Abstract
Background
Auriculocondylar syndrome (ARCND) is an extremely rare autosomal dominant or recessive condition that typically manifests as question mark ears (QMEs), mandibular condyle hypoplasia, and micrognathia. Severe dental and maxillofacial malformations present considerable challenges in patients’ lives and clinical treatment. Currently, only a few ARCND cases have been reported worldwide, but most of them are related to genetic mutations, clinical symptoms, and ear correction; there are few reports concerning the treatment of dentofacial deformities.
Case presentation
Here, we report a rare case of ARCND in a Chinese family. A novel insertional mutation in the guanine nucleotide-binding protein alpha-inhibiting activity polypeptide 3 (GNAI3) was identified in the patient and their brother using whole-exome sequencing. After a multidisciplinary consultation and examination, sequential orthodontic treatment and craniofacial surgery, including distraction osteogenesis and orthognathic surgery, were performed using three-dimensional (3D) digital technology to treat the patient’s dentofacial deformity. A good prognosis was achieved at the 5-year follow-up, and the patient returned to normal life.
Conclusions
ARCND is a monogenic and rare condition that can be diagnosed based on its clinical triad of core features. Molecular diagnosis plays a crucial role in the diagnosis of patients with inconspicuous clinical features. We present a novel insertion variation in GNAI3, which was identified in exon 2 of chromosome 110116384 in a Chinese family. Sequential therapy with preoperative orthodontic treatment combined with distraction osteogenesis and orthognathic surgery guided by 3D digital technology may be a practical and effective method for treating ARCND.
Similar content being viewed by others
Background
Auriculocondylar syndrome (ARCND; OMIM #602,483, #614,669, and #615,706) is an extremely rare autosomal dominant or recessive condition with a prevalence of less than 1 in 1,000,000 [1]. The typical triad manifestations of ARCND include question mark ears (QMEs), mandibular condyle hypoplasia, and micrognathia [2]. Other facial abnormalities [3] in the hearing [4], respiratory [5], digestive [6], reproductive [7], and even developmental [5] systems have also been reported. However, differences in gene expression have led to a wide range of differences in the clinical phenotypes between individuals and their families [6]. In addition, ARCND can be misdiagnosed as other diseases, including craniomaxillofacial deformities such as the oculo-auriculo-vertebral spectrum [7], Treacher Collins syndrome [8], mandibulofacial dysostosis [8], Guion-Almeida type, and Meier-Gorlin syndrome [9]. Ultimately, the varied individual clinical characteristics and extremely low incidence of ARCND contribute to the limited clinical knowledge of this condition.
Currently, fewer than 100 cases of ARCND have been reported in the literature [10]. However, most of them are related to genetic mutations, clinical symptoms, and ear correction in this disease, whereas correction of dentofacial deformities has rarely been reported [5, 11]. Therefore, clinicians must summarize individual clinical manifestations and report on feasible and effective clinical treatments. In this paper, we present the case of a Chinese patient with ARCND and the clinical features of her family member. A novel insertional mutation in the guanine nucleotide-binding protein alpha-inhibiting activity polypeptide 3 (GNAI3) was identified using whole-exome sequencing. Additionally, we performed sequential orthodontic treatment and craniofacial surgery, including distraction osteogenesis and orthognathic surgery, with the aid of digital technology, to treat the patient. A good prognosis was achieved, and the patient was satisfied with the treatment. Through this case report, we hope to improve our understanding of the genetic pathogenesis of ARCND and provide an effective clinical treatment for dentofacial malformations.
Case presentation
A 23-year-old woman was admitted to our hospital with severe mandibular malformations and poor occlusion, accompanied by severe sleep snoring for more than 20 years. With increasing age, the deformity became increasingly severe. Physical examination of the patient revealed facial asymmetry, a round face with prominent cheeks (more pronounced on the right), retrognathia, and mandibular hypoplasia, presenting as a typical "beak deformity" (Fig. 1a-c). Computed tomography (CT) of the skull revealed marked hypoplasia of the mandibular body, rami, and both condyles (Fig. 1d-f). The bilateral parotid glands were small and ectopic towards the front edge of the masseter muscle (red dashed lines in Fig. 1g).
Phenotypic presentation of the patient. a-c The side view of the face showing micrognathia, full cheeks, and round face shape. d-f Three-dimensional (3D) reconstruction of computed tomography (CT) data indicating micrognathia, bony prominence of the mandibular rami, and mandibular condyle hypoplasia. g The red dashed lines indicate a heterotopic parotid gland. h–l Patient’s intraoral view showing deep the overbite and overjet of anterior teeth, disordered tooth, and crowded dental arch. m The panoramic radiograph shows severe malocclusion
Intraoral examination revealed crowded teeth, malocclusion, and malalignment. The patient presented with an approximate Class I molar relationship, overbite, and overjet in the anterior teeth and a left-sided posterior crossbite (Fig. 1h-m). The interincisal distance was 30 mm, indicating limited mouth opening, but there was no clicking sound or tenderness in the area of bilateral temporomandibular joints (TMJs). No distinct cleft or notching between the lobe and helix was observed, and the morphology and function of the middle and inner ears were normal.
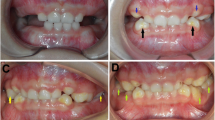
Polysomnography revealed an apnea–hypopnea index of 10.8, indicating low-grade obstructive sleep apnea syndrome (OSAS) and moderate hypoxemia. The patient’s physical and mental development was normal, and she had no speech or learning problems. Assessment of the family history revealed that her younger brother had similar symptoms (Fig. 2), whereas the proband was healthy and did not exhibit any facial abnormalities. Whole-exome sequencing revealed that the patient and their younger brother harbored a novel insertional mutation in GNAI3 (Table 1). Three-dimensional (3D) molecular structure prediction of the protein and disruption of hydrogen bonds are shown in Fig. 3.
Phenotypic presentation of the patient’s younger brother. a-c The side view of the face showing similar micrognathia, full cheeks, and a round face shape. d-f Three-dimensional (3D) reconstruction of computed tomography (CT) data indicating micrognathia, bony ridge protruding on the mandibular rami, and mandibular condyle hypoplasia. g The red dashed lines indicate a heterotopic parotid gland. h–l Intraoral photographs showing the deep overbite and overjet of anterior teeth, disordered tooth and crowded dental arch. m The panoramic radiograph shows severe malocclusion
The GNAI3 mutation contributed to the disruption of the hydrogen bond between serine 342 and glutamic acid 344. a Evaluation of amino acid conservation using Ugene. The serine indicated in the red box is highly conserved across various species. b, c Visualizing the three-dimensional (3D) molecular structure of protein–ligand using SWISS-MODEL. An overview of the wild-type (b) and mutant type (c), showing the disrupted hydrogen bond between serine 342 and glutamic Acid 344 (the red arrow)
Based on the patient’s clinical presentation and molecular diagnosis, the patient was diagnosed with ARCND I, OSAS, and moderate hypoxemia. The principal problems to be addressed were convexity of the midface and micrognathia deformity, hypoplasia of the condylar region, retrognathism, and clockwise rotation of the mandible.In April 2016, after consulting with an orthodontist, a sequential treatment plan consisting of orthodontic treatment and craniofacial surgery with the aid of digital technology was established. During the preoperative orthodontic treatment, teeth 12 (located outside the lingual dental arch), 21 (with dead pulp), 33 (affected by severe periodontal disease), and 44 were extracted. Additionally, we aligned the crowded teeth and leveled the dentition to minimize tooth compensation.
After completion of the preoperative orthodontic treatment, distraction osteogenesis (DO) was performed using a virtual surgical plan and surgical guides via a submandibular incision in July 2017. Four distractors were placed bilaterally on the mandible to lengthen the body and rami (Fig. 4a-d). After a latent period of 5 days, the distractors were activated at a rate of 0.5 mm twice daily. After the distraction phase, the left and right mandibular rums were extended by 15 and 10 mm, respectively, whereas the left and right mandibular bodies were extended by 24 and 19 mm, respectively.
Six months after DO, the patient underwent orthognathic surgery in January 2018. The patient’s front teeth were repositioned; however, the maxillary occlusal plane remained low on the left side and high on the right. A Maxillary Le Fort I osteotomy was performed to rotate the maxilla counterclockwise, achieving a central incisal cusp movement of 3 mm forward and 2 mm upward. This achieved a 4 mm drop in the mesial buccal cusp of tooth 16 and a 3 mm drop in the mesial buccal tip of tooth 26. Bilateral sagittal split ramus osteotomy (BSSRO) was performed to coordinate the jaw bones and achieve better occlusion. Finally, horizontal osteotomy and genioplasty were performed simultaneously (Fig. 4e-g).
In September 2018, the patient underwent a final surgery, including mandibular contouring and buccal fat removal, to achieve a better facial profile. The patient continued orthodontic treatment until stable and optimal occlusion was achieved in October 2019.
Treatment results and follow-up
After treatment, the patient exhibited a symmetrical facial appearance with a well-defined facial contour (Fig. 5a). The mandible was fully extended, both horizontally and vertically, and the mismatch between the jaw and teeth was corrected (Fig. 6a, b). An approximate posterior Class I relationship was achieved, and the anterior overjet was relatively small (Fig. 5b). Marked improvement in the mandibular range of movement was observed, with a maximal opening capacity of 40 mm. The 3D reconstruction of the airway volume increased from 18,672 mm3 preoperatively to 32,880 mm3 postoperatively (Fig. 7).
The patient came to our hospital for review again in May 2024, the treatment outcome showed quite stable (Fig. 6c). Due to the incomplete symmetry and remodeling of TMJs, the mandible shifted to the right side about 1.9 mm slightly (Fig. 6d).Snoring symptoms had completely disappeared during sleep. Polysomnography revealed an apnea–hypopnea index of 0.5, and blood oxygen saturation was 97%, which demonstrated that the patient’s airway dysfunction had been significantly improved. No complications or discomfort was encountered during the follow-up period, and the patient and their family members were satisfied with the results.
Discussion and conclusions
In 1970, Cosman et al. [12] first reported two cases of a similar deformity of the external ear and named it QMEs. In 1998, Jampol et al. [2] systematically reported the characteristic triplet features of ARCND in a family and considered it as a syndrome. Subsequently, an increasing number ARCND cases have been reported.
GNAI3 at 1p13.3 [13, 14], phospholipase C beta 4 at 20p12.3-p12.2 [15, 16], and endothelin 1 [10, 17] at 6p24.1 are the three major deleterious gene variants of ARCND, all of which are involved in the endothelin-1-endothelin receptor type A (EDN1-EDNRA) signaling pathway [13]. An abnormal EDN1-EDNRA signaling pathway can inhibit the migration and differentiation of cranial neural crest cells, resulting in developmental defects in the first and second pharyngeal arches, ultimately causing ARCND [15, 18, 19]. Here, we report a novel GNAI3 mutation in a Chinese family that involved the insertion of "CATTGTGAAACAGATGAA" in genes 144 and 145 in exon 2 of chromosome 110,116,384. This insertion resulted in an HCETDE segment interposing between threonine 48 and isoleucine 49, which was predicted to impair the hydrogen bonding between serine and glutamate. All these changes may potentially block the EDN1-EDNRA signaling pathway, causing ARCND. Presently, the statistics of GNAI3 gene mutation sites included in the human gene mutation database indicate one deletion and 11 missense mutations. This new insertion mutation of GNAI3 in ARCND has not been reported previously.
Liu et al. [1] reported that amniocentesis was performed to seek for potential genetic defects in the 30-weeks fetus with ARCND, and a heterozygous variant of c.140G > A (NM_0064) was found in exon 2 of the GNAI3 gene by whole exome sequencing. The report showed that genetic early detection could be an effective method of early detection during the growth period. Studies about genetic early intervention during the growth period is few. After growth completion, surgical intervention is still the optimum therapeutic method for patients with ARCND so far. With the progress of gene technology, the genetic early detection and therapy of ARCND will be further developed.
The main purpose of ARCND treatment is to correct mandibular deficiency and TMJ deformity, coordinate the skull-jaw-teeth relationship, and establish good facial appearance and function. However, to date, only a limited number of sporadic ARCND cases have been reported. Ozturk et al. [20], Papagrigorakis et al. [21], Greig et al. [10], and Yang et al. [11] reported the use of a porous polyethylene prosthesis, DO, TMJ reconstruction, mandibular iliac bone transplantation, and Le Fort type I osteotomy to treat patients with ARCND. However, the application of preoperative orthodontics, DO, maxillary Le Fort I osteotomy, BSSRO, horizontal osteotomy, and genioplasty to treat adult patients with ARCND simultaneously has not yet been reported.
Aligning the teeth and adjusting the curve and width of the dental arch can facilitate the establishment of stable occlusion and improve compensatory tooth dislocation before surgery. In previous reports, we found that the height of the mandibular rami significantly increased after vertical extension. However, the length of the mandibular body remained insufficient, leading to inadequacy in the inferior 1/3 of the face and unsatisfactory condyle-to-fossa articulation. Therefore, in this case, we innovatively performed mandibular body distraction and BSSRO synergistically to coordinate the jawbone relationship and improved the functional balancing between mandibular sides and mandibular condyles. This surgical method has not been reported previously.
The correction of QMEs is another important step in the treatment of ARCND. Many surgical techniques, including double Z-plasty [12], the use of local rotation-advancement flaps [20], V–Y technique [22], use of local chondrocutaneous flaps or chondrocutaneous composite tissue transplantation [23], double-opposing Z-plasty [24], and use of cartilage grafts or expanded flaps [25], have been reported recently. These techniques have made QME treatment evidence-based and effective. Given the relatively normal deformity of the patient’s auricle in the present case, the patient declined any plastic treatment.
The application of digital technology has made the diagnosis and treatment of ARCND more controllable and predictable [9, 26]. Through 3D reconstruction of the CT data, we were able to clearly determine and analyze the cause of the deformity in this case. For example, we identified that the anterior displacement of the parotid glands and mandibular bony ridge were the primary factors contributing to the patient’s full cheeks. In addition, we observed that vertical and sagittal mandibular dysplasia contributed to airway narrowing and chin retraction. With the help of preoperative virtual design technology, we were able to execute osteotomy precisely with surgical guides and accurately design the number and position of the distraction hardware [27]. Possible issues during the distraction period can also be simulated and predicted in advance [28]. The digital design of orthognathic surgery plays a crucial role in establishing a harmonious relationship between the skull, jaw, and teeth [5, 29]. Using a 3D printed surgical guide, the virtual surgical plan was accurately replicated in the operating room, ensuring its precise implementation.
Therefore, the pathogenesis and treatment of rare hereditary maxillofacial diseases must be considered. In conclusion, we reported a novel GNAI3 mutation case in a Chinese family and the successful treatment of dental and maxillofacial deformities with the assistance of digital technology. This study provides a reference for a better understanding of the genetic pathogenesis and practical and effective treatment of ARCND for clinicians.
Availability of data and materials
The complete data and materials described in the case report are freely available from the corresponding author on reasonable request.
Abbreviations
- ARCND:
-
Auriculocondylar syndrome
- QMEs:
-
Question mark ears
- GNAI3 :
-
Guanine nucleotide-binding protein alpha-inhibiting activity polypeptide 3
- CT:
-
Computed tomography
- TMJs:
-
Temporomandibular joints
- OSAS:
-
Obstructive sleep apnea syndrome;
- 3D:
-
Three-dimensional
- DO:
-
Distraction osteogenesis
- BSSRO:
-
Bilateral sagittal split ramus osteotomy
- EDN1-EDNRA:
-
Endothelin-1-endothelin receptor type A
References
Liu X, Sun W, Wang J, et al. Prenatal diagnosis of auriculocondylar syndrome with a novel missense variant of GNAI3: a case report. BMC Pregnancy Childbirth. 2021;21(1):780.
Jampol M, Repetto G, Keith DA, et al. New syndrome? Prominent, constricted ears with malformed condyle of the mandible. Am J Med Genet. 1998;75(5):449–52.
Li Q, Jiang Z, Zhang L, et al. Auriculocondylar syndrome: Pathogenesis, clinical manifestations and surgical therapies. J Formos Med Assoc. 2023;122(9):822–42.
Bukowska-Olech E, Sowinska-Seidler A, Lojek F, et al. Further phenotypic delineation of the auriculocondylar syndrome type 2 with literature review. J Appl Genet. 2021;62(1):107–13.
Peart LS, Gonzalez J, Bivona S, et al. Bilateral choanal stenosis in auriculocondylar syndrome caused by a PLCB4 variant. Am J Med Genet A. 2022;188(4):1307–10.
Leoni C, Gordon CT, Della MG, et al. Respiratory and gastrointestinal dysfunctions associated with auriculo-condylar syndrome and a homozygous PLCB4 loss-of-function mutation. Am J Med Genet A. 2016;170(6):1471–8.
Nabil A, El SS, El SN, et al. A familial PLCB4 mutation causing auriculocondylar syndrome 2 with variable severity. Eur J Med Genet. 2020;63(6):103917.
Marszalek-Kruk B A, Wojcicki P, Dowgierd K, et al. Treacher Collins Syndrome: Genetics, Clinical Features and Management. Genes (Basel). 2021:12(9):1392.
Yu K, Luk HM, Gordon CT, et al. Mandibulofacial dysostosis Guion-Almeida type caused by novel EFTUD2 splice site variants in two Asian children. Clin Dysmorphol. 2018;27(2):31–5.
Greig A, Podda S, Thorne CH, et al. The question mark ear in patients with mandibular hypoplasia. Plast Reconstr Surg. 2012;129(2):368e–9e.
Yang Y, Tang X, Zhang Z, et al. Comprehensive therapy of facial contour in auriculo-condylar syndrome: clinical experience. Chin J Plast Sur. 2018;34(4):279–83.
Cosman B, Bellin H, Crikelair GF. The Question Mark ear. Plast Reconstr Surg. 1970;46(5):454–7.
Rieder MJ, Green GE, Park SS, et al. A human homeotic transformation resulting from mutations in PLCB4 and GNAI3 causes auriculocondylar syndrome. Am J Hum Genet. 2012;90(5):907–14.
Romanelli TV, Gordon CT, Zechi-Ceide RM, et al. Novel variants in GNAI3 associated with auriculocondylar syndrome strengthen a common dominant negative effect. Eur J Hum Genet. 2015;23(4):481–5.
Castinetti F, Reynaud R, Saveanu A, et al. MECHANISMS IN ENDOCRINOLOGY: An update in the genetic aetiologies of combined pituitary hormone deficiency. Eur J Endocrinol. 2016;174(6):R239–47.
Vegas N, Demir Z, Gordon CT, et al. Further delineation of auriculocondylar syndrome based on 14 novel cases and reassessment of 25 published cases. Hum Mutat. 2022;43(5):582–94.
Gordon CT, Petit F, Kroisel PM, et al. Mutations in endothelin 1 cause recessive auriculocondylar syndrome and dominant isolated question-mark ears. Am J Hum Genet. 2013;93(6):1118–25.
Graham A. The development and evolution of the pharyngeal arches. J Anat. 2001;199(Pt 1–2):133–41.
Graham A, Smith A. Patterning the pharyngeal arches. BioEssays. 2001;23(1):54–61.
Ozturk S, Sengezer M, Isik S, et al. The correction of auricular and mandibular deformities in auriculo-condylar syndrome. J Craniofac Surg. 2005;16(3):489–92.
Papagrigorakis MJ, Karamolegou M, Vilos G, et al. Auriculo-condylar syndrome. Angle Orthod. 2012;82(3):556–64.
Al-Qattan MM, Al-Qattan NM. Question mark ear deformity-revisited. Eur J Plast Surg. 2017;40(2):149–52.
Pan B, Jiang H, Guo D, et al. Repair of question mark ear. Plast Reconstr Surg. 2008;122(2):76e–7e.
Bastidas N, Taylor JA. Correction of the bilateral question mark ear deformity using double-opposing z-plasty and a chondrocutaneous flap. Cleft Palate Craniofac J. 2013;50(2):249–51.
Pan B, Jiang H, Zhao Y, et al. Clinical analysis, repair and aetiology of question mark ear. J Plast Reconstr Aesthet Surg. 2010;63(1):28–35.
Nickenig HJ, Safi AF, Matta RE, et al. 3D-based full-guided ridge expansion osteotomy - A case report about a new method with successive use of different surgical guides, transfer of splitting vector and simultaneous implant insertion. J Craniomaxillofac Surg. 2019;47(11):1787–92.
Burns HR, Wang DS, Abu-Ghname A, et al. Craniofacial Distraction Osteogenesis. Semin Plast Surg. 2023;37(4):253–64.
Vinzenz K, Patel PK, Cohen M. Optimizing Facial Esthetic Outcomes: Adding Distraction Osteogenesis to Your Classic Orthognathic Surgery Armamentarium. J Craniofac Surg. 2023;34(6):1692–8.
Norholt SE, Skoldstam J, Blomlof J, et al. Zygomatic repositioning and Le Fort II distraction with intraoral devices in Apert syndrome: A case report. J Craniomaxillofac Surg. 2022;50(4):364–70.
Acknowledgements
We are grateful to the patient and their family for their permission of the use of clinical data.
Funding
The work was supported by National Natural Science Foundation of China (82301046), Nature Science Research Foundation of Shaanxi Province (2022JZ-50) and Key Research and Development Projects of Shaanxi Province (2024SF-YBXM-264).
Author information
Authors and Affiliations
Contributions
YS: wrote part of this article and participated in the surgical treatment; LR: wrote part of this article and was in charge of the follow up for the patient; SL: was in charge of the orthodontic treatment for the patient; YL: participated in the surgical treatment; CZ: contributed the organization of this clinical study; JL: participated in the surgical treatment; HS: participated in the surgical treatment; YX: was in charge of the gene testing and analysis for the patient and her family, she also contributed the organization of this study; LT: organized the study and leaded the whole treatment for his patient.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patients for publication of his Case report and any accompanying images.
Consent for publication
A written consent for publication was obtained from the patients to publish all clinical details and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, Y., Rong, L., Liu, S. et al. Novel GNAI3 mutation in a Chinese family with auriculocondylar syndrome and treatment of severe dentofacial deformities: a 5-year follow-up case report. BMC Oral Health 24, 803 (2024). https://doi.org/10.1186/s12903-024-04575-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04575-1