Abstract
Background
The neck management of clinical-nodal negative (cN0) oral squamous cell carcinoma (OSCC) remains controversial. Elective neck dissection (END) and observation are the main strategies, but it is still not clear who could benefit the most from END. The purpose of this study was to clarify the potential clinical factors that affect the therapeutic value of END and to explore the actual characteristics associated with benefit from END.
Methods
Patients with cN0 OSCC were identified in the SEER database from 2000 to 2019. 5-year Overall survival (OS) and disease-specific survival (DSS) were analyzed using the Kaplan‒Meier method, and the hazard ratios (HRs) for survival were estimated using the Cox regression model. Multiple subgroup analyses of DSS and OS among different factors, comparing END and No END, were performed.
Results
A total of 17,019 patients with cN0 OSCC were included. The basic survival analysis and Cox regression model showed that END increased the probability of 5-year DSS and OS and was an independent prognostic factor. However, among patients who underwent only primary tumor surgery, no significant differences were found between the END and No END groups in 5-year DSS (P = 0. 585) and OS (P = 0.465). Further subgroup analysis showed that primary sites and T stage, but not other factors, might influence the benefit of END. Significant differences were found for T1 (P < 0.001 for OS) and T2 (P = 0.001 for DSS and < 0.001 for OS) tongue squamous cell carcinoma (TSCC) but not for other primary tumor sites.
Conclusion
This large-scale retrospective population-based cohort study suggests that not all patients with cN0 OSCC could benefit from END. Patients with cN0 TSCC are recommended to undergo END, especially with early-stage tumors.
Similar content being viewed by others
Introduction
According to the GLOBOCAN 2020 database, there were 377,713 new cases (2.0% of the total) of lip and oral cavity cancer and 177,757 new deaths (1.8% of the total) from this condition in 2020, the majority of which were oral squamous cell carcinoma (OSCC) [1]. Surgical excision of the primary tumor is the major treatment for patients with OSCC according to the NCCN Clinical Practice Guidelines in Oncology for Head and Neck Cancers, combined with radiation therapy, chemotherapy and the newly introduced immunotherapy [2].
One of the defining features of OSCC is lymph node metastasis, which can be occult and dramatically affect the survival and prognosis of patients [3]. Although imaging technologies have evolved in decades, it is still impossible to detect all occult metastases in the cervical lymph nodes [4]. The best approach to neck management has not reached a consensus, especially for clinical-nodal negative (cN0) OSCC patients [5].
Elective neck dissection (END) and observation are the two main strategies for neck management, which are chosen mostly based on the judgments of surgeons [5]. Whether to perform END or just wait and observe has been debated for a long time but still remains controversial [6]. Many researchers found that END could significantly prolong the survival time and decrease regional recurrences in patients with tongue, floor of mouth, buccal mucosa or other sites of squamous cell carcinoma, advocating that END should be the upfront treatment to remove any occult metastasis [7, 8]. In contrast, other studies showed that the performance of END was not associated with improved rates of overall or disease-specific survival, especially in cT1-2 OSCC, and it was associated with higher rates of complications, including shoulder dysfunction, pain, and contour changes [9,10,11]. The conflict between these two decisions may be due to the lack of sufficient samples and multidimensional analysis of different kinds of patients with OSCC.
The Surveillance, Epidemiology, and End Results (SEER) database provides an appropriate opportunity to survey the necessity and benefit of END in patients with cN0 OSCC because of its large sample size and relatively comprehensive clinical records [12]. Based on the large-scale population of these patients, we thoroughly investigated the potential factors that modulate the benefit of END on patient survival and identified the optimal candidates who could gain maximum benefit from END with multiple subgroup analyses. To our knowledge, this retrospective study was conducted with the most updated data from the SEER database and the largest possible sample size. We sought to provide objective evidence for the management of the cN0 neck in patients with OSCC.
Methods
Data Sources
In this retrospective large-scale population-based study, the detailed information of patients from SEER database 17 registries (Nov 2021 Submission, 2000–2019) was downloaded using SEER*Stat 8.4.0 software with permission from NCI (reference number 12910-Nov2021). Patients who met the following criteria were extracted: (1) Histologic type ICD-O-3: 8050–8076, 8078, 8083, 8084, 8094; (2) primary sites: C02.0, C02.1, C02.2, C02.3, C02.8, C02.9, C03.0, C03.1, C03.9, C04.0, C04.9, C05.0, C06.0, C06.1, C06.2; (3) clinically node-negative (N0) neck. Exclusion criteria included (1) incomplete survival record; (2) incomplete END record; and (3) incomplete AJCC cancer staging record.
The variables investigated in this study included the age at diagnosis, year of diagnosis, sex, race recode, marital status at diagnosis, primary tumor site, derived AJCC T and M stages, SEER*Stat RX Summary-Surgery Primary Site, RX Summary-Scope Reg LN Sur, radiation recode, chemotherapy recode, survival months, vital status recode, cause of death to site recode and SEER cause-specific death classification. The primary study outcomes were overall survival (OS) and disease-specific survival (DSS), and the hazard ratios (HRs) was also calculated.This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Statistical analysis
Clinical and demographic features were compared across subgroups using the chi-square or Fisher exact test. Overall survival (OS) time was calculated from diagnosis to death from any cause and was censored if the patient was alive at the last follow-up or up to 60 months. Disease-specific survival (DSS) time was calculated from diagnosis to death from “SEER cause-specific death classification”. Patients were censored if they died from other causes or were alive at the last follow-up or up to 60 months. Survival curves of OS and DSS were analyzed using the Kaplan‒Meier method, and survival differences between subgroups were compared using the log-rank test. Then, all significant factors were included in a multivariate analysis based on a multivariate Cox proportional hazards regression model that was used to estimate the HRs for survival. Statistical calculations were performed using IBM SPSS Statistics software (version 25.0, IBM Corp. US), and visualization was performed using the “survminer” and “forestmodel” packages in R (version 4.1.0). All statistical tests were 2-sided and considered significant at P < 0.05.
Since this study did not involve interactions with human subjects or the use of any personal identifying information, institutional review board approval for the use of this deidentified dataset was not needed.
Results
Baseline characteristics and survival analysis
A total of 17,019 patients with cN0 OSCC who met the inclusion criteria were identified. The median age at diagnosis was 67 years (range 6–85 +), and the mean follow-up time was 47.37 months. The majority of these patients were male (9448, 55.5%), white (14,540, 85.4%) and married (9059, 53.2%). END was performed in 4078 patients (24.0%), while the other 12,941 (76.0%) patients did not undergo END.
Significant differences in OS and DSS were found for END (Fig. 1), age, race, marital status, primary sites, T stage, M stage, surgery, radiation and chemotherapy (P < 0.001) but not for sex (P = 0.049 in DSS but = 0.74 in OS, Supplementary Figs. 1–2). The Cox regression model showed that age, race, marital status, primary sites, T stage, M stage, surgery, radiation, chemotherapy, and most importantly, END, were independent prognostic indicators (Supplementary Fig. 3). The END group was associated with prolonged DSS (HR, 0.72; 95% confidence interval [CI], 0.64–0.80; P < 0.001) and OS (HR, 0.77; 95% CI, 0.71–0.84; P < 0.001) compared with the No END group. As shown in Table 1, except for sex, the dead/alive ratio for age, race, marital status, primary sites, T stage, M stage, surgery, radiation, and chemotherapy were significantly different between the END group and the No END group, both for OS and DSS. These results were consistent with previous studies [13].
Subgroup survival analysis
From the results above, it seems that END could increase the 5-year survival rates in cN0 OSCC patients, but it is still not clear which kind of patients could benefit most from END or who could not benefit from END. To further identify the actual candidates, we performed a subgroup analysis of all of the independent prognostic factors. Indeed, END significantly increased the probability of 5-year DSS and OS in most subgroups of age, race, marital status, primary sites, T stage, M stage, surgery, radiation and chemotherapy (P < 0.001 for both DSS and OS), except for age < 50 (P = 0.214 for DSS and P = 0.074 for OS), age 50–80 (P = 0.086 for DSS and P = 0.505 for OS), American Indian/Alaska Native (AI, P = 0.320 for DSS and P = 0.979 for OS) and unknown race (P = 0.382 for DSS and P = 0.250 for OS) and unknown M stage (MX, P = 0.442 for DSS and P = 0.883 for OS, Fig. 2, Supplementary Figs. 4–5).
To our surprise, the results of the surgery and END subgroup analyses showed that there was no difference in DSS and OS among the patients who underwent surgery, regardless of whether they received END (Supplementary Fig. 6). In contrast, patients had better survival if they underwent surgery in both the END and No END groups (Supplementary Fig. 6). In addition, the constituent ratios between the END and No END groups displayed significant differences only for T stage and surgery. A total of 99.8% of patients in the END group underwent surgery, while only 83.5% of patients did in the No END group (P < 0.001) (Table 1). These results indicated that the benefit brought by END might mostly come from undergoing surgery and further confirmed that not all patients with cN0 OSCC could benefit from END.
Further exploration of potential subgroups that benefited from END
To identify the patients who received the most benefit from END, we first performed subgroup analysis of different treatment strategies. As shown in Supplementary Fig. 7, there was a dramatic difference among these strategies, with surgery only being the optimal one for both DSS and OS. Among these subgroups, END outweighed No END only in the Surgery+Radiation+Chemotherapy− group (P < 0.001 for both DSS and OS) and Surgery+Radiation+Chemotherapy+ group (P = 0.005 for DSS and P = 0.026 for OS). Interestingly, in the only surgery group, END still showed little difference from No END both in DSS (P = 0.585) and OS (P = 0.465), which further proved our assumption (Fig. 2).
Since radiation and chemotherapy could greatly interfere with the survival analysis of END, we excluded these patients and focused on the patients who merely underwent primary site surgery. A total of 11,836 patients were identified, 45.4% of whom were female and 54.6% of whom were male. Their median age was 66 years (range 6–85 +), and the majority were also white (10,257, 86.7%) and married (6533, 55.2%). There were a total of 9229 (78.0%) patients in the END group and 2607 (22.0%) in the No END group. We estimated the potential factors using a Cox regression model in these separate groups of patients. As displayed in Fig. 3, variables including age, sex, race, marital status, primary site, T stage, M stage and END were independent prognostic factors.
Forest plots summarizing hazard ratios for DSS (A) and OS (B) of patients who only underwent primary site surgery without radiation and chemotherapy. Abbreviations: AI American Indian/Alaska Native, API Asian or Pacific Islander, B black, CI Confidence interval, DSS Disease-specific survival, END Elective neck dissection, HR Hazard ratio, MX Unknown M stage, OS Overall survival
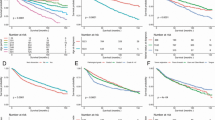
We then performed subgroup analysis of DSS and OS for these factors and surprisingly found that for most indicators, the difference in DSS and OS between the END group and the No END group was no longer significant, including sex, age, race, marital status and M stage (Supplementary Figs. 8–9). However, for primary site and T stage, END showed better results for tongue (P = 0.009 for OS), T1 (P = 0.003 for OS) and T2 (P < 0.001 for both DSS and OS, Fig. 4). Therefore, we focused on these two independent indicators and conducted cross-subgroup survival analysis in multiple subgroups, as shown in Fig. 5. The results showed that in tongue squamous cell carcinoma (TSCC), END lead to better prognostic outcomes in T1 (P = 0.001 for OS) and T2 (P < 0.001 for both DSS and OS). In cN0 T3 and T4 TSCC patients, the DSS and OS curves also showed a trend toward a benefit from END, but the differences were not significant, perhaps because of the lack of samples (T3: n = 197, 2.7%; T4: n = 99, 1.3%). There was no significant difference in DSS or OS between the END and No END groups at other primary sites. The detailed characteristics of the TSCC patients are listed in Table 2. All of these results suggested that patients with TSCC may benefit from END, espesially with early-stage tumors.
Subgroup survival analysis of END in cN0 OSCC patients who only underwent primary site surgery without radiation and chemotherapy according to the primary site (A, B) or T stage (C, D). Abbreviations: DSS Disease-specific survival, END Elective neck dissection, OS Overall survival, OSCC Oral squamous cell carcinoma
DSS (A) and OS (B) curves represent the cross-subgroup survival analysis of END in cN0 OSCC patients who only underwent primary site surgery without radiation and chemotherapy according to the primary sites and T stages. Abbreviations: DSS Disease-specific survival, END Elective neck dissection, OS Overall survival, OSCC Oral squamous cell carcinoma
Discussion
Based on the large-population survival analysis of patients with cN0 OSCC acquired from the SEER database, we found that END was an independent prognostic factor. Surprisingly, in the subgroup analysis, END did not affect survival in patients who underwent primary site surgery. After excluding the influence of radiation or chemotherapy on survival, we found that not all patients with cN0 OSCC could definitely benefit from END. Further analysis showed that patients with TSCC, even those with early-stage tumors, could benefit from END, but END did not lead to significantly better survival results for tumors arising from other sites.
In recent decades, researchers around the world have continuously focused on END in OSCC patients, especially those with early-stage tumors. Before 2010, four randomized controlled trials (RCTs) were carried out with small samples (only 67–71), three of which did not find differences in survival between END or observation [14,15,16,17]. A surgical team from Brazil found that patients treated with elective supraomohyoid neck dissection had a significant benefit in terms of disease-free survival (DFS) only in those whose tumor thickness was > 4 mm and a later stage, leaving the question unanswered [16]. In 2015, D’Cruz AK and his team performed the largest single-center RCT, the Mumbai trial [18], comparing END and therapeutic node dissection (watchful waiting followed by neck dissection for nodal relapse). Their results showed an improved rate of overall survival (80.0% vs. 67.5%, P = 0.01) and disease-free survival with END relative to those in the therapeutic surgery group (69.5% vs. 45.9%, P < 0.001), with similar complication rates (6.6% vs. 3.6%). Nevertheless, these studies could not provide conclusive evidence because of the low quality of the trials [19]. Later, the high-quality SEND study [19] in 2019 with 27 hospitals in the UK and 250 randomized patients indicated that those who underwent END had a lower risk of death or local recurrence, even with small tumors. However, the lack of enough samples from extensive areas still limits the generalization of END in cN0 OSCC patients.
Many researchers have conducted meta-analyses to summarize the effect of END from a larger cohort [20, 21], but the inherent heterogeneity among different studies, especially between RCTs and retrospective studies, makes it difficult to provide convincing conclusions [22]. Three meta-analyses, which included only the RCTs mentioned above, were conducted in 2011 [23], 2015 [24] and 2019 [25]. Their results revealed that END significantly reduced the risk of regional recurrences and the risk of disease-specific death and revealed a longer OS and DFS compared to observation. These studies, however, included low-quality RCTs, leading to their inferior reliability.
The SEER Program of the National Cancer Institute is a relatively comprehensive source of information on cancer incidence and survival in the United States, covering 48% of the U.S. population currently [25]. Several studies have investigated cN0 OSCC patients within this database [26]. Alimujiang et al. performed two SEER-based analyses comparing END and observation in cT1N0 or T2N0 OSCC patients separately [13, 27]. Through survival analysis and the Cox regression model, they showed that END was an independent prognostic indicator, improving both DSS and OS. These results are in accordance with our findings, but in our study, we further explored the potential factors that affect the survival of END-treated patients and the actual characteristics that predict a benefit from END.
To our knowledge, our study is the first to evaluate the effect of END in cN0 OSCC with multidimensional subgroup analysis. However, there are still several shortcomings of this study. An analysis of pathological grade was not included because the records of pathological grade were missing in most cases, and those with this record were censored at 2 years. Another disadvantage lies in the missing data of the actual affected lymph node distribution in different areas of the neck in those who underwent END, making it impossible to elucidate which district should be surgically excised among the different sites [28].
Conclusions
To conclude, primary tumor site and T stage are the essential factors that influence the benefit of END on patient survival, and END is recommended in patients with cN0 TSCC, especially those with early-stage tumors. In the future, the potential immunological or molecular mechanism of END should be clarified, and large-scale multicenter RCTs investigating new surgical methods, such as sentinel lymph node dissection (SLND), are urgently needed [29].
Availability of data and materials
All data used in this paper (individual case listings as well as US population mortality data) may be accessed and analysed via the SEER*Stat web program following the submission of a request for access to the data at https://seer.cancer.gov/seertrack/data/request/. Further information is available from the corresponding author upon request.
Abbreviations
- AI:
-
American Indian/Alaska Native
- API:
-
Asian or Pacific Islander
- B:
-
Black
- CI:
-
Confidence interval
- cN0:
-
Clinical-nodal negative
- DSS:
-
Disease-specific survival
- END:
-
Elective neck dissection
- HRs:
-
Hazard ratios
- MX:
-
Unknown M stage
- OS:
-
Overall survival
- OSCC:
-
Oral squamous cell carcinoma
- RCTs:
-
Randomized controlled trials
- SEER:
-
The Surveillance, Epidemiology, and End Results
- SLND:
-
Sentinel lymph node dissection
- TSCC:
-
Tongue squamous cell carcinoma
- W:
-
White
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–49.
Pfister DG, Spencer S, Adelstein D, et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18(7):873–98.
Warshavsky A, Rosen R, Nard-Carmel N, et al. Assessment of the Rate of Skip Metastasis to Neck Level IV in Patients with Clinically Node-Negative Neck Oral Cavity Squamous Cell Carcinoma: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2019;145:542–8.
Roy P, Mallick I, Arun I, et al. Nodal yield and topography of nodal metastases from oral cavity squamous cell carcinoma - An audit of 1004 cases undergoing primary surgical resection. Oral Oncol. 2021;113:105115.
Koyfman SA, Ismaila N, Crook D, et al. Management of the Neck in Squamous Cell Carcinoma of the Oral Cavity and Oropharynx: ASCO Clinical Practice Guideline. J Clin Oncol. 2019;37:1753–74.
Gupta T, Maheshwari G, Kannan S, et al. Systematic review and meta-analysis of randomized controlled trials comparing elective neck dissection versus sentinel lymph node biopsy in early-stage clinically node-negative oral and/or oropharyngeal squamous cell carcinoma: Evidence-base for practice and implications for research. Oral Oncol. 2022;124:105642.
Ding Z, Xiao T, Huang J, et al. Elective Neck Dissection Versus Observation in Squamous Cell Carcinoma of Oral Cavity with Clinically N0 Neck: A Systematic Review and Meta-Analysis of Prospective Studies. J Oral Maxillofac Surg. 2019;77:184–94.
Dias FL, Kligerman J, de MatosSá G, et al. Elective neck dissection versus observation in stage I squamous cell carcinomas of the tongue and floor of the mouth. Otolaryngol Head Neck Surg. 2001;125:23–9.
Amit M, Liu C, Mansour J, et al. Elective neck dissection versus observation in patients with head and neck cutaneous squamous cell carcinoma. Cancer. 2021;127:4413–20.
Liu TR, Chen FJ, Yang AK, et al. Elective neck dissection in clinical stage I squamous cell carcinoma of the tongue: Does it improve regional control or survival time? Oral Oncol. 2011;47:136–41.
van Hinte G, Sancak T, Weijs WLJ, et al. Effect of elective neck dissection versus sentinel lymph node biopsy on shoulder morbidity and health-related quality of life in patients with oral cavity cancer: A longitudinal comparative cohort study. Oral Oncol. 2021;122: 105510.
Gao F, Li N, Xu Y, Yang G. Effects of Postoperative Radiotherapy on Survival of Patients with Stage IIIA Resected Non-Small Cell Lung Cancer: Analysis of the SEER Database. J Natl Compr Canc Netw. 2020;18:718–27.
Wushou A, Wang M, Yibulayin F, et al. Patients With cT1N0M0 Oral Squamous Cell Carcinoma Benefit from Elective Neck Dissection: A SEER-Based Study. J Natl Compr Canc Netw. 2021;19:385–92.
Vandenbrouck C, Sancho-Garnier H, Chassagne D, Saravane D, Cachin Y, Micheau C. Elective versus therapeutic radical neck dissection in epidermoid carcinoma of the oral cavity: results of a randomized clinical trial. Cancer. 1980;46:386–90.
Fakih AR, Rao RS, Borges AM, Patel AR. Elective versus therapeutic neck dissection in early carcinoma of the oral tongue. Am J Surg. 1989;158:309–13.
Kligerman J, Lima RA, Soares JR, et al. Supraomohyoid neck dissection in the treatment of T1/T2 squamous cell carcinoma of oral cavity. Am J Surg. 1994;168:391–4.
Yuen AP, Ho CM, Chow TL, et al. Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Head Neck. 2009;31:765–72.
D’Cruz AK, Vaish R, Kapre N, et al. Elective versus Therapeutic Neck Dissection in Node-Negative Oral Cancer. N Engl J Med. 2015;373:521–9.
Hutchison IL, Ridout F, Cheung SMY, et al. Nationwide randomised trial evaluating elective neck dissection for early stage oral cancer (SEND study) with meta-analysis and concurrent real-world cohort [published correction appears in Br J Cancer. 2022 Mar; 126(5):831]. Br J Cancer. 2019;121:827–36.
Oh LJ, Phan K, Kim SW, Low TH, Gupta R, Clark JR. Elective neck dissection versus observation for early-stage oral squamous cell carcinoma: Systematic review and meta-analysis. Oral Oncol. 2020;105: 104661.
Suton P, Luksic I. Prognostic value of elective neck dissection in adenoid cystic carcinoma of head and neck: a meta-analysis: A call for randomized trials and international consensus. Int J Oral Maxillofac Surg. 2021;50:1403–7.
Abu-Ghanem S, Yehuda M, Carmel NN, et al. Elective Neck Dissection vs Observation in Early-Stage Squamous Cell Carcinoma of the Oral Tongue with No Clinically Apparent Lymph Node Metastasis in the Neck: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016;142:857–65.
Fasunla AJ, Greene BH, Timmesfeld N, Wiegand S, Werner JA, Sesterhenn AM. A meta-analysis of the randomized controlled trials on elective neck dissection versus therapeutic neck dissection in oral cavity cancers with clinically node-negative neck. Oral Oncol. 2011;47:320–4.
Ren ZH, Xu JL, Li B, Fan TF, Ji T, Zhang CP. Elective versus therapeutic neck dissection in node-negative oral cancer: Evidence from five randomized controlled trials. Oral Oncol. 2015;51:976–81.
Xiang M, Colevas AD, Holsinger FC, Le QX, Beadle BM. Survival After Definitive Chemoradiotherapy With Concurrent Cisplatin or Carboplatin for Head and Neck Cancer. J Natl Compr Canc Netw. 2019;17:1065–73.
Marchiano E, Patel TD, Eloy JA, Baredes S, Park RC. Impact of Nodal Level Distribution on Survival in Oral Cavity Squamous Cell Carcinoma: A Population-Based Study. Otolaryngol Head Neck Surg. 2016;155:99–105.
Wushou A, Yibulayin F, Sheng L, Luo Y, Yang ZC. Elective neck dissection improves the survival of patients with T2N0M0 oral squamous cell carcinoma: a study of the SEER database. BMC Cancer. 2021;21:1309.
Majumdar KS, Rao VUS, Prasad R, Ramaswamy V, Sinha P, Subash A. Incidence of Micrometastasis and Isolated Tumour Cells in Clinicopathologically Node-Negative Head and Neck Squamous Cell Carcinoma. J Maxillofac Oral Surg. 2020;19(1):131–5.
Hasegawa Y, Tsukahara K, Yoshimoto S, et al. Neck Dissections Based on Sentinel Lymph Node Navigation Versus Elective Neck Dissections in Early Oral Cancers: A Randomized, Multicenter, and Noninferiority Trial. J Clin Oncol. 2021;39:2025–36.
Acknowledgements
The authors wish to give special thanks for the efforts of the SEER tumor registry team. The authors are also grateful to American Journal Experts (https://www.aje.com) for checking the English of the article.
Funding
This work was supported by the National Natural Science Foundation of China (31871464, 82071115) and Natural Science Foundation of ChongQing, China (CSTB2023NSCQ-BHX0102).
Author information
Authors and Affiliations
Contributions
Qiuyu Wu: Data collection and assembly, data analysis and visualization. Yuanhang Xia: Data analysis and visualization. Ling Qiu: Data collection and assembly, manuscript review and editing. Shuqiong Wen: Data collection and assembly, data analysis. Qunxing Li: Data collection and assembly. Xiang Gao: Data collection and assembly. Wenrong Jiang: Data analysis. Tao Wang: Data collection and assembly. Ping Ji: Study concept and design, manuscript writing, manuscript review and editing. Zhanpeng Ou: Study concept and design, data analysis, visualization, manuscript writing, manuscript review and editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not required for this SEER-based study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure 1.
DSS curves of patients with cN0 OSCC according to (A) sex, (B) age group, (C) race, (D) marital status, (E) T, (F) M, (G) primary sites, (H) surgery, (I) radiation, (J) chemotherapy. Supplementary Figure 2. OS curves of patients with cN0 OSCC according to (A) sex, (B) age group, (C) race, (D) marital status, (E) T, (F) M, (G) primary sites, (H) surgery, (I) radiation, (J) chemotherapy. Supplementary Figure 3. Forest plots summarizing HR for (A) DSS and (B) OS. Supplementary Figure 4. DSS curves of patients with cN0 OSCC according to (A) age, (B) race, (C) primary sites, (D) T, (D) M, (E) Radiation, (F) Chemotherapy with END subgroups analysis. Supplementary Figure 5. OS curves of patients with cN0 OSCC according to (A) age, (B) race, (C) primary sites, (D) T, (D) M, (E) Radiation, (F) Chemotherapy with END subgroups analysis. Supplementary Figure 6. Subgroup analysis of END and surgery of patients with cN0 OSCC. Supplementary Figure 7. DSS and OS curves of patients with cN0 OSCC according to different treatment categories. Supplementary Figure 8. DSS of cN0 OSCC patients only performed primary sites surgery without radiation and chemotherapy according to (A) primary sites, (B) age, (C) race, (D) marital status and (E) M with END subgroups analysis. Supplementary Figure 9. OS of cN0 OSCC patients only performed primary sites surgery without radiation and chemotherapy according to (A) primary sites, (B) age, (C) race, (D) marital status and (E) M with END subgroups analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, Q., Xia, Y., Qiu, L. et al. Do patients with cN0 oral squamous cell carcinoma benefit from elective neck dissection? A large-scale population-based study. BMC Oral Health 24, 32 (2024). https://doi.org/10.1186/s12903-023-03632-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03632-5