Abstract
Background
COVID-19 and the subsequent intermittent lockdown measures from 2020 to 2022 in China critically disrupted regular medical activities, including dental care. This study aimed to investigate the impact of COVID-19 on long-term follow-up at the Stomatology Hospital, Zhejiang University School of Medicine and to evaluate potential causes of loss to follow-up.
Methods
A total of 1062 patients with periodontitis who visited the hospital from January 2019 to June 2022 were included in this study, and patient information was collected retrospectively in the form of a telephone questionnaire. The questionnaire consisted of 19 questions in four areas: demographic characteristics, clinical periodontal parameters, oral hygiene habits, and follow-up-related open-ended questions (specific reasons for loss to follow-up, attitudes toward follow-up and suggestions for increasing participation in future follow-ups). Regression analysis of factors influencing the follow-up of patients with periodontitis were analyzed by regression analysis using R (v4.2.3) software.
Results
A total of 536 (50.47%) valid questionnaires were collected from 1062 patients. Personal factors (42.5%), instead of the COVID-19 epidemic (20.0%), were the main factors that impacted the loss to follow-up in long-term periodontal treatment, while work factors (19.8%), hospital factors (16.4%), and transportation or distance factors (14.7%) were all important factors. A family history of periodontitis [odds ratio (OR) = 0.567, 95% confidence interval (CI): 0.393, 0.817, p = 0.002], as well as frequent use of dental devices (OR = 0.540, 95% CI: 0.375, 0.777, p = 0.001), were significantly associated with a “negative” attitude toward follow-up visits.
Conclusion
This survey suggests that the COVID-19 epidemic factor was an important cause contributed to the loss to follow-up during supportive periodontal therapy (SPT) among a variety of potential factors. Majority of patients had negative attitudes toward subsequent continued participation in supportive care.
Similar content being viewed by others
Background
Periodontitis is the primary cause of adult tooth extractions in China [1]. Patients with periodontitis usually suffer from bleeding gums and loss of periodontium support; this is manifested by a loss of clinical attachment and the presence of periodontal pockets and alveolar bone resorption on radiographs [2]. In severe cases, periodontitis can result in loosening and loss of teeth, which can in turn lead to impaired speech and chewing functions, affecting patients’ physical appearance and having a negative impact on their nutrition, quality of life and mental health [3,4,5,6]. A thorough treatment plan is therefore needed for patients with periodontitis to avoid these conditions. The treatment procedure for periodontitis consists of the following four stages: initial therapy, periodontal surgery, restorative therapy, and supportive periodontal therapy (SPT) [1]. SPT is an integral part of a systemic periodontal treatment plan and is a prerequisite for the long-term maintenance of periodontal efficacy [7, 8]. Individually scheduled SPT based on the specific patient’s risk profile needs to be started immediately after initial therapy, and it requires consistent patient participation for the whole treatment duration thereafter [9].
Long-term periodontal health maintenance largely depends on regular and frequent check-ups; unfortunately, many patients are lost to follow-up after active therapy [10,11,12] despite dentists’ repeated emphasis on the importance and necessity of follow-up in long-term SPT. Previous studies have suggested that age, severity of periodontitis, periodontal surgery and the level of self-efficacy for self-care might be effective predictors of loss to follow-up in long-term SPT among patients with periodontitis [10, 13, 14]. COVID-19 and subsequent intermittent lockdown measures disrupted dental visits, during which dental offices were closed and patient access became more complicated. We hypothesized that COVID-19 might have an impact on loss to follow-up among patients with periodontitis.
Therefore, this study aimed to investigate the impact of COVID-19 on the long-term follow-up among periodontal patients and to evaluate potential causes of loss to follow-up.
Ethics and study design
This study consisted of a questionnaire survey of the loss to follow-up using telephone callbacks, and the purpose of the trial was clearly explained to the patients to obtain their verbal consent before the questionnaire was administered. After the survey, the researchers answered other inquiries from the patients. This study was approved by the Ethics Committee of the Stomatology Hospital at the School of Stomatology of the Zhejiang University School of Medicine (IP 2022(041)) and was conducted in accordance with the Declaration of Helsinki, as revised in 2013.
Telephone questionnaire
The questionnaire used in this survey was developed for this study. The process of development consisted of a literature review study, two group discussions and a telephone questionnaire test with 18 randomly selected patients with periodontitis. It consisted two parts: data collection form and telephone questionnaire. The part one data collection form which including gender, age and clinical periodontal parameters was collected and filled by Pan, W.Y. Telephone surveys were conducted by Xu, Y.X. and Wang, M.L. both of whom had undergone standardized training. Questions 11, 12, and 13 of Part 2 were asked in an open-ended manner. The specific details of the content for the question are presented in Table 1. The specific reasons for failure to attend follow-up visits were discussed by Wang, M.L. and Xu, Y.X. and reviewed by Wang, Q.T. before being classified into 11 factors. The explanation of the classification of each factor is presented in Supplementary file 1.
Materials and methods
Study population
The information of 16,385 patients visited the Periodontics Department of the Stomatology Hospital, Zhejiang University School of Medicine who underwent supragingival scaling from January 2019 to June 2022 were collected. The patients initial visit of the two senior periodontists were then extracted, comprising a total of 2883. Patients were reviewed in conjunction with their medical records, and a total of 1062 patients were included based on the inclusion and exclusion criteria. In this study, SPT compliance was defined as a patient attending repeated SPT appointments within 6 ± 1 months, whereas appointments that took place more than 6 ± 1 months apart were classified as loss to follow-up.
Eligibility criteria
Patients who met the following criteria were included: (a) ≥ 18 years old, (b) diagnosis of periodontitis: interdental clinical attachment loss (CAL) is detectable at ≥ 2 non-adjacent teeth, or buccal or oral CAL ≥ 3 mm with probing pocket depth (PD) > 3 mm is detectable at ≥ 2 teeth [15], (c) underwent full-mouth subgingival instrumentation, (d) no follow-up visits within 6 ± 1 months of completion of treatment, and (e) complete set of information present in the patient’s medical records, along with panoramic oral film and electronic periodontal record sheet. The exclusion criteria consisted of (a) having undergone periodontal surgery, (b) patients who clearly expressed their unwillingness to participate in the program during the telephone survey, and (c) patients who did not answer after 3 separate calls (first call, 30 min later, any time the following day).
Statistical analysis
Data were analyzed using R Version 4.2.3. A p value of < 0.05 was considered statistically significant in all analyses. Continuous variables are expressed as means ± standard deviations, and a t test was used for comparison between groups; categorical variables are expressed as frequencies (composition ratios), and a χ2 test was used for comparison between groups. For variables that did not meet the application conditions of the χ2 test, Fisher’s exact probability method was used. Patients were divided into two groups, those with “positive” and “negative” visits, based on their attitudes toward follow-up. Regression analysis was performed using a binary logistic regression model, with attitudes toward follow-up as the dependent variable; the model included 16 factors, such as gender, age, and mean PD, as independent variables to analyze the factors influencing the “negative” attitude toward follow-up visits and were expressed as ratios (ORs) and their 95% confidence intervals (95% CIs).
Results
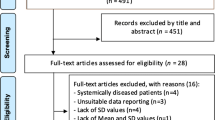
A total of 536 valid data points were obtained from 270 (50.4%) males and 266 (49.6%) females, with an effective rate of 50.47%. 45 patients whose calls could not be connected, 310 patients who refused to answer the phone, and 171 patients who refused to participate in this study after being connected were excluded. The specific screening process is shown in Fig. 1.
Characteristics of the study population
The average age of the participants was 42.1 ± 11.4 years old. The periodontal clinical data of all participants had a mean PD of 3.4 ± 0.8 mm, a mean CAL of 3.5 ± 0.9 mm, and a BOP of 63.9 (20.3%); participants with periodontitis at stage III and IV accounted for 69.9%. Gender, age, occupation, education level, family history of periodontitis, smoking habits, drinking habits, health insurance, income of family per month (yuan), and oral hygiene habits are described in detail in Table 2.
Reasons for loss to follow-up
The specific reasons for failure to attend follow-up visits were varied. The top three factors were personal factors, COVID-19 epidemic factors and work factors, as shown in Fig. 2.
Attitudes toward follow-up visits and related influencing factors
324 patients (60.4%) held a positive attitude toward follow-up visits, while 212 patients (39.6%) believed that they would not attend any follow-up visits at the periodontal department. To investigate which factors had an impact on patients’ attitudes toward treatment at a later time, a univariate analysis of the included variables was conducted, as shown in Table 2. In the univariate correlation model, 3 independent variables emerged as significant predictors of required periodontal treatment: a family history of periodontitis, family income per month (yuan), and whether dental devices (e.g., dental floss and water irrigator) were regularly used (p < 0.05).
All the variables mentioned above were included in a binary logistic regression analysis (Table 3), while family history of periodontitis (OR = 0.567, 95% CI: 0.393, 0.817) and frequent use of dental devices (OR = 0.540, 95% CI: 0.375, 0.777) were negatively correlated with patients’ attitudes toward follow-up visits.
Discussion
Failure to attend follow-up visits among patients with periodontitis has a negative impact on adherence to good periodontal health after successful periodontal treatment [16]. The present study adopted open-ended questions to allow participants to self-report their particular situation to analyze the specific reasons and related influences for loss to follow-up in depth.
The reasons for loss to follow-up are varied. A total of 381 patients (71.7%) self-reported not attending follow-up appointments due to a single factor, while the remaining 28.9% did not attend due to multiple factors. Personal factors were the most important reasons for loss to follow-up. Patients felt that they had good periodontal health, forgot the time of the follow-up visit, or subjectively avoided treatment. It is evident that patients’ periodontal health awareness is still very inadequate. It has been documented that chief complaints are associated with patient compliance and that acute symptoms may be a positive predictor of periodontal treatment initiation but may be a negative predictor of treatment completion [17]. This view was confirmed in the present study, in which the majority of patients reported that they felt asymptomatic with regard to periodontitis after treatment, which to some extent confirmed the treatment effect. At the same time, since patients often forget to attend appointments (due to the long-time intervals between visits), health care professionals need to provide more ways to remind them to see the doctor. For example, the development and improvement of follow-up reminder systems may have a positive effect on improving appointment adherence, as the literature shows with applications in the orthodontic field [18]. Some patients were subjectively reluctant to receive treatment, stating that they were aware of their doctor’s recommendations for follow-up but still refused to attend appointments on time. Based on previous research, patients suffering from a lack of information and motivation are by far the leading cause of poor adherence, as reported by patients themselves [11]. Therefore, in addition to reminding patients not to miss follow-up visits due to personal factors, the most important thing is to provide them with the corresponding health education, that is, to reinforce the concept outside the clinic to increase their motivation to participate in treatment [18].
The main objective of this study was to investigate the effect of COVID-19 on the long-term follow-up among periodontal patients, which, as shown by the results, accounted for the second reason for loss to follow-up (20.0%), with patients stating that their fear of infection and subsequent intermittent lockdown measures made it difficult for them to move forward, which is a global phenomenon [19]. COVID-19 is now classified as a Class B infectious disease, and this barrier can be removed. 79 (14.7%) of the patients felt that the hospital was not close enough to a subway station, and a significant proportion of patients from out of town were unable to maintain regular follow-ups due to the distance. Both of these factors can be aided by teledentistry. In the last few years, teledentistry has evolved to such an extent that it is able to improve medical efficiency by reducing geographical barriers and the risk of infectious diseases [20, 21]. Teledentistry is an excellent way to provide health education, patient follow-up management, etc. It is therefore important to continuously strengthen the construction and promotion of internet-based applications in hospitals. An increased prevalence of teledentistry to connect specialist dental hospitals with community hospitals or dental clinics for basic review and intelligent referral can, to a certain extent, solve the problem of distance and congestion at the dental hospital. However, China’s current dental specialty institution information technology investment scale is small, and the service level of each dental hospital varies; thus, a more sustainable development path needs to be explored [22].
A total of 106 patients (19.8%) were unable to attend follow-up visits due to work. 88 (16.4%) of the patients abandoned further visits due to hospital factors, such as difficulty in making appointments with periodontists and long waiting times. Both of these objective factors can be explained by the fact that the number of private dental institutions in China is currently twice that of public institutions. The ratio of the number of dentists to the population is 1:7768, which is lower than the WHO standard of 1:5000. The overall number of oral/dental staff and institutions is insufficient and unevenly distributed [23, 24], but most people in China tend to seek treatment at public institutions [25]. Medical resources for public oral/dental institutions are always in short supply, and the treatment of periodontitis requires multiple visits, which inevitably leads to longer waiting times or an inability to provide more doctors on weekends. China rolled out a series of policies in 2015–2016 to establish medical alliances to integrate resources at all levels, expand the scale of private hospitals and relax requirements for doctors to practice at a single location. However, private health care is expensive and caters to only a fraction of patients [26]. This is a very difficult issue. We have the following suggestions: We have the following suggestions: public hospitals can try to open more branches to cover more districts and alleviate the burden on medical resources; rationalize doctors’ working hours; and increase the number of oral healthcare professionals.
Periodontitis requires not only professional treatment and good patient adherence but also effective daily oral maintenance. In addition to tooth brushing, the use of interdental cleaning equipment at home can effectively prevent and control periodontal diseases [27]. In this study, 90% of patients self-reported brushing ≥ 2 times a day, 60% brushed for ≥ 3 min each time, and 66.4% used dental floss, oral irrigators or other cleaning devices, indicating that despite the low patient compliance, patients improved their awareness of oral hygiene after seeing a doctor, which is a good sign.
A family history of periodontitis is associated with SPT adherence, as also mentioned in this paper. However, there was no correlation observed between smoking and attitudes toward follow-up visits, which is inconsistent with the findings of previous studies [11]. This may be due to the large number of nonsmokers or former smokers in the study population. People who regularly used floss or oral irrigators had a more negative attitude toward follow-up visits, probably because they already had better oral hygiene habits and relatively less pronounced periodontal symptoms, that is, no obvious major complaints, which also echoes the points made above.
This study included advice taken from 108 participants, although not all of it was valid. Based on the results, a number of common suggestions were made: simplifying the visiting process and reducing the number of periodontal follow-up visits; increasing the weekend and nighttime availability of doctors in periodontal departments; ability to change online follow-up visits; having a person responsible for reminding patients of upcoming visits or using online tools such as mini-programs and public accounts to remind patients of appointment times; reducing treatment prices; increasing cooperation with online platforms to promote an understanding of periodontitis; and mobilizing social support from patients’ families. The above recommendations should be incorporated and referenced to improve compliance with future visits.
The current study has several limitations that need to be noted. First, the effectiveness of the telephone-based questionnaire was only 50.47%, with 481 patients refusing to answer the phone. One of the reasons may be the high level of distrust among Chinese people in revealing personal information over the phone; otherwise, a more representative set of findings could have been obtained. In addition, only one tertiary care hospital was investigated during this study, which covered most local periodontitis patients but could not span a wide geographical area and did not include private dental clinics or public general hospital dentistry departments. The level of self-efficacy for self-care may be a valid predictor of loss to follow-up [10], but the SESS questionnaire was not used in this survey, which would have made it more difficult given the length of the telephone survey. Therefore, larger and more diverse samples should be evaluated in future studies. This is an issue that the authors will address, as well as the possibility of considering combining prospective study surveys with telephone callbacks to minimize patient resistance regarding surveys.
Conclusions
COVID-19 epidemic factors contributed to the loss to follow-up of periodontitis patients, but the personal factor of poor periodontal health awareness of the individual still remained the most important reason. Although the COVID-19 factor is no longer a threat at present, majority of patients have a negative attitude towards long-term SPT. Hence, patients who negatively toward compliance should be screened early, and targeted interventions need to be explored and implemented to reduce the loss to follow-up rate.
Availability of data and materials
All data generated during this study are included in this published article’s Supplementary file 2.
Abbreviations
- SPT:
-
Supportive periodontal therapy
- AAP:
-
American Academy of Periodontology
- EFP:
-
European Federation of Periodontology
- PD:
-
Pocket depth
- CAL:
-
Clinical attachment loss
- BOP:
-
Bleeding on probing
- SESS:
-
Self-efficacy scale for self-care
References
Meng H, Shu R, Yan F. Peridontology. 5th ed. Beijing: People’s Medical Publishing House; 2020.
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral Diseases: a global public health challenge. The Lancet. 2019;394:249–60.
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal Diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol. 2017;44:456–62.
Miao L, Feng J, Wu L, Zhang S, Ge Z, Pan Y. The mediating role of general self-efficacy in the association between perceived social support and oral health-related quality of life after initial periodontal therapy. BMC Oral Health. 2016;16:68.
Levin L, Zini A, Levine J, Weiss M, Lev R, Chebath Taub D, et al. Demographic profile, oral Health Impact Profile and Dental anxiety scale in patients with chronic periodontitis: a case–control study. Int Dent J. 2018;68:269–78.
Zheng D, Kang X, Wang Y, Huang Y, Pang C, Chen Y, et al. Periodontal Disease and emotional disorders: a meta-analysis. J Clin Periodontol. 2021;48:180–204.
Costa FO, Lages EJP, Cota LOM, Lorentz TCM, Soares RV, Cortelli JR. Tooth loss in individuals under periodontal maintenance therapy: 5-year prospective study. J Periodont Res. 2014;49:121–8.
Costa FO, Vieira TR, Cortelli SC, Cota LOM, Costa JE, Aguiar MCF, et al. Effect of compliance during periodontal maintenance therapy on levels of bacteria associated with periodontitis: a 6-year prospective study: levels of bacteria in periodontal maintenance. J Periodontol. 2018;89:519–30.
Renvert S, Persson GR. Supportive periodontal therapy. Periodontol 2000. 2004;36:179–95.
Wu D, Yang HJ, Zhang Y, Li XE, Jia YR, Wang CM. Prediction of loss to follow-up in long-term supportive periodontal therapy in patients with chronic periodontitis. PLoS ONE. 2018;13:e0192221.
Amerio E, Mainas G, Petrova D, Giner Tarrida L, Nart J, Monje A. Compliance with supportive periodontal/peri-implant therapy: a systematic review. J Clin Periodontol. 2020;47:81–100.
Novaes AB, Novaes AB, Moraes N, Campos GM, Grisi MFM. Compliance with supportive Periodontal Therapy. J Periodontol. 1996;67:213–6.
Lorentz TCM, Miranda Cota LO, Cortelli JR, Vargas AMD, Costa FO. Prospective study of complier individuals under periodontal maintenance therapy: analysis of clinical periodontal parameters, risk predictors and the progression of periodontitis. J Clin Periodontol. 2009;36:58–67.
Perrell-Jones C, Ireland RS. What factors influence patient compliance with supportive periodontal therapy in a general practice setting? Br Dent J. 2016;221:701–4.
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol. 2018;45:149–61.
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Berglundh T, et al. Treatment of stage I–III periodontitis—the EFP S3 level clinical practice guideline. J Clin Periodontology. 2020;47:4–60.
Yeh H-C, Lai H. Association between patients’ chief complaints and their compliance with periodontal therapy: Chief complaint and compliance. J Clin Periodontol. 2011;38:449–56.
Fernández CE, Maturana CA, Coloma SI, Carrasco-Labra A, Giacaman RA. Teledentistry and mHealth for Promotion and Prevention of Oral Health: a systematic review and Meta-analysis. J Dent Res. 2021;100:914–27.
Sycinska-Dziarnowska M, Maglitto M, Woźniak K, Spagnuolo G. Oral health and Teledentistry Interest during the COVID-19 pandemic. JCM. 2021;10:3532.
Wolf TG, Schulze RKW, Ramos-Gomez F, Campus G. Effectiveness of Telemedicine and Teledentistry after the COVID-19 pandemic. IJERPH. 2022;19:13857.
Islam MRR, Islam R, Ferdous S, Watanabe C, Yamauti M, Alam MK, et al. Teledentistry as an effective Tool for the communication improvement between dentists and patients: an overview. Healthcare. 2022;10:1586.
Zhao Q, Tian Y, Gao M, Yu H, Zhang W. Research on the current situation and countermeasures of internet medical development in stomatological medical institutions. Chin Hosp. 2023;27:27–30.
Report of the National. Investigation of resources for oral health in China. Chin J Dent Res. 2018;21:285–97.
Statistical Analysis of Current Oral Health Care and Dental Education Resources in China. Chin J Dent Res. 2019;22:37–43.
Xue X. Annual Report on China’s private hospitals development (2017). Beijing: Social Sciences Academic Press; 2018.
Zhu J, Li J, Zhang Z, Li H, Cai L. Exploring determinants of health provider choice and heterogeneity in preference among outpatients in Beijing: a labelled discrete choice experiment. BMJ Open. 2019;9:e023363.
Worthington HV, MacDonald L, Poklepovic Pericic T, Sambunjak D, Johnson TM, Imai P, et al. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries. Cochrane Database Syst Rev. 2019;2020.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers: 82001045) in data collection, paper submitting, and data analysis.
Author information
Authors and Affiliations
Contributions
MLW, YXX and QTW designed the study. MLW, YXX, WF and QTW collected the data. WF and WYP analysed the data. MLW and YXX drafted and wrote the manuscript. QTW and YWP revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Stomatology Hospital, School of Stomatology, Zhejiang University School of Medicine, IP 2022 (041), and carried out in accordance with the Declaration of Helsinki, as revised in 2013. It was a retrospective study in the form of a telephone survey, with informed verbal consent obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, M., Xu, Y., Fang, W. et al. Impact of COVID-19 on patient follow-up during supportive periodontal therapy: a retrospective study based on phone call survey. BMC Oral Health 23, 811 (2023). https://doi.org/10.1186/s12903-023-03539-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03539-1