Abstract
Global neglect of oral healthcare services (OHCS) provision, mainly in Low- and Middle-Income Countries, exacerbates the deterioration of health systems and increases global health inequality.
Objectives
The objective is to explore the profiles of available oral healthcare services in the WHO Eastern Mediterranean Region (EMR) countries.
Methods
A systematic literature search was conducted of grey literature and databases (PubMed, Medline, Embase, and the Cochrane Library). Peer-reviewed articles that reviewed and/or evaluated OHCS in WHO-EMR countries were identified. No time or language limitations were applied. Two independent reviewers conducted the screening and data extraction. A third reviewer arbitrated disagreement. The evaluation of the OHCS provision followed the WHO framework for health system performance assessment. The extraction included socio-demographic characteristics of the studied population, OHCS profile, responsiveness, and health insurance coverage.
Results
One hundred and thirty-seven studies were identified. The studies that met the inclusion criteria were fifteen published between 1987 and 2016. In addition, two reports were published in 2022. The included studies were conducted in Pakistan, Saudi Arabia, Iran, Libya, Egypt, Oman, Syria, Jourdan, Kuwait, and Tunisia. Generally, Ministries of Health are the main providers of OHCS. The provision for national dental care prevention programmes was highly limited. Furthermore, most of these Ministries of Health have struggled to meet their local populations’ dental needs due to limited finances and resources for OHCS.
Conclusions
Oral and dental diseases are highly prevalent in the WHO-EMR region and the governments of the region face many challenges to meeting the OHCS needs of the population. Therefore, further studies to assess and re-design the OHCS in these countries to adapt dental care prevention into national health programmes are crucial.
Similar content being viewed by others
Background
The most recent global WHO survey reported a lack of preventive oral health programmes in Low- and Middle-Income Countries (LMICs). Moreover, the same report shows a scarcity of information on oral healthcare services (OHCS) in the WHO Eastern Mediterranean Region (WHO-EMR) [1]. Furthermore, other recent reviews also highlighted the same shortage of preventative oral healthcare programmes in the region [2, 3]. Internationally, there is a growing consensus that neglect of oral health prevention and services [4, 5], lack of dental public health education, and growing political conflict negatively affect the population's dental health. Consequently, the risks of deterioration of oral health, services, and health equality are increasing.
As an example of the destructive impact of long-lasting armed conflicts on oral healthcare, the persistent conflict in the Occupied Palestinian Territories has produced a severe deterioration of health, oral health, and social care services [6,7,8]. As a result of the financial restrictions affecting existing health services, local governments and international bodies were unable to meet healthcare needs and promote overall oral health [9,10,11,12].
In addition, previous studies found deficiencies in the availability and effectiveness of oral health interventions aimed at promoting children and maternal oral health in LMICs [2, 3, 5]. The United Nations Relief and Works Agency (UNRWA) reported increased oral health impairments among Palestinian refugees living in the Occupied Palestinian Territories and the surrounding countries (Jordan, Syria, and Lebanon) [13]. Oral health surveys conducted in Jordan [14, 15], Syria [16] and Lebanon [17] highlighted the same poor oral health status among Indigenous populations. Besides that, the situation in other Middle Eastern countries does not show any better oral health profiles [18, 19], even in high-income countries such as the Arab Gulf states [20]. The most recent report published by the WHO demonstrated a high deficiency in the contribution of the national health budget to OHCS. In addition, there was a lack of preventive programmes in these countries associated with a high prevalence of untreated decayed teeth, mainly among children [5].
Therefore, the necessity of empowering OHCS and integrating the evidence-based WHO oral health promotion programmes into ongoing healthcare programmes should be a priority for policy makers in the Region [5, 12, 21].
To achieve that, there is still a need to explore the profile of current oral healthcare systems in WHO-EMR countries, which include 19 out of the 22 Arab countries, at least eight of which are in conflict zones. This information would help assess the performance and efficacy of promoting oral health in the region. In addition, it would enable healthcare stakeholders and scientists to investigate if the ongoing OHCS in LMICs including conflict zones could adapt the WHO oral health promotion interventions while maintaining high performance and outcomes to reduce oral health inequalities [21].
Unfortunately, such information is not currently available to answer these questions. The information is essential to identify factors, gaps, and challenges influencing the performance of OHCS. Moreover, it will help to envisage OHCS's capability to adapt the WHO oral health promotion interventions and maintain high performance. Therefore, the main aim of this scoping review is to explore the profiles of OHCS in the WHO-EMR countries and to evaluate their performance.
Methods
Research questions formulation
This scoping review was conducted to determine the profiles of OHCS in the WHO-EMR countries, evaluate their performance, and identify the gaps and challenges for OHCS in these countries.
Therefore, the main research questions are ‘What is the profile of the provided OHCS in the countries of the WHO-EMR?’ and ‘Do these services perform effectively to promote the oral health of populations?’
Additionally, ‘What factors, gaps, and challenges influence this performance?’ and ‘What is the capability of OHCS to adapt the WHO oral health promotion interventions and maintain its high performance?’
Determining the search strategy
A literature search was conducted using the following databases: MEDLINE, Embase, and the Cochrane Library. Furthermore, the websites of the Ministries of Health in WHO-EMR countries, the World Health Organization (WHO), the International Union for Health Promotion and Education (IUHPE), the United Nations Children's Fund (UNICEF), United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA), and the United Nations Refugee Agency (UNHCR) were searched.
Search terms were investigated, including: 1 “exp refugee/ or UNRWA.mp.”, 2 “Eastern Mediterranean*.mp.”, 3 “Middle East*.mp.”, 4 “Afghanistan.mp.”, 5 “Bahrain.mp.”, 6 “Djibouti.mp.”, 7 “Egypt.mp.”, 8 “Iran.mp.”, 9 “Iraq.mp.”, 10 “Jordan.mp.”, 11 “Kuwait.mp.” 12 “Lebanon.mp.”, 13 “Libya.mp.”, 14 “exp Palestine/ or Occupied Palestinian territory.mp.”, 15 “Morocco.mp.”, 16 “Oman.mp.”, 17 “Pakistan.mp.”, 18 “Qatar.mp.”, 19 “Saudi Arabia.mp.”, 20 “Somalia.mp.”, 21 “Sudan.mp.”, 22 “Syria.mp. or exp Syrian Arab Republic/”, 23 “Tunisia.mp.”, 24 “United Arab Emirates.mp.”, 25 “Yemen.mp.”, 26 “Algeria.mp.”, 27“WHO EMRO*.mp.”, 28 “1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27”, 29“*dental care/ or Oral Health*.mp.”, 30 “*health care delivery/ or health system*.mp. or *health care system/”, 31 “*primary health care/”, 32 “*total quality management/”, 33 “*dental health/ or *dental care/ or Dental Health*.mp.”, 34 “29 or 33”, 35 “30 or 31 or 32”, 36 “34 and 35”, 37 “28 and 36”.
The search was conducted between 15 Jan 2022 and 30 Jan 2023. No limitations for the period or language of studies were specified. All eligible papers determined after the first screening were reviewed ensuring that each paper met the inclusion and exclusion criteria (Table 1).
Screening: Selecting the literature
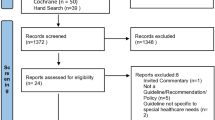
Two independent researchers selected the studies relevant to the research question. The two independent researchers screened the title and abstracts. After that, they independently reviewed the full text obtained to identify the included studies, as detailed in the PRISMA flow diagram in Fig. 1. The third reviewer arbitrated disagreement on study inclusion between the two reviewers.
Prisma chart for studies screening and inclusion [20]
The current review explored the profiles of OHCS in WHO-EMR countries. A systematic search was conducted for relevant databases and grey literature. Two reports were identified from the grey literature: [1] the OHCS provided by UNRWA were found in the annual health report published by the UNRWA [22], and [2] the global oral health status report [5].
Data extraction strategy
The articles and reports that met the inclusion criteria were retained for data extraction. A data extraction chart collated and compared available OHCS inputs, outputs, and oral healthcare processes in WHO-EMR countries. Two reviewers developed this chart; one reviewer extracted the data to an electronic data form (Excel), and the second reviewer double-checked the extraction for the content. The extracted data was standardised based on the WHO standards for evaluating healthcare services the WHO framework for health system performance assessment within WHO-EMRO countries [23,24,25].
The final characteristics and data charting form were discussed by the research team and follow the WHO recommendations. The evaluation of oral health services profile and performance followed the WHO framework for health system performance assessment within WHO-EMR countries [23,24,25]. System performance is the extent to which health systems meet their goals [26]. Effective oral healthcare systems should achieve the main three cross-goals for the health system [23]: Health (Oral Health); Responsiveness; and Fairness in Financing.
The extraction table contains the following elements: Population size of the targeted country; Availability of OHCS; and Oral Health: a) Institutions providing OHCS, b) Personnel providing the care, c) Type of services: emergency, curative, prevention, treatment protocols, or referral system, d) Intervention and/or programmes for oral health prevention, e) Population size receiving the service? targeted age groups?, f) Inter-sectorial action: integration of oral healthcare in ongoing primary health programmes, g) Standard set of medical (dental) equipment and furniture, h) Information system for oral health practice and quality: information system for data collection, management, indicators and measurement of oral health outcome and quality of service, i) Staff capacity building: professional development and training programmes, j) Safety and accreditation programme, k) International health organisation support and contribution to OHCS, l) Responsiveness, m) Measurement to the respect of the oral health care system for persons (person’s dignity, autonomy, and confidentiality) and meeting client orientation (consumer satisfaction), n) Fair financing and financial risk protection, o),Health insurance coverage for oral health curative and prevention programmes, and p) Contribution of the national health budget to oral health care expenditure
Risk of bias (quality) assessment
This review has not included studies assessing the effect size of a specific intervention. Thus, the methodological quality assessment and risk of bias assessment were not conducted as an essential part of the scoping reviews [27, 28].
Strategy for data synthesis
The outcome of the review was presented using a descriptive-analytical method. A narrative summary of included studies and outcomes was presented in tables and discussed the findings' meanings and implications to the overall purpose of the review question. The tables included extracted data for the change in the incidence or indicators of oral health, responsiveness, and fairness in financing because of implementing OHCS.
Results
One hundred thirty-seven studies met the review’s inclusion criteria in the databases searched. Of those, only 23 studies were retained for full-text review. Figure 1 shows that eight studies were excluded for the following reasons: not finding the full text of the record, the study not being conducted in one of the WHO-EMR countries, or the study design not evaluating the OHCS in these countries. In total, fifteen studies were included in the review for data extraction (Fig. 1). The included peer-reviewed studies were published between 1987 and 2016. In addition, two reports were identified from the grey literature: [1] the OHCS provided by UNRWA, found in the annual health report published by UNRWA [22], and [2] the global oral health status report [5].
The data related to oral and dental healthcare in the reviewed studies and grey literature is summarised in Tables 2, 3 and 4. While, the data related to oral and dental healthcare from the WHO global oral health report [5] was summarised in Table 5.
Demographic characteristics of the included populations
Based on the list of Development Assistance Committee (DAC) in the United Nations [37], the included studies reviewing the OHCS in three high-income countries (Saudi Arabia, Kuwait, Oman), two upper-middle-income countries (Libya, Jordan) and five LMICs (Iran, Egypt, Syria, Pakistan, Tunisia). The information about OHCS provided by UNRWA to the Palestinian refugees living in the refugee camps located in the Palestinian Territories (Gaza Strip and West Bank), Jordan, Syria, and Lebanon was extracted from the most recent UNRWA Health Department Annual Report for the year 2022 [22].
Table 2 summarises the political and socio-demographic characteristics of the countries in the included studies. Most countries had stable political statuses when the studies were conducted, except for Libya [34] and Palestinian refugees’ camps [22]. Among the included studies, Pakistan had the highest populous size (̴ 152 million), whereas Kuwait was the lowest (̴ 2.2 million) [20]. Population growth rates ranged between 2% and 2.7%. In 1988, the reported growth rate in the rural areas of Egypt (29.7%) was the highest in the WHO-EMR and the world [36].
In 2022, Pakistan's population doubled (227.2 million) and remained the highest in the region. Meanwhile, Djibouti (1.1 million) accounted for the lowest population size, as shown in Table 4.
Healthcare and oral healthcare services
The assessment of the performance of OHCS in this review followed the WHO framework for health system performance assessment and health services research tools [1, 23,24,25, 38].
In included countries, governmental MOHs are the dominant provider of these services. UNRWA is the main provider of OHCS for Palestine refugee camps in five fields of operation (Jordan, West Bank, Gaza Strip, Syria, and Lebanon) [13] (Table 3).
The contribution percentage of Gross Domestic Product to Health Expenditure/year was the lowest in Pakistan (0.7%) and the highest in Libya (4%). Oral healthcare services accounted for 5%, 15.5%, and 3.7% of the national health budgets in Saudi Arabia (1984), Iran (2009) and UNRWA (2022) respectively (Table 2). Table 5 shows that in 2021, the contribution of per capita National health expenditure to per capita oral health expenditure was the highest in Iran (4.8%). In the high-income countries, it ranges between 3% in Qatar and 0% in Oman, while for all the rest of the countries, it is less than 1.3%.
The information regarding health insurance coverage for OHCS is rare; only Tunisia, Saudi Arabia, and UNRWA illustrated that health insurance covers essential treatments (fillings and extractions) and preventative dental care where available.
The oral health profile, services, and workforce are detailed in Tables 3 and 4. Syria, Oman, Iran, Saudi Arabia, Pakistan, Tunisia, and Kuwait included OHCS within the country’s national health plan. No study provided any information about gross national product allocation for oral health per year.
In some countries, the private sector, the Ministry of Education (for school oral health programmes), the Ministry of Defence (military medical services) and schools of dentistry in the local universities contribute to OHCS. The proportion of the population receiving OHCS from government MOH was reported only in Syria (8%), Pakistan (55%), Iran (70% by government in rural areas and 80% by private sectors in cities) and Saudi Arabia (100%), as shown in Table 3.
Oral and dental health status
Table 3 illustrates that dental caries and oral diseases were highly prevalent in the countries included and significantly higher in poor groups. Pakistan had the second-highest oral cancer prevalence in the world [19]. Dental caries prevalence and experience (decay, missing and filled deciduous teeth (dmft) and Decayed, Missing, and Filled Permanent Teeth (DMFT)) was high among children and adults in all the reviewed studies and increased over the years. For example, dental caries in Iran were highly prevalent in all age groups (up to 98.8%). Moreover, the prevalence of dental caries and periodontitis was higher among older age groups [33, 35]. A large part of decayed primary and permanent teeth was left untreated in Syria [16]. The prevalence of gingivitis and periodontal disease is also extraordinarily high, with high plaque accumulation as it reached 94% among 15-year-old children in Syria. Tunisia had the highest prevalence of malocclusion compared to other EMR countries [29, 39]. Poor oral health and toothbrushing practices were common among most of the included populations, except in Tunisia, which reported good toothbrushing practices among its population [29] despite the high prevalence of dental caries.
Table 5 shows that, most recently, Saudi Arabia had the highest level of untreated deciduous and permanent decayed teeth (53.2% and 38.8%, respectively) in the region despite it being a high-income country. Generally, sugar intake is extremely high among the population of the EMR (46.8 - 112.8 g/day).
Workforce in oral healthcare
Dentist to population ratio varies widely between countries; a shortage in this ratio was detected in Pakistan and southern Tunisia (1 dentist: 120,000 inhabitants). The availability of dental auxiliary and administrative staff was deficient in the studies included, mainly in Ministries of Health. Libya, Egypt, Oman, Bangladesh and UNRWA provided no information (Table 3).
Recent figures show countries where the dentists to population ratio is less than 2:10,000 are Yemen, Djibouti, Afghanistan, Bahrain, Pakistan, and Morocco. Most countries do not have a national oral health policy or action plan. Thus, oral health has not yet been incorporated into the NCD programmes at the Ministries of Health (Table 5).
Oral healthcare curative and preventive services (Table 4)
The OHCS programmes and responsiveness information are presented in Table 4. Water fluoridation for the prevention of dental caries is applied in Saudi Arabia, Iran, and Oman. Most of the included studies' oral health prevention programmes varied between screening and applying fissure sealant and fluoride modalities (e.g., fluoride mouth rinse, toothbrushing with fluoride toothpaste and fluoride varnish).
Oral healthcare-related research and surveillance are rare. In addition, there are remarkable shortcomings in the management of information and analysis of available data to use these data for bureaucratic purposes. Only UNRWA illustrated that an annual assessment of the oral health programme’s staff workload, needs, productivity, and efficiency is conducted in all five fields. Otherwise, existing dental care prevention programmes were not assessed for their effectiveness. Finally, all health planners in the included studies agree on shifting from curative to preventive oral health strategies.
The countries applying tax strategies on sugary diets are Bahrain, Afghanistan, Oman, Pakistan, Iran, Saudi Arabia, Tunisia, Morocco, and the United Arab Emirates (Table 5). Oral health screening is unavailable in Jordan, Sudan, Lebanon, and Somalia. The latter three countries do not provide basic restorative dental procedures to treat existing dental decay. In addition to that, Somalia does not offer urgent treatment for emergency oral care or pain relief. Countries that included oral health interventions in governmental public Health Benefit Packages (routine and preventive oral healthcare, essential curative oral healthcare, advanced curative oral/dental care, and rehabilitative oral healthcare) are Oman, Tunisia, Iran, the United Arab Emirates, Kuwait, and Syria (Table 5).
Discussion
This review found that few studies were published for evaluations of the OHCS in the countries of the WHO-EMR. Most recently, the WHO Global Oral Health Status Report [5] summarised OHCS profiles in these countries.
As mentioned, the included studies were published between 1987 and 2016. This was when most of the EMR countries were in stable political situations. Even so, dental caries and other oral health diseases were highly prevalent during that period. In addition, most of the included studies reported the OHCS's failure to meet the served population's oral healthcare needs. The enormous increases in political unrest in the WHO-EMR since 2016, and specifically in the most recent decade, undoubtedly worsened oral health status among the region's population. This may explain why more than half the children (1-9 years) had untreated caries in the deciduous teeth [5]. Nonetheless, the WHO report lacked information about Palestinian refugees’ oral health needs and services in the region. Moreover, the availability of dental public health education and capacity building for dental public health in the higher education sector were rare.
The governments’ neglect of OHCS provision is a well-known global issue [4]. The review results show that the contribution of national health expenditure to OHCS was extremely low (<5%), even in high-income countries. This explains why the information on health insurance coverage for the OHCS is rare. Moreover, any contribution of health insurance to OHCS was limited to covering the basic treatments (fillings and extractions) and prevention of dental care if it existed, as in Tunisia and Saudi Arabia [29, 30]. Iran operated a unique OHCS system, that depended on health workers in early detection and preventive oral health care, mainly in rural areas [33, 35]. Nonetheless, dental caries is still high among its population.
As in most countries worldwide, the provision of healthcare, including OHCS, is the responsibility of MOHs in the WHO-EMR [1, 23], with UNRWA the leading provider of healthcare services for Palestinian refugee camps situated in five fields of operation (Jordan, West Bank, Gaza Strip, Syria and Lebanon) [13]. Based on that, the WHO raised the necessity of elevating governmental support and consideration of the OHCS in the national and regional healthcare strategy [40].
Most of the included studies recommended this initiative and considered it part of future strategies to empower OHCS nationally. Additionally, other governmental and non-governmental health stakeholders may participate in the provision of OHCS, such as the private sector, the Ministry of Education (mainly for school oral health programmes), the Ministry of Defence (Military Medical Services) and Schools of Dentistry in the local universities. This would be an excellent opportunity to overcome the services shortage that the ministries of health are facing.
The assessment of the performance of OHCS in this review followed the WHO framework for health system performance assessment and health services research tools [1, 23,24,25, 38].
This review considered assessing the health workforce, administration, and supply of health services, OHCS quality and performance evaluation, and financial and technological support. High- and upper-middle-income countries (Saudi Arabia, Qatar, United Arab Emirates, Kuwait, Jordan, Libya, and Lebanon), in addition to Syria, reported dentist-to-population ratios of more than or equal to five dentists per 10,000 population. This is better than the worldwide dental workforce profile, which shows that over 68% of WHO Member States had less than five dentists per 10,000 population, and 37% had less than 1 [40]. A persistent shortage of dental assistants and technicians is a substantial issue in the WHO-EMR.
It is unclear whether water fluoridation interventions cover all populations in Saudi Arabia, Iran, and Oman [31, 32, 35]. However, water fluoridation is a highly recommended intervention to reduce dental caries among the whole population [41], combined with school-supervised toothpaste brushing with fluoridated toothpaste programmes as such intervention showed considerable effectiveness in reducing dental caries among six years old children, mainly in conflict zones [42, 43]. Unfortunately, dental caries and the promotion of healthy oral and eating behaviours are seldom in the WHO EMR, as this review clarified.
The limitations of the current review are that firstly, the evaluation of OHCS in the WHO-EMR has been conducted for a long time; secondly, the grey literature (respective countries' dental/medical councils, commission, societies, and Ministries information) has been searched, and unfortunately, information related to dental healthcare services are seldom available and highly ignored. Thirdly, no data about OHC responsiveness (person’s dignity, autonomy, confidentiality and/or satisfaction) were available in the included studies. However, Table 5 included the latest information reported by the WHO regarding oral and dental disease prevalence, challenges to dental care, and OHCS profile in the WHO-EMR.
Conclusions
OHCS provision in the countries of the WHO-EMR region need better dental care prevention strategies. The high prevalence of dental diseases and resource deficiencies (OHCS expenditure is unknown) means MOHs struggle to meet populations’ dental care needs. Moreover, the current dependence of governmental OHCS primarily on basic dental treatment provisions and a scarcity of prevention programmes exacerbates the problem.
Therefore, further studies are needed to assess the OHCS performance, gaps, and effectiveness to predict the most effective and cost-effective OHCS practical preventive model. This model should tackle the seriously deteriorated oral health status in the region, to implement the most recent WHO recommendation and integrate OHCS as an essential part of Universal Health Coverage [44].
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- DAC:
-
Development Assistance Committee
- Dmft:
-
Decay, missing and filled deciduous teeth
- DMFT:
-
Decayed, Missing and filled Permanent Teeth
- IUHPE:
-
International Union for Health Promotion and Education
- LMICs:
-
Low- and Middle-Income Countries
- MOH:
-
Ministry of Health
- OHCS:
-
Oral Health Care Services
- UNHCR:
-
United Nations Refugee Agency
- UNICEF:
-
United Nations Children's Fund
- UNRWA:
-
United Nations Relief and Works Agency for Palestine Refugees in the Near East
- WHO:
-
World Health Organization
- WHO-EMR:
-
WHO-Eastern Mediterranean Region
References
Petersen PE, Baez RJ, Ogawa H. Global application of oral disease prevention and health promotion as measured 10 years after the 2007 World Health Assembly statement on oral health. Community Dent Oral Epidemiol. 2020;48(4):338–48.
Abuhaloob L, Carson S, Richards D, Freeman R. Community-based nutrition intervention to promote oral health and restore healthy body weight in refugee children: a scoping review. Community Dent Health. 2018;35(2):81–8.
Abuhaloob L, MacGillivray S, Mossey P, Freeman R. Maternal and child oral health interventions in Middle East and North Africa regions: a rapid review. Int Dent J. 2019;69(6):409–18.
Watt RG, Daly B, Allison P, Macpherson LMD, Venturelli R, Listl S, Weyant RJ, Mathur MR, Guarnizo-Herreno CC, Celeste RK, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394(10194):261–72.
World Health Organization. Global oral health status report: towards universal health coverage for oral health by 2030. Regional summary of the African Region: World Health Organization; 2023.
Rawaf S: Palestine: Feasibility Study to Establish a National Institute of Public Health. In. London-United Kingdom: Imperial College London; 2010.
Keelan E. Medical care in Palestine: working in a conflict zone. Ulster Med J. 2016;85(1):3.
Humphris R, Abuhaloob L. A Double Burden or Triple Burden for Palestinian Children Residing in Gaza Refugee Camps? Exploring the Role of Diet in Malnutrition, Obesity and Dental Caries. J Palest Refug Stud. 2014:87.
Ministry of Health: The Annual report of Oral Health Department 2011. In. Palestine: Ministry of Health-Health Management Information System; 2012.
UNRWA: The Annual Report of the Department of Health 2011. In. Amman - Jordan: United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA); 2012.
Biscaglia L, di Caccamo P, Terrenato I, Arrica MA, Seita A, Campus G. Oral health status and caries trend among 12-year old Palestine refugee students: results from the UNRWA’s oral health surveys 2011 and 2016. BMC Oral Health. 2019;19(1):1–10.
Abuhaloob L, Petersen PE. Oral health status among children and adolescents in governmental and private schools of the Palestinian Territories. Int Dent J. 2018;68(2):105–12.
UNRWA: The Annual Report of the Department of Health 2020. In. Amman, Jordan: UNRWA United Nations Relief and Works Agency for Palestine Refugees in the Near East Department of Health; 2021.
Rajab LD, Petersen PE, Baqain Z, Bakaeen G. Oral health status among 6-and 12-year-old Jordanian schoolchildren. Oral Health Prev Dentistry. 2014;12(2).
Taani DS. Oral health in Jordan. Int Dent J. 2004;54(6 Suppl 1):395–400.
Beiruti N, Palenstein Helderman WV. Oral health in Syria. Int Dental J. 2004;54(6):383–8.
Doumit M, Doughan B. Dental caries and fluorosis among children in Lebanon. Indian J Dental Res. 2018;29(3):317.
Iyer K, Krishnamurthy A, Pathak M, Krishnan L, Kshetrimayum N, Moothedath M. Oral health taking a back seat at primary health centers of Bangalore urban district, India–A situation analysis. J Fam Med Prim Care. 2019;8(1):251.
Basharat S, Shaikh BT. Primary oral health care: a missing link in public health in Pakistan. East Mediterr Health J. 2016;22(9):703–6.
Behbehani JM, Scheutz F. Oral health in Kuwait. Int Dental J. 2004;54(6 Suppl 1):401–8.
Sheiham A, Williams D. Reducing inequalities in oral health in the Africa and Middle East region. Adv Dental Res. 2015;27(1):4–9.
UNRWA: The Annual Report of the Department of Health 2022. In. Amman, Jordan: The United Nations Relief and Works Agency for Palestine Refugees in the Near East Department of Health (UNRWA); 2023.
Murray CJ, Frenk J, Organization WH: A WHO framework for health system performance assessment. 1999.
Nashat N, Hadjij R, Al Dabbagh AM, Tarawneh MR, Alduwaisan H, Zohra F, AlFaris EA, Quezada-Yamamoto H, van Weel C, Rawaf S. Primary care healthcare policy implementation in the Eastern Mediterranean region; experiences of six countries: Part II. Eur J Gen Pract. 2020;26(1):1–6.
Kandelman D, Arpin S, Baez RJ, Baehni PC, Petersen PE: Oral health care systems in developing and developed countries. Periodontology. 2000. 2012; 60(1):98-109.
Busse R, Klazinga N, Panteli D, Quentin W: European Observatory Health Policy Series. In: Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies. edn. Edited by Busse R, Klazinga N, Panteli D, Quentin W. Copenhagen (Denmark): European Observatory on Health Systems and Policies © World Health Organization (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies) and OECD (2019). 2019.
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evid Implement. 2015;13(3):141–6.
Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Scoping reviews. Joanna Briggs Institute Reviewer’s Manual. 2017;2015:1–24.
Abid A. Oral health in Tunisia. Int Dent J. 2004;54(6 Suppl 1):389–94.
Baghdadi ZD. Managing dental caries in children in Saudi Arabia. Int Dent J. 2011;61(2):101–8.
Gallagher JE, Manickam S, Wilson NH. Sultanate of Oman: building a dental workforce. Hum Resour Health. 2015;13:50.
Guile EE, Shammary AA. Saudi Arabian dentistry: a factual and conceptual view. J Public Health Dent. 1987;47(1):16–8.
Pakshir HR. Oral health in Iran. Int Dent J. 2004;54(6 Suppl 1):367–72.
Peeran SW, Altaher OB, Peeran SA, Alsaid FM, Mugrabi MH, Ahmed AM, Grain A. Oral health in Libya: addressing the future challenges. Libyan J Med. 2014;9:23564.
Tahani B, Khoshnevisan MH, Yazdani S, Ebn Ahmady A, Dugdale P. Stewardship of National Oral Health system in Iran: its strengths and weaknesses. Arch Iran Med. 2013;16(12):717–24.
Wissa AA, Zahran MA. Evaluation of governmental dental health services in rural health centers in Egypt. Commun Dentistry Oral Epidemiol. 1988;16(1):16–8.
DAC List of ODA Recipients. https://www.oecd.org/dac/financing-sustainable-development/development-finance-standards/daclist.htm.
Holland W: Improving health services: background, method and applications: Edward Elgar Publishing; 2013.
Maatouk F, Maatouk W, Ghedira H, Mimoun SB. Effect of 5 years of dental studies on the oral health of Tunisian dental students. East Mediterr Health J. 2006;12(5):625–31.
Health workforce: Dentistry personnel [https://www.who.int/data/gho/data/indicators/indicator-details/GHO/dentists-(number)#:~:text=Over%2068%25%20of%20WHO%20Member%20States%20report%20to,%28about%2037%25%20report%20to%20have%20less%20than%201%29]
World Health Organization: Ending childhood dental caries: WHO implementation manual. 2019.
Petersen P, Hunsrisakhun J, Thearmontree A, Pithpornchaiyakul S, Hintao J, Jürgensen N, Ellwood R. School-based intervention for improving the oral health of children in southern Thailand. Commun Dent Health. 2015;32(1):44–50.
Abuhaloob L, Petersen PE. Health-Promoting Schools Project for Palestine Children's Oral Health. Int Dent J. 2023;73(5):746–53. https://doi.org/10.1016/j.identj.2023.03.011.
World Health Organization: Follow-up to the Political Declaration of the Third High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases. Proceedings of the Seventy-Fifth World Health Assembly, Geneva, Switzerland. 2022:22-28.
Behbehani JM, Shah NM. Oral health in Kuwait before the Gulf War. Med Princ Pract. 2002;11 Suppl 1:36–43. https://doi.org/10.1159/000057777.
Maatouk F, Jmour B, Ghedira H, Baaziz A, Ben Hamouda L, Abid A. Goals for oral health in Tunisia 2020. East Mediterr Health J. 2012;18(10):1072–7. https://doi.org/10.26719/2012.18.10.1072.
Shah MA, Darby ML, Bauman DB. Improving oral health in Pakistan using dental hygienists. Int J Dent Hyg. 2011;9(1):43–52. https://doi.org/10.1111/j.1601-5037.2009.00434.x.
Acknowledgements
To Rachel Backer for her review of the manuscript.
Funding
The authors have no funding to report.
Author information
Authors and Affiliations
Contributions
LA developed the project idea, objectives, and methods, conducted all review processes, wrote the main manuscript text, and was the first reviewer. CT was the second reviewer in the stages of screening and full-text review. FA was the third reviewer in the stages of screening and full-text review. SR supervised the development of the project ideas and methods. All authors reviewed the manuscript.
Authors’ information
WHO Collaborating Centre for Public Health Education and Training, Primary Care & Public Health, School of Public Health, Faculty of Medicine, Imperial College London, UK.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abuhaloob, L., Tabche, C., Amati, F. et al. Provision of oral healthcare services in WHO-EMR countries: a scoping review. BMC Oral Health 24, 705 (2024). https://doi.org/10.1186/s12903-024-04446-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04446-9