patients at end of life: a retrospective cohort design 2003–2012. Asian Pac J Cancer Prev. 2014;15(13):5265–70.
Huo J, Hong YR, Turner K, Bian J, Grewal R, Wilkie DJ. Utilization pattern and service settings of palliative care for patients with metastatic non-small cell lung cancer. Cancer. 2019;125(24):4481–9.
Yadav S, Heller IW, Schaefer N, Salloum RG, Kittelson SM, Wilkie DJ, Huo J. The health care cost of palliative care for cancer patients: a systematic review. Support Care Cancer. 2020;28(10):4561–73.
National Cancer Center of Korea. Statistics of hospice and palliative services by National Hospice Center. https://hospice.go.kr:8444/?menuno=53. Accessed 07 Sept 2021.
Parajuli J, Tark A, Jao YL, Hupcey J. Barriers to palliative and hospice care utilization in older adults with cancer: A systematic review. J Geriatr Oncol. 2020;11(1):8–16.
Morrison RS, Maroney-Galin C, Kralovec PD, Meier DE. The growth of palliative care programs in United States hospitals. J Palliat Med. 2005;8(6):1127–34.
Dumanovsky T, Augustin R, Rogers M, Lettang K, Meier DE, Morrison RS. The Growth of Palliative Care in USS Hospitals: A Status Report. J Palliat Med. 2016;19(1):8–15.
Mark TL, Levit KR, Vandivort-Warren R, Coffey RM, Buck JA. SAMHSA spending estimates team. Trends in spending for substance abuse treatment, 1986–2003. Health Aff (Millwood). 2007;26(4):1118–28.
Rush B, Hertz P, Bond A, McDermid RC, Celi LA. Use of Palliative Care in Patients With End-Stage COPD and Receiving Home Oxygen: National Trends and Barriers to Care in the United States. Chest. 2017;151(1):41–6.
Kim SJ, Shen J, Ko E, Kim P, Lee YJ, Lee JH, Liu X, Ukken J, Kioka M, Yoo JW. Life-sustaining procedures, palliative care, and cost trends in dying copd patients in USS Hospitals: 2005–2014. Korean J Hospice Palliat Care. 2018;21(1):23–32.
Dev R, Del Fabbro E, Miles M, Vala A, Hui D, Bruera E. Growth of an academic palliative medicine program: patient encounters and clinical burden. J Pain Symptom Manage. 2013;45(2):261–71.
Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S, Weissman D. Pediatric palliative care programs in children’s hospitals: a cross-sectional national survey. Pediatrics. 2013;132(6):1063–70.
Hughes MT, Smith TJ. The growth of palliative care in the United States. Annu Rev Public Health. 2014;35:459–75.
Sokol LL, Bega D, Yeh C, Kluger BM, Lum HD. Disparities in Palliative Care Utilization Among Hospitalized People With Huntington Disease: A National Cross-Sectional Study. Am J Hosp Palliat Care. 2021:10499091211034419. https://doi.org/10.1177/10499091211034419. Epub ahead of print.
Sheridan PE, LeBrett WG, Triplett DP, Roeland EJ, Bruggeman AR, Yeung HN, Murphy JD. Cost Savings Associated With Palliative Care Among Older Adults With Advanced Cancer. Am J Hosp Palliat Care. 2021;38(10):1250–7.
Mor V, Wagner TH, Levy C, Ersek M, Miller SC, Gidwani-Marszowski R, Joyce N, Faricy-Anderson K, Corneau EA, Lorenz K, Kinosian B, Shreve S. Association of Expanded VA Hospice Care With Aggressive Care and Cost for Veterans With Advanced Lung Cancer. JAMA Oncol. 2019;5(6):810–6.
Triplett DP, LeBrett WG, Bryant AK, Bruggeman AR, Matsuno RK, Hwang L, Boero IJ, Roeland EJ, Yeung HN, Murphy JD. Effect of Palliative Care on Aggressiveness of End-of-Life Care Among Patients With Advanced Cancer. J Oncol Pract. 2017;13(9):e760–9.
Acknowledgements
Not applicable.
Funding
This paper was supported by 2021 Sabbatical Year of Soonchunhyang University and BK21 FOUR(Fostering Outstanding Universities for Research, No.:5199990914048, Korean Ministry of Education).
Author information
Authors and Affiliations
Contributions
JWC, KTH and SJK led the design and conception of the study, performed the data analysis, and wrote the manuscript. MM contributed to the discussion, reviewed and edited the manuscript. The authors read and approved the final manuscript. SJK is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data we use was secondary data and all patient data were encrypted and unable to identify. This study was approved for waiver from the Institutional Review Board of Soonchunhyang University (202109-SB-083).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests or conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chang, J., Han, KT., Medina, M. et al. Palliative care and healthcare utilization among deceased metastatic lung cancer patients in U.S. hospitals. BMC Palliat Care 21, 136 (2022). https://doi.org/10.1186/s12904-022-01026-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-022-01026-y