Abstract
Background
The present study aimed to evaluate the effectiveness of using platelet-rich fibrin (PRF) as the apical matrix for the placement of MTA in nonsurgical endodontic therapy for teeth with periapical lesions and open apices.
Methods
Twelve teeth from eleven patients with periapical periodontitis and open apices were enrolled in the study. Nonsurgical endodontic therapy was performed with the PRF used as an apical barrier and the MTA manipulated as an apical plug for further thermoplasticized gutta percha in the remaining part of the root canal. Clinical signs and periapical digital radiographs were recorded and analyzed to evaluate the curing progress after periodical follow-ups of 1, 3, and 6 months. The horizontal dimension of the periapical lesion was determined, and the changes in the dimensions were recorded each time. The Friedman test was used for statistical analysis, with P < .05 serving as the threshold for determining statistical significance.
Results
All patients had no clinical symptoms after the first month of treatment, with a significant reduction in the periapical lesion after periodical appointments.
Conclusions
PRF is an effective barrier when combined with MTA for the treatment of teeth with periapical periodontitis and open apices.
Similar content being viewed by others
Background
Teeth with open apices and periapical lesions because of traumatic or abnormal reasons have been endodontically treated by many methods, from conventional apexification with calcium hydroxide to modern application of MTA [1].
The traditional nonsurgical approach for apexification using calcium hydroxide Ca(OH)2 has certain drawbacks, such as prolonged follow-up, multiple visits, patient compliance requirements, difficulty, and distinctive manipulation [2]. Although this conventional method is not a sensitive technique, the weakened dentin structure could be an unexpected outcome of this uncomplicated measurement. Patient compliance is paramount for the success of this long-term process because of the possibility of reinfection of the root canal space resulting from inaccurate follow-up checks, accidentally broken temporary filling or even the remaining weak tooth structure [3].
Apical closure using MTA on the canal cervical third and a blood clot in the whole root canal space for revascularization of the pulp complex connective tissue is also a promising option [4]. However, this sensitive technique has unpredictable outcomes with certain unfavorable consequences.
Both of the above methods are not suitable for severely missing dental structure teeth, where immediate requirements for restoration are urgently needed. Occlusal situation and aesthetic issues are also important factors in determining the choice of these two treatment options. If these circumstances are unfavorable, apexification and apical closure with regeneration of the pulp complex are not proper choices for the operator.
The prevention of apical extrusion of material is a considerable challenge for teeth with wide apices and periapical lesions. In addition to being wet and dark, substances are easily removed from the apex foramen because of the open space, especially for slurries and substances with extensive setting times, such as calcium silicate-based cement and endodontic sealers. Although the apical extrusion of MTA has an unconsiderable effect on the healing process of periapical lesions, healing progress takes longer, and this outcome was not recommended by the authors of a previous study [5].
Chemical or thermal gutta-percha for root canal obturation of the apical third is an ineffective and unreliable technique for accessing teeth with open apices, especially those with severe periapical lesions [1].
The formation of an apical barrier for a certain biological substance is necessary for predictable, favorable, and effective placement of calcium-silicate material such as MTA [1]. Hemostatic collagen membranes have been successfully applied to the barrier at the apical region to prevent apical extrusion of substances in previous studies [1, 6]. However, this material has not been an autogenous substance for ensuring a completely biocompatible healing process.
By introducing platelet-rich fibrin (PRF) [7], this strong fibrin membrane enriched with platelets and growth factors has become popular in dentistry, especially in endodontic therapy [8,9,10]. The PRF membrane has been successfully used as an apical barrier for safe MTA or Biodentine placement in previous studies [11, 12]. Leukocyte PRF (L-PRF) [13] has been used in these case reports with promising results. However, to date, advanced PRF (A-PRF) [13] has not been manipulated as an apical barrier in the endodontic treatment of teeth with open apexes and periapical lesions [14,15,16].
The aim of the present study was to evaluate the effectiveness of the combination of A-PRF as an apical barrier and MTA for the treatment of teeth with periapical lesions and open apices.
Methods
This study was approved by the Research Ethics Committee of the University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam, with the approval number 236/ĐHYD-HĐĐĐ. Informed consent was obtained from all participants or their parents, and all methods were performed in accordance with the relevant guidelines and regulations. Informed consent was also obtained from all patients and/or their legal guardians for the publication of identifying information/figures in an online open-access version.
The sample size was calculated using G*Power version 3.1.9.6 (Universität Kiel, Germany) with an effect size of 1.05, an alpha of 0.05, and a power of 0.9, leading to a sample size of 12 teeth. The Wilcoxon signed-rank test (matched pairs) in the software was chosen for the reduction of the horizontal dimension of the periapical radiolucent area before and after nonsurgical endodontic therapy at the periodical appointments.
A total of eleven patients with teeth on both the maxillary and mandibular sides were recruited for the present study. The inclusion criteria were teeth with a diagnosis of symptomatic or asymptomatic apical periodontitis, periapical lesions, and open apices. The exclusion criteria were patients who had orofacial chronic pain, such as migraine, sinusitis, temporomandibular pain, or trigeminal neuralgia. Teeth with severe structures that were unrestorable, had unacceptable crown-to-root ratios, or were cracked were also not included in the present study.
The subjects were recruited at the Department of Operative Dentistry and Endodontics, Faculty of Odonto-Stomatology, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam, from November 2021 to April 2023.
All endodontic procedures were performed by the same endodontist via the same standard procedure. For the first appointment, after completing the administrative procedure, a putty silicone bite registration impression was made to capture the first long cone periapical digital radiograph using the X-Mind unit and the phosphor plate (Satelec, Acteon Group, France) with a 16-inch position device.
Local anesthesia was administered using 2% lidocaine (Lignospan standard, Septodont, France), followed by rubber dam isolation (Ash Rubber Dam, Dentsply Sirona, Switzerland). A 3D dental operating microscope (Promise Vision 3D, Seiler, St. Louis, MO, USA) was used for enhanced vision and illumination during the entire nonsurgical root canal procedure.
The endodontic access cavity was prepared using Martin and Endo-Z burs (Dentsply Sirona, Maillefer, Switzerland) under copious sterile water spray. The root canal length was subsequently measured via the synthesis of information from an electronic apex locator (ProPex PiXi, Dentsply Sirona, Maillefer, Switzerland), a periapical digital radiograph, and observation under a dental microscope. The working length was shorter than the root canal length at 2 mm. The root canal was prepared using K-files (Dentsply Sirona, Maillefer, Switzerland) with gentle, circumferential motion. A Max-i-Probe needle (Dentsply Sirona, Maillefer, Switzerland) was used to deliver 3% sodium hypochlorite (Canal Pro, Coltene Whaledent, Altstätten, Switzerland) into the root canal space for copious irrigation.
Root canal preparation was performed with the purpose of at least dentin removal and as much content cleaning as possible. Saline solution was used for final irrigation of the root canal. After being parched by sterile paper points, the root canal was filled with calcium hydroxide paste (Endo Cal, Septodont, France), which was subsequently gently condensed using a proper plugger (Dentsply Sirona, Maillefer, Switzerland), ensuring that the paste fully occupied the entire root canal, from the apical end to the cemento-enamel junction. The Cavit (GC, Tokyo, Japan) was used to fill the access cavity with an underlying sterile cotton pellet.
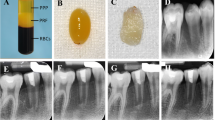
The next appointment was scheduled for one week after the first visit. The apical plug procedure was prepared after the completion of the root canal content removal and drying. Ten milliliters of venous blood was drawn from the subjects’ venae brachia and centrifuged at 1300 rotations per minute (RPM) for 8 min at a maximal relative centrifugal force (RCF-max) of 208 g [13] using an apparatus (PRF Duo Quattro, Nice, France). The fibrin clots containing the platelets were extracted. The PRF block was then placed under the cover of the box, over the flat plane inside the box, for 120 s to allow the formation of the PRF membrane. The PRF membrane was subsequently cut into 3 mm × 3 mm pieces, inserted, and gently condensed into the apical apex region with an appropriate plugger. Under the microscope, the pieces of the cut PRF membrane were condensed incrementally through the canal into the periapical area using the proper condenser until a firm barrier was established at the apex of the root. The procedure was performed rapidly and easily because of the widening of the apical portion of the root. The position and texture of the PRF barrier were checked for stability with a plugger under a dental operating microscope, and additional pieces of PRF could be further condensed into place if needed.
MTA Angelus (Angelus, Brazil) was mixed following the manufacturer’s instructions and inserted into the MTA carrier by digging the gun into the prepared MTA material mass. The MTA material was delivered into the apical region by triggering the piston of the carrier. The plugger was used to gently pack the material against the PRF barrier until 5 mm of MTA was placed. The placement of MTA was checked for appropriateness or any material extrusion by digital radiography.
The remaining canal space was obturated with thermoplastic gutta-percha (EQV, Meta Biomed, Korea) and AH Plus sealer (Dentsply Sirona, Maillefer, Switzerland). A composite and bonding system (GC, Tokyo, Japan) was used to restore the access cavity after ensuring obturation quality via digital radiography.
Periodical follow-up periods of 1 month, 2 months, 3 months, and 6 months were scheduled for collecting the clinical and radiographical findings (using the individual bite registration impressions). Clinical symptoms such as postoperative pain and analgesic consumption, pain upon palpation or percussion, and sinus tract were recorded. Treatment failure was confirmed if any of the above clinical symptoms existed. Certain dimensions of the periapical lesion were measured to obtain the data for analysis. The dimension was determined as the largest distance of the segment from the two intersections between the lesion circumferential and the line drawn perpendicular to the root axis (Fig. 1). Radiographic success was confirmed if the dimension was reduced or unchanged. All measurements were conducted by the same operator, and the Kappa (for clinical symptoms) or Intra-class correlation (for radiographic dimensions) coefficient was used to evaluate intra-examiner agreement. All horizontal dimensions of the periapical lesions were remeasured by the same examiner after each two-week period, following the periodic examinations to calculate the intra-class correlation coefficients.
All the statistical analyses were performed using IBM SPSS Statistics version 27 (IBM, Armonk, NY, US), with a significance level of p < .05. The data were first tested for normality by the Shapiro–Wilk test or paired t test. If the data were not normally distributed, they were analyzed using the Friedman and Dunn–Bonferroni post hoc correction.
Results
The Kappa and Intra-class correlation coefficients were greater than 0.9 for the examiner.
The horizontal dimensions of the periapical lesions on the radiographs are displayed and analyzed in Table 1.
There was a width of nearly ten millimeters at the diagnostic stage, and the patient was completely cured after all at 6 months. In fact, the patient healed within the first few months because of the continuous reduction in the periapical lesion width. The lesion width reached a small value at 3 months and nearly reached zero at 6 months of follow-up, which indicated that all lesions had progressed and cured during the investigated examinations.
The results revealed that there were significant differences among the horizontal dimensions of periapical lesions on digital radiographs at the different investigated time points (P < .05).
The horizontal dimensions were successively reduced at each periodic radiographic measurement. This proves that the healing process has successfully and firmly progressed.
The differences in the width of the periapical lesions are displayed and analyzed in Table 2.
The Dunn–Bonferroni post hoc correction revealed that there were significant differences among the five pairs of values at the examined periodic measurements (P < .05). This result proves that the curing process has been continuously occurring in a positive direction, with significant improvement occurring through every successive periodical examination.
The dimensional differences between the two successive periodic examinations are displayed in Table 3.
There were significant differences in the width of the periapical lesions among the periods of periodic examination (P < .05).
The differences in the width of the periapical lesion between the two successive periodic examinations are further analyzed in Table 4.
The Dunn–Bonferroni post hoc correction revealed that there was a significant difference in one pair of measurements between the two successive periodic examinations for each period of periodic examination. The results demonstrated that the lesion dimensions decreased rapidly in the first month and then decreased at a slower rate in the last month.
Between the 3- and 6-month periodic examinations, the mean difference in the reduction in lesion width was nearly zero, which indicated that there was no further room for reduction in lesion width. The differences in the decreases in the first period are greater than those in the last period, which means that the healing process is rapid in the first month.
The first signs of continuing formation of the root end were observed in the second month after completion of the procedure. The continuing creation of the root end in the present study has proven that this nonsurgical endodontic procedure is definitely the regenerative approach, according to contemporary knowledge. This firm evidence has been fundamental for modern knowledge in the evaluation of certain approaches to regenerative concepts in root canal therapy.
Discussion
The results of the present study showed that all treated patients healed at different levels at periodical evaluations of both periapical digital radiographs and clinical signs.
Table 1 reveals that there are significant differences in lesion width among the different examination times according to the digital radiographs, and these measurements were continuously reduced throughout the investigated periods. The difference in lesion width occurred immediately after the first month, regardless of sex, age, or tooth type. The results of Table 2 reveals that the amplitude of this difference is greater than that of the other fluctuations during the following periodic examinations. These results prove the strong reaction of periapical lesions to the combination of the two modalities of PRF and MTA and indicate another proper treatment option for teeth with open apices and periapical radiolucent lesions. On the radiographs, not only was the horizontal dimension reduced but also the vertical dimension decreased. The periapical lesion image was changed from a radiolucent area to a radiopaque area throughout the examination period. Along with the change in the periapical digital radiograph, clinical symptoms did not occur immediately after the first month, and there were no other negative clinical signs on subsequent periodic examinations. Therefore, the success rate of nonsurgical endodontic procedures can reach 100%.
The procedure that was described in the present study is independent of root canal enlargement, which requires rotary nickel-titanium instruments [11, 12]. The irrigation protocol is important for this kind of nonsurgical endodontic procedure. All disinfected solutions were kept inside the root canal space to ensure no further irritation of the periapical tissue. This is a difficult task because of the wide open apical foramen facilitating the outflow of the irrigation solution at all times. These irrigation solutions should be sufficiently and properly activated to obtain enough water. The concentration of the irrigation solution should not have been high, as approximately 2% is reasonable.
A dental operating microscope with proper magnification is essential, indispensable, and invaluable in this delicate, complicated, and difficult procedure. Almost normal routine instruments could have been used for this special procedure, as long as the field of view was clear and illuminated enough. Unless the MTA carrier is used for insertion into the apical region, there is no further need for any other special instruments, as with microsurgical procedures under a dental operating microscope, where special microinstruments are indispensable [17]. Manipulation of a dental operating microscope for the present procedure has made working length determination less complicated [18]. The operator could clearly observe the length of the root canal from the occlusal surface through the apical foramen. The length of the root canal could be measured directly using a proper plugger and reconfirmed via periapical digital radiography. The electronic apex locator becomes redundant in these circumstances.
Illumination has been a very important factor in this nonsurgical endodontic procedure. Manipulation of the periapical region in the present protocol requires maximum light intensity to ensure clear vision in the field of view [17, 19]. However, periapical tissue should not be illuminated with high light intensity because this is a living tissue; much or less, it has been affected by high light intensity. Therefore, the field of view was intermittently illuminated by the on and off buttons or by the light intensity change knob on the body of the dental operating microscope. Sometimes, the right direction of the light into the periapical region is modified simply by changing the angle of the dental mirror whenever the operator desires it. The contrast filter of the dental operating microscope is sometimes used for temporarily adjusting the light intensity. Because almost all the teeth recruited into the study were lower teeth, the posture of the mandibular and, therefore, the position of the head of the patient was adjusted to the uncomfortable location. However, patient cooperation has been very good for nonsurgically sensitive endodontic treatment [17, 20].
The fluid squeezed from the PRF membranes was clearly observed by the operator and could be evaluated exactly until the PRF membranes were sufficient for the beginning of MTA placement.
Indirect vision in the dark, wet, complicated apical region requires a powerful light source and suitable magnification that cannot be achieved by conventional dental light or a normal head loupe even with enhanced illumination. This procedure is not difficult if the operator has been fully trained in a reasonable amount of time [17, 18, 20].
Blood sample preparation is a rather uncomfortable issue for adolescents and their parents in Vietnamese culture. A sample of ten millimeters of blood is a barrier to parental consensus because of the fear of disease. An increase in the amount of blood is uncomfortable for parents [21]. Several patients declined to enrol in the study because of the ten millimeters of blood sample needed for nonsurgical endodontic procedures. For fresh and immediate PRF blocks to manipulate the process, blood is withdrawn from the patient simultaneously with the endodontic progress to ensure a smooth journey from the beginning of the procedure to the insertion of pieces of PRF membranes into the periapical region [21].
Once the PRF block was extracted, it was then placed under the cover of the box for two minutes to create the PRF membrane. Preparation of the root canal and periapical region was accomplished before the PRF membrane was cut into 3 mm × 3 mm pieces for easier insertion into the periapical region.
The PRF membrane used in the present study was constructed with a box instrument accompanied by a centrifuge machine [22]. The steel plane is properly designated for the formation of the PRF membrane once the membrane is withdrawn from the vacuum sterile tube. The dimension of the piece of the PRF membrane correlates with the size of the apical foramen for each circumstance and facilitates the manipulation of the insertion through the foramen. The size of the plugger is suitable for the apical foramen because it does not further damage the delicate dentinal wall of the apical third [11, 12].
The patient posture during the procedure is certainly uncomfortable because of the time-consuming nature of the procedure and the unfavorable mandibular tooth position [19].
The results of the present study revealed that although PRF is an autogenous substance, the healing process time is not rapid enough compared with that of the collagen membrane used in a previous study [1]. Although PRF has certain advantages over collagen membranes, the manipulation of this autogenous material requires a strictly sterilized environment [11], leading to difficulty in normalizing the procedure in common clinical situations.
Once the apical barrier of the PRF membrane has been confirmed, the insertion of MTA into the desired position in the apical third of the root canal has not been further complicated. MTA could be carried out using an MTA carrier, a hand spiral instrument, or even ultrasonic energy, with the hope of a better result [23].
The MTA used for the apical plug was chosen for discoloration of the dental structure, especially for the anterior tooth. Although calcium silicate-based cement is placed only in the apical third, discoloration of the coronal portion of the tooth should be considered an adverse effect during this procedure [10]. Modern MTA erases the discoloration of teeth and is a reasonable reason for its use in the clinical setting. The moisture environment required for the setting of the conventional MTA was eliminated during the manipulation of this modern MTA; therefore, the following appointment for treatment completion was unnecessary. Water is rapidly separated from the PRF membrane; therefore, this substance should be manipulated as soon as possible to establish a parched region, facilitating subsequent MTA placement. The volume of the PRF barrier should be extended further into the apical region to compensate for the shrinkage of the PRF block after compression by sterile cotton.
The apical MTA barrier combined with the PRF membrane offers a high chance of successful restoration of extremely weakening tooth structure compared with other long-term, multiple visits, such as calcium hydroxide apexification and apical closure regeneration. Once the tooth has been fully restored on time, its functional, aesthetic, and stable abilities can be restored and enhanced in terms of both function and aesthetics, ensuring the best outcome for this kind of nonsurgical conservative endodontic procedure [24].
The texture of the PRF membrane seems tougher than that of the collagen membrane under the conditions of these PRF extraction parameters. This characteristic facilitates the manipulation of PRF pieces in the delicate apical region, although fluid separates from the compressed substance during placement [22].
The estimation of the blood volume needed for PRF extraction is not an issue if a previous cone-beam computed tomography image is available. The dimensions of the periapical lesion could be estimated more exactly via CBCT than via conventional periapical digital radiography, as described in the present study. CBCT is a very good method for evaluating the reduction of periapical lesions in all three dimensions in space. Further investigations using CBCT should be performed to obtain additional details on the healing process of this nonsurgical endodontic procedure. However, there is concern as to the radiation exposure used in CBCT capture to ensure the As Low As Reasonably Achieve (ALARA) principle [25].
PRF loaded with antibiotics after oral surgery has been advocated for in recent studies because of its many advantages [26].
The firm evidence of root apex development in the present study contributes to the contemporary knowledge of the regenerative approach in endodontics.
The limitations of the present study include the small sample size, short follow-up period, small number of teeth, and the use of only periapical digital radiographs. Further investigations should be performed using other calcium silicate-based materials, other PRF forms, and a broader range of teeth and ages. Fluid separation from the PRF membrane should be investigated to confirm that there is no considerable effect on the quality of the PRF membrane compared to that of the PRF block.
The PRF membrane is a good autogenous substance for the apical barrier formation procedure for preventing apical extrusion of material used in the apical region.
Data availability
No datasets were generated or analysed during the current study.
Change history
09 March 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12903-024-04087-y
Abbreviations
- PRF:
-
platelet-rich fibrin
- RCF:
-
relative centrifugal force
- RPM:
-
Rotations Per Minute
- L-PRF:
-
Leukocyte Platelet Rich Fibrin
- A-PRF:
-
Advanced platelet-rich fibrin
- MTA:
-
mineral trioxide aggregate
- CBCT:
-
Cone-beam computed tomography
- ALARA:
-
As Low As Reasonably Achieve
References
Pham KV, Tran TA. Effectiveness of MTA apical plug in dens evaginatus with open apices. BMC Oral Health. 2021;21(1):566.
Frank AL. Therapy for the divergent pulpless tooth by continued apical formation. J Am Dent Assoc (1939). 1966;72(1):87–93.
Joshi SR, Palekar AU, Pendyala GS, Mopagar V, Padmawar N, Shah P. Clinical success of platelet-rich fibrin and Mineral Trioxide Aggregate (MTA) or MTA-like agents in Healing of Periapical Lesion in Nonsurgically treated Pulpless Immature Permanent Teeth: a systematic review. J Int Soc Prev Community Dentistry. 2020;10(4):379–83.
Namour M, Theys S. Pulp revascularization of immature permanent teeth: a review of the literature and a proposal of a new clinical protocol. TheScientificWorldJournal 2014, 2014:737503.
Roy S, Kumari A, Chandra P, Agarwal R, Bankoti P, Ahmed F. Evaluation of Healing of Periapical Tissue in Permanent incisors with Open Apices after Unintentional Extrusion of Mineral Trioxide Aggregate - A Retrospective Study. J Pharm Bioallied Sci. 2021;13(Suppl 1):97–s100.
Graziele Magro M, Carlos Kuga M, Adad Ricci W, Cristina Keine K, Rodrigues Tonetto M, Linares Lima S, Henrique Borges A, Garcia Belizário L. Coêlho Bandeca M: Endodontic Management of Open Apex Teeth using lyophilized collagen sponge and MTA cement: report of two cases. Iran Endodontic J. 2017;12(2):248–52.
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics 2006, 101(3):e37–44.
Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, Fujioka-Kobayashi M, Bishara M, Zhang Y, Wang H-L, et al. Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Invest. 2017;21(6):1913–27.
Sabeti MA, Lee ES, Torabinejad M. PRF applications in endodontics. Quintessence Publishing Company, Incorporated; 2020.
Wang X, Xiao Y, Song W, Ye L, Yang C, Xing Y, Yuan Z. Clinical application of calcium silicate-based bioceramics in endodontics. J Translational Med. 2023;21(1):853.
Sharma S, Sharma V, Passi D, Srivastava D, Grover S, Dutta SR. Large periapical or Cystic Lesions in Association with roots having Open Apices Managed Nonsurgically using 1-step apexification based on platelet-rich fibrin matrix and biodentine apical barrier: a Case Series. J Endod. 2018;44(1):179–85.
Yadav P, Pruthi PJ, Naval RR, Talwar S, Verma M. Novel use of platelet-rich fibrin matrix and MTA as an apical barrier in the management of a failed revascularization case. Dent Traumatol. 2015;31(4):328–31.
Miron RJ, Pinto NR, Quirynen M, Ghanaati S. Standardization of relative centrifugal forces in studies related to platelet-rich fibrin. J Periodontol. 2019;90(8):817–20.
Dhall S, Mittal R, Tandan M. Single-visit apexification with Biodentine and Platelet-Rich Fibrin. J Dent Res Rev 2020, 7(4).
Dubey J, Saini R, Gaur A, Dutta A. Single-visit apexification by Platelet-Rich Fibrin and Biodentin - A Case Report. Asian J Dent Sci. 2023;6(1):67–72.
Priyanka A. One step apexification in a resorbed tooth using autologous PRF as internal matrix and biodentine apical Plug. Univ J Dent Sci 2022, 9(1).
Liu B, Zhou X, Yue L, Hou B, Yu Q, Fan B, Wei X, Qiu L, Huang Z, Xia W, et al. Experts consensus on the procedure of dental operative microscope in endodontics and operative dentistry. Int J Oral Sci. 2023;15(1):43.
Jenner A, Ana J, Rafael G, Rodrigo V. Endodontics fine motor skills with the use of the conventional and 3D microscopy - a comparative study. Roots. 2022;18(2):6–9.
Isozaki H, Taniguchi T, Miake Y. A STUDY OF ERGONOMIC POSTURE IN MICROSCOPIC DENTISTRY. Int J Microdentistry. 2022;13(2):74–83.
Jalali P, Kim C, Woodmansey K. Comparison of optical performance among three dental operating microscopes: a pilot study. J Conservative Dentistry. 2020;23:374.
Thakkar S, Naik S, Nadig B, Bellal S, Thaliyil A. A comparative clinico-radiographic analysis of regenerative endodontic procedure on immature necrotic permanent teeth using blood clot and PRF as scaffold: a retrospective study. Saudi Dent J. 2023;35(6):753–9.
Algahtani FN, Almohareb R, Aljamie M, Alkhunaini N, Barakat SSAL. Application of advanced platelet-rich fibrin for through-and-through bony defect during endodontic surgery: three case reports and review of the literature. World J Clin Cases. 2023;11(17):4168–78.
Chen S-J, Chen L-P. Radiographic outcome of necrotic immature teeth treated with two endodontic techniques: a retrospective analysis. Biomedical J. 2016;39(5):366–71.
Lee L-W, Hsieh S-C, Lin Y-H, Huang C-F, Hsiao S-H, Hung W-C. Comparison of clinical outcomes for 40 necrotic immature permanent incisors treated with calcium hydroxide or mineral trioxide aggregate apexification/apexogenesis. J Formos Med Assoc. 2015;114(2):139–46.
Beach DA. CBCT Use in Endodontic diagnosis. Dent Today. 2016;35(2):80.
Bennardo F, Gallelli L, Palleria C, Colosimo M, Fortunato L, De Sarro G, et al. Can platelet-rich fibrin act as a natural carrier for antibiotics delivery? A proof-of-concept study for oral surgical procedures. BMC Oral Health. 2023;23(1):134.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
V-K.P. designed, conceived, wrote the original, reviewed, and approved the manuscript. M-H.T., N-P.N., and T-A-T.T. performed, data collected, review, and approved the manuscript. A-T.P. and T-L-K.P. wrote the original manuscript, data collected, reviewed, and approved the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the University of Medicine and Pharmacy at Ho Chi Minh City, Viet Nam, with the approval number of 236/ĐHYD-HĐĐĐ, the informed consent was obtained from parents of all participants, or participant herself, and all methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Informed consent had been obtained from all subjects and/or their legal guardian(s) for publication of identifying information/images in an online open-access publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pham, VK., Pham, TLK., Pham, AT. et al. Platelet rich fibrin and MTA in the treatment of teeth with open apices. BMC Oral Health 24, 230 (2024). https://doi.org/10.1186/s12903-024-03923-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-03923-5