Abstract
Objectives
This study aimed to evaluate the feasibility of monolithic zirconia laminate veneers (MZLV) compared to lithium disilicate laminate veneers (LDLV).
Materials and methods
Sixty resin replicas, each prepared with depths of 0.5 mm, 0.7 mm, and 1 mm, were produced using a 3D printer from acrylic teeth. Laminate veneers of these thicknesses were milled from pre-sintered monolithic zirconia (3rd generation) and lithium disilicate blocks. The intaglio surface of MZLV was treated with air abrasion using 110 μm diameter silica-modified aluminium oxide particles and ceramic primer, while LDLV was etched with etchant gel and treated with the ceramic primer before cementation with resin cement. Vertical marginal discrepancy (VMD) was assessed using a stereomicroscope, and a load-to-failure test was conducted using a universal testing machine. Failure modes were evaluated macroscopically on fractured surfaces. Data were analysed statistically using Two-way ANOVA and Bonferroni correction (α = 0.05).
Results
LDLV samples exhibited significantly larger VMD compared to MZLV samples across all thicknesses, especially in cervical, palatal, and mean data. Within the LDLV group, load-to-fracture values for 0.7 mm and 1.0 mm thicknesses were similar, whereas for 0.5 mm thickness, it was significantly lower. In the MZLV group, load-to-fracture values were lower for 0.7 mm and 1.0 mm thicknesses compared to LDLV, but higher for 0.5 mm thickness.
Conclusions
Material choice and restoration thickness significantly influence laminate veneer restorations’ success. MZLV generally exhibits superior vertical marginal fit compared to LDLV, with varying load-to-failure values across different thicknesses. Clinical management of debonding in MZLV is simpler compared to restoration fracture in LDLV.
Clinical relevance
Considering clinical factors, MZLV may be a preferable option to LDLV for this restoration with the thickness of 0.5 mm.
Similar content being viewed by others
Introduction
Monolithic computer-aided design (CAD) and computer-aided manufacturing (CAM) ceramic restorations have become increasingly prevalent in daily practice due to their high accuracy, rapid fabrication methods, and extensive range of available materials [1, 2]. Recent studies have indicated that CAD-CAM restorations exhibit superior marginal adaptation compared to conventionally fabricated indirect restorations [3, 4]. Also, Laminate veneers (LVs) can be manufactured utilising CAD-CAM technology [5]. A variety of materials are employed in the fabrication of monolithic CAD-CAM LVs, including glass ceramics (such as lithium disilicate, leucite-reinforced feldspathic, and feldspathic porcelain), zirconia, resin composite, resilient (hybrid) ceramics, polymer-infiltrated ceramics, and zirconia-reinforced lithium silicate [6, 7]. Lithium disilicate has emerged as a leading glass ceramic utilized in dentistry [8]. Veneers represent one of its notable applications, offering clinicians an optimal balance between aesthetics and strength for all ceramic monolithic restorations [9]. However, caries, cracks, chipping, debonding, aesthetic matches, surfaces, marginal discoloration, and marginal defects are the most common complications that may occur resulting from the use of lithium disilicate laminate veneers [10].
Zirconia laminate veneers, when precision-milled using CAD-CAM technology, offer several advantages. For instance, they are applicable in clinical scenarios involving wide diastema or damaged teeth due to injury or decay, where the inner surface (lingual) remains undamaged. Glass-ceramic veneers have been noted as inappropriate in clinical scenarios where there are traumatic parafunctional occlusal forces, particularly in cases of reverse and edge-to-edge occlusal relationships. These conditions engender loading stress during functional activities, rendering glass ceramic veneers unsuitable for such cases. Traditional porcelain veneers are delicate and pose challenges in terms of adjustment and contouring before cementation. Nevertheless, the robustness of zirconia enables easier handling, facilitating adjustments of the veneer before cementation [11]. Moreover, zirconia laminate veneers may be considered when patients desire exceptionally bright teeth.
The mechanical and optical properties of zirconia are influenced by the mol concentration of yttria [12]. To enhance its translucency, increasing the yttria content in Y-PSZ to up to 5% results in 5Y-PSZ with larger grain sizes. This process involves replacing tetragonal grains with cubic grains, which reduces light scattering and birefringence at grain boundaries, thereby achieving ultra-translucency [13]. Manufacturers recommend not using monolithic cubic zirconia (MCZ) below 0.4 mm thickness.
Mechanical properties are crucial for the long-term clinical success of laminate veneer restorations. However, the selection of new restorative materials should ideally be based on clinical evidence. Consequently, in vitro, testing of dental materials is a valuable alternative for evaluating their properties and understanding their behaviour [14].
The marginal edges of the laminate veneer ceramic restorations are very critical areas that play a key role in the success of this type of aesthetic restoration [15]. Marginal integrity is essential for the long-term success of porcelain laminate veneers. However, evidence regarding their marginal fit remains unclear [16].
This study aimed to evaluate the feasibility of monolithic zirconia laminate veneers in comparison to lithium disilicate laminate veneers. Our investigation involved an in vitro analysis focusing on vertical marginal discrepancy and load-to-failure. The null hypotheses posited that there would be no statistically significant differences between monolithic zirconia laminate veneers (MZLV) and lithium disilicate laminate veneers (LDLV) of different thicknesses regarding vertical marginal discrepancy and load-to-failure.
Materials and methods
Design and fabrication of laminate veneers
Three prefabricated acrylic teeth (Maxillary left central, Frasaco GmBh, Germany) were prepared using depth-gauge diamond burs to achieve depths of 0.5 mm, 0.7 mm, and 1.0 mm, respectively. To ensure a palatal butt joint, a 1.5 mm reduction was made from the incisal edge, and preparations were finalized with a chamfer finish line across all depths. Subsequently, the preparations were scanned using a desktop scanner (Freedom HD, DOF, Seoul, Korea), and 60 resin dies were produced using a 3D printer (NextDent 5100, 3D Systems, NextDent B.V., Soesterberg, The Netherlands).
A maxillary left central laminate veneer restoration was designed using computer-aided design software. The cement thickness was set at 40 μm [17], and the restoration thicknesses were adjusted to 0.5 mm, 0.7 mm, and 1 mm, with the restoration extending 1 mm above the cervical edge. Subsequently, laminate veneers were milled from pre-sintered monolithic zirconia (3rd generation, KATANA Zirconia STML Noritake Dental Supply Co., Ltd., Miyoshi, Japan) [18] and lithium disilicate blocks (IPS E-Max CAD, Ivoclar Vivadent, Shaan, Liechtenstein) using a 5-axis milling machine (Ceramill Motion 2, Amann Girrbach, Austria). Figure 1 represents a laminate veneer sample on the resin die.
Monolithic zirconia laminate veneers (MZLV) (A total of 30 zirconia laminate veneers, n = 10 in each thickness) were sintered in the sintering furnace according to the manufacturer’s instructions (6 h 42 min, 1530 °C) and manually polished after sintering (Luster Zirconia Adjusting and polishing kit, Meisinger, Germany).
Lithium disilicate laminate veneers (LDLV) (A total of 30 lithium disilicate laminate veneers, n = 10 in each thickness) were submitted to the specific crystallization cycle in a porcelain oven (Programat, Ivoclar Vivadent, Shaan, Liechtenstein) following the manufacturer’s instructions and then polished with rubber diamond points (ST102 HP, R1020HP, R1040HP. Edenta AG). The thicknesses of the veneers were controlled with a digital caliper (Digimatic Caliper IP67, Mitutoyo, Tokyo, Japan). The measurements were done 1 mm above the chamfer finish line.
Cementation protocols
The intaglio surface of the MZLV underwent air abrasion using 110 μm diameter silica-modified aluminum oxide particles (Rocatec Plus, 3 M ESPE) at a pressure of 0.2 MPa for 10 s by the same operator. Subsequently, the surface was treated with a primer (Clearfil Ceramic Primer Plus; Kuraray Noritake Dental) containing 3-trimethoxysilylpropyl methacrylate (3-TMSPMA) and 10-Methacryloyloxydecyl dihydrogen phosphate (10-MDP).
LDLV were etched with etchant gel (K-etchant gel, Kuraray Noritake Dental) for 20 s, rinsed, and dried. Subsequently, the surfaces of the laminate veneers were treated with the same agent (Ceramic Primer Plus, Kuraray Noritake Dental). A resin cement (Panavia V5 Clear, Kuraray Noritake Dental) was applied to each veneer, placed on its corresponding resin die, and seated with finger pressure for one minute. Then the excess cement was removed and restoration was light cured for 20 s from palatal and labial surfaces. The specimens were stored in distilled water for 24 h at 37 °C.
Measurement of vertical marginal discrepancy
The vertical marginal discrepancy was examined using a stereomicroscope (Olympus Model SZ61, Tokyo, Japan) at ×40 magnification (Fig. 2). The measurements were conducted by the same researcher, whereby the discrepancy between the resin dye and the laminate veneer restorations at four points (midpoints of mesial, distal, cervical, and palatal finish line) at the finish line was examined (Fig. 3). Three repetitive measurements were taken, and the mean value was recorded for this point value [19, 20].
Load-to-failure test and failure mode
A load-to-failure test was conducted using a universal testing machine (Instron, Canton, MA, USA). The load was applied perpendicular to the lingual surface of the resin die, positioned 1 mm away from the incisal edge of the laminate veneer (LV) restoration, at a cross-head speed of 0.5 mm/min. To ensure consistent test conditions, a mounting jig and custom-made plunger were employed. The load applied was recorded at the point of failure [21,22,23]. (Fig. 4)
The failure modes were then evaluated macroscopically on the fractured surfaces. The failure modes were: cohesive failure (laminate fracture), adhesive failure (debonding of laminate), mixed failure (adhesive and cohesive failure), and root fracture.
Statistical analysis
The minimum required sample size was determined by analysing previous research data using the Minitab Program (Minitab 22, Minitab LLC) [21]. To assess the differences in obtained data across the four study groups, we set a significance level (alpha-type error) of 0.05 and a statistical power (beta power) of 0.80. Based on these criteria, a minimum sample size of 10 samples per group was calculated.
The vertical marginal discrepancy and load-to-failure data were analysed using the IBM SPSS Statistics Standard Concurrent User V 26 (IBM Corp., Armonk, New York, USA) statistical package program. The conformity of numerical data to a normal distribution was assessed using the Shapiro-Wilk test, while the homogeneity of variances was evaluated using the Levene test. Comparisons between groups were conducted using a Two-Way Analysis of Variance. Bonferroni correction was applied to adjust for all pairwise comparisons. Statistical significance was defined as p < 0.05.
Results
Measurement of vertical marginal discrepancy
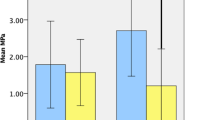
Table 1 displays the outcomes of the two-way ANOVA and Bonferroni test carried out on data regarding mesial, distal, cervical, palatal, and mean vertical marginal intervals. The results of the two-way ANOVA revealed significance in all regions except for the distal. Notably, the vertical marginal discrepancy of LDLV samples was significantly greater than that of MZLV samples across all thickness types, with particularly noteworthy differences observed in the cervical, palatal, and mean data (Fig. 5).
Load-to-failure test and failure mode results
Based on the results of the two-way ANOVA, a statistically significant difference was found in load-to-fracture values between MZLV and LDLV manufactured in all thicknesses (p < 0.001). (Table 2)
According to the Bonferroni test results, the load-to-fracture values for 0.5 mm, 0.7 mm, and 1.0 mm thicknesses are statistically similar within the MZLV group. In the LDLV group, the load-to-fracture values for 0.7 mm and 1.0 mm thicknesses are statistically similar. In contrast, the value for 0.5 mm thicknesses is statistically lower than those for 0.7 mm and 1.0 mm (p < 0.001). In the MZLV group, the load-to-fracture value is statistically lower than in the LDLV group for the 0.7 mm and 1.0 mm thickness groups; however, it is higher in the 0.5 mm group (p = 0.039).
The results of the failure modes are presented in Table 3. No cohesive fractures were detected in the MZLV samples. Adhesive failure was more prevalent in MZLV samples, occurring in 100% of the 1 mm thickness samples, 80% of the 0.7 mm thickness samples, and 70% of the 0.5 mm thickness samples. In LDLV samples, the type of failure was influenced by the material thickness. Cohesive fractures were more prevalent in 0.5 mm LDLV samples, whereas adhesive failure was observed in 1 mm LDLV samples. Figure 6 illustrates the failure modes observed in the samples from this study.
Discussion
Zirconia and lithium disilicate materials have gained increasing popularity for laminate veneer restorations due to their superior mechanical properties and ease of fabrication using CAD-CAM systems. The null hypothesis of this study posited that there would be no statistically significant differences in VMD and load-to-fracture between CAD-CAM MZLVs and LDLVs manufactured at different thicknesses. However, the study findings reveal a notable distinction in load-to-failure test outcomes between materials, with thickness exerting an influence on this parameter. Regarding VMD, although thickness appears to not affect marginal adaptation, the choice of material significantly influences this aspect. Consequently, the null hypothesis is only partially accepted.
The choice of the maxillary right central incisor was deliberate, as central incisors are among the most prominent teeth in the mouth, often raising significant aesthetic concerns addressed by clinicians [5, 24]. The restoration preparations followed the guidelines provided by manufacturers for veneers as 1.5 mm incisal reduction [21]. The study by Arora et al. [25] and Vaidya et al. [26] concluded based on the result of their studies that the butt joint is the most effective preparation for ceramic veneers if incisal coverage is desired. Consequently, in the present study, a palatal butt joint and labial chamfer finish lines were employed at specified depths. Replica-prepared central incisor teeth were obtained using a 3D printer to ensure standardization, mirroring the methodology employed in the studies conducted by Jurado et al. [5]
The adhesive resin is shielded against repeated exposure to oral fluids through a tight fit between the restorative margins and the tooth structure. This reduction minimizes the occurrence of progressive chemical, mechanical, and physical disintegration, which are known to lead to issues such as recurrent deterioration, microleakage, and the formation of stress concentrations [27, 28]. Ensuring a sufficient marginal fit in laminate veneers holds significant importance [29].
Baig et al. [16], in their systematic review and meta-analysis evaluating the marginal and internal fit of porcelain laminate veneers, included research findings suggesting that zirconia laminate veneers offer improved marginal fit compared to lithium disilicate veneers. The observed effect may be attributed to inherent disparities in the production methods. In the present study, both CAD-CAM materials were fabricated using a 5-axis milling machine, thus eliminating potential discrepancies arising from variations in production methods. In line with the outcomes reported in the studies referenced by Baig et al. [16], the VMD was significantly reduced in MZLVs compared to LDLVs in the present study.
Hasan et al. [15], in their study investigating the marginal chipping of machinable zirconia and lithium disilicate ceramic veneer restorations of various thicknesses (0.3 and 0.5 mm), observed that zirconia veneer restorations exhibited less chipping, resulting in a reduced VMD in comparison to lithium disilicate veneer restorations. Our study yielded similar findings.
The literature describes a broad spectrum of marginal opening values, influenced by factors such as the type of restoration and its location [30]. Baig et al. [31] reported the mean and standard deviation (SD) values of 66.4 (42.2) µm for zirconia and 36.6 (32.1) µm for lithium disilicate ceramic. In our study, the mean and the SD values were 27.95 ± 3.77, 31.77 ± 7.09, and 38.32 ± 8.90 for MZLV and 57.85 ± 13.19, 72.02 ± 8.18, 63.75 ± 12.45 for LDLV, respectively 1.0, 0.7 and 0.5 mm. More precisely, the maximum marginal discrepancy for CAD-CAM restorations has been reported to range between 40 and 90 μm in the literature [31,32,33]. As indicated by the results of the present study, although the average VMD value is greater in LDLVs compared to MZLVs, it remains within clinically acceptable limits for both materials.
To assess the load to failure of laminate veneers in vitro, various loading angles of 90° [24, 34, 35] and 135° [11] have been suggested. Similar to the study of Saker and Özcan [21], the veneers were positioned at a 90-degree angle to the long axis of the tooth structure to specifically evaluate the horizontal component of the load exerted on the palatal surface of maxillary incisors by mandibular incisors. Given that ceramic material is more susceptible to fracture under tensile loads, this investigation loaded the veneers at a 90-degree angle to the long axis of the tooth structure. This approach was intended to assess only the horizontal component of the load applied to the palatal surface of maxillary incisors by mandibular incisors. Additionally, this angle prevents the sliding of the Instron crosshead on the specimens’ palatal surface [22, 23].
Lawson et al. [36] found that the material type significantly influenced crown fracture load in their study, which compared the fracture load of lithium disilicate and zirconia crowns. The lower failure load of LDLV was anticipated due to their lower flexural strength compared to MZLV. Additionally, Yan et al. [37] reported that despite 5Y-Z material exhibiting a higher biaxial flexural strength than lithium disilicate, the fracture load of lithium disilicate bonded to a resin tooth die (18.6 GPa) exceeded that of 5Y-Z.
According to the load-to-failure test results, MZLV showed lower values (261.79 ± 42.21, 289.10 ± 28.70 N) than LDLV (336.22 ± 31.27, 339.89 ± 36.23 N) at thicknesses of 0.7 and 1.0 mm, while demonstrating higher values at a thickness of 0.5 mm (271.13 ± 38.18, 228.39 ± 76.54 N). While there was no significant difference in load-to-failure values between different thicknesses of MZLVs, LDLVs with a thickness of 0.5 mm exhibited significantly lower results than those with thicknesses of 0.7 mm and 1.0 mm. When comparing the materials, a notable difference in thickness is evident. Although LDLVs with thicknesses of 0.7 mm and 1.0 mm demonstrated higher load-to-failure values, LDLVs with a thickness of 0.5 mm exhibited a significantly smaller difference compared to MDLVs with the same thickness. This variance may be attributed to the increased occurrence of adhesive failure in MDLVs with thicknesses of 0.7 mm and 1.0 mm.
Previous studies [14, 38] have consistently demonstrated a decrease in load-to-failure values as the thickness of LDLVs decreases. The findings of the present study align closely with these established trends in the literature.
The failure mode was impacted by both the type of material and, as expected, the thickness of the material. According to the failure mode analysis in the present study, debonding is identified as the predominant cause of failure for zirconia restorations across all thicknesses, and for lithium disilicate laminate veneers at thicknesses of 0.7 and 1 mm. Conversely, laminate fractures become more prevalent in LDLV at a thickness of 0.5 mm.
A palatal butt-joint finish line was utilized in the present study and no instances of root fracture were observed in any of the materials or thicknesses examined. A meta-analysis of in vitro studies conducted by Da Costa et al. [39] concluded that while there was no statistical difference in ceramic fractures between both preparation types, the butt joint incisal preparation potentially offers greater advantages compared to the palatal chamfer in terms of ceramic fracture incidence and tooth fracture occurrence. The lack of root fracture can be attributed to the findings documented by Da Costa et al. [39].
The authors acknowledge the limitations of correlations between in vitro simulations of intraoral function. Specifically, the simulations conducted in this study did not incorporate thermal or mechanical load cycling. Nevertheless, the data obtained on failure mode and marginal adaptation provide valuable insights into the biomechanical properties of these dental materials. Further, in vivo studies are warranted to ascertain the longevity of zirconia veneers in the oral environment and to investigate their modes of failure.
Conclusions
The success of laminate veneer restorations is influenced by both the selection of materials and the thickness of the restoration. Across all thicknesses, the vertical marginal fit of MZLV is superior to that of LDLV. Additionally, LDLV demonstrates lower load-to-failure values compared to MZLV in samples with a thickness of only 0.5 mm, while the load-to-failure value is higher in LDLV than in MZLV for thicknesses of 0.7 mm and 1.0 mm. Furthermore, lamina fracture emerges as the most common failure mode in LDLV. Restoration fracture represents the catastrophic failure of laminate veneer restorations, necessitating restoration reproduction. While debonding is the most frequent failure in MZLV restorations, it should be noted that this failure does not lead to catastrophic consequences. Thus, addressing this failure is clinically more straightforward and cost-effective. Considering all these factors, including clinical parameters, MZLV restorations may be considered a viable alternative to LDLV restorations when opting for a thin laminate veneer restoration of 0.5 mm.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Ahrberg D, Lauer HC, Ahrberg M, Weigl P. Evaluation of fit and efficiency of CAD/CAM fabricated all-ceramic restorations based on direct and indirect digitalization: a double-blinded, randomized clinical trial. Clin Oral Investig. 2016;20(2):291–300.
Dickens N, Haider H, Lien W, Simecek J, Stahl J. Longitudinal analysis of CAD/CAM restoration incorporation rates into navy dentistry. MilMed. 2019;184(5–6):365–72.
Hasanzade M, Aminikhah M, Afrashtehfar KI, Alikhasi M. Marginaland internal adaptation of single crowns and fixed dental prostheses by using digital and conventional workflows: a systematic review and meta-analysis. J Prosthet Dent. 2021;126(3):360–8.
Hasanzade M, Shirani M, Afrashtehfar KI, Naseri P, Alikhasi M. Invivo and in vitro comparison of internal and marginal fit of digital and conventional impressions for full-coverage fixed restorations: a systematic review and meta-analysis. J Evid Based Dent Pract. 2019;19(3):236–54.
Jurado CA, Sadid-Zadeh R, Watanabe H, Robbins CE, Afrashtehfar KI, Fischer NG, Lee DJ. (2024). Effect of incisal preparation design on the fracture strength of monolithic zirconia‐reinforced lithium silicate laminate veneers. J Prosthodont, 2024;33(3), 281–287.
Spitznagel FA, Boldt J, Gierthmuehlen PC. CAD/CAM ceramic restorative materials for natural teeth. J Dent Res. 2018;97(10):1082–91.
Marchesi G, Camurri Piloni A, Nicolin V, Turco G, Di Lenarda R. Chairside CAD/CAM materials: current trends of clinical uses. Biology. 2021;10(11):1170.
Martins FV, Vasques WF, Fonseca EM. How the variations of the thickness in ceramic restorations of Lithium Disilicate and the Use of different photopolymerizers influence the degree of Conversion of the Resin cements: a systematic review and Meta-analysis. J Prosthodont. 2019;28(1):395–403.
Nawafleh N, Hatamleh M, Elshiyab S, Mack F. Lithium disilicate restorations fatigue testing parameters: a systematic review. J Prosthodont. 2016;25(2):116–26.
Beier US, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont. 2012;25(1):79–85.
Alghazzawi TF, Lemons J, Liu PR, Essig ME, Janowski GM. The failure load of CAD/CAM generated zirconia and glass-ceramic laminate veneers with different preparation designs. J Prosthet Dent. 2012;108(6):386–93.
Michailova M, Elsayed A, Fabel G, Edelhoff D, Zylla I, Stawarczyk B. Comparison between novel strength-gradient and color‐gradient multilayered zirconia using conventional and high‐speed sintering. J Mech Behav Biomed Mater. 2020;111:103977.
Zhang Y, Lawn B. Novel zirconia materials in dentistry. J Dent Res. 2018;97(2):140–7.
Malallah AD, Hasan NH. Thickness and yttria percentage influence the fracture resistance of laminate veneer zirconia restorations. Clin Exp Dent Res. 2022;8(6):1413–20.
Hasan NH, Malallah AD, Qasim MH. Marginal chipping factor in machinable zirconia and lithium disilicate ceramic veneer restorations. Int J Dent Mater. 2024;6(1):1–5.
Baig MR, Qasim SSB, Baskaradoss JK. Marginal and internal fit of porcelain laminate veneers: a systematic review and meta-analysis. J Prosthet Dent. 2024;131(1):13–24.
Ferrari M, Marucci A, Cagidiaco EF, Pontoriero DI, Fuzzi M. Sealing ability of New Translucent Zirconia crowns made with Digital Workflow and cemented with different types of cement. Int J Periodontics Restor Dent. 2021;41(5):703–10.
Čokić SM, Cóndor M, Vleugels J, Van Meerbeek B, Van Oosterwyck H, Inokoshi M, Zhang F. Mechanical properties–translucency–microstructure relationships in commercial monolayer and multilayer monolithic zirconia ceramics. Dent Mater. 2022;38(5):797–810.
Faul F, Erdfelder E, Lang AG, Buchner A. G* power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Refaie A, Fouda A, Bourauel C, Singer L. Marginal gap and internal fit of 3D printed versus milled monolithic zirconia crowns. BMC Oral Health. 2023;23(1):448.
Saker S, Özcan M. Marginal discrepancy and load to fracture of monolithic zirconia laminate veneers: the effect of preparation design and sintering protocol. Dent Mater J. 2021;40(2):331–8.
Tuğcu E, Vanlıoğlu B, Özkan YK, Aslan YU. Marginal adaptation and fracture resistance of lithium disilicate laminate veneers on teeth with different preparation depths. Int J Periodontics Restor Dent. 2018;38:87–95.
Kusaba K, Komine F, Honda J, Kubochi K, Matsumura H. Effect of preparation design on marginal and internal adaptation of translucent zirconia laminate veneers. Eur J Oral Sci. 2018;126:507–11.
Machado AW. 10 commandments of smile esthetics. Dent Press JOrthod. 2014;19(4):136–57.
Arora A, Upadhyaya V, Arora S, Jain P, Yadav A. Evaluation of fracture resistance of ceramic veneers with different preparation designs and loading conditions: an in vitro study. J Indian Prosthodont Soc. 2017;17(4):325–31.
Vaidya N, Rodrigues S, Hegde P, Shetty T, Pai U, Saldanha S. A comparative evaluation of the effect of different incisal preparations on the fracture resistance and fracture pattern of mandibular anterior porcelain laminate veneers using two different materials—an in vitro study. Indian J Forensic Med Toxicol. 2019;13(4):214–9.
Lin TM, Liu PR, Ramp LC, Essig ME, Givan DA, Pan YH. Fracture resistance and marginal discrepancy of porcelain laminate veneers influenced by preparation design and restorative material in vitro. J Dent. 2012;40(3):202–9.
Stappert CFJ, Ozden U, Att W, Gerds T, Strub JR. Marginal accuracy of press-ceramic veneers influenced by preparation design and fatigue. Am J Dent. 2007;20(6):380–4.
Thaj B, Joseph A, Ramanarayanan V, Singh P, Ravi AB, Krishnan V. Fracture resistance of two Preparation designs on Anterior Laminate veneers: a systematic review and Meta-analysis. World J Dent. 2022;13(6):666–76.
Kokubo Y, Ohkubo C, Tsumita M, Miyashita A, von Steyern V, Fukushima P. Clinical marginal and internal gaps of Procera AllCeram crowns. J Oral Rehabil. 2005;32(7):526–30.
Baig MR, Tan KB, Nicholls JI. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J Prosthet Dent. 2010;104(4):216–27.
Abduo J, Lyons K, Swain M. Fit of zirconia fixed partial denture: a systematic review. J Oral Rehabil. 2010;37(11):866–76.
Tinschert J, Natt G, Mautsch W, Spiekermann H, Anusavice KJ. Marginal fit of alumina-and zirconia-based fixed partial dentures produced by a CAD/CAM system. Oper Dent. 2001;26(4):367–74.
Castelnuovo J, Tjan AHL, Phillips K, et al. Fracture load and mode of failure of ceramic veneers with different preparations. J Prosthet Dent. 2000;83(2):171–80.
Schmidt KK, Chiayabutr Y, Phillips KM, et al. Influence of preparation design and existing condition of tooth structure on load to failure of ceramic laminate veneers. J Prosthet Dent. 2011;105(6):374–82.
Lawson NC, Jurado CA, Huang CT, Morris GP, Burgess JO, Liu PR, Givan DA. Effect of surface treatment and cement on fracture load of traditional zirconia (3Y), translucent zirconia (5Y), and lithium disilicate crowns. J Prosthodont. 2019;28(6):659–65.
Yan J, Kaizer MR, Zhang Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 2018;88:170–5.
André M, Kou W, Sjögren G, Sundh A. Effects of pretreatments and hydrothermal aging on biaxial flexural strength of lithium di-silicate and Mg-PSZ ceramics. J Dent. 2016;55:25–32.
da Costa DC, Coutinho M, de Sousa AS, Ennes JP. A meta-analysis of the most indicated preparation design for porcelain laminate veneers. J Adhes Dent. 2013;15(3):215–20.
Acknowledgements
The authors thank Prof Dr Ferhan Elmalı for statistical consultancy. This study was supported by the Scientific Research Projects Unit of Nuh Naci Yazgan University, Kayseri/Türkiye, grant no 2020-SA.DH-BP/11.
Funding
This study was supported by the Scientific Research Projects Unit of Nuh Naci Yazgan University, Kayseri/Türkiye, grant no 2020-SA.DH-BP/11.
Author information
Authors and Affiliations
Contributions
All of them contributed to the study’s conception and design. PY: Project administration, study design, drafting the manuscript conceiving the ideas, data analysis, and Writing – original draft, Conceptualization, DG: Methodology, investigation, data curation, data collection, supervision, conceptualization, HMA: Methodology, study design formal analysis, data curation, conceptualization.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.





Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yıldız, P., Güneş Ünlü, D. & Aydoğdu, H.M. Evaluation of vertical marginal discrepancy and load-to-failure of monolithic zirconia and lithium disilicate laminate veneers manufactured in different thicknesses. BMC Oral Health 24, 913 (2024). https://doi.org/10.1186/s12903-024-04685-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04685-w