Abstract
Background
Compassionate communities are rooted in a health promotion approach to palliative care, aiming to support solidarity among community members at the end of life. Hundreds of compassionate communities have been developed internationally in recent years. However, it remains unknown how their implementation on the ground aligns with core strategies of health promotion. The aim of this review is to describe the practical implementation and evaluation of compassionate communities.
Methods
We undertook a scoping review of the empirical peer-reviewed literature on compassionate communities. Bibliographic searches in five databases were developed with information specialists. We included studies in English describing health promotion activities applied to end-of-life and palliative care. Qualitative analysis used inductive and deductive strategies based on existing frameworks for categorization of health promotion activities, barriers and facilitators for implementation and evaluation measures. A participatory research approach with community partners was used to design the review and interpret its findings.
Results
Sixty-three articles were included for analysis. 74.6% were published after 2011. Health services organizations and providers are most often engaged as compassionate community leaders, with community members mainly engaged as target users. Adaptation to local culture and social context is the most frequently reported barrier for implementation, with support and external factors mostly reported as facilitators. Early stages of compassionate community development are rarely reported in the literature (stakeholder mobilization, needs assessment, priority-setting). Health promotion strategies tend to focus on the development of personal skills, mainly through the use of education and awareness programs. Few activities focused on strengthening community action and building healthy public policies. Evaluation was reported in 30% of articles, 88% of evaluation being analyzed at the individual level, as opposed to community processes and outcomes.
Conclusions
The empirical literature on compassionate communities demonstrates a wide variety of health promotion practices. Much international experience has been developed in education and awareness programs on death and dying. Health promotion strategies based on community strengthening and policies need to be consolidated. Future research should pay attention to community-led initiatives and evaluations that may not be currently reported in the peer-review literature.
Similar content being viewed by others
Background
The concept of compassionate community is rooted in a health promotion approach to palliative care [1, 2]. Historically, the vision of compassionate communities has been anchored in the work of the World Health Organization’s Ottawa Charter [3] and Healthy City movement [4, 5]. The Ottawa Charter describes five major pillars of health promotion: 1- Develop personal skills, 2- Create supportive environment, 3- Reorient health services, 4- Strengthen community actions, 5- Build healthy public policy. Kellehear adapted these core health promotion strategies to palliative care, proposing that “the goals of health-promoting palliative care are to provide education, information and policy-making for health, dying and death.” ([5] p. 26).
Compassionate communities address a holistic definition of health that goes beyond the simple treatment of symptoms to include psychological, spiritual and social well-being. It emphasizes the strengthening of social capital, mutual aid relationships and the ability of citizens to actively participate in the development of their communities, to create social connections and care for each other [6]. As an intersectoral approach, compassionate communities mobilize a variety of civic actors outside the professional health care system (e.g., education, municipalities, community organizations, spiritual groups), as well as patients, family members, neighbors and citizens. As a model, it encourages partnership building to support community capacity-building and resilience in issues surrounding dying, death and bereavement, often with a focus on health inequalities, diversity and social inclusion.
Health promotion approaches have received considerable attention within and beyond palliative care. In recent decades, hundreds of compassionate communities have been established around the world [7]. This demonstrates an international willingness towards community-led models of social and practical support for people living with advanced illness and their caregivers ([8] p.1). However, it remains unknown how the implementation of compassionate communities on the ground aligns with core principles for health promoting palliative care.
The aim of this review is to describe the practical implementation of compassionate communities, analyze which stakeholders are engaged in their development, what core health promotion strategies are used, and how compassionate communities are evaluated.
Review questions
The goal of this review was to understand how compassionate communities have been implemented and evaluated in practice. More specifically, we sought to describe:
-
1.
Which stakeholders are engaged in compassionate community development?
-
2.
What barriers and facilitators have been identified?
-
3.
Which health promotion activities have been implemented in practice?
-
4.
How have compassionate communities been evaluated?
Methods
Given the diversity of the literature on compassionate communities, we adopted a scoping review design as a preliminary evaluation of available research literature [9]. As described by the Joanna Briggs Institute [10], scoping reviews are best suited “to answer questions regarding the nature and diversity of the evidence/knowledge available” (p. 409). Our review process was composed of 5 steps: 1- identification of potential studies; 2- sorting references and selecting studies; 3- data extraction; 4- analysis and synthesis; and 5- collating, summarizing, and reporting the results to inform practice and future research. The review protocol is available from the authors upon request. Reporting of the scoping review methods and results followed PRISMA-ScR reporting guidelines (Additional file 5) [11].
Search strategy
We designed, piloted and implemented our bibliographic search strategies with the help of information specialists. The search strategy was limited to English language articles published but without restrictions regarding the year of publication. Initial search terms were built around the following concepts: (end-of-life, dying, palliative care) AND (compassionate communities, compassionate cities OR health promotion). A pilot search was undertaken on Ovid MEDLINE and EBSCOhost-CINAHL to refine the search strategy, using previously identified articles meeting our inclusion criteria. Text words and index terms were adapted, based on this preliminary search. A final, more detailed search was conducted in August 2019 in EBSCOhost-CINAHL, EMBASE, Ovid MEDLINE, Ovid PsychInfo, Web of Science. The final search strategy, and its adaptation for specific electronic databases is described in Additional file 1: “ Search Strategy. Research results were saved using the bibliographic management software EndNote.
Inclusion and exclusion criteria
To be included, published articles needed to: 1- be an empirical article; 2- describe health promotion activities, as defined by the World Health Organization Ottawa Charter for Health Promotion [3]; 3- be applied to end-of-life or palliative care, including care of bereaved people.
Abstract-only publications (i.e., no full-text article available), grey literature, books and doctoral theses were excluded. Only empirical studies and articles in journals were included, conceptual or theoretical papers, advocacy, opinion articles and secondary literature were excluded. Published systematic reviews were not analyzed directly but were used to identify further primary studies and articles meeting our inclusion criteria. Three research assistants applied the inclusion and exclusion criteria of identified abstracts and articles, without automatic computer screening assistance. Disagreements were resolved through discussion, or in consultation with the two study principal investigators.
Analysis and presentation of results
All included papers were imported into QSR International’s NVivo 12 software for data extraction and analysis. Included articles were imported directly into NVivo for data extraction and qualitative thematic analysis. Analysis proceeded in two stages. In Stage 1, we used an inductive approach to categorize the stakeholders involved, barriers/facilitators, and activities evaluation approaches (study design, and evaluation measures). In Stage 2, we used a deductive approach to organize the presentation of results, according to existing frameworks and models for barriers and facilitators [12], health promotion activities (Ottawa Charter), and categories of evaluation measures [13]. To analyze how compassionate communities were evaluated, we only analyzed articles that reported both their evaluation methods and results within the article (i.e., we excluded from this analysis articles reporting “evaluation results” without mentioning how these evaluations were conducted). We classified study design based on Hartling’s [14] design classification tool.
Community engagement in research
To increase the pragmatic value and relevance of the review, community members and practitioners were engaged in the design of the scoping review protocol, interpretation of findings, and co-authorship of the manuscript. Following a collaborative participatory research approach [15], community members and practitioners (patient partner, community developer, healthcare professional and palliative care manager) were integrated in the scoping review steering committee, which oversaw the design (questions and scope) of the review, participated in a two-hour data interpretation workshop to analyze implications of findings for practice, and contributed as co-authors on the manuscript to increase relevance for practitioners.
Results
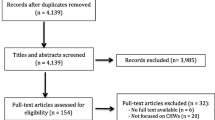
Figure 1 provides a PRISMA flow chart diagram of included studies [16]. A total of 5486 individual records were screened for eligibility and a final set of sixty-three studies (n = 63) were included for analysis. Of the 63 articles included in the scoping review, all (100%) included information on stakeholder engagement as well as barriers and facilitators for implementation. Of the included papers, 39 (62%) provided information about the type of health promotion activities implemented, and 19 (30%) provided information about evaluation methods and results.
Description of included studies
Table 1 provides a summary description of included studies (n = 63). Most included articles were published after 2011 (74.6%). The majority of studies were conducted in the United States (USA) (30.6%), Australia (28.6%), and the United Kingdom (UK) (15.9%) and with a minority of articles (4.8%) from developing countries (Malaysia, India and Uganda). The detail of all 63 included articles is provided in Additional file 2: Description of included articles.
Which stakeholders are engaged in compassionate community development?
The included literature reports on a variety of stakeholders engaged in compassionate communities’ development. Table 2 classifies these stakeholders by individual and organizational categories. Health and social care providers (55.5%) and health services (44.4%) are most often engaged as compassionate community stakeholders and leaders. Community members were engaged in 47.6% of articles, most often as target population and participants (42.8%), in contrast to being the leaders and co-leaders (20.6%) of compassionate community initiatives. Most of the published programs target the general population (people at the end of life, caregivers and bereaved people), with a minority of included articles specifically reporting on programs designed with and for marginalized populations (eg. ethnic minorities).
Barriers and facilitators for compassionate community implementation
Of the included studies, 13 categories of factors were identified as barriers and facilitators for compassionate community implementation [12] (Table 3). Adaptation to local culture, social attitudes and local context was the most frequently reported barrier for implementation (31.7% of articles), including: social attitudes toward asking for and receiving help at the end of life, alignment of proposed activities with cultural norms and attitudes, and sensitivities to language, religious attitudes and reaching out toward ethnic minorities. Information, open discussions and awareness about the end of life was the most frequently reported facilitator for implementation of compassionate communities (26.0% of articles). Access to informal and political support were also highlighted as key facilitators, along with practical support for traveling, duration of activities, location and convenient scheduling of activities (22.2% of articles for both categories). Styles of leadership facilitating community partnership and empowerment were also highlighted as facilitators. While the availability or lack of human and financial resources may either be reported as a facilitator (20.6%) or barrier (14.3%), existing policies and organizational structures were essentially reported as a barrier for implementation of compassionate communities (15.9% listing it as a barrier, while no article described the role of supporting policies as facilitating implementation).
Which activities have been implemented in practice?
Figure 2 organizes activities according to compassionate community development stages. Needs assessments: includes activities related to exploring existing interventions, assessing community capacity and identifying needs. These activities include focus groups, interviews, literature review, consultations, etc. Needs assessments activities represented only 9.4% of compassionate community development activities reported in the included literature. Stakeholders’ engagement & mobilization: includes activities related to solicitation, recruitment and training of stakeholders involved in the implementation of the design and implementation of compassionate communities. These represented 13.1% of all reported activities. Priority setting: includes activities related to planning activities and agenda setting, framing of the problem and target population, and prioritization of activities and resources. This phase represented only 6.1% of the overall identified activities reported in the literature, which is the less represented category.
Implementation: this stage includes a description of compassionate communities’ activities implemented in practice. Description of implemented activities represented the most commonly reported stage of development for compassionate communities (64.3% of reported activities), as opposed to upstream development stages (needs assessment, priority setting and stakeholder engagement) and evaluation.
Implemented activities were further categorized inductively (Fig. 2). In order of frequency, these activities included: education and awareness programs (46.2%); direct help, support, and care (27.7%); resources mobilization and linkages (10.8%); build partnerships and collaborations (7.7%); policy development and lobbying (7.7%). Table 4 offers specific examples for these activities. A complete list of activities described in the included article is provided in Additional file 3 “List of activities”.
Figure 3 offers a complementary perspective on activities implemented by compassionate communities, categorized according to the five Ottawa Charter action strategies for health promotion. The most frequent action strategy was aimed at developing personal skills of community members (30%), while two pillars of health promotion were less frequently targeted: building health policy (11.3%) and strengthening of community actions (10.8%).
How have compassionate communities been evaluated?
Evaluation constituted 6.6% of compassionate communities’ activities. The goals of evaluation reported in the articles include: 1- research (for example: verification of achievements [17], 2- quality improvement (example: evaluation of practice innovations with key stakeholders [18]) and 3- certification (as a compassionate community, institution or city [17]). Figure 4 illustrates what is being measured by compassionate community evaluations. Documentation of process indicators related to activities and programs was most frequently evaluated (25.9%), followed by participants’ attitudes, opinions and preferences (20.7%). Needs, policies and culture were least often included as part of compassionate communities’ evaluations (9.5%). Additional file 4 includes a detailed description of evaluation approaches (what is measured, how and at which levels) for each article reporting evaluation methods and results.
As health promotion strategies targeting change at the level of communities and populations, compassionate communities processes and outcomes can be collected and analyzed at different levels [13, 19]. Figure 5 classifies compassionate community evaluation measures reported in the included literature. Measurement and analysis at the individual patient, family and caregiver level was most common (79% of articles), followed by meso-level measures of changes in healthcare services (26%) and communities (21%). Macro-level changes were evaluated in only one population study (5%).
Based on Hartling’s [14] study design classification tool (Fig. 6), we note that a majority of articles (57.9%) used non-comparative study methods, a few (26.3%) used a before-after study design and one (5.3%) used a controlled before-after study design. Two published protocols of ongoing studies have used controlled trial designs.
Discussion
This review provides a comprehensive mapping of how compassionate communities have been implemented and evaluated in practice, as reported in the international peer-review literature. A striking finding of this empirical overview is that the umbrella concept of “compassionate communities” encompasses a wide diversity of health promotion practices in the context of palliative and end-of-life and palliative care.
All of the 5 core health promotion strategies described in the Ottawa Charter have been reported in compassionate community initiatives around the world. However, not all strategies are equally represented in practice. Developing personal skills through education and awareness programs represents the majority of reported activities. This finding is consistent with the observation that patients, families and community members are most often engaged as the target audience of compassionate community initiatives, rather than as full partners of community-led programs. Despite the emphasis of ecological approaches to community development highlighted in theoretical models [2, 4, 6], strengthening community action and building healthy public policy are the least common health promotion strategies observed in this review.
Kellehear ([5] p.35) underscores the tendency for health-promoting palliative care to favor direct-services approaches, which aligns with the findings of this review. The fact that most of the reported initiatives are led by healthcare organizations and providers, who may be more accustomed to playing an educator rather than a community facilitator role, may partly explain this dominance of education activities. Alternatively, it is possible that individual education programs serve as a stepping stone for healthcare organizations to initiate collaborations with community groups, or as a pre-condition to put death and dying on the policy agenda. Understanding why and how compassionate community initiatives can move from individual education to community action would be an important area for future development.
Finally, it may also be the case that the neighborhood/local community emphases of the compassionate community movement has led to a more necessary prioritizing of personal skills and creating supportive environments because these seem more relevant to local efforts. The compassionate cities movement, whose emphasis has been similarly ecological in approach, has tended to focus on inter-sectoral co-operation, civic events, policies, and actions across large geographical and cross-institutional terrain (compassionate cities) [5]. While compassionate cities were included in our search strategy, there are far fewer compassionate cities than compassionate communities worldwide and most of them do not have published evaluation. For example, the Public Health Palliative Care International Association website currently lists only 10 cities aspiring to use health-promoting palliative care principles in its city-wide operations (https://phpci.info/cities). Most of these cities employ, or are guided by, the Compassionate City Charter and this charter has an explicit policy-building agenda [20]. Perhaps in the future when these social experiments are more widely published, viewed comparatively with the more local compassionate communities studies, the balance between policy-building emphasis and the development of individual skills and knowledge may be better assessed.
A number of barriers and facilitators have been reported in the literature to guide compassionate community development and implementation. The published literature is also rich in examples of how to overcome common barriers, such as building awareness, adapting compassionate communities to diverse cultural settings, and building balanced and sustainable partnerships with community organizations. An apparent dissonance in findings is the emphasis on adaptation to local culture and social attitude (reported as the most common barrier to implementation) and the relative lack of compassionate community initiatives specifically targeting marginalized populations. Furthermore, the published literature places a heavy emphasis on the implementation and result stages, as opposed to the early phases of compassionate community development (stakeholder mobilization, needs assessment and priority-setting). This observation reflects a broader trend in the literature, which tends to view community development as a process of implementing pre-packaged interventions in the community, rather than a process of social empowerment driven and designed with the community [21]. Findings from the review points to a certain leadership style favoring the development of compassionate communities, where individuals and organizations share leadership and ownership of projects.
A minority of articles evaluated compassionate community initiatives, despite our restriction to peer-review publications. Research designs were largely non-comparative. When they are conducted, the vast majority of evaluations assess change at the individual level, as opposed to community and population change. This gap in evaluation is significant, given the role that evaluation can play in the development, improvement and sustainability of compassionate communities. The individual-level evaluation focus is congruent with pressures on community-based programs to demonstrate impact on individual health outcomes [22], difficulties in operationalizing ecological evaluation models [13], and the need for flexible approaches to evaluation that allows definition of compassionate communities’ goals by community members themselves [23, 24].
Strengths, limitations and future research
This scoping review has provided a comprehensive overview of compassionate community initiatives in four important ways: 1- by describing the current pattern of participation, leadership, and practice emphasized in compassionate community programs in English-speaking countries; 2- by charting the growing profile, strength, and resulting influence of the compassionate communities movement in the health sciences literature in general, palliative the end-of-life care literature specifically; 3- by providing a state of the art understanding of the current challenges, barriers, and problems encountered in the implementation and research evaluation of these health promotion projects, and; 4- by providing a clearer academic assessment of the limitations of current research communications about this topic.
Because this has been a review of the English language peer-review literature, it is limited by its exclusion of non-English language publications. It has also been limited by excluding books, book chapters, grey literature reports, and unpublished compassionate community initiatives. These restrictions have three important implications for limiting our generalizations.
First, the culture-specific academic strategy of privileging journal literature in the biomedical and health sciences marginalizes the work of community activists, social sciences, and social care academics and workers who often employ other types of outputs, including books, to communicate their work. For example, Wegleitner, Heimerl and Kellehear (2016) document 10 empirical case studies of how different national examples of compassionate communities were implemented, but these cases appear in an edited book [25].
Secondly, many compassionate communities have been established in non-English-speaking countries and their evaluations are poorly represented in the English language literature, especially those from Europe, South America, South-East Asia, East Asia, and Africa. The existing English-language conceptual literature, especially those emerging from Taiwanese, Spanish, German, or Dutch writers for example, indicates major civic and academic activity around compassionate communities work, but this is largely inaccessible to English language-reviews. Furthermore, there are translation challenges even in English-language contexts. For example, in many German-speaking countries, compassionate communities are known as ‘caring communities’ [25, 26]. In Spanish-speaking contexts, where the term ‘compassion’ can have religious connotations or can have a closer and less desirable association with the word ‘pity’, the alternative phrases of ‘togetherness’ or ‘everybody’ in community has commonly been used. This means that even when translated into English, such community development examples would not necessarily be selected by the usual search terms employing community initiatives linked to the word ‘compassion’.
Thirdly, given the importance of developing countries and other areas of the world in the compassionate community movement, restriction to the peer-review literature could overemphasize the relative importance of professionally-led and academically-funded compassionate community initiatives, as opposed to grassroot community-led initiatives that may not have the resources (or priorities) to report their findings in the academic literature.
Finally, scoping reviews aim at mapping the existing literature rather than providing a synthesis of evidence about the effectiveness of specific interventions [10]. While our findings are useful to describe the range of available strategies used to develop, implement and evaluate compassionate communities, it cannot provides simple answers as to “what works best”.
Future research should seek to document emerging community-led initiatives being conducted outside of professional and academic settings, which may not be self-labeled as “compassionate communities” but nonetheless fall within the principles of health promoting palliative care. Future reviews should expand on geographical scope, language and cultural settings in which compassionate communities have been implemented. Early stages of compassionate community development, including engagement of community members in leadership and priority-setting stages, requires more research attention, as does the condition for adaptation to local culture, partnerships with marginalized communities and issues of sustainability.
Further research on the implementation and evaluation of compassionate communities might also include (even comparatively) the dementia-friendly communities’ movement [27]. Dementia-friendly communities—in terms of conceptual design and practice vision – are closely aligned with health promotion and civic program developments in end-of-life care. However, diagnosis-specific their origins have been compared to compassionate community programs, those programs remain part of the recent emergence, and merging, of ‘new’ public health ideas into health service management programs at the end-of-life.
Finally, it might also be useful to investigate and describe an additional and complementary scoping review that surveyed only the book, conference, or grey literature for their descriptions of implementation and evaluation of compassionate communities. This would provide a more interdisciplinary, non-health services research approach to this emerging field, and therefore a more complete portrayal. This would enlarge and deepen our understanding of an important end-of-life care initiative that has been embraced by the health and social care sectors, but also the broader civic society that is increasingly being asked to partner and support both.
Implications for practice and policy
This review has important and useful implications for practice and policy. First, it lists a broad list of published examples of compassionate communities, using a variety of practical approaches and health promotion strategies. This is helpful to provide “grounding” and anchoring of the complex concepts of health promotion palliative and its translation into concrete examples and activities. The categorization of activities undertaken as part of compassionate communities’ implementation is an added value of this review, and could help practitioners reflect on a menu of possible strategies and ideas that may be adapted to their specific context. Identifying the main barriers and facilitators encountered on the ground may also help community members prospectively reflect on strategies to minimize them. Our findings also support the “slow growth” of compassionate community initiatives, highlighting the early stages of community mobilization, needs assessment and prioritization. The current global pandemic, with its heavy toll on grief, bereavement and social isolation, have further highlighted the importance and need for supportive networks among community members [28].
Conclusion
The empirical literature on compassionate communities demonstrates a wide variety of health promotion practices across the world. Much international experience has been developed in education and awareness programs on death and dying. Health promotion strategies based on community strengthening and policies need to consolidated. Future research should pay attention to community-led initiatives and outcomes that may not be currently reported in the peer-review literature.
Availability of data and materials
Original data is available upon request from the authors.
References
Sallnow L, Paul S. Understanding community engagement in end-of-life care: developing conceptual clarity. Crit Public Health. 2015;25(2):231–8.
Abel J. Compassionate communities and end-of-life care. Clin Med. 2018;18(1):6–8.
Organization WH. Ottawa charter for health promotion health promotion international. 1986;1. https://www.who.int/teams/health-promotion/enhanced-wellbeing/first-global-conference.
Kenzer M. Healthy cities: a guide to the literature. Public Health Rep. 2000;115(2–3):279.
Kellehear A. Compassionate cities. London: Public health and end-of-life care; 2005.
Kellehear A. Compassionate communities: end-of-life care as everyone’s responsibility. QJM. 2013;106(12):1071–5.
Librada-Flores S, Nabal-Vicuña M, Forero-Vega D, Muñoz-Mayorga I, Guerra-Martín MD. Implementation models of compassionate communities and compassionate cities at the end of life: a systematic review. Int J Environ Res Public Health. 2020;17(17):6271.
Aoun SM, Abel J, Rumbold B, Cross K, Moore J, Skeers P, et al. The compassionate communities connectors model for end-of-life care: a community and health service partnership in Western Australia. Palliative Care and Social Practice. 2020;14:2632352420935130.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108.
Institute JB. The Joanna Briggs institute reviewers’ manual 2020: methodology for JBI scoping reviews [Internet]. South Australia: The Joanna Briggs Institute; 2020.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Légaré F, Ratté S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73(3):526–35.
Pfaff KA, Dolovich L, Howard M, Sattler D, Zwarenstein M, Marshall D. Unpacking “the cloud”: a framework for implementing public health approaches to palliative care. Health Promot Int. 2019;27:27.
Hartling L, Bond K, Santaguida PL, Viswanathan M, Dryden DM. Testing a tool for the classification of study designs in systematic reviews of interventions and exposures showed moderate reliability and low accuracy. J Clin Epidemiol. 2011;64(8):861–71.
Masters J. The history of action research. first published. 1995.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P, Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS med. 2009;6(7).
Librada Flores S, Herrera Molina E, Boceta Osuna J, Mota Vargas R, Nabal VM. All with You: a new method for developing compassionate communities-experiences in Spain and Latin-America. Annals of Palliative Medicine. 2018;7(Suppl 2):S15–31.
Paul S. Working with communities to develop resilience in end of life and bereavement care: hospices, schools and health promoting palliative care. J Soc Work Pract. 2016;30(2):187–201.
Robert É, Ridde V. L’approche réaliste pour l’évaluation de programmes et la revue systématique: de la théorie à la pratique. Mesure et évaluation en éducation. 2013;36(3):79–108.
Kellehear A. The Compassionate City Charter : Inviting the cutlural and social sectors into end of life care. In: Wegleitner KH, A. Kellegear editor. Compassionate Cities: Case studies from Britain and Europe: Abingdon, Routledge; 2016. p. 76–87. https://www.routledge.com/Compassionate-Communities-Case-Studies-from-Britain-and-Europe/Wegleitner-Heimerl-Kellehear/p/book/9781138552036.
Rifkin SB. Paradigms lost: toward a new understanding of community participation in health programmes. Acta Trop. 1996;61(2):79–92.
Sallnow L, Richardson H, Murray SA, Kellehear A. The impact of a new public health approach to end-of-life care: a systematic review. Palliat Med. 2016;30(3):200–11.
Rifkin SB. Examining the links between community participation and health outcomes: a review of the literature. Health policy and planning. Health policy and planning. 2014;29(suppl_2):ii98–106.
South J, Phillips G. Evaluating community engagement as part of the public health system. J Epidemiol Community Health. 2014;68(7):692–6.
Wegleitner K, Heimerl A, Kellegear A. Compassionate Cities : Case studies from Britain and Europe: Abingdon, Routledge. 2016.
Tronto J. Caring democracy, markets, equality and justice. New York: New York University Press; 2013.
Buckner S, Darlington N, Woodward M, Buswell M, Mathie E, Arthur A, et al. Dementia friendly communities in England: a scoping study. Int J Geriatr Psychiatry. 2019;34(8):1235–43.
Abel J, Taubert M. Coronavirus pandemic: compassionate communities and information technology. BMJ Support Palliat Care. 2020;10(4):369–71.
Acknowledgements
Funding for this study was provided by the J.-Louis Lévesque Foundation. Pierre Pluye (McGill University), Nathalie Rheault and Hervé Zomahoun (Unité Soutien SRAP-Québec) contributed to the search strategy and scoping review design. Agustina Gancia (Center of Excellence on Partnership with Patients and the Public) drafted the study protocol. Genevieve Castonguay (Canada Research Chair in Partnership with Patients and Communities/Unité Soutien SRAP-Québec) provided methodological support through the data collection, analysis and synthesis stages.
Funding
This study was funded by the J.-Louis Lévesque Foundation. The funder had no role in the study design, data collection, analysis, interpretation nor publication decisions.
Author information
Authors and Affiliations
Contributions
AB, IM, EW, KD, RC, SD, GR, and AK contributed to the study design. EW, FA, BA, GB, AM, KD, AB and IM contributed to data collection and analysis. All authors contributed to data interpretation and implications of findings for practice and research. KD, AB and IM drafted the manuscript. All authors approved the final version of the article for publication.
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the CHUM research ethics committee (project # 2019–8177, 18.353).
Consent for publication
Not applicable.
Competing interests
S. Robin Cohen is an Associate Editor of this journal. The Authors declare that they have no other competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy. Describes exhaustively the search strategy (concepts, keywords and electronic databases).
Additional file 2.
Description of included studies. Includes the titles of the selected studies, years, countries, population types and contexts.
Additional file 3.
List of activities. Includes the activities and their categorization (development stages, implementation types, health promotion strategies) for each article reporting implemented activities in practice.
Additional file 4.
Evaluation approaches. Includes detailed description of evaluation approaches (what is measured, how and at which levels) for each article reporting evaluation methods and results.
Additional file 5.
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dumont, K., Marcoux, I., Warren, É. et al. How compassionate communities are implemented and evaluated in practice: a scoping review. BMC Palliat Care 21, 131 (2022). https://doi.org/10.1186/s12904-022-01021-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-022-01021-3