Abstract
Background
Poor oral health is a chronic condition that can be extremely costly to manage. In Australia, publicly funded dental services are provided to community members deemed to be eligible—those who are socio-economically disadvantaged or determined to be at higher risk of dental disease. Historically public dental services have nominally been allocated based on the size of the eligible population in a geographic area. This approach has been largely inadequate for reducing disparities in dental disease, primarily because the approach is treatment-focused, and oral health is influenced by a variety of interacting factors. This paper describes the developmental process of a multi-dimensional community-level risk assessment model, to profile a community’s risk of poor oral health.
Methods
A search of the evidence base was conducted to identify robust frameworks for conceptualisation of risk factors and associated performance indicators. Government and other agency websites were also searched to identify publicly available data assets with items relevant to oral diseases. Data quality and analysis considerations were assessed for the use of mixed data sources.
Results
Several frameworks and associated indicator sets (twelve national and eight state-wide data collections with relevant indicators) were identified. Determination of the system inputs for the Model were primarily informed by the World Health Organisation’s (WHO) operational model for an Integrated Oral Health-Chronic Disease Prevention System, and Australia’s National Oral Health Plan 2004–2013. Data quality and access informed the final selection of indicators.
Conclusions
Despite limitations in the quality and regularity of data collections, there are numerous data sources available that provide the required data inputs for community-level risk assessment for oral health. Assessing risk in this way will enhance our ability to deliver appropriate public oral health care services and address the uneven distribution of oral disease across the social gradient.
Similar content being viewed by others
Background
In Australia, publicly funded dental services are provided free or at little cost only to community members who are socio-economically disadvantaged, or at higher risk of developing dental disease for other reasons. The historical approach of allocating public dental services nominally on the size of the eligible population in a geographic region has been largely inadequate for reducing disparities in dental disease. Further, the approach has generally focused on treatment needs rather than the causes of oral diseases, with the role of public dental services in disease prevention remaining under-developed. Oral health should also not be considered in isolation however, and to reduce the social gradient in the prevalence of dental disease, the underlying causes of ill health more broadly also need to be considered.
Whitehead identifies that health is influenced by individual lifestyle factors; social and community networks; living and working conditions; and socio-economic, cultural and environmental conditions [1]. The causes of social inequality in health are considered to be multiple and inter-related, which therefore requires that actions to address the issue must be interconnected across the different levels of influence. Further, the socio-ecological framework proposed by McLeroy et al. [2] identifies that numerous systems and contexts shape human development [3, 4]. As such, the outcomes of both whole system, and more focussed interventions will depend upon factors operating at multiple levels. Points of intervention exist at the policy, community, organisational, interpersonal and intrapersonal levels [5].
There has been some conceptualisation of the social determinants of oral health, and the factors that operate and interact at multiple levels to influence oral health [6]. However, there has been little translation of the conceptual frameworks into a tangible mechanism to drive decision-making in public dental services. The question remains as to how public oral health services, and the broader public oral health care system, should be re-oriented to reduce inequities in oral health using an evidence-based, public health approach.
The aim of this paper is to describe the developmental process for a community-level risk assessment model for oral health to inform the service-delivery approach of Dental Health Services Victoria (DHSV) into the future.
Methods
Stakeholder consultation
DHSV is the leading public oral health care provider in Victoria, which is the second most populous state in Australia. In 2013–14, through the Royal Dental Hospital of Melbourne and over 90 community dental clinics, DHSV provided public oral health services to 411,217 Victorians. However, to enhance the service provided, reduce health inequities, and ensure future activities are appropriately oriented, an evidence-informed, public health approach to planning is to be utilised.
Within DHSV, consultation with a broad range of stakeholders identified that although risk assessment for oral disease is routinely performed at an individual-level in the dental clinic, to develop a state-wide service and public oral health care system, it is necessary to develop a method of assessing risk of oral disease at a community-level. Such a community risk assessment model would need to acknowledge the multiple factors influencing oral health, as well as the broader social determinants of health. To operate at a service and system-level, the model would also need to be updateable with new data as it becomes available, allow ongoing monitoring and surveillance, have capacity to examine geographical variation in oral health needs, and have utility to inform the optimal allocation of public oral health care services across Victoria.
This project aims to use the best research available to develop a multi-dimensional, community-level risk model which predicts the oral health needs in a given community. The profile would then identify which aspects of the oral health care system should be improved. An overview of the entire process to be undertaken is provided in Fig. 1; this paper reports on the first two steps in the process.
Identification of guiding theoretical frameworks
An important aspect of the developmental stage was to identify a robust and evidence-based theoretical framework to guide the selection of appropriate indicators and data sources. A comprehensive literature review of published frameworks for risk factors of oral health for children and adults and associated indicators was conducted. The Ovid Medline bibliographic database was searched for relevant articles using the following terms and their combinations: ‘frameworks’, ‘indicators’, ‘oral health survey’, ‘oral health monitoring’, ‘epidemiological data’, ‘modelling’, ‘dental need’, and ‘population data’. Health Department and other government websites were also searched for documents relating to oral or dental health monitoring.
Identification of available data sources
The following sources were examined to identify existing Australian data collections for use in the statistical modelling: websites of offices of national statistics; national and state-wide population health surveys (interview and examination); longitudinal cohort studies, and surveillance networks.
There was a particular focus on identifying data sources with participants comparable to (or comprising) the Victorian population and where data was collected as part of health surveys, or as part of clinical or administrative data collections. Oral health examination and interview surveys restricted solely to population groups with special needs were excluded from further consideration.
Selection of indicators and assessment of data quality
The selection of the indicator set was guided by consistency with underpinning theoretical frameworks, current oral health policy priorities, and scientific validity, reliability and relevance. The Australian Bureau of Statistics (ABS) report ‘Measuring Wellbeing: Frameworks for Australian Social Statistics 2001’ [7] underlines these basic measurement and analysis issues associated with available data sources in Australia. Inclusion of an indicator in the risk model was also determined after assessing the basic data quality dimensions of: methodological soundness, accessibility, accuracy and reliability [8, 9], as described below.
Methodological soundness
The methodological basis for the statistics follows internationally accepted standards, guidelines, or good practices.
-
Concepts and definitions used are in accord with internationally-accepted statistical frameworks.
-
The scope is in accordance with internationally accepted standards, guidelines, or good practices
Accessibility
Data and metadata are easily available and assistance to users is adequate
-
Statistics are presented in a clear and understandable manner, forms of dissemination are adequate, and statistics are made available on an impartial basis.
-
Up-to-date and pertinent metadata are made available.
Accuracy and reliability
Source data and statistical techniques are sound and statistical outputs sufficiently portray reality.
-
Source data available provide an adequate basis to compile statistics
-
Statistical techniques employed conform to sound statistical procedures
Ethics and consent
As no data was collected for this study no ethics approval or participant consent was sought.
Results
Identification of frameworks
Several multi-level frameworks were identified through the searching. The most relevant for this project were: Australia’s National Oral Health Plan 2004–2013 [10], The Socio-Ecological Model of Health [2], Fisher-Owens Model of Child Oral Health [11], WHO model for Oral Health Diseases Surveillance and WHO operational model for an integrated oral health-chronic disease surveillance system [9] and the Framework of Socioeconomic Determinants of Health [12]. The system inputs for our community-level risk assessment model were developed primarily around the WHO frameworks [9, 13, 14] and Australia’s National Oral Health Plan 2004–2013 [10]. The framework encompasses two ‘Tiers’, covering Determinants and Risk factors, and Outcomes. Each tier has a number of domains, each defining a distinct aspect of the tier. The Determinants and Risk factors tier has six domains that bring together a range of factors that affect oral health at individual and population levels: Policy, Health Systems, Sociocultural, Environmental, Behaviours, and Use of Services. The Outcomes tier has two domains that summarise the impact of oral health conditions on individuals: Disease and Quality of Life. The framework is depicted in Fig. 2.
The Australia’s National Oral Health Plan 2004–2013 [10] encompasses nineteen process and outcomes indicators for Oral Health under the key domains of the WHO framework [10], which address the main dental diseases: dental caries, periodontal diseases, and oral cancer.
Identification of data sources
Identified national and state-wide sources with items relevant to oral health status and outcomes indicators, diseases and related risk factors were of two main categories: statistical sources (including surveys and censuses); and administrative sources (including population registries and hospital databases).
A wide range of administrative systems and statistical data collections were compiled by the Australian Institute of Health and Welfare (AIHW) from data supplied by states and territories. Other national sources were: the Australian Bureau of Statistics (ABS), the Department of Human Services (DHS), the Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA), and the Australian Institute of Family Studies (AIFS).
Majority of identified state-wide data collections were sourced from the Department of Health and Human Services (DHHS) and Dental Health Services Victoria (DHSV) Other sources were the Cancer Council Victoria (CCV) and the Victorian Department of Education and Training (DET).
The complete list of data sources is summarised in Table 1.
Data quality assessment
Table 1 summarises the detailed quality assessment of each of the identified data collections. The majority of the surveys provided incidental information on self-reported outcomes, subject to recall and reporting bias. In contrast, national and Victorian population registries and hospital data are collected routinely, based on medical diagnosis, with large samples, thus the information is generally more reliable. However, their capacity to identify differences in disease profile and service utilisation of population subgroups is restricted, due to limited demographics.
National surveys conducted by the Australian Institute of Health and Welfare (AIHW) and Dental Statistics Research Unit (DSRU) used random sampling design and collected incidental information, with the only exception being the National Dental Telephone Interview Survey (NDTIS) repeated every two and a half years. In contrast, data from state-wide surveys are regularly available. Sampling weights were applied in all surveys. In relation to the Census data, several strategies are employed by the ABS to produce high quality data by minimising respondent errors (choosing suitable content, question and form design), processing errors (repairs, coding errors, and validation), partial response and undercount.
Data collections and indicators by framework domain
When searching for data sources with items relevant to oral health, and within the domains of the underpinning frameworks, twelve national and eight state-wide data collections were identified.
Oral health status and outcomes indicators were identified in a variety of national data collections including: i) population based surveys: the National Survey of Adult Oral Health (NSAOH) [15], the National Dental Telephone Interview Survey (NDTIS) [16] the Child Dental Health Survey (CDHS) [17], and Child Oral Health Study (COHS) 2002–2004 [17]; ii) administrative systems : the Australian Cancer Database (ACD) [18].
Indicators covering the risk factors and determinants domains were identified in the following national collections: Census of Population and Housing survey [19], Health Care Card data [20], National Health Workforce Data Set (NHWDS) [21],National Hospital Morbidity Database(NHMD) [22],Longitudinal Survey of Dentists’ Practice Activity (LSDPA) [23], National Dental Labour Force Data Collection (NLFDC) [24],and Longitudinal Study of Australian Children (LSAC) [25].
The main state-wide hospital database with oral health status, outcomes, and risk factors items was Titanium [26], a patient record system for Victorian public dental agencies. Data collections with behavioural risk factors were primarily population surveys including theVictorian Population Health Survey (VPHS) [27], the Victorian Child Health and Wellbeing Survey (VCHWS) [28], and the School Entrant Health Questionnaire (SEHQ) [29]. The complete list of identified data collections and indicators is summarised in Table 1.
A total of forty-eight evidence-based indicators of interest were selected across all domains. Majority of determinants and risk factors indicators were within the domains of: i) use of services: dental attendance, reason for attendance, dental general anesthetics (DGA), early detection, preventive care, emergency care and recall period for children; and ii) systems and services: financing care, access to services, waiting time, and organisational practices. Selected oral health conditions and quality of life indicators for measuring outcomes were: caries severity and prevalence, untreated tooth decay, fissure sealants, functional and non-functional dentition, periodontal disease severity, oral cancer mucosal lesions, experience of pain, and psychosocial and functional impacts of oral illness. The list of all selected indicators of interest against the framework domains is summarised in Table 2.
A selection of twenty indicators to be included in the model is shown in Table 3, along with the associated data sources. All except for two (caries experience and functional dentition) were determinants and risk factors.
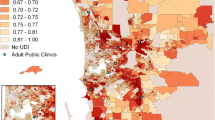
The selection was based on: alignment with the theoretical model, data/item availability and currency, suitability (similarity) of sample population, potential for use in a mixed data-source statistical model. The number of variables from each dataset that have been incorporated into the model varies. Available data is collected at the levels of Local Government Area (LGA), postcode, community dental agency and census collection district (CCD) levels, and where necessary will be disaggregated or aggregated and used at suburb/postcode level to minimise averaging errors. Most recent available datasets for each data collection will be sourced and used.
Discussion
Identification of communities at high risk of developing dental disease across multiple dimensions enables the appropriate allocation of public dental services and resources, as a first step to reducing oral health inequalities across the population. In the current study, we have identified a guiding framework and multiple data sources to develop a risk assessment model to enable re-orientation of public oral health care services. We have also catalogued available oral health-related data sources to provide a resource for public oral health researchers, policy makers and service providers.
An appropriately directed public oral health service must be able to regularly monitor the costs and clinical effectiveness of the interventions provided, as well as population disease and health inequalities. This requires a shift in the focus and reporting systems from an emphasis on outputs to outcomes. It also requires quality data collections and robust indicator sets. Our research identified numerous sources with items relevant to oral status and outcomes indicators, diseases and related risk factors. These sources were of two main categories: statistical sources, including surveys and censuses, and administrative sources, such as population registries and hospital databases.
The majority of the survey data collected provided incidental information on self-reported outcomes, and were subject to recall and reporting bias. In contrast, population registries and hospital data are based on medical diagnosis thus the information is generally more reliable; however, their capacity to identify differences in disease profile or service utilisation by population subgroups is restricted, due to only limited demographic data being collected. Further, these data collections only include members of the population who utilise such services, and generally do not include individuals who use alternative, privately run services. However, the data sources identified were generally stand-alone and not articulated in with other data collections or monitoring systems. Exploring options for integration of datasets in real time is important to enable more integrated health services to be delivered. Further, improving the data system, so that data linkage at an individual level can occur, will enhance future use of existing data assets, providing a quantum leap in our ability to explore causal pathways and long-term impacts through prospective, longitudinal data sets which are also large and representative. This need, and the potential of this powerful approach for improving oral health, has been recognised by others [30].
Despite the limitations with the data collections, it is clear that there is a wealth of existing survey and routinely collected data that can be better utilised to inform decisions in relation to oral health policy, programs and service delivery. Importantly, we have identified that the available data is not solely located within the health sector which highlights the need for collaborations and partnerships that are cross-sectoral. In this research we have also moved beyond analysing individual items or indicators in data sets, and have identified a robust framework that provides a guiding structure for assembling the available data in a coherent and useful way. This enables us to paint a picture of the risk factors for poor oral health that are operating in the population at a given point in time. Importantly, it is also apparent from this study that no single data collection contains all the necessary information for an integrated oral health-chronic disease surveillance system, as recommended by WHO [9]. Many of the difficulties of using data from multiple and varied sources have previously been identified [31, 32], however the focus has been largely on the appropriate statistical methods to use to provide robust results. There has been little discussion of the practicalities of sourcing, assessing, cleaning, and harmonising data collected at multiple levels such as the individual, family, community and area, although the importance of this for public health has been identified [33].
Data collection is a resource-intensive exercise, and in the absence of a routine oral health monitoring or surveillance system in Australia, a community risk assessment model presents the opportunity to explore patterns and clusters of multiple risk factors in the population based on geographic area. The Model will also enable the examination of multi-dimensional impacts of past and future strategies, interventions and policies on populations, services and systems. This information can then inform health service planning and the approaches to addressing common risk factors and preventing chronic diseases. In the context of limited resources for research and evaluation, having a mechanism to examine population impacts of innovative public health strategies is critical.
Limitations
This study is limited to the information available at the time of searching. This relates to searching for both frameworks and available datasets. Not all of the data required in the framework could be sourced. It is possible that additional sources are now available. The ability to use the identified data sources in the statistical modelling has not been tested in this phase of the study, which is a further limitation, although this will be the focus of the next stage of the project. We were also unable to find directly comparable studies with which to compare our findings.
Next steps
The project will continue to progress through the remaining stages shown in Fig. 1. This involves harmonising and combining data sources that were initially collected for different purposes, in different geographical areas, from different subpopulations and/or at different times. Statistical models that have utilised mixed data sources will be scrutinised to inform the best methods to use in the community-level risk assessment model for oral health. Initially the data will be used to investigate the statistical relationship between risk factors and oral health outcomes, to confirm the predictive value of the selected indicators. After exploring and describing the relationships between indicators and outcomes the statistical models of community-level risk will be developed, appropriately including a selection of the indicators of risk. The model deliberately contains both risk and protective factors, as these factors occur concurrently at the community level. This next stage of the project will determine the relative importance of the different influences and provide important, policy-relevant findings. The oral health risk model will be developed for all geographic areas in Victoria and will be used by DHSV to guide resource allocation for public dental services. Routinely collected clinical data will also be monitored to evaluate the effect of utilising a population health planning model for public oral health services on disparities in oral disease across the population.
Conclusions
The community-level risk assessment model is being developed as a response to a need to transform the approach to reducing disparities in oral health, and re-orient the allocation of public oral health services in contemporary Australia. Given our growing knowledge of the multi-dimensional influences of oral health, and our ability to prevent or arrest the disease with appropriate strategies, there is a clear need to move from a traditional approach to a more meaningful, responsive and effective model for providing public oral health services.
Abbreviations
- ABS:
-
Australian bureau of statistics
- ACD:
-
Australian cancer database
- AIFS:
-
Australian institute of family studies
- AIHW:
-
Australian institute of health and welfare
- CCV:
-
cancer council victoria
- CDHS:
-
child dental health survey
- COHS:
-
child oral health study
- DET:
-
department of education and training
- DHHS:
-
department of health and human services
- DHS:
-
Australian government department of human services
- DHSV:
-
dental health services victoria
- DSRU:
-
dental statistics and research unit, aihw
- FaHCSIA:
-
department of families, housing, community services and indigenous affairs
- LSDPA:
-
longitudinal survey of dentists’ practice activity
- LSAC:
-
longitudinal study of australian children
- NRASL:
-
national registration and accreditation scheme
- NDTIS:
-
national dental telephone interview survey
- NLFDC:
-
national dental labour force data collections
- NHWDS:
-
national health workforce data set
- NHMD:
-
national hospital morbidity database
- NHWDS:
-
national health workforce data set
- NSAOH:
-
national survey of adult oral health
- SEIFA:
-
socio-economic index for areas (index of disadvantage)
- SEHQ:
-
school entrant health questionnaire
- VAED:
-
victorian admitted episodes dataset
- VCR:
-
victorian cancer registry
- VCHWS:
-
victorian child health and wellbeing survey
- VPHS:
-
victorian population health survey
References
Whitehead M. A typology of actions to tackle social inequalities in health. Journal Epidemiology and Comminity Health. 2007;61:473–8.
McLeroy KR et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
Bronfenbrenner U. The Ecology of Human Development. London: Harvard University Press; 1979.
Bronfenbrenner U. Ecology of the familiy as a context for human development: Research perspectives. Dev Psychol. 1986;22(6):723–42.
Moore SN, Murphy S, Moore L. Health improvement, nutritional behaviour and the role of school meals: the usefulness of a socio-ecological perspective to inform policy design, implementation and evaluation. Critical Public Health. 2011;21(4):441–54.
Petersen PE. The World Oral Health Report 2003. Continuous improvement of oral health in the 21st century - the approach of the WHO Global Oral Health Programme. Available at http://www.who.int/oral_health/media/en/orh_report03_en.pdf.
Australian Bureau of Statistics. Measuring Wellbeing: Frameworks for Australian Social Statistics. 2001 31 July 2006 [cited 2015 24 April 2015]; Available from: http://www.abs.gov.au/ausstats/abs@.nsf/0/44AD1E3F6E6F27A2CA25713F0014E6DA?opendocument.
International Monetary Fund. Data Quality Assessment Framework. 2006.
Petersen PE et al. Oral health information systems-towards measuring progress in oral health promotion and disease prevention. Bulletin World Health Organisation. 2005;9(83):686–93.
National Advisory Committee on Oral Health. Australia’s National Oral Health Plan. 2004.
Fisher-Owens SA et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120(3):510–20.
Turrell G et al. Socioeconomic determinants of health: towards a national research program and a policy and intervention agenda. Canberra: Queensland University of Technology; 1999.
Wilkinson R, Marmot M. Social Determinants of Health. The solid facts. Denmark: World Health Organisation; 2003.
World Health Organisation. Social Determinants 2015 [cited 2011 28 November 2011]; Available from: http://www.euro.who.int/en/health-topics/health-determinants/social-determinants/social-determinants.
AIHW Dental Statistics and Research Unit (2007) Australia’s dental generations: the National Survey of Adult Oral health 2004–06. 292
Australian Institute of Health and Welfare. Dental and Oral Health Publications 2015 [cited 2014 14 October 2014]; Available from: http://www.aihw.gov.au/dental-and-oral-health-publications/.
Armfield, J.M. and A.J. Spencer. Dental health behaviours among children 2002–2004: the use of fluoride toothpaste, fluoride tablets and drops, and fluoride mouthrinse 2012 [cited 2014 15 October 2014]; Available from: http://www.aihw.gov.au/publication-detail/?id=10737421052
Australian Institute of Health and Welfare. Australian Cancer Database (ACD) 2015 [cited 2014 14 October 2014]; Available from: http://www.aihw.gov.au/australian-cancer-database/.
Australian Bureau of Statistics. Census. 2015 11 March 2015 [cited 2014 20 October 2014]; Available from: http://www.abs.gov.au/census
Australian Government Department of Human Services. Data.gov.au. 2014.
Australian Institute of Health and Welfare. National Health Workforce Data Set. 2014 [cited 2014 14 October 2014]; Available from: http://www.aihw.gov.au.
Australian Institute of Health and Welfare. National Hospital Morbidity Database (NHMD). 2015 [cited 2014 14 October 2014]; Available from: http://www.aihw.gov.au/hospitals-data/national-hospital-morbidity-database/.
Australian Institute of Health and Welfare. Age and the costs of dental care in Research Report Series. Australia: Australian Institute of Health and Welfare Canberra; 2010.
Chrisopoulos, S. and T. Nguyen. Trends in the Australian Dental labour Force, 2000 to 2009: dental labour force collection, 2009. 2012 [cited 2014 15 October 2014]; Available from: http://www.aihw.gov.au/publication-detail/?id=10737421917.
Australian Institute of Family Studies. Longitudinal Study of Australian Children (LSAC) 2010 [cited 2014 20 October 2014]; Available from: http://www.aifs.gov.au/institute/media/mediabackgrounders/lsac.html..
Dental Health Services Victoria. Titanium Database 2014 [cited 2014 14 October 2014]; Available from: https://www.dhsv.org.au
Victorian Department of Health and Human Services. Victorian Population Health Survey (VPHS). 2014 [cited 2014 20 October 2014]; Available from: http://docs.health.vic.gov.au/docs/doc/Victorian-population-health-survey-2014-–-information-brochure
Victorian Department of Education and Training. Victorian Child Health and Wellbeing Survey (VCHWS) 2014 [cited 2014 14 October 2014]; Available from: http://www.education.vic.gov.au/about/research/pages/newdata.aspx.
Victorian Department of Education and Training. School Entrant Health Questionnaire (SEHQ). 2014 [cited 2014 14 October 2014]; Available from: http://www.education.vic.gov.au/about/research/pages/reportdatahealth.aspx.
Slack-Smith L. How population-level data linkage might impact on dental research. Community Dentistry Oral Epidemiology. 2012;40:90–4.
De Angelis D et al. Four key challenges in infectious disease modelling using data from multiple sources. Epidemics. 2015;10:83–7.
Samsa G, Hu G, Root M. Combining Information From Multiple Data Sources to Create Multivariable Risk Models: Illustration and Preliminary Assessment of a New Method. Journal Biomedicine and Biotechnology. 2005;2005(2):113–23.
Murray CJL, Lopez AD. Measuring the Global Burden of Disease. New England Journal Medicine. 2013;369(5):448–57.
Cancer Council Victoria. Victorian Cancer Registry 2014 22 December 2014 [cited 2014 21 October 2014]; Available from: http://www.cancervic.org.au/research/registry-statistics/vcr.
Cancer Council Victoria and Dental Health Services Victoria. Oral Health Policy Data 2014 [cited 2014 15 October 2014]; Available from: https://www.dhsv.org.au.
Heilbrunn-Lang AY et al. Reviewing public policy for promoting population oral health in Victoria, Australia (2007–12). 2015. Australian Health Review.
Dental Health Services Victoria. Workforce Dataset. 2014 [cited 2014 16 October 2014]; Available from: https://www.dhsv.org.au.
Dental Health Services Victoria. Smiles 4 Miles. 2014 [cited 2014 17 October 2014]; Available from: https://www.dhsv.org.au/oral-health-programs/smiles4miles.
Dental Health Services Victoria. Victorian Census Collection Districts 2014 [cited 2014 20 October 2014]; Available from: https://www.dhsv.org.au/
Victorian Department of Health and Human Services. Victorian Admitted Episodes Dataset (VAED). 2014 [cited 2014 15 October 2014]; Available from: http://www.health.vic.gov.au/hdss/vaed.
Victorian Department of Health and Human Services. Water Fluoridation Program. Available from: https://www2.health.vic.gov.au/public-health/water/water-fluoridation.
Acknowledgments
Thank you to Rhydwyn McGuire and Martin Whelan for assistance with data sourcing and data management. We also acknowledge the contributions of Jacqueline Martin-Kerry, Holly Brown and Michelle Chatelier for assistance with formatting the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AdeS conceptualised the study and oversaw the project and prepared draft versions of the paper. PG was involved in developing the design of the study, developing the methods, locating and reviewing data sources, performing the quality assessment, and writing the manuscript. LC was involved in the method development, locating and reviewing data sources, and drafting the manuscript. DC provided input into the design of the study, had significant input into interpretation of the findings and assisted with writing of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
de Silva, A.M., Gkolia, P., Carpenter, L. et al. Developing a model to assess community-level risk of oral diseases for planning public dental services in Australia. BMC Oral Health 16, 45 (2016). https://doi.org/10.1186/s12903-016-0200-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-016-0200-5