Abstract
Background
The correlation between temporomandibular disorders (TMD) and imaging features remains unclear. This study compared the cone beam computed tomography (CBCT) and magnetic resonance imaging (MRI) features in the temporomandibular joints (TMJs) with and without TMD symptoms.
Methods
The participants were recruited from the TMJ Diagnosis and Treatment Center from March 2022 to September 2022. Condylar morphology and condylar position were evaluated by CBCT. Disc morphology, disc position, and joint effusion were evaluated by T2-weighted image of MRI. The Chi-Square test and binary logistic regression analysis were carried out.
Results
Eighty-two patients with bilateral symptoms, 196 patients with unilateral symptoms, and 79 asymptomatic participants received MRI and CBCT examination. There were significant differences in the distribution of sex, age, condylar morphology, condylar position, disc morphology, disc position, and joint effusion in symptomatic and asymptomatic TMJs (P < 0.05), which showed a positive correlation with symptoms (P < 0.05). In multiple logistic regression, 19–30-year-age group, > 30-year-age group, abnormal condylar morphology, posterior condylar position, disc displacement with reduction (DDWR), and disc displacement without reduction (DDWoR) were found to be statistically significant (P < 0.05). The odds of having symptomatic TMJ were 1.952 higher in the 19–30-year-age group and 1.814 higher in the > 30-year-age group when compared to those aged ≤ 18-year-age group. The odds of having symptomatic TMJ were 2.360 higher in persons with abnormal condylar morphology when compared to those with normal condylar morphology. The odds of having symptomatic TMJ were 2.591 higher in persons with posterior condylar position when compared to those with the normal condylar position. The odds of having symptomatic TMJ were 2.764 higher in persons with DDWR and 4.189 higher in persons with DDWoR when compared to those with normal disc position. The area under the curve of the model was 0.736 ± 0.019 (95% CI 0.700–0.773, P = 0.000), which indicated that the model has a good fitting effect.
Conclusions
The imaging findings of TMJs were significantly different between symptomatic and asymptomatic TMJs. TMD is affected by multiple factors including > 19-year-age, abnormal condylar morphology, posterior condylar position, DDWR, and DDWoR, which could be risk factors for the development of TMD symptoms.
Trial registration This study was retrospectively registered on 28/03/2022 and endorsed by the Ethics Committee of Affiliated Stomatology Hospital of Guangzhou Medical University (LCYJ2022014).
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Temporomandibular disorder (TMD) is a general term for a group of diseases involving temporomandibular joints (TMJs), masticatory muscles, and the surrounding tissues [1, 2]. TMD is the second most common musculoskeletal disorder that causes pain and disability [3, 4]. According to the Diagnostic Criteria for TMD (DC/TMD) Axis I, TMD could be divided into Group I: muscle disorders (including myofascial pain with and without mouth opening limitation); Group II: including disc displacement with or without reduction and mouth opening limitation; Group III: arthralgia, arthritis, and arthrosis [5]. TMD is often accompanied by the following symptoms: pain, decrease in the mouth opening, muscle or joint tenderness on palpation, limitation of mandibular movements, joint sounds, and otologic complaints like tinnitus, vertigo, or ear fullness, etc.
The treatment of atherogenic TMD usually includes non-surgical and surgical treatment. Non-surgical management options include non-steroidal anti-inflammatory drugs (NSAIDs), occlusal appliances, physical therapy, laser therapy, and some minimally invasive procedures such as intra-articular injections of hyaluronic acid (HA), corticosteroids, blood-derived products, and joint lavage through arthrocentesis [6,7,8,9]. Conservative treatment is now considered a first-choice therapy for TMD because of its low risk of side effects. In the case of severe acute pain or chronic pain resulting from serious disorders, inflammation, and/or degeneration pharmacotherapy, and minimally invasive/invasive procedures should be considered [10].
Internal derangement of the TMJ (TMJ ID) is considered the most common cause of TMD [11] and affects up to 80% of TMD patients. TMJ ID is attributed to an abnormal interaction of the articular disc, condyle, and joint eminence and may include a deformation, perforation, or displacement of the disc and/or posterior attachment of the disc [12]. Runci Anastasi et al. [13] believed that the disc-condyle complex is of great significance in TMD. Chantaracherd et al. [14] concluded that many people view IDs as a group of disorders that starts as disc displacement with reduction (DDWR), develops to disc displacement with reduction (DDWoR), and then to degenerative joint disease (DJD). Thus, the diagnosis of TMD requires not only sufficient clinical examination but also radiographic imaging examination.
Different radiographic imaging techniques have been proposed for evaluating the TMJ, such as computed tomography cone beam (CBCT), magnetic resonance imaging (MRI), TMJ arthrography, and panoramic radiography. TMJ intra-articular status was usually assessed by MRI and CBCT, although they have their shortcomings in enabling the clinician to effectively visualize the TMJ structures. At present, many studies are based on MRI or CBCT imaging data to evaluate its correlation with clinical symptoms [15,16,17,18]. However, these conclusions are not comprehensive enough.
MRI is the gold standard imaging method for evaluating the abnormalities of soft tissue in the TMJ, and masticatory muscles, and for determining the disc-condyle relationship [19]. MRI is usually used to evaluate the disc shape and disc position, joint effusion, the condylar bone marrow signal, and pannus formation [20]. MRI can also detect degenerative joint disease and condylar bone abnormalities, but could not efficiently detect the severity of the abnormalities [21]. There is currently a lack of large sample-size studies on the relationship between MRI and TMD clinical symptoms.
An important advantage of CBCT imaging of the TMJ is that it allows accurate measurements of the volume and the surface osseous changes, such as erosion, flatting, osteophytes, hypoplasia, sclerosis, and subchondral cyst with higher sensitivity, especially the early changes [22]. Additionally, it can be used to accurately assess the relative position of the condyle within the fossa. However, the morphology and position of the articular disc cannot be evaluated by CBCT. This means that CBCT alone cannot be used to evaluate the disc-condyle complex, but it is an important method to assist in the diagnosis of TMD. Based on the above-mentioned facts, this study aimed to compare the CBCT and MRI imaging features in the TMJs with and without TMD symptoms and to provide a reference for clinical diagnosis and treatment.
Methods
Ethical approval and study population
This study was endorsed by the Ethics committee of the Affiliated Stomatology Hospital of Guangzhou Medical University (LCYJ2022014). Informed consent to participate was obtained from all the participants and legally authorized representatives of minors age patients (< 16 Yrs). The selected participants were recruited from the patients referred for TMJ examination at the TMJ Diagnosis and Treatment Center of the Affiliated Stomatology Hospital of Guangzhou Medical University from March 2022 to September 2022. The CBCT was done for various reasons: evaluation of TMJ, impacted third molars, impacted teeth, implant site, pre-orthodontic assessment, or other reasons required CBCT. The MRI was done for the evaluation of the TMJ region. In the participants included in this retrospective study, both CBCT and MRI were taken before treatment and the time interval between the two scans was < 1 month.
Inclusion and exclusion criteria
All participants received clinical examination according to Diagnostic Criteria for TMDs (DC/TMD) [5]. MRI and CBCT imaging data were obtained before treatment. Inclusion criteria were as follows: (1) both MRI and CBCT imaging performed within < 1-month intervals before TMD treatment; (2) sufficient valid clinical data exist for statistical analysis; (3) agree to participate in the study. Exclusion criteria were as follows: (1) tumor or fracture in TMJ area; (2) maxillofacial trauma, TMJ surgery, orthodontics treatment, rheumatism, or rheumatoid disease history; (3) severe morphological abnormalities of the condyle; (4) simply masticatory muscle problems; (5) restricted mouth opening due to interstitial infection and mucosal fibrosis; (6) severe psychological disorders; (7) poor quality scanning images; (8) contraindications to MRI or CBCT images; (9) disagree to participate in the study.
Clinical examination
All participants were subjected to a standard clinical examination according to DC/TMD Axis I. Joint click, pain, and limited mouth opening were recorded. TMJ with at least one symptom is considered to be a symptomatic joint.
Joint sounds
Joint sounds were recorded by palpation on the TMJ region. Patients were asked to open their mouths as wide as possible and to do lateral, backward, and forward motions slowly 3 times respectively. Clicking, popping, or crepitation was recorded.
Pain
Pain intensity on a visual analog scale (VAS) was recorded. The VAS ranges from 0 to 10, where 0 indicates no pain and 10 indicates the worst pain.
Maximal interincisal opening (MIO)
The distance between the upper and lower incisors was measured when the patient opens his mouth. The limited mouth opening was defined as MIO < 42 mm.
CBCT imaging
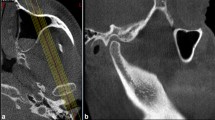
CBCT images were used to evaluate the condylar morphology and condylar position. Patients wear protective clothing when filming CBCT (Carestream CS9300, USA). Image reconstruction conditions were as follows: (1) the vertical fault was 60 mm in width and 0.3 mm in thickness; (2) the thickness of the deformed and coronal layer is 0.5 mm. The TMJ region in the oblique sagittal position was evaluated.
Condylar morphology
Condyles were divided into normal and abnormal in this study. Normal condyles have continuous cortical bone, while abnormal condyles are mainly divided into surface erosion, osteophyte, subcortical cyst, and generalized sclerosis [23]. The different condyle morphology was scored: 0 points represented normal condyle; 1 point represented the four abnormal types respectively; the cumulative value of abnormal types represented the degree of bone abnormality.
Condylar position
Anterior joint space (AJS), superior joint space (SJS), and posterior joint space (PJS) in the oblique sagittal position were recorded by the same doctor as shown in Fig. 1A. The average of the three measurements was used for comparison. The condylar position within the glenoid fossa was classified according to the value of the condylar ratio, which was assessed on the basis of the formula presented by Pullinger and Hollende [24]. Condylar ratio = (P−A)/(P + A) × 100% (Fig. 1B). The explanation is as follows: (1) − 12% ≤ ConRat ≤ 12% indicates concentric position; (2) ConRat > 12% indicates anterior position; (3) ConRat < -12% indicates posterior position.
MRI
MRI of bilateral TMJs with closed and open mouth position was obtained by a 1.5 T MRI scanner (UNITED IMAGING uMR, China). MRI images based on oblique sagittal adiposity-suppressed T2W1 were used to evaluate the disc morphology, disc position, and joint effusion.
Disc morphology
The normal disc is biconcave, which has narrowed intermediate zone and fully visible posterior and anterior bands. In this study, the disc morphology was divided into the following four types according to the degree of folding as shown in Fig. 2: biconcave, lengthened, contracture, and irregular [25].
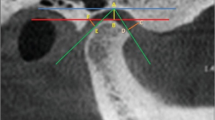
Disc position
Disc position was evaluated at the closed-mouth position and the reduction of disc displacement was evaluated at the open-mouth position. The normal disc position is the posterior band located directly superior to the condylar head in the closed-mouth position [26]. Three types of disc position were evaluated: (1) − 15°–15° indicates the normal position; (2) > 15° indicates anterior disc displacement (ADD); (3) < -15° indicates posterior disc displacement (PDD) [27]. According to the reduction of disc position, disc position can be divided into the following five types (Fig. 3): (1) normal (NA); (2) anterior disc displacement with reduction (ADDWR); (3) anterior disc displacement without reduction (ADDWoR); (4) posterior disc displacement with reduction (PDDWR); (5) posterior disc displacement without reduction (PDDWoR)[28].
Disc position. A–E MRI images in the open-mouth position, F–J MRI images in the open-mouth position. Where: NA: normal; ADDWR: anterior disc displacement with reduction; ADDWoR: anterior disc displacement without reduction. PDDWR: posterior disc displacement with reduction; PDDWoR: posterior disc displacement without reduction
Joint effusion
There are three types of joint effusion included in this study (Fig. 4): (1) 0 point represented no joint effusion; (2) 1 point represented slight joint effusion: spot-like or linear high signal shadow; (3) 2 points represented massive effusion: high signal shadow of effusion pool is visible.
Establishment of binary logistic regression model
The absence and presence of symptoms of TMJ were taken as dependent variables, and the Logistic regression values were 0 and 1, respectively. The following imaging features were used as independent variables to establish a Logistic model (including criteria P < 0.05 and excluding criteria P > 0.1). The forward method was used for stepwise regression. Criteria for assigning values: sex (male = 0 and female = 1); condylar morphology (normal = 0 and abnormal = 1); condylar position (anterior = 0, concentric = 0 and posterior = 1); disc morphology (normal = 0 and abnormal = 1); condylar position (biconcave = 0 and lengthened = 0, contracture = 0 and irregular = 1) and joint effusion (normal = 0, slight = 0, and massive = 1).
Data analysis
Eligible data were analyzed by SPSS Statistics 23.0 software. The mean age and joint spaces were described by mean ± standard deviation. Independent-sample T test was performed for the comparison of mean age, AJS, SPS, and PJS between the symptomatic and asymptomatic TMJs. Continuous variables of three groups were analyzed by one-way ANOVA. Chi-Square test was performed for the distribution of sex, age, condylar morphology, condylar position, disc morphology, disc position, and joint effusion. Pearson Chi-Square test was performed for the expected frequency of less than 5. The correlations between the study variables were assessed using the Spearman correlation coefficient. Single-factor binary logistic regression and multiple logistic regression analysis were conducted between the asymptomatic and symptomatic TMJs. The receiver operating curve (ROC) was used to assess the predicting accuracy of this model. Furthermore, the area under the curve (AUC) was evaluated. P < 0.05 was considered statistically significant.
Results
Basic information
A total of 357 participants (286 females and 71 males) with 714 TMJs were included in the study and divided into three groups: symptoms on one side (54.9%, 196/357), symptoms on both sides (23.0%, 82/357), and no symptoms on both sides (22.1%, 79/357), with the mean age of 27.27 ± 11.50, 26.38 ± 11.44, and 22.94 ± 9.51 years, respectively (P = 0.014) (Table 1). There were significant differences in the distribution of sex and age in different symptom sides (χ2 = 13.105, P = 0.001 and χ2 = 11.583, P = 0.021). In the No symptoms on both sides group, the 19–30-year-age-group ranked first followed by ≤ 18 and > 30-year-age groups. In Symptoms on one side and Symptoms on both sides groups, the 19–30-year-age group ranked first followed by > 30 and ≤ 18-year-age groups. The mean age of patients with symptoms on one side was significantly higher than that of patients with no symptoms and symptoms on both sides (F = 4.338 and P = 0.014).
Secondly, as shown in Table 2, all the 714 TMJs included in the study were divided into two groups according to the presence or absence of clinical symptoms: asymptomatic (n = 354, 25.34 ± 10.85 years) and symptomatic (n = 360, 26.88 ± 11.50 years) (P = 0.066). There were significant differences in AJS and SPS between asymptomatic and symptomatic groups, but no significant differences in PJS (P = 0.741). The value of AJS in the asymptomatic group was significantly lower than that in the symptomatic group (P = 0.000). The value of SJS in the asymptomatic group was significantly higher than that in the symptomatic group (P = 0.038).
Comparison of demographic/disease features with symptomatic and asymptomatic groups
The distribution and the indirect relation of demographic/disease features with the occurrence of symptoms were performed by Pearson Chi-Square test and Spearman correlation coefficient respectively, as shown in Table 3. There were significant differences in the distribution of sex (χ2 = 8.554, P = 0.000), age (χ2 = 8.084, P = 0.018), condylar morphology (χ2 = 64.693, P = 0.000), condylar position (χ2 = 14.681, P = 0.001), disc morphology (χ2 = 65.170, P = 0.000), disc position (χ2 = 83.642, P = 0.000) and joint effusion (χ2 = 53.911, P = 0.000) in symptomatic and asymptomatic TMJs, and showed positively correlated with symptoms (P < 0.05). The proportion of women in the symptomatic group was higher than that in the asymptomatic group, and sex was positively correlated with symptoms (r = 0.109, P = 0.003). In the asymptomatic group, the 19–30-year-age group ranked first followed by ≤ 18 and > 30-year-age groups. In the symptomatic group, the 19–30-year-age group ranked first followed by > 30 and ≤ 18-year-age groups. And age was positively correlated with symptoms (r = 0.075 and P = 0.044).
Zero ranked first followed by 1, 2, 3, and 4 in both the asymptomatic and symptomatic group, and condylar morphology was positively correlated with symptoms (r = 0.281, P = 0.000). The proportion of normal condyle in the asymptomatic group was significantly higher than that in the symptomatic group. In the asymptomatic group, concentric ranked first followed by posterior and anterior. In the symptomatic group, the posterior ranked first followed by concentric and anterior. And the condylar position was positively correlated with symptoms (r = 0.130 and P = 0.001).
In the asymptomatic group, biconcave ranked first followed by contracture, irregular, and lengthened. In the symptomatic group, contracture ranked first followed by irregular, biconcave, and lengthened. And disc morphology was positively correlated with symptoms (r = 0.279 and P = 0.000). In the asymptomatic group, NA ranked first followed by ADDWoR, ADDWR, PDDWR, and PDDWoR. In the symptomatic group, ADDWoR ranked first followed by ADDWR, NA, PDDWR, and PDDWoR. And disc position was positively correlated with symptoms (r = 0.300 and P = 0.000). Zero ranked first followed by 1 and 2 in both the asymptomatic and symptomatic groups, and joint effusion was positively correlated with symptoms (r = 0.273, P = 0.000).
Risk factors for TMD symptoms
Firstly, a single-factor binary logistic regression analysis was conducted between the asymptomatic and symptomatic groups. There was no significant difference in condylar positions, lengthened disc morphology, DDWR, or joint effusion between the two groups (P > 0.05). There were significant differences in sex, 19–30 years, > 30 years, condylar morphology, contracture disc morphology, irregular disc morphology, and DDWoR between the two groups (P < 0.05, Table 4).
Then, sex, age, condylar morphology, condylar position, disc morphology, and disc position were included in the multifactor analysis according to clinical knowledge. In multiple logistic regression, the six factors were found to be statistically significant: 19–30 years [P = 0.001, OR = 1.952, CI (95%) = (1.296–2.939)], > 30 years [P = 0.017, OR = 1.814, CI (95%) = (1.113–2.954)], abnormal condylar morphology [P = 0.000, OR = 2.360, CI (95%) = (1.613–3.453)], posterior condylar position [P = 0.000, OR = 2.591, CI (95%) = (1.578–4.253)], DDWR [P = 0.000, OR = 2.764, CI (95%) = (1.737–4.397)], and DDWoR [P = 0.000, OR = 4.189, CI (95%) = (2.693–6.515)].
Hence, the odds of having symptomatic TMJ were 1.952 higher in the 19–30-year-age group and 1.814 higher in the > 30-year-age group when compared to the ≤ 18-year-age group. The odds of having symptomatic TMJ were 2.360 higher in persons with abnormal condylar morphology when compared to those with normal condylar morphology. The odds of having symptomatic TMJ were 2.591 higher in persons with posterior condylar position when compared to those with the normal condylar position. The odds of having symptomatic TMJ were 2.764 higher in persons with DDWR and 4.189 higher in persons with DDWoR when compared to those with normal disc positions.
ROC curve analysis of the model
The ROC was used to assess the predicting accuracy of this model as shown in Fig. 5. The area under the curve (AUC) was evaluated. The AUCs of the model were 0.736 ± 0.019 (95% CI 0.700–0.773, P = 0.000), which indicated that the model has a good fitting effect and can be used to predict the occurrence of TMJ symptoms.
Discussion
This study was conducted to compare the CBCT and MRI imaging features in the TMJs with and without TMD symptoms. A total of 357 participants with 714 TMJs were included in the study. There were significant differences in the distribution of sex, age, condylar morphology, condylar position, disc morphology, disc position, and joint effusion in symptomatic and asymptomatic TMJs, and these features were positively correlated with TMD symptoms. In multiple logistic regression, the 19–30-year-age group, > 30-year-age group, abnormal condylar morphology, posterior condylar position, DDWR, and DDWoR were found to be statistically significant.
Patients with TMD symptoms are diagnosed over a broad age range, but a peak occurs between 20 and 40 year-age [29]. There was no statistically significant difference in mean age between the asymptomatic and symptomatic groups, possibly because patients in the unilateral asymptomatic group overlapped in both groups. In this study, the odds of having symptomatic TMJ were 1.952 higher in the 19–30-year-age group and 1.814 higher in the > 30-year-age group when compared to the ≤ 18-year-age group.
Although there was a poor correlation between condylar changes (as observed on CBCT images), pain, and symptoms in TMJ OA [30]. Many studies have confirmed the correlation between condylar bone changes and articular disc displacement and believed that it is related to TMD symptoms [31, 32]. Consistent with previous research results, normal condylar morphology was 75.1% in the asymptomatic group and 48.9% in the symptomatic group in this study. The odds of having symptomatic TMJ were 2.360 higher in persons with abnormal condylar morphology when compared to those with normal condylar morphology.
The relationship between condylar location and TMD symptoms is controversial. Shokri et al. observed that the posterior condylar position is more common in TMD patients [33]. And Yasa et al. found that the presence of TMD is associated with the condylar position in the TMJ [34]. However, Ma et al. [35] compared the condylar position in symptomatic and asymptomatic participants with and without chewing side preference and found that the condylar position is not a strong indicator. Paknahad et al. found the condylar position is associated with different severity of TMD [36]. However, the sample sizes of both studies were small. In this study, there were significant differences in AJS and SPS between asymptomatic and symptomatic groups, but no significant differences in PJS. The posterior condyle was the most common in the symptomatic group, while the concentric condyle was the most common in the asymptomatic group. The odds of having symptomatic TMJ were 2.591 higher in persons with posterior condylar position when compared to those with the normal condylar position.
Disc changes can be seen in up to 80% of TMD patients, but 30% of asymptomatic cases have similar findings [37]. Articular disc morphology was divided into 4 types: biconcave, lengthened, contracture, and irregular. The biconcave disc was the most common in the asymptomatic group, while the contracture disc was the most common in the symptomatic group. But the disc morphology did not seem to be the risk factor for TMD symptoms. Disc displacement on MRI correlated well with the presence or absence of clinical signs and symptoms of TMD [18, 38, 39]. The study found that the disc position was positively correlated with symptoms. The odds of having symptomatic TMJ were 2.764 higher in persons with DDWR and 4.189 higher in persons with DDWoR when compared to persons with normal disc position.
Joint effusion is the state of accumulation of joint fluid in the joint spaces and surrounding tissue [40]. Our present study found that there was a significant difference in the distribution of joint effusion in different types of disc morphology [25]. In this study, the proportion of participants without joint effusion in asymptomatic and symptomatic groups was 93.5% and 73.3%, respectively. Consistent with the results of Khawaja’s study [41], joint effusion is not a risk factor for TMD symptoms.
Conclusions
Unilateral symptoms of TMJs are more common in TMD. The imaging findings of TMJs were significantly different between symptomatic and asymptomatic TMJs. TMD is affected by multiple factors including > 19-year-age, abnormal condylar morphology, posterior condylar position, DDWR, and DDWoR, which could be risk factors for the development of TMD symptoms. Further studies are needed to confirm the end point of TMD treatment.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to ethical concerns but are available from the corresponding author on reasonable request.
Abbreviations
- TMD:
-
Temporomandibular disorder
- TMJ:
-
Temporomandibular joint
- NA:
-
Normal
- ADD:
-
Anterior disc displacement
- PDD:
-
Posterior disc displacement
- ADDWR:
-
Anterior disc displacement with reduction
- ADDWoR:
-
Anterior disc displacement without reduction
- CBCT:
-
Cone beam computed tomography
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating curve
- AUC:
-
Area under the curve
- T2WI:
-
T2-weighted image
- VAS:
-
Visual analog scale
- MIO:
-
Maximal interincisal opening
References
Chen J, Ning R, Lu Y. Effects of occlusal splint and exercise therapy, respectively, for the painful temporomandibular disorder in patients seeking for orthodontic treatment: a retrospective study. BMC Oral Health. 2022;22(1):527.
Pigozzi LB, Pereira DD, Pattussi MP, et al. Quality of life in young and middle age adult temporomandibular disorders patients and asymptomatic subjects: a systematic review and meta-analysis. Health Qual Life Outcomes. 2021;19(1):83.
Valesan LF, Da-Cas CD, Réus JC, et al. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig. 2021;25(2):441–53.
Jin LJ, Lamster IB, Greenspan JS, et al. Global burden of oral diseases: emerging concepts, management and interplay with systemic health. Oral Dis. 2016;22(7):609–19.
Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network* and orofacial pain special interest groupdagger. J Oral Facial Pain Headache. 2014;28(1):6–27.
Kalladka M, Quek S, Heir G, et al. Temporomandibular joint osteoarthritis: diagnosis and long-term conservative management: a topic review. J Indian Prosthodont Soc. 2014;14(1):6–15.
Ferrillo M, Nucci L, Giudice A, et al. Efficacy of conservative approaches on pain relief in patients with temporomandibular joint disorders: a systematic review with network meta-analysis. Cranio. 2022. https://doi.org/10.1080/08869634.2022.2126079.
Li W, Wu J. Treatment of temporomandibular joint disorders by ultrashort wave and extracorporeal shock wave: a comparative study. Med Sci Monit. 2020;26: e923461.
Maia ML, Bonjardim LR, Quintans Jde S, et al. Effect of low-level laser therapy on pain levels in patients with temporomandibular disorders: a systematic review. J Appl Oral Sci. 2012;20(6):594–602.
Wieckiewicz M, Boening K, Wiland P, et al. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J Headache Pain. 2015;16:106.
Paesani D, Westesson PL, Hatala M, et al. Prevalence of temporomandibular joint internal derangement in patients with craniomandibular disorders. Am J Orthod Dentofacial Orthop. 1992;101:41–7.
Laskin DM, Greene CS, Hylander WL. Temporomandibular disorders: an evidence-based approach to diagnosis and treatment. Berlin: Quintessence Publishing Company; 2006.
Runci Anastasi M, Cascone P, Anastasi GP, et al. Articular disc of a human temporomandibular joint: evaluation through light microscopy, immunofluorescence and scanning electron microscopy. J Funct Morphol Kinesiol. 2021;6(1):22.
Chantaracherd P, John MT, Hodges JS, et al. Temporomandibular joint disorders’ impact on pain, function, and disability. J Dent Res. 2015;94(3 Suppl):79S-86S.
Al-Saleh MA, Alsufyani NA, Saltaji H, et al. MRI and CBCT image registration of temporomandibular joint: a systematic review. J Otolaryngol Head Neck Surg. 2016;45(1):30.
Fischer J, Augdal TA, Angenete O, et al. In children and adolescents with temporomandibular disorder assembled with juvenile idiopathic arthritis-no association were found between pain and TMJ deformities using CBCT. BMC Oral Health. 2021;21(1):518.
Sener S, Akgunlu F. Correlation between the condyle position and intra-extraarticular clinical findings of temporomandibular dysfunction. Eur J Dent. 2011;5(3):354–60.
Kumar R, Pallagatti S, Sheikh S, et al. Correlation between clinical findings of temporomandibular disorders and MRI characteristics of disc displacement. Open Dent J. 2015;9:273–81.
Lee YH, Lee KM, Auh QS. MRI-based assessment of masticatory muscle changes in TMD patients after whiplash injury. J Clin Med. 2021;10(7):1404.
Wang YH, Ma RH, Li JJ, et al. Diagnostic efficacy of CBCT, MRI and CBCT-MRI fused images in determining anterior disc displacement and bone changes of temporomandibular joint. Dentomaxillofac Radiol. 2022;51(2):20210286.
Liu SS, Xu LL, Lu SJ, et al. Diagnostic performance of magnetic resonance imaging for degenerative temporomandibular joint disease. J Oral Rehabil. 2023;50(1):24–30.
Cömert Kiliç S, Kiliç N, Sümbüllü MA. Temporomandibular joint osteoarthritis: cone beam computed tomography findings, clinical features, and correlations. Int J Oral Maxillofac Surg. 2015;44(10):1268–74.
Al-Ekrish AA, Al-Juhani HO, Alhaidari RI, et al. Comparative study of the prevalence of temporomandibular joint osteoarthritic changes in cone beam computed tomograms of patients with or without temporomandibular disorder. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:78–85.
Derwich M, Pawlowska E. Do the mandibular condyles change their positions within glenoid fossae after occlusal splint therapy combined with physiotherapy in patients diagnosed with temporomandibular joint disorders? A prospective case control study. J Pers Med. 2022;12:254.
Li C, Zhang Q. Comparison of magnetic resonance imaging findings in 880 temporomandibular disorder patients of different age groups: a retrospective study. BMC Oral Health. 2022;22(1):651. https://doi.org/10.1186/s12903-022-02666-5.
Koh KJ, Park HN, Kim KA. Relationship between anterior disc displacement with/without reduction and effusion in temporomandibular disorder patients using magnetic resonance imaging. Imaging Sci Dent. 2013;43(4):245–51.
Jung YW, Park SH, On SW, et al. Correlation between clinical symptoms and magnetic resonance imaging findings in patients with temporomandibular joint internal derangement. J Korean Assoc Oral Maxillofac Surg. 2015;41(3):125–32.
Jeon KJ, Kim YH, Ha EG, et al. Quantitative analysis of the mouth opening movement of temporomandibular joint disorder patients according to disc position using computer vision: a pilot study. Quant Imaging Med Surg. 2022;12:1909–18.
Wadhwa S, Kapila S. TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ. 2008;72(8):930–47.
Palconet G, Ludlow JB, Tyndall DA, et al. Correlating cone beam CT results with temporomandibular joint pain of osteoarthritic origin. Dentomaxillofac Radiol. 2012;41(2):126–30.
Nawawi AP, Rikmasari R, Kurnikasari E, et al. Volumetric analysis of normal condyles and those with disc displacement with reduction in the Indonesian population: a CBCT study. Imaging Sci Dent. 2022;52(1):103–8.
Al-Hadad SA, ALyafrusee ES, Abdulqader AA, et al. Comprehensive three-dimensional positional and morphological assessment of the temporomandibular joint in skeletal Class II patients with mandibular retrognathism in different vertical skeletal patterns. BMC Oral Health. 2022;22(1):149.
Shokri A, Zarch HH, Hafezmaleki F, et al. Comparative assessment of condylar position in patients with temporomandibular disorder (TMD) and asymptomatic patients using cone-beam computed tomography. Dent Med Probl. 2019;56(1):81–7.
Yasa Y, Akgül HM. Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol. 2018;34(1):31–9.
Ma J, Wang J, Huang D, et al. A comparative study of condyle position in temporomandibular disorder patients with chewing side preference using cone-beam computed tomography. J Oral Rehabil. 2022;49(2):265–71.
Paknahad M, Shahidi S. Association between mandibular condylar position and clinical dysfunction index. J Craniomaxillofac Surg. 2015;43(4):432–6.
Tegnander T, Chladek G, Hovland A, et al. Relationship between clinical symptoms and magnetic resonance imaging in temporomandibular disorder (TMD) patients utilizing the Piper MRI diagnostic system. J Clin Med. 2021;10(20):4698.
Yang Z, Wang M, Ma Y, et al. Magnetic resonance imaging (MRI) evaluation for anterior disc displacement of the temporomandibular joint. Med Sci Monit. 2017;23:712–8.
Zhao X, Xiong X, Sun W, et al. Symptoms, disc position, occluding pairs, and facial skeletal characteristics of older patients with temporomandibular disorders. J Int Med Res. 2021;49(2):300060521990530.
Koh KJ, Park HN, Kim KA. Relationship between anterior disc displacement with/without reduction and effusion in temporomandibular disorder patients using magnetic resonance imaging. Imaging Sci Dent. 2013;43(4):245–51.
Khawaja SN, Crow H, Mahmoud RF, et al. Is there an association between temporomandibular joint effusion and arthralgia? J Oral Maxillofac Surg. 2017;75(2):268–75.
Acknowledgements
We are thankful to the staff and faculty of the Affiliated Stomatology Hospital of Guangzhou Medical University.
Funding
This study was supported by the Traditional Chinese Medicine Scientific Research Project of Guangdong Province (20232113) and the Natural Science Foundation of Guangdong Province (2214050005058).
Author information
Authors and Affiliations
Contributions
CL collected and analyzed the data and wrote the main manuscript text. QZ participated in the experimental design. Both authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the Research Ethics committee of the Affiliated Stomatology Hospital of Guangzhou Medical University (LCYJ2022014). All methods were carried out in accordance with relevant guidelines and regulations. All participants provided written informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, C., Zhang, Q. Comparison of imaging findings of 714 symptomatic and asymptomatic temporomandibular joints: a retrospective study. BMC Oral Health 23, 79 (2023). https://doi.org/10.1186/s12903-023-02783-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-02783-9