Abstract
Objective
The muscle quality index (MQI) is a measurement of muscle quality that is directly related to overall health. There has been little study on the relationship between the muscle quality index and periodontitis in American people beyond 30 years. Therefore, this study aimed to explore the link between periodontitis and Muscle quality index (MQI) in older Americans.
Methods
Three thousand two hundred fifty-eight individuals (aged 30 to 59) who participated in the National Health and Nutrition Examination Survey (NHANES) 2011–2014 were considered eligible for the cross-sectional investigation. A hand dynamometer was used to determine the handgrip strength (HGS). Dual-energy X-ray absorptiometry was employed to calculate ASM (DXA). MQIArm was calculated by dividing the dominant hand’s HGS by the dominant arm’s ASM (in kg/kg). MQIApp was calculated by dividing the dominant hand’s HGS by the ASM (in kg/kg). MQItotal was calculated by dividing the sum of the dominant and non-dominant hands by the ASM (in kg/kg). To investigate the link between muscle quality index and periodontal disease, the weighted multivariable logistic regression models were used. Using generalized additive models, it was determined if a nonlinear connection existed. Then, we developed a two-piece linear regression model and calculated the inflection point using a recursive approach. A mediation study was performed to determine how much of the impact of MQItotal on periodontitis was mediated by potential variables.
Results
Three thousand two hundred fifty-eight participants from the United States were enrolled. The OR (95% CI) for the relationship between MQItotal and periodontitis in the regression model with fully adjusted variables was 0.69 (0.53–0.91), for the connection between MQIArm and periodontitis was 0.90 (0.84–0.97), and for the association between MQIApp and periodontitis was 0.49 (0.30–0.80). MQItotal and periodontitis were shown to have a J-shaped relationship with a change point of 3.64. Before the change point, the OR (95% CI) was 0.69 (0.58, 0.82). In the analysis of drinking and married status, the interaction was statistically significant. Analysis of mediation showed that alcohol use was responsible for 0.4% (0.10 to 1.2) of the effect of MQItotal on periodontitis.
Conclusion
In American adults aged over 30, the Muscle Quality Index (MQI) exhibited an independent negative correlation with moderate to severe periodontitis, demonstrating a J-shaped relationship. Furthermore, alcohol consumption may act as a mediator in the association between MQI and periodontitis.
Similar content being viewed by others
Introduction
Periodontal disease, often termed gum disease, is a complex inflammatory condition instigated by bacterial plaque microorganisms. These pathogens compromise the oral environment, leading to the degradation of crucial structures such as the alveolar bone and periodontal ligaments [1, 2]. Periodontal disease seriously affects the masticatory function of the patient [3, 4], and since it is the leading reason for tooth loss, it is being monitored in many nations [5]. The National Health and Nutrition Examination Survey is the only source of nationally representative data on periodontal disease, and it was reported that 42.2–46% of American adults aged ≥ 30 years have periodontitis, of which 7.8–8.9% have severe periodontitis [6].
Both the strength and the bulk of the muscles (sarcopenia components) decrease with increasing years [7, 8]. Muscular strength per unit of muscle mass is known as the muscle quality index (MQI), and it is used to predict the risk of mortality and disability [9, 10]. Handgrip strength (HGS) is calculated by dividing the amount of skeletal muscle in the appendicular region (ASM) [11], and by measuring HGS with muscle mass in the arms (lean soft tissue) [11, 12]. Results from the little study on the connection between HGS and periodontitis are inconsistent [13,14,15]. The HGS was negatively linked with periodontitis in the Korean population [13, 15], but not in the American population [14]. Also, one study from South Korea looked at the link between HGS and periodontitis, and when confounding factors were taken into account, the link was not significant [13]. These studies only explored the effect of HGS on the risk of periodontitis and seldom used the comprehensive new muscle quality index [16]. Therefore, the purpose of the present research was to examine the link between muscle quality index and moderate/severe periodontitis after controlling for possible confounders among the American adult population.
Materials and methods
Study participants
We used cross-sectional data from the National Health and Nutrition Examination Survey for the years 2011 to 2014 (NHANES). Survey samples need to be representative of the whole US population. The survey data will be used to estimate the prevalence of different diseases and risk factors. To gather data, personal structured interviews were conducted at home, health examinations were conducted in a mobile examination center, and specimens were analyzed in the laboratory. NHANES was approved by the National Center for Health Statistics Research Ethics Review Board. Data may be accessed for free on the Centers for Disease Control and Prevention (CDC) website (https://wwwn.cdc.gov/nchs/nhanes/Default.aspx).
The data collection was compiled from two successive NHANES cycles, 2011–2012 and 2013–2014. Among the participants in NHANES (2011–2014) (19,931 individuals), participants were selected for the research based on the following criteria: (1) age ≥ 30 years; (2) complete handgrip test; (3) diagnosis criteria of periodontitis; and (4) the lack of rheumatoid arthritis, which is a group of disorders that may affect a person’s ability to hold on to things with their hands. Due to a lack of body composition data for individuals older than 60 years old, males and females between the ages of 30 and 59 were included in the study. The lack of HGS tests from both hands, the absence of DXA data, the presence of hand discomfort or stiffness, and surgery on either hand were our criteria for excluding participants. A flow chart is displayed in Fig. 1.
Study variables
Muscle quality index
DXA, which was calibrated daily, was used to assess body composition, and findings were obtained using HologicQDR-4500 software, version Apex 3.2. (Hologic, America). Before the DXA examination, volunteers were told to refrain from using contrast or radiation in any other procedures. Body fat mass (kg and %), total lean tissue (kg), arm ASM mass (kg), and leg ASM mass were the data sources utilized in this investigation. To be consistent with the literature, we referred to lean soft tissue from limbs as adipose soft tissue (ASM). Notably, DXA-derived lean soft tissue mass is considered non-fat and non-bone tissue [7]. ASM was defined as the total of lean soft tissue from four limbs; ASM index (ASMI) was determined as the total of ASM from both arms and legs (kg)/height2 (m2) [17]. Additional information on the DXA methods may be detected on the NHANES website (https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DXX_H.htm).
A Takei dynamometer was used to measure HGS (TKK 5401; Takei Scientific Instruments, Tokyo, Japan). The participants stood with their wrists in a neutral position and their arms extended straight down. They were told to apply maximum force on the dynamometer. Each measurement was taken three times, with a 60-s break in between, for both the dominant and non-dominant hands. The dominating hand’s greatest value was employed (https://www.cdc.gov/nchs/data/nhanes/ms.pdf). The ratio of the dominant arm’s HGS to its ASM is known as MQIArm (kg/kg)10. MQIApp (kg/kg) was computed as the ratio of dominant HGS to ASM [16], and MQItotal (kg/kg) was determined by dividing the total HGS (values from both hands) by the average weight of each hand [18].
Periodontitis
A dental examiner conducted the periodontal examination at the mobile Examination Center. Adults over the age of 30 years were eligible for a whole periodontal evaluation, which contained an evaluation of attachment loss (AL) and probing depth (PD). Based on the results of the NHANES survey, the CDC and the American Periodontal Association (AAP) have come up with four grades for the cases of periodontitis monitored by PD and AL: none, mild, moderate, and severe [19]. Two interproximal sites with AL measuring 6 mm (not on the same tooth) and one interproximal site with PD measuring 5 mm were considered severe periodontitis. Two interproximal sites with AL distances of 4 mm (not on the same tooth) or two interproximal sites with PD distances of 5 mm (not on the same tooth) were considered moderate periodontitis. PPD ≥ 4 mm in two or more interproximal locations (or PD ≥ 5 mm in one location) and CAL at least 3 mm but not ≥ 4 mm in two or more interproximal locations were considered mild periodontitis [19]. The participants were dichotomized as no/mild periodontitis and moderate/severe periodontitis [14, 20].
Other covariables
The self-reported participants’ demographic information, including age, gender, marital status, household income, and education level via the initial screening questionnaire. The population was divided into the following categories: White non-Hispanics, Mexican Americans, Asian non-Hispanics, Black non-Hispanics, and others (Including Multi-Racial and Other Hispanic populations). Family poverty-income ratio (PIR) data were used to categorize household income according to its relationship to poverty and divided into three categories: low income (PIR 1.3), medium income (1.3 < PIR < 3.), and high income (> 3.5) [21]. The education level was categorized as less than ninth grade, ninth to eleventh grade, high school graduate, some college or associate (AA) degree, and college graduate or higher. The body mass index (BMI) was imputed using the following formula: body mass (kg)/height squared (m2) [22]. Smokers were divided into three categories: never-smokers, current smokers (those who have smoked more than 100 cigarettes in their lifetime), and past smokers (those who have smoked more than 100 cigarettes but have given up). Alcohol use was categorized as never, former, mild, moderate, and heavy. The diagnosis of chronic kidney disease and cardiovascular disease, rheumatoid arthritis, and diabetes was determined by the physician’s report of whether the individual had chronic kidney disease, cardiovascular disease, rheumatoid arthritis, or diabetes.
Statistical analysis
Due to the intricate nature of the survey design, the statistical analysis takes into account the sample weight for analysis following CDC recommendations. For accurate national population estimates, sample weights and main sampling units were used in all analyses. The participants were classified into four groups for baseline information using the MQI quartiles. Continuous variables are expressed as survey-weighted mean (95% CI) and categorical variables as percentages (95% CI). The baseline characteristics for continuous and categorical variables were compared using weighted linear regression and weighted Chi-square analysis, respectively. Using weighted multivariable logistic regression equations, we evaluate the connection between MQI and periodontitis. Linear trend tests were used to assess the consistency of the association. The non-linear association was then investigated using generalized additive models (GAMs) and smooth curve fittings. The inflection point was inferred from the smoothing curve using a recursive method, which was used by two-piecewise linear regression models. Adjusting the model for the aforementioned possible confounders, we conducted subgroup analyses and interaction analyses for categorical covariables such as age, gender, CVD, CKD, DM, Hypertension, alcohol consumption, smoking, and BMI. Last but not least, we did a mediation analysis using the product of coefficients method and compared the indirect effect of MQItotal on periodontitis through alcohol consumption to the total effect of MQItotal on periodontitis [23, 24]. All analyses were conducted using R software. A P value less than 0.05 was considered statistically significant.
Result
Baseline characteristics
A total of 3,258 individuals, with a mean age of 44.51 ± 9.6 years, were considered eligible for the study. In all, the weighted average MQIArm (kg/kg), MQIApp (kg/kg), and MQItotal (kg/kg) values were 12.58, 1.73, and 3.37 kg/kg, respectively. And 37.45% of participants had moderate/severe periodontitis. The most of individuals were males (50.58%) and white (41.34%) non-Hispanics, with a mean BMI (kg/m2) of 29.24 6.53 kg/m2. The majority of the participants claimed to have more than 12 years of education (72.16%) and a high income (38.0%). Based on the MQI.total quartiles, Table 1 displays the weighted distribution of population features and variables. The MQI quartiles revealed no significant differences in periodontitis, cardiovascular disease, smoking, alcohol intake, or marital status. The participants in the group with the greatest MQItotal (Q4) have a higher probability of becoming male, younger, non-Hispanic white, have a greater level of education, a higher income, a lower BMI, and a decreased chance of developing diabetes.
Association between MQI and periodontitis
The link between MQI and the risk of periodontitis is shown in Table 2. As the adjusted variables were altered, the correlation weakened but was maintained. After adjusting for age, sex, race, marital status, and education level, the risk of periodontitis was significantly reduced. After adjusting for all confounding factors, the OR remain significant. When MQI was analyzed as a continuous variable in the whole adjusted logistic regression analysis model, a statistically significant link between MQIApp, MQIArm, and MQItotal and the risk of periodontitis was observed (MQItotal: OR 0.69, 95% CI 0.53–0.91, P = 0.0078; MQIApp: OR 0.49, 95% CI 0.30–0.80, P = 0.0049; MQIArm: OR 0.90, When the MQI was analyzed as categorical variables, the OR for the Q2, Q3, and Q4 groups compared to the Q1 group was still significant.
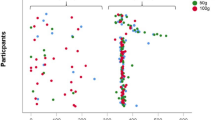
A significant relationship between dose and response was also found (MQIApp: P for trend = 0.013, MQItotal: P for trend = 0.003), but not for MQIarm (Table 3, Supplementary Tables 1 and 2). A linear association was detected between MQIarm and periodontitis (Supplementary Fig. 1A, B). A non-linear and J-shaped link was observed by GAM and smoothing curve, with a change point of 3.64 for MQItotal (Fig. 2A, B) and 2.06 for MQIArm (Supplementary Fig. 2A, B) threshold effect analysis. Before the turning point, there was a strong link between MQItotal and periodontitis (OR: 0.69, 95%:0.58–0.82, p < 0.0001). After the cut-off point, however, the link was non-significant (OR 1.27, 95% CI 0.95–1.72, P = 0.1109). Even when the relationship was stratified by gender, the relationship remained non-linear for MQItotal (Fig. 3). Similar findings were observed in Supplementary Figs. 3 and 4.
We also used a stratified analysis to explore whether there was a link between covariates and MQItotal and periodontitis (Table 4). There was a highly consistent negative correlation between the MQItotal and periodontitis across all subgroups. The impact of MQItotal on periodontitis was lower in people with females (OR 0.728, 95% CI 0.580–0.913, P = 0.008; P-interaction = 0.310). Compared with those who married or lived with a partner, those who never married had a lower risk of periodontitis (OR 0.606, 95% CI 0.444–0.828, P = 0.003, P-interaction = 0.008). Compared with subjects who currently smoke, those who never smoke or former smoke had a lower risk of periodontitis (never smoke: OR 0.727, 95% CI 0.583–0.906, P = 0.006, P-interaction = 0.100. Compared with subjects whose education level is less than 9th grade or 9-11th grade, those who obtain college graduate or above had a lower risk of periodontitis (Some college or AA degree: OR 0.665, 95% CI 0.503–0.877, P = 0.005; P-interaction = 0.055). Compared with subjects who smoke, those who never smoked had a lower risk of periodontitis (OR 0.616, 95% CI 0.457–0.829, P = 0.002, P-interaction = 0.042). Other covariates had no significant interaction on the correlation between MQItotal and periodontitis. Mediation analyses showed that 0.4% (95% CI 0.10 to 1.2; p = 0.01) of the observational association of MQItotal with the risk of periodontitis was mediated through alcohol use (Fig. 4).
Discussion
The primary findings of the study demonstrated that after controlling for confounding variables, it was found that the MQI and the risk of periodontitis were independently and negatively correlated, and the relationship was nonlinear among the US population aged over 30 years old. Following curve smoothing, we found that the positive correlation in the overall US population was J-shaped and showed a dose–response effect, with 3.60 being the change point and a considerably decreased risk of periodontitis with rising MQI.total before the turning point. Higher MQI was substantially correlated with variables including age, income, marital status, BMI, and chronic medical problems.
Currently, the KNHANES research investigated the association between RHGS and periodontitis [13]. However, after controlling for all confounders, the link was determined to be nonexistent. Another NHANES research examined the link between moderate/severe periodontitis and handgrip strength in the United States, and the results demonstrated that those with moderate/severe periodontitis had considerably lower grip strength. However, after controlling for possible confounding factors, the significance of the link vanished [14]. In the current investigation, MQI (MQIApp, MQIArm, and MQItotal) was linked with a reduced risk of periodontitis in people older than 30 years. Differences in the demographic studied (South Koreans), age of respondents (below 60), MQI definition, and periodontitis case classification (community periodontal index (CPI)) may account for the conflicting findings between this research and others on the association between MQI and periodontitis. In the research, periodontitis cases are classified based on whole mouth periodontal exploration of six regions of each tooth, except the third molar, which greatly increased the diagnostic accuracy of periodontitis [19]. Meanwhile, a more objective index (MQI) was employed to reflect muscle strength [16, 18].
The following factors may help explain the study’s findings. Periodontitis is caused mostly by the deposition of dental biofilm on the tooth surface [4, 25]. Biofilm is a sticky microbial population made up of over 700 distinct bacterial species that are bound to salivary glycoproteins [26]. Toothbrushing is the most basic and effective approach for removing dental biofilm [27]. However, the efficiency of manual teeth brushing is often dependent on several parameters, including brushing motions and hand motor performance [28, 29]. Particularly, poor finger or hand joint function is said to impact the degree of dental biofilm production [30, 31]. Growing data suggest a link between dental health and physical decline and weakness in old life [32,33,34]. Low hand grip strength is an essential indicator of physical decline in old age and one of the frailty phenotype’s defining characteristics [35].
In addition, alcohol use may mediate the relationship between muscle strength and periodontitis. It was well-known that alcohol use acted as a risk factor for periodontitis, and there was a link between drinking alcohol and a higher risk of developing periodontitis [36,37,38]. At the same time, Alcohol abuse increases the risk of sarcopenia through direct and indirect mechanisms associated with poor skeletal muscle protein metabolism, according to available research [39, 40]. Consumption of alcohol may result in dysbiosis and autophagy of the gut microbiota-induced hyperammonemia, which initiates the up-regulation of muscle protein breakdown and the down-regulation of muscle protein synthesis by activating myostatin, AMPK, and REDD1, and deactivating IGF-1. These changes take place as a result of the activation of myostatin, AMPK, and REDD1 as well as the activation of IGF-1 [41, 42].
Our study presents several limitations that warrant consideration. First and foremost, due to its cross-sectional design, it is imprudent to deduce a causal relationship between MQI and moderate to severe periodontitis. Second, the NHANES data from 2011–2014 did not encompass several recognized and potential confounders. Factors such as specific inflammatory markers and variations in daily tooth brushing habits, both in frequency and duration, were not incorporated into our analysis. Lastly, our reliance on the 2012 AAP/CDC periodontitis case definition may be perceived as a limitation. Historically, this definition was a cornerstone in global epidemiological studies concerning periodontal disease [6, 19]. However, in 2018, the EFP/AAP proposed a more nuanced classification system that nuances periodontitis based on its severity, complexity, and progression rate [43, 44]. Under this novel schema, maximum loss measurements at sites of 1–2 mm are denoted as incipient (stage 1), 3–4 mm as moderate (stage 2), and ≥ 5 mm as severe (stages 3 and 4) [43]. This transition to a newer classification system may affect the comparability and interpretation of our results in the broader context of recent periodontal research.
Nonetheless, this study holds significant importance. To our knowledge, it is the first to utilize NHANES data to examine the association between MQI and moderate to severe periodontitis among American adults. Our data suggest a consistent and independent inverse relationship between MQI levels and the risk of moderate to severe periodontitis. A comprehensive understanding of this association necessitates further prospective studies, taking into account both recognized and potential confounding factors.
Based on data from two NHANES surveys (2011–2012 and 2013–2014), we observed that the Muscle Quality Index (MQI) was independently and negatively associated with periodontitis in American adults over 30 years of age. Additionally, alcohol consumption appeared to mediate the relationship between MQI and periodontitis.
Availability of data and materials
The data supporting the findings of this study are available from the corresponding author upon request.
References
Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:17038.
Slots J. Periodontitis: facts, fallacies and the future. Periodontol 2000. 2017;75(1):7–23.
Sharaf S, Hijazi K. Modulatory mechanisms of pathogenicity in porphyromonas gingivalis and other periodontal pathobionts. Microorganisms. 2022;11(1):15.
Kwon T, Lamster IB, Levin L. Current concepts in the management of periodontitis. Int Dent J. 2021;71(6):462–76.
Nilsson H, Berglund JS, Renvert S. Periodontitis, tooth loss and cognitive functions among older adults. Clin Oral Investig. 2018;22(5):2103–9.
Eke PI, Borgnakke WS, Genco RJ. Recent epidemiologic trends in periodontitis in the USA. Periodontol 2000. 2020;82(1):257–67.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(4):601.
Landi F, Calvani R, Martone AM, et al. Normative values of muscle strength across ages in a ‘real world’ population: results from the longevity check-up 7+ project. J Cachexia Sarcopenia Muscle. 2020;11(6):1562–9.
Reinders I, Murphy RA, Koster A, et al. Muscle quality and muscle fat infiltration in relation to incident mobility disability and gait speed decline: the age, gene/environment susceptibility-reykjavik study. J Gerontol A Biol Sci Med Sci. 2015;70(8):1030–6.
Hairi NN, Cumming RG, Naganathan V, et al. Loss of muscle strength, mass (sarcopenia), and quality (specific force) and its relationship with functional limitation and physical disability: the Concord Health and Ageing in Men Project. J Am Geriatr Soc. 2010;58(11):2055–62.
Yoda M, Inaba M, Okuno S, et al. Poor muscle quality as a predictor of high mortality independent of diabetes in hemodialysis patients. Biomed Pharmacother. 2012;66(4):266–70.
Sui SX, Holloway-Kew KL, Hyde NK, et al. Handgrip strength and muscle quality in Australian women: cross-sectional data from the Geelong Osteoporosis Study. J Cachexia Sarcopenia Muscle. 2020;11(3):690–7.
Kim JE, Kim NY, Choi CH, Chung KH. Association between oral health status and relative handgrip strength in 11,337 Korean. J Clin Med. 2021;10(22):5425.
Aravindakshan V, Hakeem FF, Sabbah W. Periodontal disease and grip strength among older adults. Geriatrics (Basel). 2020;5(3):46.
An HR, Choi JS. Association between handgrip strength and periodontitis in Korean adults aged >/=30 years: data from the Korea national health and nutrition examination survey (2014–2015). Int J Environ Res Public Health. 2022;19(17):10598.
Barbat-Artigas S, Rolland Y, Zamboni M, Aubertin-Leheudre M. How to assess functional status: a new muscle quality index. J Nutr Health Aging. 2012;16(1):67–77.
Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147(8):755–63.
Lopes LCC, Vaz-Goncalves L, Schincaglia RM, et al. Sex and population-specific cutoff values of muscle quality index: results from NHANES 2011–2014. Clin Nutr. 2022;41(6):1328–34.
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ. Update of the case definitions for population-based surveillance of periodontitis. J Periodontol. 2012;83(12):1449–54.
Weintraub JA, Lopez Mitnik G, Dye BA. Oral diseases associated with nonalcoholic fatty liver disease in the United States. J Dent Res. 2019;98(11):1219–26.
Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of obesity among youths by household income and education level of head of household - United States 2011–2014. MMWR Morb Mortal Wkly Rep. 2018;67(6):186–9.
Organization WH. Obesity: preventing and managing the global epidemic: report of a WHO consultation. 2000.
Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309–34.
Afzal S, Brondum-Jacobsen P, Bojesen SE, Nordestgaard BG. Vitamin D concentration, obesity, and risk of diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol. 2014;2(4):298–306.
Larsen T, Fiehn NE. Dental biofilm infections - an update. APMIS. 2017;125(4):376–84.
Dewhirst FE, Chen T, Izard J, et al. The human oral microbiome. J Bacteriol. 2010;192(19):5002–17.
Rosema NA, Hennequin-Hoenderdos NL, Versteeg PA, et al. Plaque-removing efficacy of new and used manual toothbrushes--a professional brushing study. Int J Dent Hyg. 2013:11(4):237–43.
Digel I, Kern I, Geenen EM, Akimbekov N. Dental plaque removal by ultrasonic toothbrushes. Dent J (Basel). 2020;8(1):28.
Arweiler NB, Auschill TM, Sculean A. Patient self-care of periodontal pocket infections. Periodontol 2000. 2018;76(1):164–79.
Poole JL, Brewer C, Rossie K, Good CC, Conte C, Steen V. Factors related to oral hygiene in persons with scleroderma. Int J Dent Hyg. 2005;3(1):13–7.
Padilha DM, Hugo FN, Hilgert JB, Dal Moro RG. Hand function and oral hygiene in older institutionalized Brazilians. J Am Geriatr Soc. 2007;55(9):1333–8.
Hakeem FF, Bernabe E, Sabbah W. Association between oral health and frailty: a systematic review of longitudinal studies. Gerodontology. 2019;36(3):205–15.
Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor oral health as a determinant of malnutrition and sarcopenia. Nutrients. 2019;11(12):2898.
MacEntee MI, Donnelly LR. Oral health and the frailty syndrome. Periodontol 2000. 2016;72(1):135–41.
Cederholm T. Overlaps between frailty and sarcopenia definitions. Nestle Nutr Inst Workshop Ser. 2015;83:65–9.
Gay IC, Tran DT, Paquette DW. Alcohol intake and periodontitis in adults aged >/=30 years: NHANES 2009–2012. J Periodontol. 2018;89(6):625–34.
Wang J, Lv J, Wang W, Jiang X. Alcohol consumption and risk of periodontitis: a meta-analysis. J Clin Periodontol. 2016;43(7):572–83.
Amaral Cda S, Vettore MV, Leao A. The relationship of alcohol dependence and alcohol consumption with periodontitis: a systematic review. J Dent. 2009;37(9):643–51.
Preedy VR, Adachi J, Ueno Y, et al. Alcoholic skeletal muscle myopathy: definitions, features, contribution of neuropathy, impact and diagnosis. Eur J Neurol. 2001;8(6):677–87.
Yoo JI, Ha YC, Lee YK, Hana C, Yoo MJ, Koo KH. High prevalence of sarcopenia among binge drinking elderly women: a nationwide population-based study. BMC Geriatr. 2017;17(1):114.
Prokopidis K, Witard OC. Understanding the role of smoking and chronic excess alcohol consumption on reduced caloric intake and the development of sarcopenia. Nutr Res Rev. 2022;35(2):197–206.
Capurso G, Lahner E. The interaction between smoking, alcohol and the gut microbiome. Best Pract Res Clin Gastroenterol. 2017;31(5):579–88.
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–72.
Botelho J, Machado V, Proenca L, Mendes JJ. The 2018 periodontitis case definition improves accuracy performance of full-mouth partial diagnostic protocols. Sci Rep. 2020;10(1):7093.
Acknowledgements
The authors would like to thank the NHANES and its anonymous participants.
Funding
None.
Ethics declarations
Ethics approval and consent to participate
NHANES protocol approved by NCHS Research Ethics Review Board, and obtained informed consent from all participants (https://www.cdc.gov/nchs/nhanes/irba98.htm). And all methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure 1.
Dose-response relationship between MQIarm and periodontitis. A. is for the continuous variable of MQIarm, and B is the categorical variable of MQIarm. Supplementary Figure 2. Dose-response relationship between MQIapp and periodontitis. A. is for the continuous variable of MQIapp, and B is the categorical variable of MQIapp. Supplementary Figure 3. The association between MQIarm and periodontitis stratified by sex. Supplementary Figure 4. The association between MQIapp and periodontitis stratified by sex. Supplementary Table 1. Threshold Effect Analysis between MQIapp and periodontitis. Supplementary Table 2. Threshold Effect Analysis between MQIarm and periodontitis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, J., Wu, Y., Ma, H. et al. Association between muscle quality index and periodontal disease among American adults aged ≥ 30 years: a cross-sectional study and mediation analysis. BMC Oral Health 23, 918 (2023). https://doi.org/10.1186/s12903-023-03520-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03520-y