Abstract
Background
Dental caries is a common disease in the oral cavity, and the microorganisms in the cavity are colonized in the form of dental plaque biofilm. Streptococcus mutans is the main pathogen causing dental caries. Using probiotics to inhibit the growth and colonization of pathogenic bacteria, regulate mucosal immunity and improve oral microecological balance is an effective way to prevent or treat dental caries. The aim of this study was to evaluate the caries-prevention of probiotics in vitro and in rat caries models.
Methods
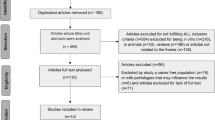
The probiotics used in this study are a combination of 4 strains of bacteria. After the fermentation of 4 strains (L. plantarum, L. salivarius, L. rhamnosus, and L. paracasei) was completed, they were mixed in equal volume proportions and used as samples to be tested. The mixture was then assessed the ability to inhibit the growth of S. mutans in vitro and in vivo. SPSS Statistics 22.0 (SPSS, Inc., Chicago, IL, USA) was used for analysis.
Results
In vitro the probiotics mixture could inhibit the growth of S. mutans and was able to remove biofilms formed by S. mutans. In a 42-day in vivo experiment, the probiotics group significantly reduced the level of S. mutans on the tooth surface of rats, reducing more than half the bacterial quantities compared with the caries model group (P < 0.05). The amount of S. mutans in the antagonist group was low and highly significant compared with the caries model group. Moreover, the mixture of 4 strains significantly reduced the caries scores (modified Keyes scoring method) in both the probiotic and antagonist groups (p < 0.05).
Conclusions
The study showed that the combination of the four strains can reduce the cavity scores, and the four strains can be used as products in oral care products. At the same time, the study also suggests that probiotic therapy can be an effective way to prevent dental caries.
Similar content being viewed by others
Background
Dental caries is one of the most common oral diseases worldwide, particularly in developing countries [1]. The WHO Global Oral Health Status Report (2022) estimated that oral diseases affect nearly 3.5 billion people worldwide, with 3 out of 4 people living in middle-income countries [2]. Globally, an estimated 2 billion people suffer from caries of permanent teeth, and 514 million children suffer from caries of primary teeth. In 2016, caries in permanent and deciduous teeth ranked second and fifth, respectively, among the 10 diseases with the highest global incidence. Caries is the result of the complex interaction between dietary carbohydrates and cariogenic microorganisms in oral bioflms, also influenced by the quality and quantity of saliva; the disease results from shifts in the balance of the resident microbiota driven by changes in the local environmental conditions [3]. Recent studies have shown that tooth decay is the result of a synergistic action of several species. Of these, S. mutans, L. acidophilus, and Actinomyces viscosus may be considered the main pathogenic species involved in the initiation and development of dental caries [4]. Streptococcus mutans is one of the main microbial pathogens of dental caries. [5]. The cell surface protein PAc is an S. mutans virulence factor because it is involved in the initial adherence of the organism to tooth surfaces [6, 7]. As S. mutans adheres to the tooth surface, it forms biofilm dental plaque. The formation of a bacterial biofilm plaque is a prerequisite for the occurrence of caries [8]. Many studies have reported the relationship between the presence of S. mutans, biofilm formation, and the related risk of caries [9,10,11]. Therefore, inhibiting the growth of S. mutans and removing the biofilm formed by S. mutans is an important method of treating dental caries.
Once dental plaque has formed, it can damage the structure of the tooth and even destroy the nerve causing toothache. Finding an effective way to prevent or reduce the cavity scores is important for oral health. Probiotics are a group of active microorganisms that are beneficial to their hosts [12]. Probiotics have been recognized in regulating gut health [13,14,15], and there also can be effective in oral health [16, 17]. For example, Chuang et al. [18] reported that probiotic L. paracasei GMNL-33 may reduce caries-associated salivary microbial counts in healthy adults. Ahola et al. [19] reported that short-term consumption of cheese containing Lactobacillus rhamnosus GG and Lactobacillus rhamnosus LC705 can reduce the counts of Streptococcus mutans and salivary yeasts in young people. Villavicencio et al. [20] showed that consumption of milk with Lactobacillus rhamnosus and Bifidobacteruim longum could reduce the amount of S. mutans in saliva. Teanpaisan et al. [21, 22] revealed that either short-term or long-term consumption of milk powder containing L. paracasei SD1 could reduce salivary cariogenic mutans streptococci resulting in low risk for caries. Our previous studies explored the ability of L. plantarum VHProbi V38 and L. rhamnosus VHProbi M14 to inhibit the growth of S. mutans and remove biofilms formed by S. mutansin vitro [23, 24]. The screening of candidate oral probiotics based on their abilities to inhibit S. mutans growth and biofilm formation may represent an alternative means of preventing tooth decay.
In this study, we first evaluated the inhibition and biofilm removal effects of the combined use of 4 strains of probiotics on S. mutansin vitro. Then we also examined oral S. mutans colonization and caries formation in rats using bacterial counts and caries scores to evaluate the effect of probiotics on the prevention or treatment of caries in vivo. These results will support and inform the development of probiotics to prevent caries.
Methods
Bacterial strains and mice
S. mutans strains BNCC 700,610 and ATCC 25,175 were purchased from the BeNa Culture Collection Centre (Beijing, China). S. mutans CCTCC AB 99,010 was purchased from the China Center for Type Culture Collection (Wuhan, China). The 3 strains were cultured in the brain-heart infusion (BHI) broth both separately for 24 h with a bacterial load of 108 CFU/mL in aerobic conditions at 37℃ and then mixed in a volume ratio of 1:1:1. All references to S. mutans fluids in this article refer to a mixture of the 3 strains.
L. plantarum VHProbi V38, Ligilactobacillus salivarius VHProbi A17, L. rhamnosus VHProbi M14 and L. paracasei VHProbi OF10 were kept in China Center for Type Culture Collection (NO: M2022173, M2022172, M2022171 and M2022170, Wuhan, China). The 4 strains were individually incubated for 24 h in Man, Rogosa, and Sharpe (MRS) broth with a bacterial load of 108 CFU/mL. They were then mixed in equal volumes to prepare the probiotic mixture for the test. All references to Lactobacillus liquid in this article refer to a mixture of the 4 strains.
Twenty 3-week-old weanling specific pathogen-free (SPF) male Wistar rats were provided by the Qinglong Mountain Animal Breeding Centre (Jiangsu, China) under license number SCXK(Su)2017-0001. The rats were fed a special pellet diet (Diet 2000, Jiangsu Synergy Biological Co., Ltd.) and housed in an SPF-class animal house after the caries model was constructed. Housing conditions included a 12 h/12 h light/dark cycle, free feeding and watering, a temperature of 20–26 °C, and relative humidity between 40% and 70%.
Bacteriostatic activity testing
The antibacterial activities of Lactobacillus strains against S. mutans were quantified using a modified agar-diffusion method and co-culture in vitro [25,26,27,28].
A volume of 100 mL melted BHI agar medium, maintained at ~ 45℃, was inoculated with 300 µL mixed bacterial suspension of S. mutans (OD600 0.5–0.6). The medium (7 mL) containing S. mutans was quickly poured into solidified agar plates. After medium solidification, Oxford cups were placed on the surfaces of the cultures, and 100 µL of the supernatant of lactic acid bacteria (LAB) isolates was dripped into the Oxford cup. All experiments were performed in triplicate. The growth inhibitory activity of the supernatant was calculated by measuring the diameter of the inhibition zone.
The BHI broth (10 mL) was initially mixed with 0.3% (v/v) of the lactic acid bacteria culture (108 CFU/mL) and S. mutans culture (108 CFU/mL) as the inoculants, and cultured at 37℃ for 48 h. The control group was inoculated with S. mutans in BHI broth only. Samples were taken to determine the viable bacterial counts (CFU/mL) for S. mutans using Mitis Salivarius Bacitracin agar. All tests were conducted in triplicate. The inhibition rate (%) was calculated as follows:
Biofilm elimination testing
Biofilm removal assay in polystyrene 24-well (flat bottom) plates was performed using the method by Zhang et al. [23] and Khan et al. [29]. A total of 600 µL of the S. mutans cultures in BHI broth was transferred to a 24-well plate with chamber slides and incubated for 24 h to form a biofilm at 37℃ under aerobic conditions. The plate was washed twice with phosphate buffer solution (PBS) (pH 7.0, 0.05 M potassium phosphate). 600 µL of cell suspension (or the supernatant) of lactic acid bacteria was inoculated into the wells. The cell suspension of lactic acid bacteria was harvested by centrifugation at 5,000 × g for 15 min, washed 3 times with PBS, and resuspended in PBS at a concentration of approximately 108 CFU/mL. MRS broth alone was used as the control. After inoculation, all plates were incubated at 37℃ for 24 h to measure the ability of the samples to remove biofilms. All tests were conducted in triplicate. The culture medium was then decanted, and the plates were gently washed 3 times with 600 µL sterilized PBS to remove planktonic and loosely bound cells.
The biofilm removal rate was determined by counting the number of bacteria on the chamber slides. The chamber slides were removed and placed in sterile homogeneous bags. The slides were then subjected to a 10-minute ultrasonic wash to diffuse the organisms into the buffer solution. After a series of dilutions, 100 µL of the samples were cultured into Mitis Salivarius Bacitracin (MSB) agar plates containing 400 U/L bacitracin (G-clone, 65000u/g, China) to determine the concentration of S. mutans. The following formula was used to calculate the removal rate of biofilm:
Animal experiments
Rat caries model and general procedures
Twenty rats (3 weeks old) were allowed to adapt to the diet and environment for 3 days. They were then divided randomly into 4 groups (n = 5/group), comprising a normal group (N), caries control group (C), probiotic group (P), and antagonist group (A). The rats in each group were then given antibiotic water at a concentration of 200 mg/L of penicillin and 1500 mg/L of streptomycin for 3 consecutive days. On day 7, the rats were taken off antibiotic water and fasted from food and water for 2 h. Saliva was collected from each group using sterile cotton swabs. The swabs were suspended in sterile saline, and the bacterial count was detected using MSB agar. The rats were fed with sterilized chow and water. The caries model was started when the MSB plates were negative. The rats in the C and P groups were subjected to 7 consecutive days of dental caries modeling. In brief, 1 mL of S. mutans culture (108 CFU/mL) was dipped into a sterile cotton stick. The sterile cotton swab was then applied to the rat’s oral cavity for 15 s per quadrant, as described by Beiraghi et al. [30]. On day 7, oral swabs were spread on MSB agar plates supplemented with 400 µg/L bacitracin (G-clone, 65000u/g, China) to confirm S. mutans colonization in the oral cavity. After successful molding, the C group was treated with high-sugar feed sterilized by Co60 irradiation and observed for 5 weeks. The P group was continuously treated with 1 mL probiotic mixture (108 CFU/mL) for 1 week and observed for 4 consecutive weeks. The N group consumed a regular diet and water throughout the 6-week experimental period. The A group was treated with 2 mL mixed fermentation solution (the probiotic mixture: S. mutans culture = 1:1) for one week and observed for 5 consecutive weeks. During the experiment, all groups except the N group were fed 5% glucose water and a high-sugar diet sterilized by Co60 irradiation for six weeks. The ingredients of the high-sugar diet (Diet 2000 caries modelling feed) were: whole meal flour 6%, sucrose 56%, skimmed unsweetened milk powder 28%, yeast 4%, alfalfa meal 3%, liver powder 1% and salt 2%. The regular diet was rat maintenance feed (HFK 1025, Beijing, China). The experimental protocol is shown in Table 1.
This study was carried out at the laboratory of BIOGENE Biotech. Co. Ltd. (Nanjing, China), which has been approved by Laboratory Animal Ethics Committee Nanjing BIOGENE Biotech. Co. Ltd. All methods were carried out in accordance with relevant guidelines and regulations. All methods were in accordance with ARRIVE guidelines.
Observations and microbial analysis
We observed the mortality, mental activity, and hair shine of mammary rats and recorded the weight of rats every week.
The whole experiment lasted 6 weeks, during which 4 samples were collected on days 7, 14, 28, and 42. The N group was tested in the first week only. The samples were collected by rubbing a sterile cotton swab in clockwise circles on the molar occlusal surface of the mouth of each group. The swab was immediately placed in a centrifuge tube containing 1 mL of saline for 2 min. After a series of dilutions, bacterial counts were performed on the MSB plates with the appropriate dilution.
Caries scoring and X-ray test
At the end of the 6-week trial, the rats were placed in the euthanasia chamber (Fengshi FSZZ-2 A, Suzhou, China), then the lid was fastened. A CO2 gas line was connected and CO2 was injected into the chamber at a rate of 10–30% of euthanasia box volume per min. After the rats have collapsed and lost the ability to move, the gas flow rate can be increased to a maximum of 0.5 Kpa. The CO2 was not switched off until the rats were immobile, not breathing and its pupils were dilated. Then the rats were observed for two minutes to determine death. The skull was removed, the soft tissues on the teeth and jaws were peeled off with a scalpel, and the jaws were cleaned with ultrasound for 20 min. Then the skull was placed in an autoclave at 121 °C for 15 min. The attached soft tissue was again peeled off with a scalpel, and the jaw was cleaned and dried at room temperature. The teeth on the left side of the rat were used to assess caries scores. The upper and lower jaws were soaked in 10% paraformaldehyde for 24 h and then washed and dried. All specimens were immersed in a 0.4% ammonium purpurate staining solution for 12 h, rinsed, and semi-sectioned along the occlusal surfaces of maxillary and mandibular molars using a diamond cutter (thickness: 0.1 mm). Caries on the rat molars were observed and evaluated under a stereomicroscope according to the caries diagnosis and scoring method reported by Keyes [31]. The method of assigning values involves judging by eye the linear extent of lesions in one plane and recording the depth of penetration under 4 headings, including enamel only (E), slight dentinal (Ds), moderate dentinal (Dm), and extensive dentinal (Dx). The scoring rules are shown in Table 2 [31].
The teeth on the right side of the rat were used for x-ray detection. Rat mandibles were scanned using a small animal X-ray machine, and the pictures were analyzed after scanning.
Statistical analysis
SPSS Statistics 22.0 (SPSS, Inc., Chicago, IL, USA) was used for analysis. All data are presented as the mean ± SD. Where applicable, ANOVA or a 2-tailed Student’s t-test was used to analyze the differences between treatments. A p-value < 0.05 was considered statistically significant. A p-value < 0.01 was considered highly statistically significant.
Results
In vitro experiments
The inhibition diameter of the supernatant was 2.45 ± 0.05 cm. This indicates that the mixture of the four strains was able to inhibit the growth of S. mutans under static conditions. Under co-culture conditions, Lactobacillus culture was able to significantly inhibit the growth of S. mutans. As shown in Fig. 1, the amounts of bacteria in the control group were 9.50 ± 0.10 log CFU/mL, while the amounts of bacteria in the experimental group were 7.66 ± 0.17 log CFU/mL at 24 h. The amounts of bacteria in the control group were 8.10 ± 0.06 log CFU/mL, while the amounts of bacteria in the experimental group were 7.27 ± 0.06 log CFU/mL at 48 h, The inhibition rate at 24 h was 98.48%±0.54%. As the growth time was extended, the bacterial load of both Lactobacillus and S. mutans decreased and the inhibition rate became lower, with an inhibition rate of 84.18%±2.11%.
The mixture of 4 strains were able to reduce the number of S. mutans in the biofilm as shown in Fig. 2. The number of S. mutans on the chamber slides of the probiotic-added group was much lower than that of the control group. In the control group, the number of S. mutans was 5.47 ± 0.05 log CFU/well. In the supernatant group, the number was < 2.00 ± 0.00 log CFU/well. In the bacteria group, the number was 4.95 ± 0.02 log CFU/well. The supernatant was able to completely remove the biofilm of S. mutans with 100%±0.00% removal, while the bacteria was able to partially remove the biofilm with 68.45%±0.74% removal.
Animal experiments
General status of WISTAR rats in each group
During the entire experimental period, the rats in each group had normal activity, shiny hair, pelleted feces, and no diarrhea. The body weight of each group of rats is shown in Table 3. No inflammation, erythema, or swelling of the oral cavity was observed in any group of rats after S. mutans application. There was no mortality in any of the groups throughout the observation period, and there was no significant difference in weight gain between the N group and the other groups (p > 0.05).
Oral strain colonisation in WISTAR rats
Bacterial colonization of the oral cavity of each group of rats was performed on days 7, 14, 28, and 42 (Fig. 3). The rats in the N (normal) group did not contain S. mutans. The number of S. mutans in the C (caries control) and P (probiotic) groups gradually increased over 7 days, showing stable colonization. The concentrations of S. mutans on the molars of the C and P groups was approximately 1.0 × 104 CFU/mL after 7 days of infection, indicating that S. mutans had successfully colonized the oral cavities. In the C group, the amount of S. mutans increased with feeding extension time and reached 7.2 × 104 CFU/mL at 42 days. In the P group, the amount of S. mutans increased first and then decreased with the intervention of probiotics. At 42 days, the amount of S. mutans in the P group was 0.4 times that in the C group, and the number significantly decreased (p < 0.05). In the A (antagonist) group, the number of S.mutans remained low throughout the trial period, about 0.5–1.7 × 103 CFU/mL. The amount of S. mutans in the A group was low and highly significant compared with the C group (p < 0.01).
Observation and scoring of the dental profile of rats
After the rat jaw bone samples were stained with ammonium purpurate staining solution, we observed that the molar teeth of the C group had different degrees of red stained caries areas under the in vivo microscope (Zeiss P30020001, Germany) (Fig. 4). The red-stained areas were observed in both the profile and cross-sectional views, indicating that the model was successfully constructed (Fig. 4B). This model can build a stable and qualified scheme for the pharmacodynamic evaluation of dental caries.
Figure 4C shows that the cavity scores were significantly reduced in the P group. Figure 4A and D shows that there was no evidence of dental caries visually in the A and N groups. The cheek, tongue and adjacent surfaces, and sulcal of a rat molar can be divided into several dental caries units according to the extent of caries damage, as shown in Table 2. Furthermore, Table 2 demonstrates how the dental caries units were determined and scored; the score results for the corresponding caries are shown in Table 4. According to the Keyes scoring rules, 12 maxillary and mandibular molars from each group were scored on 4 dimensions: E, Ds, Dm, and Dx. Caries scores for all 4 dimensions (i.e., E, Ds, Dm, and Dx) were significantly (p < 0.05) lower in the P-administered group compared with the C group. Moreover, caries scores on the sulcus surface in the A group were highly significant lower compared with the C group (p < 0.01). These caries scores in the P and A groups were less than in the C group, suggesting that probiotics have the potential to prevent caries in vivo.
WISTAR Rat teeth grinding X-ray images
The caries status of the molars of rats in each group was determined by X-ray diffraction. The results are shown in Fig. 5. The alveolar bone of the rats in all groups was well aligned, with no obvious abnormalities and no significant widening of the periodontal gaps. In the C and P groups, a certain degree of bone loss was observed in the alveolar bone (Fig. 5B, C). No alveolar damage was observed in the N and A groups (Fig. 5A, D). These 4 strains of probiotics had some protective effects on the molar tissue of rats.
Discussion
Dental caries is a multifactorial disease. Its pathogenesis involves the microbiota (mainly S. mutans), the host, and its immune mechanisms and diet, among other factors [32,33,34]. Even though all these factors must intervene for dental caries to develop, microbiological factors are still the leading cause of this disease. Therefore, bacteriotherapy is believed to positively influence the prevention of this disease [33,34,35,36].
S. mutans forms plaque biofilms through surface protein binding to sites on acquired membranes on the tooth surface. Biofilms are the main cause of dental caries formation. Therefore, the inhibition and removal of dental plaque biofilm are important for preventing caries [37]. In-vitro studies suggest that probiotics can prevent the adhesion of S. mutans to saliva-coated hydroxyapatite and interfere with caries-related biofilm formation [38,39,40,41]. The inhibitory effects of probiotics against S. mutans may be due to antimicrobial substances produced by probiotics, including organic acids, hydrogen peroxide, bacteriolytic enzymes, bacteriocins, and biosurfactants [42, 43]. In this study, the probiotics mixture showed good inhibition of the growth of S. mutans under both dynamic conditions (co-culture) and static conditions (inhibition test). Based on these results, it is hypothesized that these lactic acid bacteria can metabolize antibacterial substances, such as lactic acid and antimicrobial peptides. Organic acids can reduce the pH of the environment, thus inhibiting the growth of pathogenic bacteria. Antimicrobial peptides can interfere with the synthesis of bacterial cell wall of pathogenic bacteria, so as to achieve antibacterial effect. The whole genomes of these four strains have been uploaded into the NCBI database (M14, CP095384; OF10, CP092498; V38, CP092501; A17, CP097165), and they can also be found to have bacteriocin-related coding genes. Both the supernatant and the bacteria were able to remove the biofilm of S. mutans. The removal of biofilm by supernatant may be the effect of acid, which causes S. mutans to fall off the chamber slides. The removal of the biofilm by the bacteria should be that the probiotics have recognition protein, which can bind to the recognition protein of S. mutans, thereby destroying the biofilm. The inhibitory effects of Lactobacillus on S. mutans in vitro do not necessarily mean that Lactobacillus has the same effects in vivo. Therefore, this study further examined the anti-caries activity of the 4 strains in a rat model of dental caries. In the first 14 days of the rat experiment, there was no significant difference in the number of S. mutans between the control group and the probiotic group, indicating that the short intervention of probiotics did not play an inhibitory role. In the 28–42 days of intervention, the bacteria amount of S. mutans in probiotics was significantly lower than that in the control group, indicating that probiotics could inhibit the growth of S. mutans with the extension of intervention time (Fig. 3). But probiotics don’t completely eliminate S. mutans. From the score results and pictures (Figs. 4 and 5), the cavity scores were reduced after probiotic prevention. These results indicate that the 4 strains may be useful in the prevention of dental caries caused by S. mutans. The antagonistic experimental group simulates the coexistence of lactic acid bacteria and S. mutans in the mouth. Probiotics and S. mutans were applied to the teeth of rats at the same time to see how the teeth changed. The results showed that there was only a small amount of S. mutans on the teeth of rats in the antagonistic group on the 7th day, and basically no streptococcus mutans growth in the later period. From the staining and X-ray tooth pictures (Figs. 4 and 5), the appearance of teeth in the antagonistic group was no different from that in the normal group, indicating that taking probiotics could prevent the occurrence of dental caries in rats without dental caries. These results indicate that the 4 strains may be contribute to the prevented the development of dental caries.
The clinical effectiveness of probiotics depends on the appropriate strain, duration of treatment, concentration, and the ideal vehicle for use. Current studies have shown that probiotic products can reduce the population of S. mutans in the human oral cavity and could have a preventive effect on the development of dental caries [34, 44,45,46,47]. Future studies will include clinical trials at a later stage to explore the clinical performance of these 4 bacterial strains and lay the foundation for possible product development. Interest in postbiotics is increasing as there are limitations to the storage and use of probiotics [48]. Considering the potential future application areas, we will also explore the clinical efficacy of the postbiotic of this complex probiotic at a later stage.
Data availability
The data presented in this study are available within the article.
References
Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet (London England). 2007;369(9555):51–9.
Organization WH. Oral health In.; 2022: https://www.who.int/news-room/fact-sheets/detail/oral-health
Aas JA, Griffen AL, Dardis SR, Lee AM, Olsen I, Dewhirst FE, Leys EJ, Paster BJ. Bacteria of dental caries in primary and permanent teeth in children and young adults. J Clin Microbiol. 2008;46(4):1407–17.
Shivakumar KM, Vidya SK, Chandu GN. Dental caries vaccine. Indian J Dent Research: Official Publication Indian Soc Dent Res. 2009;20(1):99–106.
Simón-Soro A, Mira A. Solving the etiology of dental caries. Trends Microbiol. 2015;23(2):76–82.
Russell MW, Mansson-Rahemtulla B. Interaction between surface protein antigens of Streptococcus mutans and human salivary components. Oral Microbiol Immunol. 1989;4(2):106–11.
Okahashi N, Sasakawa C, Yoshikawa M, Hamada S, Koga T. Molecular characterization of a surface protein antigen gene from serotype c Streptococcus mutans, implicated in dental caries. Mol Microbiol. 1989;3(5):673–8.
Featherstone JD. The continuum of dental caries–evidence for a dynamic disease process. J Dent Res 2004, 83 Spec C:C39–42.
Bowen WH, Koo H. Biology of Streptococcus mutans-derived glucosyltransferases: role in extracellular matrix formation of cariogenic biofilms. Caries Res. 2011;45(1):69–86.
Mashima I, Nakazawa F. The interaction between Streptococcus spp. and Veillonella tobetsuensis in the early stages of oral biofilm formation. J Bacteriol. 2015;197(3):2104–11.
Huang R, Li M, Gregory RL. Bacterial interactions in dental biofilm. Virulence. 2011;2(5):435–44.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Reviews Gastroenterol Hepatol. 2014;11(8):506–14.
Yeun Y, Lee J. Effect of a double-coated probiotic formulation on functional constipation in the elderly: a randomized, double blind, controlled study. Arch Pharm Res. 2015;38(7):1345–50.
Guglielmetti S, Mora D, Gschwender M, Popp K. Randomised clinical trial: Bifidobacterium bifidum MIMBb75 significantly alleviates irritable bowel syndrome and improves quality of life–a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33(10):1123–32.
Sisson G, Ayis S, Sherwood RA, Bjarnason I. Randomised clinical trial: a liquid multi-strain probiotic vs. placebo in the irritable bowel syndrome–a 12 week double-blind study. Aliment Pharmacol Ther. 2014;40(1):51–62.
Haukioja A. Probiotics and oral health. Eur J Dentistry. 2010;4(3):348–55.
Näse L, Hatakka K, Savilahti E, Saxelin M, Pönkä A, Poussa T, Korpela R, Meurman JH. Effect of long-term consumption of a probiotic bacterium, Lactobacillus rhamnosus GG, in milk on dental caries and caries risk in children. Caries Res. 2001;35(6):412–20.
Chuang LC, Huang CS, Ou-Yang LW, Lin SY. Probiotic Lactobacillus paracasei effect on cariogenic bacterial flora. Clin Oral Invest. 2011;15(4):471–6.
Ahola AJ, Yli-Knuuttila H, Suomalainen T, Poussa T, Ahlström A, Meurman JH, Korpela R. Short-term consumption of probiotic-containing cheese and its effect on dental caries risk factors. Arch Oral Biol. 2002;47(11):799–804.
Villavicencio J, Villegas LM, Arango MC, Arias S, Triana F. Effects of a food enriched with probiotics on Streptococcus mutans and Lactobacillus spp. salivary counts in preschool children: a cluster randomized trial. J Appl oral Science: Revista FOB. 2018;26:e20170318.
Teanpaisan R, Piwat S. Lactobacillus paracasei SD1, a novel probiotic, reduces mutans Streptococci in human volunteers: a randomized placebo-controlled trial. Clin Oral Invest. 2014;18(3):857–62.
Teanpaisan R, Piwat S, Tianviwat S, Sophatha B, Kampoo T. Effect of long-term consumption of Lactobacillus paracasei SD1 on reducing mutans Streptococci and Caries Risk: a randomized placebo-controlled trial. Dentistry J. 2015;3(2):43–54.
Zhang J, Duan Z. Identification of a new probiotic strain, lactiplantibacillus plantarum VHProbi(®) V38, and its use as an oral health agent. Front Microbiol. 2022;13:1000309.
Zhang JY, Li KL, Bu XP, Cheng SM. Characterization of the anti-pathogenic, genomic and phenotypic properties of a lacticaseibacillus rhamnosus VHProbi M14 isolate. PLoS ONE. 2023;18:e0285480.
Lin T-H, Pan T-M. Inhibitory effect of Lactobacillus paracasei subsp. paracasei NTU 101 on rat dental caries. J Funct Foods. 2014;10:223–31.
Sookkhee S, Chulasiri M, Prachyabrued W. Lactic acid bacteria from healthy oral cavity of Thai volunteers: inhibition of oral pathogens. J Appl Microbiol. 2001;90(2):172–9.
Zhang XZB, Zhang XM, Li PL. Screen of bacteriocin producing lactic acid bacteria the analysis of bacteriocin related genes. Acta China Agi Univ. 2013;18(4):168–77.
Wenji Y. Experiment research of antagonistic effects of two probiotics on halitosis pathogens. In: 2015; 2015.
Khan R, Zakir M, Khanam Z, Shakil S, Khan AU. Novel compound from Trachyspermum ammi (Ajowan caraway) seeds with antibiofilm and antiadherence activities against Streptococcus mutans: a potential chemotherapeutic agent against dental caries. J Appl Microbiol. 2010;109(6):2151–9.
Beiraghi S, Rosen S, Beck F. The effect of stannous and sodium fluoride on coronal caries, root caries and bone loss in rice rats. Arch Oral Biol. 1990;35(1):79–80.
Keyes PH. Dental caries in the molar teeth of rats. II. A method for diagnosing and scoring several types of lesions simultaneously. J Dent Res. 1958;37(6):1088–99.
Iheozor-Ejiofor Z, Worthington HV, Walsh T, O’Malley L, Clarkson JE, Macey R, Alam R, Tugwell P, Welch V, Glenny AM. Water fluoridation for the prevention of dental caries. The Cochrane database of systematic reviews 2015, 2015(6):Cd010856.
Laleman I, Teughels W. Probiotics in the dental practice: a review. Quintessence Int (Berlin Germany: 1985). 2015;46(3):255–64.
Laleman I, Detailleur V, Slot DE, Slomka V, Quirynen M, Teughels W. Probiotics reduce mutans Streptococci counts in humans: a systematic review and meta-analysis. Clin Oral Invest. 2014;18(6):1539–52.
Gruner D, Paris S, Schwendicke F. Probiotics for managing caries and periodontitis: systematic review and meta-analysis. J Dent. 2016;48:16–25.
Flichy-Fernández AJ, Alegre-Domingo T, Peñarrocha-Oltra D, Peñarrocha-Diago M. Probiotic treatment in the oral cavity: an update. Med oral Patologia oral y Cir Bucal. 2010;15(5):e677–680.
Lee SH, Kim YJ. A comparative study of the effect of probiotics on cariogenic biofilm model for preventing dental caries. Arch Microbiol. 2014;196(8):601–9.
Haukioja A, Loimaranta V, Tenovuo J. Probiotic bacteria affect the composition of salivary pellicle and streptococcal adhesion in vitro. Oral Microbiol Immunol. 2008;23(4):336–43.
Söderling EM, Marttinen AM, Haukioja AL. Probiotic lactobacilli interfere with Streptococcus mutans biofilm formation in vitro. Curr Microbiol. 2011;62(2):618–22.
Lin X, Chen X, Tu Y, Wang S, Chen H. Effect of Probiotic Lactobacilli on the growth of Streptococcus Mutans and multispecies biofilms isolated from children with active caries. Med Sci Monitor: Int Med J Experimental Clin Res. 2017;23:4175–81.
Ciandrini E, Campana R, Baffone W. Live and heat-killed Lactobacillus spp. interfere with Streptococcus mutans and Streptococcus oralis during biofilm development on titanium surface. Arch Oral Biol. 2017;78:48–57.
Brul S, Coote P. Preservative agents in foods. Mode of action and microbial resistance mechanisms. Int J Food Microbiol. 1999;50(1–2):1–17.
Wannun P, Piwat S, Teanpaisan R. Purification, characterization, and Optimum conditions of Fermencin SD11, a Bacteriocin produced by human orally Lactobacillus fermentum SD11. Appl Biochem Biotechnol. 2016;179(4):572–82.
Wattanarat O, Makeudom A, Sastraruji T, Piwat S, Tianviwat S, Teanpaisan R, Krisanaprakornkit S. Enhancement of salivary human neutrophil peptide 1–3 levels by probiotic supplementation. BMC Oral Health. 2015;15:19.
Jindal G, Pandey RK, Agarwal J, Singh M. A comparative evaluation of probiotics on salivary mutans Streptococci counts in Indian children. Eur Archives Pediatr Dentistry: Official J Eur Acad Pediatr Dentistry. 2011;12(4):211–5.
Nagarajappa R, Daryani H, Sharda AJ, Asawa K, Batra M, Sanadhya S, Ramesh G. Effect of Chocobar ice cream containing Bifidobacterium on salivary Streptococcus mutans and lactobacilli: a Randomised Controlled Trial. Oral Health Prev Dent. 2015;13(3):213–8.
Salem R, Abd-El-Aziz A, Erfan D. Assessment of the Effect of Probiotic Yoghurt and different probiotic strains on salivary Streptococcus Mutans in children: an in Vivo and an in Vitro Study. Egypt J Med Microbiol. 2016;25:35–41.
Mosca A, Abreu YAAT, Gwee KA. The clinical evidence for postbiotics as microbial therapeutics. 2022, 14(1):2117508.
Acknowledgements
This study was supported by the Mountain Tai New Strategy Industry Leader Program and Qingdao Vland Biotech Group Co., Ltd.
Funding
This study was supported by a grant from the Mountain Tai New Strategy Industry Leader Program (grant No. tscy20180317).
Author information
Authors and Affiliations
Contributions
Jingyan Zhang : Conceptualization, Methodology, Software, Validation, Formal analysis, Data curation, Investigation, Writing—original draft, Writing—review &editing draft; Qian Wang: Conceptualization, Methodology, Data curation, Writing—original draft. Zhi Duan: Conceptualization, Methodology , Investigation, Re-sources, Data curation, Writing—review and editing, supervision, Visualization, Project administration, Funding acquisition.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. All methods were in accordance with ARRIVE guidelines. The animal test was approved by Laboratory Animal Ethics Committee Nanjing BIOGENE Biotech. Co. Ltd.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, J., Wang, Q. & Duan, Z. Preventive effects of probiotics on dental caries in vitro and in vivo. BMC Oral Health 24, 915 (2024). https://doi.org/10.1186/s12903-024-04703-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04703-x