Abstract
Background
This study aims to describe the Libyan oral health care system in terms of its structure, function, workforce, funding, reimbursement and target groups.
Methods
A single descriptive case study approach and multiple sources of data collection were used to provide an in-depth understanding of the Libyan oral health care system. A purposeful sample of the key informants (Managers of oral health centers, dentists of various specialties with experience in the field, dentists, nurses, dental technicians, and officials in the affairs of medical insurance) was recruited. The case and its boundaries were guided by the study’s aim. Both qualitative and quantitative analyses were conducted. Descriptive statistics were used for quantitative data. Framework analysis, informed by the study objectives, was used to analyze interviews and documents.
Results
The analysis showed that oral health services are integrated into medical services. The provision of dental care is mainly treatment-based, in the private sector. The oral health services in the public sector are mainly emergency care and exodontia. The dental workforce included in the study were mostly dentists (89% General Dental Practitioners (GDPs), 11% specialists), with a marked deficiency in dental technicians and nurses. Around 40% of dentists work in both the private and public sectors. The government provides the funding for the public sector, but the private sector is self-funded. No specific target group(s) nor clear policies were reported. However, the system is built around primary health care as an overarching policy. Dental caries is the most common oral problem among Libyan preschool children affecting around 70% and is the most common cause of tooth loss among adults.
Conclusion
The oral health care system in Libya is mainly privatized. The public health services are poorly organized and malfunctioning. There is an urgent need to develop policies and plans to improve the oral health care system in Libya.
Similar content being viewed by others
Introduction
A health care system is a complex organization whose primary goal is to promote, restore or maintain health. It includes all institutions, people and actions that work together to achieve its aim [1]. According to the World Health Organization (WHO), a health care system includes service delivery, health workforce, information, medical products, vaccines and technologies, financing, and leadership/governance [2]. Dentistry is only one component of the broader health care system. According to Gift and Andersen, any oral health care system can be described in terms of six aspects (Structure, Functions, Personnel, Funding, Reimbursement and Target population) which vary in their application in different countries [3]. In addition, health care systems are not static and influenced by many factors such as demographic changes, advances in technology, expectations and a country’s economic and political situation [4, 5]. Disparities in human and financial resources, dental workforce and the provision of health services between developed and developing countries are well documented [6]. It is, therefore, crucial for each country to regularly examine its health care system to ensure that it is taking account of population changes, health needs, workforce numbers, skills and expectations [7].
In recent years many countries have been affected by political, security, economic, and social challenges that have significant impact on health care services [8]. Libya is one of the Arab League countries that went through turmoil of political, armed and economic crises since February 2011 [9]. As a result, the Libyan health care system which was once a model of success for other developing countries, is negatively affected [10]. Although several conferences and workshops were organized by local and international agencies to assess and address the challenges facing the Libyan health care system [11], little attention has been given to oral health care which has its own challenges. For instance, there is an unprecedented increase in the number of graduating dentists at the expense of their quality [12]. Moreover, recently published studies highlighted highly unmet treatment needs among Libyan children and adults [13,14,15]. It is important to understand the dynamics of the oral health care system in Libya to inform future planning of oral health services. Therefore, the present study aims to describe the oral health care system in Libya according to the six aspects suggested by Gift and Andersen [3], which include Structure, Functions, Personnel, Funding, Reimbursement and Target population.
Methods
Study design
A single descriptive, exploratory case study design with a mix of qualitative and quantitative data collection tools was used to describe the Libyan oral health care system. This approach allows the triangulation of evidence from multiple sources and a comprehensive and detailed understanding of the studied phenomenon [16,17,18].
The case is defined as the oral health care system in Libya. The case boundaries were guided by the study research question and the aspects of the oral health care system according to Gift and Andersen [3] as follows: (1) Structure: how the system is structured; (2) Functions: what the system set out to achieve; (3) Personnel: who delivers the work; (4) Funding: where the funds are derived from; (5) Reimbursement: how workers are paid; (6) Target population: which groups are prioritized.
Setting
The study was conducted in Benghazi, the second-largest city in Libya, encompassing both urban and rural districts. Although Libya is one the largest countries in Africa, it has around seven million inhabitants mainly living in northern cities and most of them live in Tripoli and Benghazi. The city of Benghazi has the oldest dental school in Libya. The city of Benghazi has a full range of oral health care facilities and services and hence is considered a representative of the Libyan oral health care system.
Data collection
Three strands of data collection were carried out sequentially: (1) semi-structured qualitative interviews; (2) documentary analysis; and (3) a questionnaire survey. The data was collected from the chief staff working in the Ministry of Health (MoH), health insurance companies, administrative personnel, business owners, and service providers (dental practitioners and dental auxiliaries).
Qualitative interviews
Semi-structured interviews with a purposeful sample of the key informants (Managers of oral health centers and hospitals, dentists of various specialties with experience in the field, nurses, dental technicians, and officials in the affairs of medical insurance) were recruited for qualitative data collection. Chief staff of health care institutions and senior dental professionals were first identified by contacting the officials in the MoH and by consulting the senior staff in the dental school. The informants were invited to take part in the study. The aim of the study was explained and the informants were handed out study information sheets and a consent form. Another appointment was then decided to conduct the interview. A snowballing of the study sample was then applied to identify the potential key informants who were approached at their workplace.
The interviews were undertaken by the principal investigator (PI) who received special training in conducting interviews. All interviews were audio-recorded and took place in a quiet non-clinical room. The interviews were conducted using a topic guide based on the research question and the aspects of the oral health care system according to Gift and Andersen [3]. They started with an open question: How do you describe the oral health care system in Libya? The data collection continued until no new information was obtained which is known as saturation [16].
Document analysis
Documentary analysis was conducted to examine the relevant reports, policies, service documents, and academic publications. All accessible electronic and paper reports at local and national levels were included. While studies published in the last ten years were only included to obtain current health status information, searching policies and other reports were not limited to a specific time. Relevant documents were identified through searches in electronic databases like PubMed and Google Scholar, as well as governmental websites. Additionally, grey literature was sourced by reaching out to key individuals in academic and healthcare institutions [16].
Questionnaire survey
A self-administered, paper-based questionnaire survey was conducted among dentists in Benghazi. A purposeful sample approach was adopted to recruit participants who were selected in a way that ensures including a range of dentists who represent various oral health care settings and facilities and years of experience to reflect the range of dental care provided in the city. Therefore, the dental facilities were the sampling units. In each dental facility, dentists were approached personally and invited to take part in the survey. The questionnaire was designed by the research team and the questions revolved around the six components of the oral health care system and were informed by the findings of qualitative analysis. The questionnaire was pre-tested for clarity and understandability among a group of 10 dentists. Most of the feedback received was related to question wording, which was modified accordingly. The final questionnaire comprised of sixteen questions. These were five open-ended questions and eleven close-ended questions (Yes/No and multiple-choice, eight of them have an open option). Due to the exploratory nature of the study, a free text response section was included at the end of each structured question, allowing participants to add any additional comments. The final questionnaire had 6 sections representing the components of the oral health care system and an introductory section collecting professional and socio-demographic characteristics of the participants. The questionnaire took on average 15 min to be completed.
The PI handed the questionnaire to the dentists in their work setting and explained the aim of the study. The PI was available (via phone) to clarify any issue related to the study and the questionnaire. The questionnaires were collected within a week from the reception desk. The consent to take part in the study was implicit by returning a completed questionnaire.
Data analysis
The quantitative and qualitative analyses were conducted separately and then integrated into one framework comprised of the pre-defined six components of the oral health care system.
Qualitative data
A framework analysis approach was performed to analyze the qualitative interviews and retrieved documents according to the six components of oral health care system [17, 19]. The analysis process started with initial familiarization through listening to the audiotapes, reading and re-reading of interviews transcribed verbatim to gain an overview of ranges and diversities of the gathered material. The analysis was conducted concurrently with data collection and emerging codes and sub-themes were explored in the subsequent interviews. Only data that showed relevance to research questions were coded. Finally, the coded data were organized into overarching six themes representing the components of the oral health care system. A discussion among the research team was held to remove unsupported themes, create new themes, reduce homogenous themes together, and split heterogeneous ones Then data extracts were selected to be presented in the research context. The validity of the analysis has been achieved with the participation of an experienced researcher other than the principal investigator in the analysis. In addition, a third person from outside the dental field was involved in confirming that the extracts are representative to the themes emerged from the analysis.
Quantitative data
Descriptive quantitative analysis was undertaken to summarize the distribution of study sample characteristics. The answers to free-text questions were analyzed using a qualitative content analysis strategy, which involved categorization of the answers [20].
Results
Characteristics of study samples
Twelve qualitative interviews were conducted. The interviewees were dentists working in different sectors and facilities (5), chief staff, university and health insurance (3), dental nurses (2), and dental technicians (2) (appendix 2). In the questionnaire survey, a total of 121 out of 150 questionnaires were received with complete information, suitable for data analysis, giving a response rate of 80.6%. The participants aged between 23 and 63 years of age, and almost three-quarters of them were females (89, 73.6%), The majority of the participants were GDPs (108, 89.3%), and held only Bachelor of Dental Surgery (BDS). The participants worked in the public sector, private sector and both sectors were, respectively, 33.9%, 26.4%, and 39.7%. (Table 1)
Components of the Libyan oral health care system
Structure: how the system is structured?
The Libyan oral health care system is a hybrid system comprised of public and private sectors. Dental services were provided in medical polyclinics/hospitals or through a standalone dental facility (Table 2).
Dental care in the public sector is mainly run by MoH. However, non-MoH facilities also provide dental services such as that affiliated to educational institutions for training purposes or other health service facilities affiliated to the ministries of defense, justice and social services.
Informant (5): “Not all health institutions are affiliated with the Ministry of Health; dental services are also provided by other facilities that do not belong to MoH. These can be classified as educational which includes teaching hospitals and training centers, and service-oriented such as ministries of defense and interior and social care institutions”.
Dental services are generally integrated within health care facilities providing medical services. However, this is not always the case and there are separate dental facilities that exclusively provide dental care, such as the Specialized Dental Center and dental schools. Exclusively dental care facilities are mainly in the private sector taking the form of solo or multiple units’ dental practices and private dental schools’ clinics Interestingly, only three out of the six dental schools have their own private dental clinics for training and providing dental services. The other three schools are newly established and do not yet have dental clinics. Yet, private medical polyclinics and hospitals including dental units provide dental care.
Informant (1): “There are dental services that are provided in private clinics and private hospitals through departments in these clinics and hospitals, and some dental services are provided as a part of the dental training courses for dental students at universities or private institutes”.
Informant (4): “In the private sector, dental clinics are mostly found as multi-chair centers, 5 dental chairs or more, but also there are places with one or two chairs”.
The MoH has a two-level administrative hierarchy (Fig. 1). The national level is expected to offer secondary and tertiary care level. Facilities at the national level are under the direct supervision of the MoH and include general, central and specialized hospitals, rural hospitals, including the Specialized Dental Center.
Informant (4): “The Specialized Dental Center is the only institution that is directly affiliated to the Ministry of Health and funded by the Ministry directly”.
The local level is organized into Regional Health Service Administration that is responsible for health units, centers, polyclinics, and primary health care facilities.
Dental services are distributed throughout health care facilities at both local and national levels. However, the integration of dental care into medical service did not mean providing the same primary, secondary and tertiary care. Instead, general dental services with unclear distinctions between care levels are provided. Any type of dental care can be provided in any health facility depending on the availability of resources.
Informant (5): “No we are not aware of primary, secondary, or tertiary services in dentistry. All services are provided according to availability. In Aljala trauma hospital we treat maxillofacial trauma and injuries but also there is a dental unit to provide dental care such as simple filling and extraction though not always available because of shortage of LA or dental materials”.
Function: what does the system set out to achieve?
The available policy documents indicate that the Libyan health care system adopts a primary health care preventive services policy and provides emergency dental care to all people but this was not the case on the ground.
Informant (7): “The services required from the public sector are supposed to be all services related to pain removal, whether with or without treatment, but in reality, the state is currently unable to provide these services. It only provides services such as examination and simple extraction, due to the lack of capabilities”.
The dental services were treatment-oriented and mainly provided in the private sector (Table 3). Preventive dental services and primary health care services are rarely provided and are limited to volunteer activities by some non-governmental organizations and educational institutions as part of their training.
Informant (1): “In the past, the school programs and primary health care services provided along with mother and child services were active, but now none of this exists. It is only the building and a small staff without any activities”.
Informant (6): “Most oral health education campaigns are performed by scientific groups such as community and pediatric associations and internship students with support from toothpaste companies”.
In the private sector, a whole range of dental services is available. Private dental centers were well-equipped with dental facilities and experienced staff. On the other hand, the dental services provided in the public sector were limited to diagnostic services and exodontia. An exception to this is the Specialized Dental Center which offers a range of services such as restorative dentistry, minor oral surgery, periodontics and removable prosthodontics.
Informant (2): “The only place in the public sector that provides all dental services is the Specialized Dental Center”.
Informant (4): “Private dental centers are well-equipped with dental facilities; the whole range of dental services are provided in this sector”.
The analysis of published studies indicates that there are highly unmet treatment needs among Libyan children and adults. More than 40% of Libyan children had untreated dental caries in their primary and permanent teeth (Table 4). In addition, Untreated caries and severe periodontitis are the most common reasons for tooth loss among Libyan adults [21, 22].
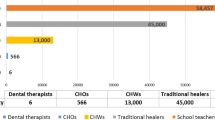
Personnel: who delivers the work
The dental workforce in the Libyan health care system is comprised of dentists, dental nurses, and dental technicians. The number of dentists has increased markedly in the last 10 years (Fig. 2 shows the rising number of dental graduates in one dental school) following the increased admission of new dental students in the only government dental school at the University of Benghazi. In addition, Benghazi hosts six private dental schools. One of these schools has graduated approximately 340 dentists over the past decade, with a recent increase in new student enrollment. Two of the schools have students in their final year of study, while the remaining three are newly established.
Informant (3): “The increase in the number of private universities, which are 6 universities, made the situation worse and caused overcrowding of dental graduates”.
Informant (4): “There is no control over the numbers of dental students despite the attempts to restrict the inclusion rate and the result is that there are large numbers of dentists and most of them are jobless”.
Most dentists work as general dental practitioners, with shortage in numbers of specialists in orthodontics and maxillofacial surgery.
Informant (6): “At the level of Benghazi, there is a big shortage of dental specialists in Orthodontics and Maxillofacial surgery”.
Other dental care personnel in the Libyan oral health care system includes dental laboratory technicians and dental nurses. None of them are allowed to work on dental patients. There is a clear shortage in the numbers of qualified dental nurses.
Informant (4): “Throughout my career as a dentist, I met a few officially trained dental nurses. Most of nurses worked for me are either medical nurses, dental hygienist or I trained them to be dental assistant.”
In recent years, dental hygienists have emerged as a new dental care personnel category. Dental hygienists are dental auxiliaries who are trained to provide preventive dental care and oral prophylaxis, unlike dental nurses who are not allowed to provide any type of dental care. However, the Libyan health care system does not recognize them as a specialty and hence they left without jobs in the public sector and many of them work as nurses in private practices.
Informant (3): “I graduated from the Higher Institute of Medical Professions as a dental hygienist but in reality, our profession is not recognized in Libyan law, and legally it is forbidden for anyone except the dentists to work on the patients. Therefore, most of us were left without jobs or worked as dental nurses in the private clinics, if they are lucky”.
Funding: where the funds are derived from
The public dental services are funded by the government through the National Bureau of Medical Supplies. The Libyan health services including dental care, are provided free of charge. The public oral health care system in Libya relies heavily on the state’s general budget, allocating approximately 4% of Libya’s Gross Domestic Product to health care [28]. In addition, national-level facilities receive a separate fund to purchase required equipment and consumables, but in recent years dental services have been less prioritized and many non-governmental organizations and companies provided dental supplies as informal support.
Informant (5): “The Libyan public health sector is funded by the Ministry of finance and operated through the medical supply unit and offers all dental materials and equipment”.
Informant (6): “In recent years, the resources are very scarce and most dental supplies are offered as support from private organizations and companies”.
The private sector is self-funded. The patients usually pay fees for service or through one of the insurance schemes offered by some companies such as oil companies and banks to the employees and their families. The insurance schemes usually cover diagnostic and treatment services but do not include prosthodontic and orthodontic treatment.
Informant (5): “In private, financing is done through the fees paid by patients and insurance companies”.
Reimbursement: how workers are paid
The reimbursement in the Libyan oral health care system includes salaries and a proportion of income. Fixed salaries are provided to those who work in the public sectors and dental auxiliaries in the private sector. Most dentists working in the private sector are reimbursed by the pre-agreed proportion of their income.
Informant (5): “All dental workers in the public sector and dental nurses in the private sector receive a fixed salary”.
Informant (7): “The reimbursement in the private sector varies according to the agreement between the employer and the dentist or dental technicians. It is usually a pre-agreed percentage of the income incurred by the dentist and often ranges between 30% and 70%, depending on the years of experience and qualifications”.
Target population: prioritized groups
There are no specified target groups in the Libyan oral health care system. The private sector provides care on demand to anyone seeking dental services, while the public sector operates on the principle of health for all. Consequently, all groups are targeted at their point of entry into the system. For instance, psychiatric patients receive care at the psychiatry hospital, which includes a dental unit. Similarly, other groups with special needs, such as the mentally disabled, diabetics, and the elderly, are also targeted.
Informant (4): “There are no places that have priorities. Dental services are distributed through all medical facilities, such as centers for communicable diseases, diabetes, mental illnesses, and the disabled, and large hospitals”.
Discussion
The present exploratory case study set out to describe the Libyan oral health care system in terms of its structure, function, personnel, funding, reimbursement and target groups. The Libyan oral health care system, like many other countries [5, 29, 30] is generally comprised of the public sector and a pre-dominating private sector. However, the privatization of the Libyan oral health care system appeared to be the result of the chaotic nature of the public dental services which were managed by multiple bodies (MoH and Non-MoH), integrated into the medical services and mostly limited to routine oral examinations and simple extraction with scarcity of resources.
The public dental services in Libya were poorly functioning which might be attributed to the low priority given to dental care in the light of limited funding and increased health care demands; evoked by the ongoing political and armed conflict in the country since the 2011 uprisings [31]. Although the health care policy in Libya promotes equal and free access to health services, it has not been implemented appropriately. Therefore, there is a need for dental services reform to embrace the primary health care approach and ensure universal access to care [32]. There are many initiatives in the region already in place that enhance the accessibility of dental care, such as including dental services in the national health insurance program [33, 34]. Moreover, establishing a separated administrative body for dental services, as is the case in Saudia Arabia, can ensure the appropriate allocation of resources and support of oral health research and promotion intatives [35].
The private sector, on the other hand, is self-funded and independently regulated. As a result, the provision of dental care is thriving and subject to quality-based competition. In addition, fixed salary is the only reimbursement method in the public sector which could have negatively affected the staff’s motivation and the type and quality of services provided as indicated in other research [36]. On the other hand, reimbursement in the private sector is linked to the type of services provided and the income generated, which appears to be a motivating factor for delivering high-quality and varied dental care. Additionally, financial factors have been identified by Libyan dentists as a significant barrier to providing preventive dental services [37].
An important aspect explored in the current study was the Libyan dental workforce. It was found that the dental care personnel in Libya include mainly dentists, dental nurses, dental technicians, and dental hygienists. Anecdotal evidence suggests that the number of dental graduates and dental schools is increasing in other parts of Libya. It is estimated that the dentist-population ratio in Libya is approximately 8.8 per 10,000 individuals, which exceeds the recommended global ratio and is higher than that observed in other countries in the region [38,39,40,41,42,43].
The high influx of Libyan dentists who graduated with questionable quality and limited job opportunities is attributed to the lack of coordination between health and education authorities which resulted in large numbers of dental students beyond the capacity of the low-resourced governmental dental schools and establishment of large number of private dental schools [12].
On the other hand, there is a clear deficiency in the number of qualified dental nurses. This may partly be explained by the absence of an official dental nursing training program in any Libyan educational institution over the past two decades. Alternately, there was a program for dental hygienists, but it is not a recognized profession in Libya. Consequently, graduated dental hygienists were not allowed to work in the public sector and many of them work in the private sector as dental nurses. Taken together, these observations highlight both quality and planning problems related to the Libyan dental workforce and the provision of dental care which require urgent interventions at the national level to control the dental education and training sector.
Unlike many developed countries that have established initiatives to target special groups such as elderly people, pregnant women, and low-income families [44,45,46], there are no specific target groups in the Libyan oral health care system. This may be attributed to the fact that the Libyan health care system was originally built on the idea of integrating primary oral health services at multiple points of entry for the entire population. However, targeting special groups requires the establishment of dental data infrastructure and surveillance data to guide these efforts.
This study has some limitations worth discussing. First, the study was conducted in the city of Benghazi as a representative of the whole country. There could be small differences in the numbers and distribution of dental facilities, such as private dental schools, which are concentrated in Benghazi and Tripoli. However, the Libyan health care system is centrally organized, and anecdotal evidence indicates similar elements of the health care system across the country. Additionally, the use of semi-structured interviews may be influenced by the personal thoughts and ideas of the interviewees, and it can be time-consuming. Furthermore, the documentary analysis might be limited by the availability of documents online and other grey materials. However, the researcher expanded the search beyond online resources and contacted key informants in health care facilities to ensure covering as many resources as possible.
Conclusions
The oral health care system in Libya is comprised of general and private sectors, although it is mainly privatized. The public dental services are poorly functioning, with highly unmet treatment needs, inappropriate implementation of primary health care policies, and uncontrolled production of the dental workforce. There is an urgent need to develop policies and plans to improve the oral health care system in Libya, involving both health and education parties. Establishing a separate administrative body for oral health services and reorienting oral health programs to meet the needs of underprivileged populations, such as children and elderly people, is highly recommended. Supporting dental schools to admit smaller numbers of dental students and provide appropriate training can enhance the quality of the dental workforce, increase the availability of dental services, and enable better control of the emerging workforce. Fostering collaboration between health and educational providers is of paramount importance for an appropriately functioning oral health care system.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BDS:
-
Bachelor of Dental Surgery
- PhD:
-
Doctor of Philosophy
- GDP:
-
General Dental Practitioners
- MSc:
-
Master of Science
- MoH:
-
Ministry of Health
- PI:
-
Principal investigator
- WHO:
-
World Health Organization
References
World Health Organization. Everybody’s business - strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: WHO; 2007.
Mounier-Jack S, Griffiths UK, Closser S, Burchett H, Marchal B. Measuring the health systems impact of disease control programmes: a critical reflection on the WHO building blocks framework. BMC Public Health. 2014;14:278.
Gift HC, Andersen RM. The principles of organisation and models of delivery of oral health care. In: Pine C, Harris R, editors. Community oral health. 2nd ed. New Malden: Quintessence Publishing; 2007. pp. 423–54.
Arah OA, Klazinga NS, Delnoij DM, ten Asbroek AH, Custers T. Conceptual frameworks for health systems performance: a quest for effectiveness, quality, and improvement. Int J Qual Health care: Int J Qual Health Care. 2003;15:377–98.
Widström E, Eaton KA. Oral healthcare systems in the extended European union. Oral Health Prev Dent. 2004;2(3):155–94.
Kandelman D, Arpin S, Baez RJ, Baehni PC, Petersen PE. Oral health care systems in developing and developed countries. Periodontol 2000. 2012;60:98–109.
Gallagher JE, Wilson NHF. The future dental workforce? Br Dent J. 2009;206:195–9.
Woodward A, Sondorp E, Witter S, Martineau T. Health systems research in fragile and conflict-affected states: a research agenda-setting exercise. Health Res Policy Syst. 2016;14:1–4.
Kruk ME, Freedman LP, Anglin GA, Waldman RJ. Rebuilding health systems to improve health and promote statebuilding in post-conflict countries: a theoretical framework and research agenda. Soc sci med. 2010;70:89–97.
Sullivan R, McQuinn B, Purushotham A. How are we going to rebuild public health in Libya? J R Soc Med. 2011;104:490–2.
El Oakley RM, Ghrew MH, Aboutwerat AA, Alageli NA, Neami KA, Kerwat RM, et al. Consultation on the Libyan health systems: towards patient-centred services. Libyan J Med. 2013;8:20233.
Arhoma N, Arheiam A. The dental workforce in Libya: an overlooked research topic. Libyan J Dent. 2022;6:1–3.
Arheiam A, Aloshiby A, Gaber A, Fakron S. Dental Fluorosis and its Associated factors amongst Libyan schoolchildren. Int Dent J. 2022;72:853–8.
Arheiam AA, Elareibi I, Elatrash A, Baker SR. Prevalence and factors associated with traumatic dental injuries among schoolchildren in war-torn Libya. Dent Traumatol. 2020;36:185–91.
Arheiam AA, Harris RV, Baker SR. Changes in dental caries and sugar intake before and during the conflict in Libya: a natural experiment. Community Dent Oral Epidemiol. 2020;48:201–7.
Baxter P, Jack S. Qualitative case study methodology: study design and implementation for novice researchers. Qualitative Rep. 2008;13:544–59.
Yin RK. Case study research: design and methods. Thousand Oaks Calif : SAGE Publictions. 2014;5th ed:2014.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med res Methodol. 2011;11:100–8.
Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative research practice: a guide for social science students. and researchers: sage; 2013.
Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14.
Elzer A, Ensir H, Elsalhi A, Kablan R, Jedeh M, Elramli A, et al. Reasons for tooth extraction among Libyan Adults: Multi-center Cross-sectional Study. Libyan J Dent. 2021;5:109–19.
Byahatti SM, Ingafou MS. Reasons for extraction in a group of Libyan patients. Int dent J. 2011;61(4):199–203.
Arheiam A, Omar S. Dental caries experience and periodontal treatment needs of 10- to 15-year old children with type 1 diabetes mellitus. Int Dent J. 2014;64:150–4.
Ballo L, Arheiam A, Marhazlinda J. Determinants of caries experience and the impact on the OHRQOL of 6-year-old Libyan children: a cross-sectional survey. BMC Oral Health. 2021;21:1–9.
Elrefadi R, Beaayou H, Herwis K, Musrati A. Oral health status in individuals with Down syndrome. Libyan J Med. 2022;17:2116794.
Aoun E, Ballo L, Elhabony S, Arheiam A. Association between dental caries and obesity among Libyan schoolchildren during the armed conflict in Benghazi. BMC Oral Health. 2023;23:1–8.
Fakroon S, Arheiam A, Omar S. Dental caries experience and periodontal treatment needs of children with autistic spectrum disorder. Eur Arc Paediatr Dent. 2015;16:205–9.
Peeran SW, Altaher OB, Peeran SA, Alsaid FM, Mugrabi MH, Ahmed AM, Grain A. Oral health in Libya: addressing the future challenges. Libyan J Med. 2014;9(1).
Kronfol N. Delivery of health services in arab countries: a review. East Mediterr Health J. 2012;18:1229–38.
Bravo M, San Martín L, Casals E, Eaton KA, Widström E. The healthcare system and the provision of oral healthcare in European Union member states. Part 2: Spain. Br Dent J. 2015;219:547–51.
Munezero E, Manoukian S. The social determinants of health and health seeking behaviour in populations affected by armed conflict: a qualitative systematic review. Med Confl Surviv. 2021;37:293–318.
Prasad M, Manjunath C, Murthy AK, Sampath A, Jaiswal S, Mohapatra A. Integration of oral health into primary health care: a systematic review. J Family med prim care. 2019;8:1838–45.
Koornneef EJ, Robben PB, Seiari A, M. B., Siksek A, Z. (, Amsterdam. Netherlands), 108(2–3), 115–21.
Fasseeh A, ElEzbawy B, Adly W, ElShahawy R, George M, Abaza S, ElShalakani A, Kaló Z. Healthcare financing in Egypt: a systematic literature review. J Egypt Public Health Assoc. 2022;97(1):1.
Almajed OS, Aljouie A, Alghamdi R, Alabdulwahab FN, Laheq MT. Transforming dental care in Saudi Arabia: challenges and opportunities. Cureus. 2024;16(2).
Dougherty S, Lorenzoni L, Marino A, Murtin F. The impact of decentralisation on the performance of health care systems: a non-linear relationship. Eur J Health Econ. 2022;23:705–15.
Arheiam A, Masoud I, Bernabé E. Perceived barriers to preventive dental care among Libyan dentists. Libyan J Med. 2014;9(1).
AlBaker AM, Al-Ruthia YSH, AlShehri M, Alshuwairikh S. The characteristics and distribution of dentist workforce in Saudi Arabia: a descriptive cross-sectional study. Saudi Pharma J. 2017;25:1208–16.
El Tantawi M, Aly NM, Attia D, Abdelrahman H, Mehaina M. Dentist availability in Egypt: a 20-year study of supply, potential demand and economic factors. East Mediterr Health J. 2020;26:1078–86.
Zouag N, Driouchi A. Trends and prospects of the Moroccan Health System: 2010–2030. Labor and Health Economics in the Mediterranean Region: Migration and mobility of medical doctors. IGI Global; 2014. pp. 314–36.
Halappa M, B HN, Kumar S, Sreenivasa H. SWOT Analysis of Dental Health Workforce in India: A Dental alarm. J clin Diagn res: JCDR. 2014;8:3–5.
Huang CS, Cher T-L, Lin C-P, Wu K-M. Projection of the dental workforce from 2011 to 2020, based on the actual workload of 6762 dentists in 2010 in Taiwan. J Formos. 2013;112:527–36.
World Health Statistics. 2022 Monitoring health for the SDGs Sustainable Development Goals [Internet]. https://cdn.who.int/media/docs/default-source/gho-documents/world-health-statistic-reports/worldhealthstatistics_2022.pdf
Johnston B, Thomas S, Burke S. Can people afford to pay for health care? New evidence on financial protection in Ireland [Internet]. iris.who.int. World Health Organization. Regional Office for Europe; 2020 [cited 2024 Feb 11]. https://iris.who.int/handle/10665/332978
Ziller S, Eaton K, Widström E. The healthcare system and the provision of oral healthcare in European Union member states. Part 1: Germany. Br Dent J. 2015;218:239–44.
Bravo M, Martín LS, Casals E, Eaton K, Widström E. The healthcare system and the provision of oral healthcare in European Union member states. Part 2: Spain. Br Dent J. 2015;219:547–51.
Bowen GA. Document analysis as a qualitative research method. Qual res J 22009;9:27–40.
Acknowledgements
Not applicable.
Funding
The authors declare that there was no external funding or financial support for this research.
Author information
Authors and Affiliations
Contributions
AAl conceived the ideas, collected the data, analyzed the data and wrote an initial draft of the manuscript, AA conceived the ideas, participated in data analysis and led the writing; AG Participated in writing and final editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for this study was obtained from the Research Ethics Committee at the Faculty of Dentistry, University of Benghazi (#060).
Consent to participate
All participants provided informed consent prior to their involvement in the study. They were informed about the aim of the research, the procedures involved, potential benefits and confidentiality measures.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Aloshaiby, A., Gaber, A. & Arheiam, A. The oral health care system in Libya: a case study. BMC Oral Health 24, 888 (2024). https://doi.org/10.1186/s12903-024-04684-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04684-x