Abstract
Aim
The purpose of this study was to i) synthesise TEGDMA-DHEPT microcapsules in a laboratory setting; ii) characterise the resultant microcapsules for quality measures.
Materials & methods
Microcapsules were prepared by in situ polymerization of PUF shells. Microcapsules characterisation include size analysis, optical and SEM microscopy to measure the diameter and analyse the morphology of PUF microcapsules. FT-IR spectrometer evaluated microcapsules and benzyl peroxide catalyst polymerization independently.
Result
Average diameter of TEGDMA-DHEPT microcapsules was 120 ± 45 μm (n: 100). SEM imaging of the capsular shell revealed a smooth outer surface with deposits of PUF nanoparticles that facilitate resin matrix retention to the microcapsules upon composite fracture. FT-IR spectra showed that microcapsules crushed with BPO catalyst had degree of conversion reached to 60.3%.
Conclusion
TEGDMA-DHEPT microcapsules were synthesised according to the selected parameters. The synthesised microcapsules have a self-healing potential when embedded into dental resin composite as will be demonstrated in our future work.
Graphical Abstract
Graphical abstract showing the microcapsule components. The shell contains poly(urea-formaldehyde), and the core consists of TEGDMA-DHEPT healing agents.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Dental resin restorations have been shown to encounter two main downsides: secondary caries and bulk fractures [1]. They frequently fail due to the accumulation of micro-cracks generated from masticatory forces and thermal stresses [2]. Self-healing composites and polymers involving microencapsulated healing liquids demonstrate the capability for providing long-life structural materials, with the potential to repair crack damage and recover mechanical performance in polymeric materials [3].
Self-healing systems to date are bioinspired from autonomic repair mechanisms in living tissues such as broken bone healing or/and soft tissue healing processes, with an effort to mimic natural components and implement self-healing capabilities into resin polymers [4,5,6,7,8]. Self-healing mechanisms have been achieved in bulk thermosetting polymers [9,10,11,12,13], self-healing fibre-reinforced composites [14,15,16,17,18,19], self-healing dental resin composites [20,21,22,23,24], self-healing adhesives [25], self-healing bonding resins [26], elastomers [27, 28] and coatings [29]. Self-healing approaches may involve hollow fibres [16, 17, 30, 31], nano-fibres [32, 33], microcapsules [3, 12, 14, 20, 22, 23, 34,35,36], nano-capsules [26, 37,38,39], or solid-state repairable polymers (heat application) [40, 41].
Microencapsulation is defined as “a technology of packaging solids, liquids or gaseous materials in miniature, sealed capsules that can release their contents at controlled rates under the influence of specific conditions” [42]. This is a promising approach to increasing the durability of resin composites as the microcapsules will rupture and release of polymerisable healing agents to seal and stop crack propagation when the composite is subjected to fracture [3, 14, 22].
Technological advances in microencapsulation methods have been introduced; allowing a higher level of standardisation in microencapsulation process. Published reports of lab-based microcapsules synthesis vary but include microfluidic (micro-channels) encapsulation method, mostly used in biological substances, controlled drug release and pharmaceuticals [43,44,45]. Although a higher precision can be achieved with microfluidics system, the microchannels are at a higher risk of clogging by PUF shell polymerization during microencapsulation which might be a limiting factor.
Studies have reported the incorporation of poly(urea-formaldehyde) PUF microcapsules encapsulating triethylene glycol dimethacrylate (TEGDMA) monomer and N,N-dihydroxyethyl-p-toluidine (DHEPT) tertiary amine accelerator as healing agents in self-healing dental composite [21,22,23]. Also, benzoyl peroxide (BPO) catalyst is an essential part of the resin matrix, functioning as a self-healing initiator, facilitating the chemical polymerization of the healing agents involved in the microcapsules [21,22,23]. A successful self-healing efficacy and recovery of the virgin fracture toughness (KIC) of approximately 65% have been reported [22]. The materials involved in self-healing dental composite have proven biocompatibility for dental use [22], however, further investigation is necessary before any in vivo studies in order to rule out the risk of cytotoxic unreacted free formaldehyde [46].
In the present study, the aims were to synthesise and characterise TEGDMA-DHEPT microcapsules, including optimisation of in situ emulsion polymerization of PUF shells, size analysis, optical and SEM imaging, and FT-IR of crushed microcapsules with BPO catalyst.
Materials and methods
Raw materials
The microcapsule shells were composed of urea, ammonium chloride, resorcinol and a 37% aqueous solution of formaldehyde (Sigma–Aldrich Company Ltd., Dorset, UK). The healing agent was a mixture of N,N-dihydroxyethyl-p-toluidine (DHEPT) amine (Esschem Europe Ltd., Seaham, UK) and triethylene glycol dimethacrylate (TEGDMA) monomer (Sigma–Aldrich Company Ltd., Dorset, UK). The surfactant used is poly (ethylene-alt-maleic anhydride) (EMA) (Average Mw 100,000–500.000 powder) (Sigma–Aldrich Company Ltd., Dorset, UK). pH regulators were hydrochloric acid (HCl) and sodium hydroxide (NaOH) 1 M solutions (Sigma–Aldrich Company Ltd., Dorset, UK). The chemical catalyst was benzoyl peroxide (BPO) (Sigma–Aldrich Company Ltd., Dorset, UK). All chemicals were analytical grade and used as received with no further purification.
Synthesis of microcapsules
Microcapsules were prepared by in situ polymerization in an oil-in-water (O/W) emulsion (Fig. 1). At room temperature, 100 mL of distilled water and 26 mL of 2.5 wt% aqueous solution of poly (ethylene co-maleic anhydride) (EMA) copolymer were mixed into a 400 mL beaker flask. The beaker was held in a water bath on a hotplate with a digital display of temperature (Carousel tech stirring hotplate, Radleys, UK). A mechanical stirrer was used to agitate the solution, driving a four-bladed PTFE (40 mm) low-shear mixing propeller positioned just above the bottom of the beaker (Eurostar, IKA Ltd., UK). The stirring speed was set to 400 rpm. Then, 2.50 g urea, 0.25 g ammonium chloride and 0.25 g resorcinol were added into the flask. After dissolution of solids, the pH was checked and adjusted to 3.5 via drop-wise addition of 1 M NaOH solution.
Afterwards, the stirring speed was increased to 500 rpm. The healing liquid consisted of TEGDMA monomer and 1 wt% DHEPT amine. A slow stream of 60 mL of TEGDMA-DHEPT liquid was introduced to the reaction flask. After 10 min of stirring, a stabilised emulsion of fine TEGDMA-DHEPT droplets was formed. Then, 6.30 g of 37% aqueous solution of formaldehyde was added, and the flask was sealed with aluminium foil to prevent evaporation. The target temperature in the flask was 55–60 °C; an external temperature probe was placed in the bath for further confirmation.
The shell materials of the microcapsules were isothermally polymerised under continuous agitation. After 4 h, the suspension of microcapsules was left to cool to ambient temperature. Then, filtration through centrifugation and sedimentation were employed. The microcapsules suspension was centrifuged with distilled water. This process was repeated 5 times, for each 5 min cycle the solution was replaced with fresh distilled water in order to remove the remnant surfactant. Sieving of the microcapsules was undertaken with rinsing with distilled water repeatedly throughout the sieving process, microcapsules were then left to dry for 24 h.
Microcapsules characterisation
Sizing of microcapsules
In order to separate the microcapsules according to size, a vibratory sieve shaker (Retsch® AS 200 digital, Retsch Limited, UK) was used. Four different sieves were used (45, 90, 150 and 300 μm pores sizes). The suspension of microcapsules was poured into the sieves and left for 30 min in the shaker (amplitude of 70% - 2.1 out of 3 mm). The microcapsules were allowed to dry overnight. Microcapsules were then collected with a plastic spatula into four glass bottles according to the sieve size and weighed.
Imaging analysis
An optical microscope (Leica DMI6000 B, Germany) was used to assess the encapsulation process, and to confirm the diameter of the microcapsules by image processing software (ImageJ, NIH Image). Following that, microcapsule surface morphology and further size analysis were conducted using a scanning electron microscope (Zeiss EVO60, Germany). A small number of microcapsules were spread onto adhesive tape and sputter-coated with gold (7 nm).
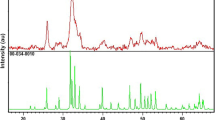
Degree of conversion of the microcapsules with the catalyst
An FT-IR spectrometer has been used to measure the degree of polymerization of TEGDMA-DHEPT healing agents with benzoyl peroxide catalyst (Avatar 360, Nicolete Analytical Instrument, Thermo Electron Corp., Cambridge, UK). A mixture of microcapsules and 0.5 wt% of BPO were broken in an agate mortar and pestle grinding bowl then placed and pressed in a PTFE disc mould (4 mm internal diameter, 0.5 mm height). Another PTFE disc mould (4 mm internal diameter, 2 mm height) was also used to test the polymerization of this mixture in 2 mm depth. The spectra were recorded over the range of 4000 to 400 cm−1 with 32 scans at a resolution of 4 cm−1, the degree of conversion (DC) of TEGDMA monomer was calculated from the peak intensity ratio of C=C at 1637 cm−1 against the internal standard peak of C=O at 1715 cm−1 immediately post-curing and 24 h after polymerization [47].
Results
Microcapsules characterisation
Size analysis
Synthesis of TEGDMA-DHEPT microcapsules was achieved by in situ polymerization to form poly(urea-formaldehyde) capsular shells. The distribution of microcapsule showed, a small number of microcapsules had a diameter between 45 μm to 90 μm. The size range of most microcapsules was 150 μm to 300 μm (Fig. 2).
Microcapsules imaging
After the filtration process, microcapsules presented as a white powder (Fig. 3, A). However, a number of the synthesised microcapsule batches showed as agglomerated and clustered particles (Fig. 3, B). Optical imaging further confirmed microcapsule sizes (as quantified in two dimensional planes of the sphere and averaged for each microcapsule); this revealed a diameter average of 120 ± 45 μm (n: 100). It is also showed an outer black ring that indicates shell formation and a moderately brighter area interiorly representing the encapsulated healing agents (Fig. 3, C and D).
Self-healing TEGDMA-DHEPT microcapsules prepared via polymerization in situ;(A) Microcapsules presented as a free-flowing white powder, (B) poor quality microcapsules batch showing agglomerated and fused microparticles, (C and D) Optical microscope images presenting capsular shells as a dark outer ring, encapsulating the healing agents of a lighter shade opacity
SEM showed a uniform external surface without voids detectable. The microcapsule diameter (Fig. 4, A), was estimated to be around 150 ± 50 μm (n: 100). The smooth external wall forms a rough surface morphology with the presence of PUF nanoparticles. (Fig. 4, B).
Degree of conversion of the microcapsules with the catalyst
The healing agents TEGDMA-DHEPT successfully polymerised in both 0.5 mm and 2 mm specimens after 24 h, showing a degree of conversion of 60.3 and 34.8% respectively. The analysis of the final polymer spectra confirmed the reactivity of the microcapsules after being crushed and mixed with BPO catalyst.
Discussion
Self-healing composites and polymers, which incorporate microencapsulated healing liquids, have shown great promise in providing durable structural materials. These materials have the ability to repair crack damage and restore mechanical performance in polymeric materials, offering the potential for long-lasting functionality [3]. In the present work, TEGDMA-DHEPT microcapsules were successfully synthesised via emulsion polymerization to achieve polymeric capsular shells [36, 48]. Microcapsules were prepared by in situ polymerization; EMA acts as a surfactant, which helps to form an O/W emulsion, the oil being TEGDMA-DHEPT liquid. The microcapsules consisted of poly(urea-formaldehyde) shells with TEGDMA monomer and 1 wt% DHEPT amine as healing agents.
The final product of microcapsules was a free-flowing white powder, however, some agglomerated microcapsules were also found. Clustered or fused microcapsules are not ideal, but upon microcapsules dispersion into resin matrix, even distribution was achieved. One of the key factors for the creation of free-flowing microcapsules is the filtration process, which is a very sensitive and delicate procedure [36]. Poor filtration can result in an over-dryness of the microcapsules and may affect the permeability of the capsular shells by opening the shell pores. As a result, the microcapsules can become yellowish with time, due to healing liquid leaking through the shells resulting in the agglomeration and fusion of the microcapsules together.
Microcapsule size is an important factor to allow the encapsulation of sufficient healing agents to achieve self-healing capability in resin-based matrix. Smaller-sized microcapsules ≤70 μm will not be able to fill a crack due to the small amount of healing liquid. However, larger-sized microcapsules ≥300 μm will negatively impact the polymer matrix strength which may lead to voids following microcapsules rupture, resulting in deterioration of the mechanical properties of the polymeric material [49]. Microcapsule diameter can be controlled by stirring speed; an average diameter of 10–1000 μm was obtained by 200–2000 rpm [36]. A stirring speed of 500 rpm was set to obtain an average diameter of 150 μm microcapsules. Then, microcapsules were sieved using different sieves according to their capsular size, and showed the range was more of 150–300 μm microcapsule sizes. This technique was found to be a reliable and repeatable method for size sorting according to the anticipated application in resin-based materials. Optical or SEM microscopy can also be used to quantify microcapsule surface diameter although is time-consuming and requires the examination of several hundreds of particles to obtain statistically representative data. Optical and SEM imaging have also confirmed the microcapsules diameter ranging from 120 ± 45 μm to 150 ± 50 μm. Previous studies manufactured microcapsules with a similar diameter of 150–200 μm [36], or a smaller diameter of ≤70 μm microcapsules by using a higher stirring speed [22, 36].
Shell thickness of microcapsules is of a vital importance; it has been reported that if too thin, shells are more prone to breakdown during resin paste mixing, handling and packing [22]. However, if too thick, shells are more resistant to rupture upon composite fracture, which will prevent the delivery of healing liquid to the crack. Previous studies have reported an average shell thickness of 160–230 nm with DCPD or TEGDMA-DHEPT microcapsule, and showed that microcapsules ruptured upon composite fracture and self-healing capability was achieved [3, 22, 36].
SEM imaging showed that PUF nanoparticles existed on the external surface of the capsular shells. Deposition and aggregation of higher molecular weight pre-polymer on the outer PUF capsular surface during in situ polymerization resulted in a rough and porous surface morphology [36]. The inner shell surface was a smooth non-porous wall as a result of low molecular weight pre-polymer deposition. PUF nanoparticles on the outer surface of the microcapsules can facilitate mechanical interlocking interface (micromechanical retention) to the host resin polymer matrix upon photo activation (light-curing) [22]. This retention interface will allow the microcapsules to break when subjected to cracking. If the outer surface of the microcapsules had a smooth, non-porous morphology, the interlocking interface will be missing and the crack may bypass the microcapsules without breaking them, resulting in no healing liquid to fill the crack [22].
The ability of TEGDMA-DHEPT microcapsules to polymerise when crushed and mixed with 0.5 wt% benzoyl peroxide (BPO) catalyst was reported. BPO within the host polymeric material promotes the chemical reaction by free radical polymerization when it reacts with tertiary aromatic amine DHEPT in the healing liquid inside the ruptured microcapsules. An FT-IT spectral analysis was conducted within the range of 4000 to 400 cm−1, utilizing 32 scans at a resolution of 4 cm−1. To determine the degree of conversion (DC) of TEGDMA monomer, the peak intensity ratio of C=C at 1637 cm-1 was compared to the internal standard peak of C=O at 1715 cm-1. This comparison was done both immediately after curing and 24 hours after polymerization. In another study involving TEGDMA-DHEPT microcapsules, similar findings were observed [47]. A degree of conversion of 60.3% (in 0.5 mm depth) and 34.8% (in 2 mm depth) were obtained after 24 h self-cure at room temperature. Similar findings were reported by a recent study involving TEGDMA-DHEPT microcapsules crushed with 1 wt% BPO; a DC of 67.2% was reported [22]. In general, dimethacrylate resins have residual unsaturated monomers in the final polymerised resin matrix which can reach up to 43% [50]. In service, it is important to investigate how the reparative resin is released, rate of release, and the extent of mixing with BPO initiator. Also, the consequences of homopolymerization of TEGDMA as a reparative resin should be addressed, along with reaction kinetics of low molecular weight, high mobility resins and cyclisation reaction.
The current study used dental materials including TEGDMA monomer and DHEPT amine in the microcapsules and BPO catalyst within the resin composite matrix. The materials used have been approved by the Food and Drug Administration, and are available in commercial resin-based dental composites. Human gingival fibroblast cytotoxicity tests in vitro have shown that TEGDMA-DHEPT microcapsules exhibit an acceptable biocompatibility, hence the incorporation of microcapsules in resin does not drastically compromise cell viability [22], although the possibility of leakage of unreacted free formaldehyde from PUF shells should be taken under consideration for cytotoxicity testing.
Conclusion
TEGDMA-DHEPT microcapsules were successfully synthesised by in situ polymerization of an O/W emulsion. The microcapsules have the ability to polymerise when they are ruptured and triggered by a BPO catalyst in the host composite. Microcapsule sizes ranged between 150 and 300 μm with an average of 120 ± 45 μm (n: 100). The morphology analysis showed a rough outer shell due to the presence of PUF nanoparticles. Microcapsules and BPO mixture showed a degree of conversion reached up to 60.3%, which confirms encapsulation of the healing agents and proves functionality of the microcapsules.
The incorporation of TEGDMA-DHEPT microcapsules in a self-healing dental composite model will be presented in our future studies. As yet, cytotoxicity testing should be conducted, considering the unreacted free formaldehyde in the PUF shells of microcapsules.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Demarco FF, et al. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28(1):87–101.
Baran G, Boberick K, McCool J. Fatigue of restorative materials. Crit Rev Oral Biol Med. 2001;12(4):350–60.
White SR, et al. Autonomic healing of polymer composites. Nature. 2001;409(6822):794–7.
Brochu AB, Craig SL, Reichert WM. Self-healing biomaterials. J Biomed Mater Res A. 2011;96(2):492–506.
Esser-Kahn AP, et al. Three-dimensional microvascular Fiber-reinforced composites. Adv Mater. 2011;23(32):3654–8.
Hager MD, et al. Self-healing materials. Adv Mater. 2010;22(47):5424–30.
Diesendruck CE, et al. Biomimetic self-healing. Angew Chem Int Ed. 2015;54(36):10428–47.
Zhao N, et al. Bioinspired materials: from low to high dimensional structure. Adv Mater. 2014;26(41):6994–7017.
Brown EN, Sottos NR, White SR. Fracture testing of a self-healing polymer composite. Exp Mech. 2002;42(4):372–9.
Caruso MM, et al. Solvent-promoted self-healing epoxy materials. Macromolecules. 2007;40(25):8830–2.
Caruso MM, et al. Full recovery of fracture toughness using a nontoxic solvent-based self-healing system. Adv Funct Mater. 2008;18(13):1898–904.
Blaiszik B, et al. Microcapsules filled with reactive solutions for self-healing materials. Polymer. 2009;50(4):990–7.
Wilson GO, et al. Autonomic healing of epoxy vinyl esters via ring opening metathesis polymerization. Adv Funct Mater. 2008;18(1):44–52.
Kessler M, Sottos N, White S. Self-healing structural composite materials. Compos A: Appl Sci Manuf. 2003;34(8):743–53.
Kessler M, White S. Self-activated healing of delamination damage in woven composites. Compos A: Appl Sci Manuf. 2001;32(5):683–99.
Pang JW, Bond I. A hollow fibre reinforced polymer composite encompassing self-healing and enhanced damage visibility. Compos Sci Technol. 2005;65(11):1791–9.
Pang J, Bond I. ‘Bleeding composites’—damage detection and self-repair using a biomimetic approach. Compos A: Appl Sci Manuf. 2005;36(2):183–8.
Moll JL, White SR, Sottos NR. A self-sealing fiber-reinforced composite. J Compos Mater. 2010;0:1–11.
Alshabib A, Jurado CA, Tsujimoto AJDMJ. Short fiber-reinforced resin-based composites (SFRCs); Current status and future perspectives. Dent Mater J. 2022;41(5):647–54.
Wertzberger BE, et al. Physical characterization of a self-healing dental restorative material. J Appl Polym Sci. 2010;118(1):428–34.
Wu J, et al. Development of novel self-healing and antibacterial dental composite containing calcium phosphate nanoparticles. J Dent. 2015;43(3):317–26.
Wu J, et al. Novel self-healing dental resin with microcapsules of polymerizable triethylene glycol dimethacrylate and N, N-dihydroxyethyl-p-toluidine. Dent Mater. 2016;32(2):294–304.
Wu J, et al. Effects of water-aging on self-healing dental composite containing microcapsules. J Dent. 2016;47:86–93.
Abid Althaqafi K, et al. Properties of a model self-healing microcapsule-based dental composite reinforced with silica nanoparticles. J Funct Biomater. 2022;13(1):19.
Miller GM, et al. Self-healing adhesive film for composite laminate repairs on metallic structures. Master of Science Thesis. Department of Aerospace Engineering, University of Illinois at Urbana-Champaign; 2007.
Ouyang X, et al. Synthesis and characterization of triethylene glycol dimethacrylate nanocapsules used in a self-healing bonding resin. J Dent. 2011;39(12):825–33.
Keller M, White S, Sottos N. Torsion fatigue response of self-healing poly (dimethylsiloxane) elastomers. Polymer. 2008;49(13):3136–45.
Keller MW, White SR, Sottos NR. A self-healing poly (dimethyl siloxane) elastomer. Adv Funct Mater. 2007;17(14):2399–404.
Cho SH, et al. Polydimethylsiloxane-based self-healing materials. Adv Mater. 2006;18(8):997–1000.
Dry CM. Smart materials which sense, activate and repair damage: Hollow Porous Fibers in Composites Release chemicals from fibers for self-healing, damage prevention, and/or dynamic Controll. In SPIE Digital Library. 1992.
Trask R, Bond I. Biomimetic self-healing of advanced composite structures using hollow glass fibres. Smart Mater Struct. 2006;15(3):704.
Lee MW, et al. Self-healing nanofiber-reinforced polymer composites. 1. Tensile testing and recovery of mechanical properties. ACS Appl Mater Interfaces. 2015;7(35):19546–54.
Lee MW, et al. Self-healing nanofiber-reinforced polymer composites. 2. Delamination/Debonding and adhesive and cohesive properties. ACS Appl Mater Interfaces. 2015;7(35):19555–61.
Blaiszik B, et al. Self-healing polymers and composites. Annu Rev Mater Res. 2010;40:179–211.
Huyang G, Debertin AE, Sun J. Design and development of self-healing dental composites. Mater Des. 2016;94:295–302.
Brown EN, et al. In situ poly (urea-formaldehyde) microencapsulation of dicyclopentadiene. J Microencapsul. 2003;20(6):719–30.
Blaiszik B, Sottos N, White S. Nanocapsules for self-healing materials. Compos Sci Technol. 2008;68(3):978–86.
Lee JY, Buxton GA, Balazs AC. Using nanoparticles to create self-healing composites. J Chem Phys. 2004;121(11):5531–40.
Blaiszik BJ, White SR, Sottos NR. Nanocapsules for self-healing composites. Proceedings of the 2006 SEM Annual Conference and Exposition on Experimental and Applied Mechanics. Vol 1. 2006.
Yin T, et al. Self-healing epoxy composites–preparation and effect of the healant consisting of microencapsulated epoxy and latent curing agent. Compos Sci Technol. 2007;67(2):201–12.
Hayes S, et al. Self-healing of damage in fibre-reinforced polymer-matrix composites. J R Soc Interface. 2007;4(13):381–7.
Anal AK, Singh H. Recent advances in microencapsulation of probiotics for industrial applications and targeted delivery. Trends Food Sci Technol. 2007;18(5):240–51.
Omi S. Preparation of monodisperse microspheres using the Shirasu porous glass emulsification technique. Colloids Surf A Physicochem Eng Asp. 1996;109:97–107.
Yuan Q, Williams RA. Large scale manufacture of magnetic polymer particles using membranes and microfluidic devices. China Particuology. 2007;5(1–2):26–42.
Yuan Q, Williams RA, Biggs S. Surfactant selection for accurate size control of microcapsules using membrane emulsification. Colloids Surf A Physicochem Eng Asp. 2009;347(1–3):97–103.
Duong A, et al. Reproductive and developmental toxicity of formaldehyde: a systematic review. J Mutat Res/Rev Mutat Res. 2011;728(3):118–38.
Collares FM, et al. Discrepancies in degree of conversion measurements by FTIR. Braz Oral Res. 2014;28(1):9–15.
Asua JM. Miniemulsion polymerization. Prog Polym Sci. 2002;27(7):1283–346.
Trask R, Williams H, Bond I. Self-healing polymer composites: mimicking nature to enhance performance. Bioinspir Biomim. 2007;2(1):1–9.
Moldovan M, et al. Evaluation of the degree of conversion, residual monomers and mechanical properties of some light-cured dental resin composites. Materials. 2019;12(13):2109.
Funding
This research was funded by Ministry of Education in Saudi Arabia, grant number IFKSUOR3-168-4.
Author information
Authors and Affiliations
Contributions
Conceptualization, K.T. and A.S.; methodology, N.S. and J.S.; investigation,K.T , A.S.; writing—original draft preparation,K.T. writing—review and editing, N.S, AS and JS.; supervision, N.S. and J.S.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Althaqafi, K.A., Satterthwaite, J., AlShabib, A. et al. Synthesis and characterisation of microcapsules for self-healing dental resin composites. BMC Oral Health 24, 109 (2024). https://doi.org/10.1186/s12903-023-03764-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03764-8