Abstract
Background
The development of periodontal disease is closely linked to individual oral healthcare behaviors. This study aimed to investigate the knowledge, attitude, and practice (KAP) toward the self-control of dental plaque among patients with periodontal diseases.
Methods
This cross-sectional study was conducted at Jinan Stomatological Hospital between July 2022 and September 2022 through a self-administrated questionnaire for patients with periodontal diseases.
Results
A total of 563 participants were included. Among them, 147 (26.11%) had gingivitis and 416 (73.89%) had periodontitis. Participants' knowledge, attitude, and practice scores were 8.71 ± 2.81 (range 0–12), 39.82 ± 3.69 (range 10–50), 33.13 ± 5.91 (range 11–55), respectively. The multivariate logistic regression analysis showed that the knowledge [odds ratio (OR) = 1.212, 95% confidence interval (CI): 1.097–1.339, P < 0.001], attitude (OR = 1.132, 95% CI: 1.070–1.198, P < 0.001), occupation, especially in the commercial and service industry (OR = 0.488, 95% CI: 0.221–1.080, P = 0.007), and income of 10,000–20,000 yuan (OR = 0.476, 95% CI: 0.258–0.877, P = 0.017) were independently associated with good practice.
Conclusions
Chinese patients with periodontal diseases demonstrated satisfactory knowledge and attitudes regarding oral hygiene, but the practical aspects need more promotion and training, especially in daily brushing frequency, usage of oral irrigator and interdental brush. Individualized approach should consider patients' knowledge, attitudes, occupation and income level.
Similar content being viewed by others
Background
Periodontal inflammation progresses from gingival epithelium towards the periodontum, resulting in the numerous esthetic and functional problems, breakdown of the supporting periodontal tissues and tooth loss [1,2,3]. At present, the accepted three-factor theory of periodontitis is based on the interplay between acquired environmental factors, pathogenic oral bacteria and host factors [4, 5]. Although the development of clinically evidenced periodontitis usually takes time, aggressive forms may develop quickly, leading to the obvious decrease in the quality of life [5]. Moreover, periodontitis is the sixth most common disease worldwide, and severe periodontitis affects approximately 10% of the global population [6]. According to the Third National Oral Health Epidemiological Survey, the state of periodontal health in China is also poor, with 86% of the Chinese population suffering from varying degrees of periodontitis [7].
The treatment strategies for periodontal disease are based on the combination of periodontal therapeutic modalities to minimize symptoms and restore lost tissues, including subgingival instrumentation, local and/or systemic pharmacotherapy, and periodontal surgery [1]. The prevention of periodontitis involves, first and foremost, meticulous oral hygiene by tooth brushing, use of powered toothbrushes and interdental brushes, fluoridated toothpaste, flossing, and mouth rinses [3]. In addition, recent studies reported that uncontrolled diabetes mellitus, vitamin D insufficiency and smoking increase the susceptibility and severity of periodontitis [1, 3]. Therefore, enhancing individuals' knowledge of the protection of periodontitis and improving their oral healthcare behaviors are key initiatives in preventing and controlling periodontitis.
Knowledge, attitude, and practice (KAP) study is a structured survey method that can be applied to measure the known behaviors toward the medical conditions or preventive methods, and reveal obstacles to the activities or behavioral changes [8]. The KAP study serves as an information source and a predecessor of awareness or intervention programs to draw attention to the specific problem among the study population and beyond [9]. Despite the importance of individuals' knowledge on preventing and controlling periodontal disease, only a few KAP studies have been conducted so far. Although KAP in dentists and medical students are mostly encouraging [10, 11], in general population oral hygiene practices need to be improved [12]. To the best of our knowledge no KAP studies on oral healthcare behaviors were undertaken among patients with periodontitis in China.
Therefore, this cross-sectional study aimed to investigate KAP patterns toward the self-control of dental plaques among patients with periodontitis in China.
Methods
Study design and participants
This cross-sectional study was conducted at Jinan Stomatological Hospital between July 1, 2022, and September 30, 2022. Periodontitis was defined according to the new International Classification of Periodontal Diseases [13], based on the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions [14]. Patients with periodontitis aged 16–70 years, who understood the purpose of the study and volunteered to participate were included, while incomplete questionnaires were excluded. This study was ethically approved by the medical ethics committee of Jinan Stomatological Hospital (No.JNSKQYY-2022–018), and informed consent was obtained from all participants.
Procedures
This questionnaire was based on the Medical Staff Manual of Oral Health Behaviour Guidelines for Chinese Residents and the consensus of Chinese multidisciplinary experts on maintaining periodontal health [15], as well as previous studies accessing knowledge and practice of oral hygiene [16, 17] and revised with reference to comments made by three experts in periodontitis. The final version of questionnaire was distributed in Chinese and contained four dimensions, as follows: (1) demographic information about the participants; (2) knowledge assessment based on 12 questions about periodontal disease and control of dental plaques, scored 1 point for correct answers and 0 points for incorrect or unclear answers; total score ranging from 0 to 12 points; (3) attitude toward the self-control of dental plaques based on 10 questions, all using 5-point Likert scale, ranging from very positive (5) to very negative (1); total score ranging from 10 to 50 points; (4) practice among patients with periodontitis toward the self-control of dental plaques, based on 11 questions, also using 5-point Likert scale, ranging from always (5) to never (1), with a score range of 11–55 points.
The questions in this study showed high internal consistency with Cronbach’s α = 0.860 and Kaiser–Meyer–Olkin (KMO) = 0.8614. Hardcopy questionnaires were distributed in the diagnostic room and completed by patients; the clinical information was also collected at the same time. The web-based questionnaire was created and distributed using Questionnaire Star (Changsha Ranxing Information Technology Co., Ltd), which patients scanned to generate a quick response (QR) code to participate in this study. Considering that some of the patients were uncomfortable using cell phones to respond, a hardcopy version of the questionnaire was prepared and filled out by the patients after a trained research assistant explained the purpose and content of the study. All questionnaires were checked for completeness, consistency, and validity by the members of the research team.
Statistical analysis
SPSS 26.0 (IBM Corp., NY, USA) was used for statistical analysis. Continuous data were expressed as mean ± standard deviation (SD) and compared by t-test. The categorical data were expressed as n (%) and compared with the chi-square test. Pearson’s correlation was used to analyze the correlations between knowledge scores, attitude scores, and practice scores. The univariable and multivariable logistic regression analyses were used to analyze the factors influencing practice; 70% of the practice score was used as the cut-off value. All statistical tests were performed using two-sided tests, and P values < 0.05 indicated statistically significant differences.
Results
A total of 563 questionnaires were finally enrolled in this study, and the participants' knowledge scores were 8.71 ± 2.81 (range 0–12), attitude scores were 39.82 ± 3.69 (range 10–50), and practice scores were 33.13 ± 5.91 (range 11–55). Among them, 147 (26.11%) participants had gingivitis and 416 (73.89%) had periodontitis; the female participants accounted for 57.55%. As demonstrated in Table 1, most participants were from urban areas (92.54%), smoked (84.37%). Among them, 7.10% of the participants were younger than 20 years and 17.94% were older than 50 years. Almost a quarter of participants reported the frequency of toothbrushing per day as 0–1 times (24.16%), while others brushed their teeth 2 times or more.
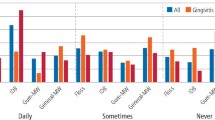
In the knowledge dimension (Table 2), the most correctly answered question was about the minimal number of toothbrushings needed per day (90.76% of the participants answered correctly), while the least correct was the “Bass method” (53.82%). In the attitude dimension (Fig. 1), the participants demonstrated a positive attitude toward the “self-control of plaque” aspect (98.80%), while a small number reported feeling anxious toward their periodontitis (22.90%). In the practice dimension (Fig. 2), the initiative for self-learning was the most notable (82.60%), while the use of an oral irrigator was the least frequent practice (8.20%).
Pearson correlation analysis showed that the correlation between knowledge and practice (r = 0.313, P < 0.001). In contrast, the correlations between attitude and knowledge (r = 0.287, P < 0.001) as well as attitude and practice (r = 0.275, P < 0.001) were slightly less strong (Table 3).
The multivariate logistic regression analysis showed that the knowledge (OR = 1.212, 95% CI: 1.097–1.339, P < 0.001) and attitude (OR = 1.132, 95% CI: 1.070–1.198, P < 0.001) were independently associated with good practice. At the same time, occupation, such as the commercial and service industry (OR = 0.488, 95% CI: 0.221–1.080, P = 0.007) and with income level of 10,000–20,000 yuan (OR = 0.476, 95% CI: 0.258–0.877, P = 0.017) were the independent predictors of poor practice. Although the education level was also shown to be linked to better practice patterns by the univariate analysis, the multivariate analysis did not confirm statistical significance (P = 0.407). Finally, among other habits, better practice patterns were linked to the frequency of toothbrushing 2–3 times per day (OR = 1.697, 95% CI: 1.013–2.844, P = 0.044) and > 3 times per day (OR = 5.742, 95% CI: 1.688–19.530, P = 0.005) (Table 4). Subgroup analyses were performed considering the differences in consultation status, taking into account the relatively stable conditions, patient education, and good compliance observed among the follow-up patients who had undergone secondary consultation, in comparison to those who had received initial consultation (Supplementary Table 1 & Supplementary Table 2).
The comparison of KAP patterns between patients with gingivitis and periodontitis is demonstrated in Table 5. There were no significant differences in most knowledge and practices, while, in the attitude dimension, the notion of postponing or canceling the consultation due to the fear of dental treatment was more typical for patients with chronic gingivitis (P = 0.038).
Discussion
This study found that the knowledge and attitudes toward oral hygiene among patients with periodontitis in China was satisfactory while practice may need to be improved. In addition to knowledge and attitudes, patients' occupation, income level, and daily brushing frequency may also influence their practice. These results might lead to divergence in periodontitis situation and changes in oral hygiene habits in patients who are aware of their diagnosis.
Knowledge and practice of oral hygiene in China are relatively poor, especially among 35- to 45-year-old and 65- to 74-year-old groups [18, 19]. This study included all age groups, and although knowledge and attitude differed slightly in different age groups, age was not associated with better practice scores. With the majority of participants demonstrating satisfactory knowledge, the mean practice scores were not high (33.13 out of 55), but many oral hygiene habits were practiced more often compared to general population. In particular, previous study by Zhu et al. [20] reported that only 32% of the 35- to 44-year-olds and 23% of the 65- to 74-year-olds brushed their teeth at least twice a day, while in this study, almost three fourths of all participants reported brushing their teeth 2 times per day or more often. In the study by An et al. [19] conducted during the same period, only 26.3% of participants used fluoride toothpaste and 73.7% did not apply or did not know about fluoride toothpaste. However, in the present study, fluoride toothpaste was used often or always by 42.1% and occasionally by 39.3% of participants. These results suggested that patients with periodontitis might be more informed about oral hygiene than the general population, most likely because of the information received during previous visits to the dentist.
Some studies reported the unsatisfactory effect of oral health education as a primary preventive method in China [19, 21]. In this study, the initiative for self-learning was the most notable (82.6%), but more practical aspects still need promotion and training, such as oral irrigator (used often or always by only 8.2% of participants) or interdental brush (used often or always by 14.6%). Knowledge was linked to practice slightly more than attitude, which was in line with previous studies conducted in China [21, 22] and worldwide [16, 23]. In patients who belonged to the risk groups for periodontitis more positive attitudes and proactive seeking for more oral health knowledge might lead to better practice [23, 24]. On the other hand in this study a positive attitude was more likely found in the answers that were impossible to check, and the actual behavior might differ. This discrepancy between actual and reported attitude should be taken into account in the future studies.
According to the most recent national health survey, Chinese adults who seek dental care services already have poor oral conditions and need treatment rather than prevention [25]. In this study, occupations such as commercial and service industry were independent factors related to better practice, suggesting that more frequent human contact needed in daily jobs might play an important role for Chinese adults, influencing better practice. At the same time, despite recent reports [26, 27] that participants with higher education levels tended to have better oral health hygiene, the multivariate analysis in this study did not confirm statistically significant correlations between education level and better practice patterns (P = 0.407) for the study population. As noted earlier, these differences were most likely explained by the knowledge obtained during the previous visits to the dentist, as well as the predominantly urban population in this study. Thus, the educational interventions carried out by dentists for the patients with periodontitis have the potential to promote the self-control of dental plaques in the population.
This study had some limitations. First, the cross-sectional design did not allow for concluding causal relationships; the questionnaire was self-designed, leading to lower applicability of the obtained results. Second, noticeable differences might exist between the reported and actual behaviors, as participants filled out the questionnaire in the hospital and thus might naturally want to appear more conscious and knowledgeable. Finally, although the study population was not small, most participants lived in urban areas; the oral hygiene practice and periodontitis prevention practice were reportedly worse in rural areas. These limitations should be taken into account while interpreting the aforementioned results and planning future studies.
Conclusion
In conclusion, this study found that Chinese patients with periodontitis demonstrated satisfactory knowledge and attitudes about plaque control, but the practical aspects, such as usage of oral irrigator and interdental brush need more promotion and training. Patients’ knowledge, attitudes, occupation, income level, and daily brushing frequency may influence their practice. These findings might contribute to the ongoing effort of enhancing individuals’ knowledge of oral hygiene and other key initiatives in preventing and controlling periodontitis in China and worldwide.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- KAP:
-
Knowledge, attitude, and practice
- KMO:
-
Kaiser-Meyer-Olkin
- QR:
-
Quick response
- SD:
-
Standard deviation
References
Machado V, Lobo S, Proença L, Mendes JJ, Botelho J. Vitamin D and periodontitis: a systematic review and meta-analysis. Nutrients. 2020;12(8):2177.
Carvalho CV, Saraiva L, Bauer FPF, Kimura RY, Souto MLS, Bernardo CC, Pannuti CM, Romito GA, Pustiglioni FE. Orthodontic treatment in patients with aggressive periodontitis. Am J Orthod Dentofacial Orthop. 2018;153(4):550–7.
Kumar S. Evidence-based update on diagnosis and management of gingivitis and periodontitis. Dent Clin North Am. 2019;63(1):69–81.
Shaddox LM, Morford LA, Nibali L. Periodontal health and disease: the contribution of genetics. Periodontol 2000. 2021;85(1):161–81.
Suzuki S, Yamada S. Epigenetics in susceptibility, progression, and diagnosis of periodontitis. Jan Dent Sci Rev. 2022;58:183–92.
Frencken JE, Sharma P, Stenhouse L, Green D, Laverty D, Dietrich T. Global epidemiology of dental caries and severe periodontitis - a comprehensive review. J Clin Periodontol. 2017;44(Suppl 18):S94-s105.
Qi X. The third national oral health epidemiological survey. People’s Medical Publishing House; 2008.
He Q, Wang G, He J, Wang Y, Zhang J, Luo B, Chen P, Luo X, Ren J. Knowledge, attitude and practice regarding occupational protection against COVID-19 among midwives in China: a nationwide cross-sectional study. Int J Disaster Risk Reduct. 2022;79:103184.
Andrade C, Menon V, Ameen S, Kumar Praharaj S. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian J Psychol Med. 2020;42(5):478–81.
Hocaoğulları SV. Evaluation of knowledge and awareness of medical students about the relationship between the periodontal diseases and diabetes mellitus. Marmara Universitesi (Turkey); 2019.
Roshene R, Gurunathan D: Periodontal disease diagnosis and treatment pattern by pediatric dentists. Drug Invent Today. 2019;12(4):857–61.
Martínez M, Montero E, Carasol M, LLodrá JC, Sanz M, Herrera D, Calvo-Bonacho E, Fernández-Meseguer A, Figuero E. Association between caries and periodontal diseases in a sample of employed adults in Spain: a cross-sectional study. Clin Oral Investig. 2021;25(6):3957–66.
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M, Tonetti MS. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1-s8.
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, et al. Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol. 2018;89(Suppl 1):S173-s182.
Zhou X, Xu X, Li J, Hu D, Hu T, Yin W, Fan Y, Zhang X. Oral health in China: from vision to action. Int J Oral Sci. 2018;10(1):1.
Varela-Centelles P, Diz-Iglesias P, Estany-Gestal A, Seoane-Romero JM, Bugarín-González R, Seoane J. Periodontitis awareness amongst the general public: a critical systematic review to identify gaps of knowledge. J Periodontol. 2016;87(4):403–15.
Saloux A, Couatarmanach A, Chauvel B, Jeanne S, Brezulier D. Knowledge, attitudes and professional practices of ortho-periodontal care of adults: a cross-sectional survey in France. BMC Oral Health. 2022;22(1):142.
Liu J, Zhang SS, Zheng SG, Xu T, Si Y. Oral health status and oral health care model in China. Chin J Dent Res. 2016;19(4):207–15.
An R, Li S, Li Q, Luo Y, Wu Z, Liu M, Chen W. Oral health behaviors and oral health-related quality of life among dental patients in china: a cross-sectional study. Patient Prefer Adherence. 2022;16:3045–58.
Zhu L, Petersen PE, Wang HY, Bian JY, Zhang BX. Oral health knowledge, attitudes and behaviour of adults in China. Int Dent J. 2005;55(4):231–41.
Wu Z, Li M, Zhu F, Lei L, Cheng R, Hu T. The effects of oral health education regarding periodontal health on non-dental undergraduates in southwestern China-exploring the feasibility of an e-learning course for oral health promotion. BMC Oral Health. 2021;21(1):119.
Li M, Wu Z, Zhang R, Lei L, Ye S, Cheng R, Hu T. Comparison of oral health behaviour between dental and non-dental undergraduates in a university in southwestern China–exploring the future priority for oral health education. BMC Oral Health. 2020;20(1):249.
Tuncer E, Darby I. Knowledge and attitudes towards periodontal health among Australians diagnosed with diabetes. Aust J Prim Health. 2021;27(6):509–13.
Akl S, Ranatunga M, Long S, Jennings E, Nimmo A. A systematic review investigating patient knowledge and awareness on the association between oral health and their systemic condition. BMC Public Health. 2021;21(1):2077.
Ou X, Zeng L, Zeng Y, Pei Y, Zhang X, Wu W, Siamdoust S, Wu B. Health behaviors and tooth retention among older adults in China: findings from the 4th Chinese national oral health survey. BMC Oral Health. 2022;22(1):285.
Dumitrescu R, Sava-Rosianu R, Jumanca D, Balean O, Damian LR, Fratila AD, Maricutoiu L, Hajdu AI, Focht R, Dumitrache MA, et al. The impact of parental education on schoolchildren’s oral health-a multicenter cross-sectional study in Romania. Int J Environ Res Public Health. 2022;19(17):11102.
Chen L, Hong J, Xiong D, Zhang L, Li Y, Huang S, Hua F. Are parents’ education levels associated with either their oral health knowledge or their children’s oral health behaviors? A survey of 8446 families in Wuhan. BMC Oral Health. 2020;20(1):203.
Acknowledgements
The authors would like to thank the experts who contributed to this study, the researchers who assisted in the carrying out of the study and all participants for their significant contributions.
Funding
The study was supported by grants from the Open Foundation of Shandong Province Key Laboratory of Oral Tissue Regeneration (SDDX202003) to Jing Sun, the Second Batch of Science and Technology Plan Projects of Jinan Municipal Health Commission (2020–3-49) to Jing Sun and the Dean’ Research Fund of Jinan Stomatological Hospital (2021–01, 2021–03, 2019–06, 2018–05).
Author information
Authors and Affiliations
Contributions
JS, DT and JM carried out the studies, participated in collecting data, and drafted the manuscript. CS, ZZ and XW performed the statistical analysis and participated in its design. YL, LQ, LK and XL participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by the Ethic Committee of Jinan Stomatological Hospital (No.JNSKQYY-2022–018), and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. Subgroup analysis for initial consultation.
Additional file 2:
Supplementary Table 2. Subgroup analysis for secondary consultation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, J., Tong, D., Sun, C. et al. Knowledge, attitude, and practice toward self-control of dental plaque among patients with periodontal diseases: a cross-sectional study. BMC Oral Health 23, 628 (2023). https://doi.org/10.1186/s12903-023-03352-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03352-w