Abstract
Background
Glucocorticoids and sclerostin act as inhibitors of the Wnt signaling pathway, thereby hindering bone formation. Given the pathway's intricate association with mesenchymal stem cells, the hypothesis suggests that heightened sclerostin levels may be intricately linked to an augmentation in marrow adiposity induced by glucocorticoids. This study endeavored to delve into the nuanced relationship between circulating sclerostin and bone marrow adipose tissue in postmenopausal women grappling with glucocorticoid-induced osteoporosis (GIO).
Methods
In this cross-sectional study, 103 patients with autoimmune-associated diseases underwent glucocorticoid treatment, boasting an average age of 61.3 years (standard deviation 7.1 years). The investigation encompassed a thorough assessment, incorporating medical history, anthropometric data, biochemical analysis, and dual-energy X-ray absorptiometry measurements of lumbar and femoral bone mineral density (BMD). Osteoporosis criteria were established at a T-score of -2.5 or lower. Additionally, MR spectroscopy quantified the vertebral marrow fat fraction.
Results
BMD at the femoral neck, total hip, and lumbar spine showcased an inverse correlation with marrow fat fraction (r = –0.511 to – 0.647, P < 0.001). Serum sclerostin levels exhibited a positive correlation with BMD at various skeletal sites (r = 0.476 to 0.589, P < 0.001). A noteworthy correlation emerged between circulating sclerostin and marrow fat fraction at the lumbar spine (r = –0.731, 95% CI, –0.810 to –0.627, P < 0.001). Multivariate analysis brought to light that vertebral marrow fat fraction significantly contributed to sclerostin serum concentrations (standardized regression coefficient ß = 0.462, P < 0.001). Even after adjusting for age, body mass index, physical activity, renal function, BMD, and the duration and doses of glucocorticoid treatment, serum sclerostin levels maintained a significant correlation with marrow fat fraction.
Conclusions
Circulating sclerostin levels exhibited a noteworthy association with marrow adiposity in postmenopausal women grappling with GIO.
Similar content being viewed by others
Introduction
Sclerostin, derived from osteocytes, navigates through canalicular networks to reach bone surfaces. Upon reaching these surfaces, sclerostin impedes the canonical Wnt-beta-catenin pathway, thereby reducing osteoblastogenesis and accelerating osteoclastogenesis [1,2,3]. In 2019, the European Medicines Agency approved romosozumab, an anti-sclerostin antibody, for osteoporosis treatment [4].
The regulatory influence of the Wnt pathway intricately shapes the differentiation process of bone marrow mesenchymal stem cells (BMSCs) [5]. Glucocorticoids promote the differentiation of BMSCs towards adipocytes rather than osteoblasts, and both endogenous and exogenous glucocorticoids may induce the accumulation of bone marrow adipose tissue (BMAT) [6, 7]. Central to the pathogenesis of glucocorticoid-induced osteoporosis (GIO) is the suppression of bone formation. One of the key mechanisms by which glucocorticoids diminish the production of osteoblasts is through the antagonism of the Wnt/β-catenin signaling pathway [8]. Additionally, sclerostin acts as a Wnt signaling inhibitor, obstructing osteogenic differentiation and impeding the acquisition of bone mass [3, 8, 9]. Fascinatingly, treatments with sclerostin-neutralizing antibodies demonstrated the ability to reduce overall marrow adiposity in both a time-dependent and dose-dependent fashion [5]. Furthermore, a discernible negative correlation was observed between the areas of bone and BMAT [10]. This suggests that elevated sclerostin levels may be associated with increased bone marrow adiposity induced by glucocorticoids.
Currently, our comprehension of the intricate relationships involving skeletal integrity, marrow fat, body compositions, and the impact of circulating sclerostin on these dynamics is notably limited, further complicated by conflicting findings reported in the existing literature [1, 5, 11,12,13]. Sclerostin levels rise in the serum of mice subjected to both synthetic glucocorticoid treatment and exposure to endogenous glucocorticoids. However, the regulation of its expression in bone tissue or murine BMSCs treated with glucocorticoids remains ambiguous. In contrast, sclerostin levels decrease in human BMSCs when stimulated with glucocorticoids and in patients with rheumatoid arthritis and polymyalgia rheumatica who necessitate glucocorticoid therapy [14]. Interestingly, other reports have demonstrated elevated serum levels of sclerostin in patients undergoing glucocorticoid therapy [15]. Furthermore, no association was found between circulating sclerostin levels and bone marrow adiposity in postmenopausal women with osteoarthritis [1]. However, comprehensive data on circulating sclerostin levels, particularly its correlation with marrow adiposity in postmenopausal women with GIO, is limited.
The primary aim of this study was to explore the potential association between circulating sclerostin levels and BMAT assessed by MR spectroscopy in postmenopausal women with GIO.
Methods
Ethics approval and informed consent
The research protocol underwent a comprehensive review and obtained approval from the Institutional Review Board at Zhoupu Hospital, affiliated with Shanghai University of Medicine & Health Sciences. Before participating in the study, all participants provided written informed consent.
Study population
We undertook a cross-sectional investigation that involved consecutive postmenopausal females undergoing chronic glucocorticoid treatment, defined as a daily dose of ≥ 5 mg of prednisone or its equivalent for a duration exceeding 3 months [16]. Patients enrolled in this study were referred to our unit between January 2018 and December 2023, with a primary emphasis on assessing bone metabolism. At the study's onset, each participant underwent a comprehensive clinical visit and a thorough laboratory evaluation. Major exclusion criteria included: (1) the use of anti-osteoporotic drugs at any point, including bisphosphonates, hormone replacement therapy, parathyroid hormone, selective estrogen receptor modulators, etc.; (2) a diagnosis of metabolic bone disease unrelated to GIO; (3) chronic kidney disease with calculated creatinine clearance < 30 mL/min; (4) contraindication for magnetic resonance imaging. Additionally, other conditions impeding study participation, such as mental illness, were considered as exclusion criteria. A total of 103 postmenopausal women who met the inclusion criteria were considered for the final analysis.
In the process of gathering our data, we systematically compiled a comprehensive array of clinical information. This encompassed a spectrum of demographic details, including age, gender, menopausal status, and individual health status. Our focus extended to a meticulous examination of medication history, with a particular emphasis on factors contributing to osteoporosis risk, such as glucocorticoid doses—including the daily current dose, duration, and cumulative dose in prednisone equivalent. We also delved into the use of additional immunosuppressant agents and explored diverse lifestyle factors. This encompassed intricate aspects like dietary habits, including dairy consumption, the usage of vitamins or calcium supplements, as well as behaviors like cigarette smoking and alcohol intake. Furthermore, anthropometric data, comprising height, weight, and body mass index (BMI) measured in kilograms per square meter, were meticulously recorded. Physical activity was precisely defined as active participation in exercise sessions occurring at least three times a week, each lasting a minimum of 30 min.
Laboratory analyses
Blood samples were meticulously collected between 8 and 9 a.m. following an overnight fast, a precautionary measure aimed at minimizing potential confounding factors and ensuring the precise assessment of bone health. Utilizing enzymatic methods (ADVIA Chemistry XPT; SIEMENS, German), we conducted a thorough analysis, encompassing the measurement of serum uric acid, creatinine, phosphorus, calcium, and the serum lipid profile, which included total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglyceride levels, as well as fasting blood glucose. The estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula (mL/min). For the evaluation of markers of bone turnover, serum was separated by centrifugation and kept at − 20 °C for the determination of parathyroid hormone, c-terminal telopeptide, total osteocalcin, intact N-terminal propeptide of type I collagen, 25-hydroxyvitamin D, sclerostin and osteocalcin using electrochemiluminescence assays (Cobas e601; Roche Diagnostics, Basel, Switzerland). Additionally, plasma glycated hemoglobin levels were determined with high-performance liquid chromatography (MQ-6000; Shanghai Medconn Biotechnology Co., Ltd., China).
Dual-energy X-ray absorptiometry
The assessment of areal bone mineral density (BMD, g/cm2) at the lumbar spine and proximal femur (femoral neck and total hip) is a pivotal marker for gauging bone health, a task commonly executed through dual-energy X-ray absorptiometry (DXA, GE Healthcare, WI, USA). Renowned for its precision and steadfastness in BMD measurements, this machine enjoys widespread adoption in the field. In order to safeguard the credibility of our DXA scans, our center strictly adheres to rigorous quality control protocols. A crucial determinant of reliability is the coefficient of variation. In our study, the coefficients of variation for total femur and lumbar spine BMD measurements was 1.40% and 1.18%, respectively, underscoring the robustness and precision of our assessments. Densitometric osteoporosis was defined according to the WHO criteria with T–score values ≤ –2.5 (in subjects > 50 years) or Z–score values < –2 (in subjects < 50 years) [16].
MR spectroscopy acquisition and quantification
We employed MR spectroscopy to precisely assess the fat content within the vertebral marrow. The MRI procedures were executed on a 3-T clinical system (MAGNETOM Skyra; Siemens Medical Systems, Erlangen, Germany). A surface coil was strategically placed as the radiofrequency receiver beneath the lumbar spine region, while the body volume coil served as the radiofrequency transmitter. Participants assumed a supine position within the scanner to ensure the accuracy of imaging. In order to cater to individual clinical needs, a standard clinical MRI of the lumbar spine was conducted. This thorough examination encompassed sagittal turbo-spin echo T1- and T2-weighted imaging, along with a transaxial T2-weighted fast spin echo sequence. Sagittal images of the lumbar spine were acquired to facilitate the precise positioning of the L3 vertebral body. Following this, a stimulated echo acquisition method (STEAM) sequence was implemented for MR spectroscopy to ascertain the percentage of bone marrow fat.
In the realm of lumbar MR spectroscopy, a precisely defined voxel measuring 1.5 cm × 1.5 cm × 1.5 cm was strategically positioned within the intricate confines of the L3 vertebral body. The volume of interest, meticulously centered in the middle of the vertebral body, maintained unwavering dimensions throughout the entirety of the study. A region-specific STEAM (stimulated echo acquisition mode) sequence was employed for MR spectroscopy. Water suppression was not implemented during the acquisition process. The sequence parameters were meticulously configured as follows: repetition time = 3000 ms, echo times) = 12, 24, 36, 48, and 72 ms, data points = 1028, and receiver bandwidth = 2000 Hz. Automated procedures were adeptly employed for gradient shimming and the fine-tuning of transmit and receive gain. At each echo time, the signal intensities of the distinct fat and water peaks were precisely measured through integration of their corresponding spectral regions. Following a meticulous consideration of T2 decay, accomplished by fitting an exponential function to the signal evolution across echo time, the precise determination of fat percentage unfolded with exactitude. This intricate calculation relied on the scrupulous measurement of signal intensities linked to both fat and water [17, 18], as impeccably illustrated in Supplementary Material Fig. 1.
Serum sclerostin levels according to degree of marrow fat fraction (MFF) given in quartiles. Trend analysis was performed for serum sclerostin levels to describe a linear component of the trend from quartile 1 (Q1) to quartile 4 (Q4) of the vertebral MFF adjusted for age, body mass index, physical activity, renal function, bone mineral density, and the duration and doses of glucocorticoids treatment. MFF quartiles: Q1 < 56.0% (n = 25); 56.0% ≤ Q2 < 60.5% (n = 26); 60.5% ≤ Q3 < 69.0% (n = 26); and 69.0% ≤ Q4 (n = 26). Error bars represent standard deviation values of the mean
Statistical analysis
The descriptive statistics included in the analysis were the mean ± standard deviation (SD), median values with interquartile ranges (IQ1-IQ3), counts, and frequencies. The Shapiro-Wilks test was performed to estimate the normal distribution of all outcomes. The association between variables was assessed using Pearson’s or Spearman’s rank test, as appropriate. Serum sclerostin levels were subjected to trend analysis to reveal the linear progression across quartile groups (Q1 to Q4), determined by the distribution of marrow fat fraction in quartiles. The impact of independent variables on serum sclerostin levels was evaluated through a multiple regression analysis using the ordinal least squares method. Models were adjusted for age, BMI, physical activity, renal function, BMD, and the duration and doses of glucocorticoids treatment as previous studies have reported associations with sclerostin levels [11, 19,20,21]. A p-value of < 0.05 was considered statistically significant. The statistical analysis was performed with SPSS version 25.0 (IBM Corp., SPSS Statistics, Armonk, NY, USA).
Results
Baseline characteristics
A total of 103 postmenopausal women met the inclusion criteria, with a mean age of 61.3 years (SD 7.1 years) spanning from 50 to 75 years, were undergoing chronic treatment with glucocorticoids. The median duration and doses of glucocorticoids treatment were calculated at 14.5 months (IQR: 8.3, 27.8 months) and 8 mg/day (IQR: 6, 10 mg/day), respectively. The primary autoimmune-associated diseases prevalent among the participants including rheumatoid arthritis (n = 70), polymyalgia rheumatica (n = 19), vasculitis (n = 4), systemic lupus erythematosus (n = 5), inflammatory myopathies (n = 3), and collagenosis (n = 2). For a comprehensive overview of the clinical characteristics of the patients, refer to Table 1.
Associations between serum sclerostin and parameters of interest
Table 2 delineates the correlations between serum sclerostin and key parameters. Positive correlations emerged between circulating sclerostin and BMD at the femoral neck, total hip, and lumbar spine in postmenopausal women with GIO. Additionally, BMD at the femoral neck, total hip, and lumbar spine exhibited an inverse correlation with marrow fat fraction. Noteworthy is the significant negative correlation identified between sclerostin serum concentrations and eGFR, as well as between marrow fat fraction and eGFR, suggesting higher serum sclerostin levels or elevated marrow adiposity in individuals with lower eGFR. No significant correlations were observed between age, markers of bone turnover, and circulating sclerostin or marrow fat fraction.
Associations between circulating sclerostin and marrow fat fraction
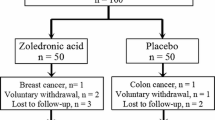
As depicted in Fig. 1, serum sclerostin levels exhibited a noteworthy decrease in higher vertebral PDFF quartiles compared to lower quartiles (P for trend < 0.05), with adjustments made for age, BMI, physical activity, renal function, BMD, and the duration and doses of glucocorticoids treatment. A significant correlation was identified between circulating sclerostin and marrow fat fraction at the lumbar spine (r = –0.731, 95% CI, –0.810 to –0.627, P < 0.001) (Fig. 2). Moreover, in the multiple regression analysis, vertebral marrow fat fraction significantly contributed to sclerostin serum concentrations (standardized regression coefficient ß = 0.462, P < 0.001), even after accounting for age, BMI, physical activity, renal function, BMD, and the duration and doses of glucocorticoids treatment.
Discussion
Sclerostin, a glycoprotein, plays a pivotal role in impeding the processes associated with bone formation and stands as a key factor in diminishing osteoblast function. Additionally, sclerostin upregulates the expression of proteolytic enzymes in osteoclasts [22]. Several studies have demonstrated a direct association between BMD and sclerostin concentration in both healthy humans and individuals with spinal cord injuries [23,24,25]. Consistent with the findings in patients with a fresh hip fracture [26] or hematological disorders undergoing 1-year glucocorticoid therapy (> 7.5 mg/day) [15], as well as in mice exposed to endogenous and exogenous glucocorticoids [14], we identified significant positive correlations between circulating sclerostin levels and BMD measurements in postmenopausal females with GIO. These studies suggest that sclerostin concentration might serve as a complementary or potentially alternative indicator to densitometric testing [2, 23, 24]. One suggested rationale for this positive association between sclerostin and BMD posits that circulating sclerostin levels are contingent upon the number and activity of osteocytes, theoretically correlating with the overall bone mass [26]. Elevated BMD might lead to an increased number of osteocytes, consequently resulting in higher levels of circulating sclerostin.
Nevertheless, Patalong-Wojcik and collaborators found no discernible disparity in sclerostin levels between groups with normal and diminished BMD. Moreover, there was an absence of correlation between sclerostin concentration and lumbar vertebrae BMD in young adult women [2]. The observed disparity could potentially be attributed to variations in population characteristics, including factors such as gender, menopausal status, and notably, the age range of the study cohort.
Descriptive studies involving both humans and animals have been conducted on serum sclerostin, with a primary focus on assessing skeletal integrity and bone marrow adipose tissue [1, 2, 5, 11, 13,14,15, 23,24,25,26,27,28,29,30,31,32,33]. The results are presented in Table 3. A few studies suggested that sclerostin may be associated with marrow adiposity [5, 11]. Ma et al. reported that vertebral marrow adiposity was greater in elderly men with higher serum sclerostin levels in models adjusted for age, BMI and diabetes, but not in women [11]. There were a few limitations to that study, such as the age of the population, which included only older white adults (mean age 79 years). Additionally, the factors used for adjustment were different from those used in our study and did not include eGFR, BMD, and the duration and doses of glucocorticoids treatment, which may have influenced the results. However, the complex interplay between the marrow adipose depot and osteocytes, along with osteocyte-derived molecules like sclerostin, remains largely unexplored. Fairfield and colleagues shed light on this relationship by demonstrating that sclerostin not only promotes adipocyte differentiation in pre-adipocyte cell lines but also in primary MSCs obtained from both mouse and human, exerting its effects at the expense of osteoblastogenesis. Reinforcing their findings with two in vivo models designed to inhibit sclerostin, the research unequivocally affirms that the induction of BMAT is orchestrated by sclerostin and is diminished in the absence of sclerostin, achieved through either knockout or neutralization using a specific antibody [5, 10].
However, others reported that no substantial correlations were found between circulating sclerostin and marrow proton density fat fraction in the lumbar spine, femoral neck, and femoral diaphysis in both postmenopausal women with fragility fractures and controls (postmenopausal women with osteoarthritis). This lack of correlation persisted both before and after accounting for factors such as age, eGFR, and BMD [1].
The correlation between vertebral marrow fat fraction in our study cohort and BMD values demonstrated an inverse relationship, consistent with previously published data highlighting the negative association between bone marrow adipocytes and BMD in GIO [6]. While numerous studies, particularly those conducted clinically and in vivo with rodents, have highlighted an augmentation in bone marrow adipose tissue in response to glucocorticoids [6, 34,35,36], it's crucial to note that this phenomenon is not universally observed. For instance, a study on outbred Swiss mice, exposed to short-term glucocorticoid excess at two different doses (2.8 and 5.4 mg/kg/d), revealed no significant impact on adipocyte volume density. This density was estimated by dividing the total number of points hitting adipocytes within the bone marrow by the total number of points hitting the bone marrow. Surprisingly, only the higher dose of glucocorticoids demonstrated a substantial increase (+ 48%) in adipocyte cross-sectional area compared to the placebo pellet [37]. The variations observed in these research findings could be attributed to a spectrum of factors, encompassing fluctuating glucocorticoid dosages, durations of drug intervention, the inclusion of diverse rodent species, the methodologies applied in measuring adipose tissue, and discrepancies in skeletal locations.
The primary discovery from our study reveals a negative association between sclerostin serum concentrations and marrow adiposity in postmenopausal females with GIO. In the literature, conflicting findings arise when investigating the regulation of sclerostin by glucocorticoids. Several previous studies have indicated that both the administration of synthetic glucocorticoids and exposure to endogenous glucocorticoids led to elevated systemic sclerostin levels in mice [14, 38]. Intriguingly, in animal models, skeletal sclerostin expression either witnessed an increase [39] or displayed no discernible difference [14, 40] following glucocorticoid treatment.
Differing from observations in animal studies, the regulation of sclerostin in the human system demonstrated increased consistency, marked by a reduction observed after glucocorticoid treatment in human bone marrow stromal cells. Additionally, patients undergoing glucocorticoid therapy for conditions such as rheumatoid arthritis, polymyalgia rheumatica and chronic inflammatory diseases exhibited a noteworthy decrease in sclerostin levels [14, 28, 29]. The regulation of sclerostin shows variations in individuals with hypercortisolism. One study documented reduced sclerostin levels in those with endogenous hypercortisolism compared to healthy controls [30], whereas another reported increased sclerostin levels [31, 41]. The contrasting results could be linked to differing methodologies, including variations in the timing of blood sample collection, the differentiation between non-fasting and fasting blood samples, discrepancies in study populations, or differences in the methods used to assess blood sclerostin levels.
Despite its strengths, our study has limitations, primarily associated with its cross-sectional nature and the absence of a designated control group. Examining the temporal correlation between circulating sclerostin and BMAT proved impractical. Additionally, our study focused solely on postmenopausal women aged 50 years and older, potentially constraining the applicability of our findings to younger women or men. Notable strengths, however, include the comprehensive assessment of marrow fat across all subjects in the study and the homogeneity of the patient group, as all individuals were undergoing chronic glucocorticoid treatment with a daily dose of ≥ 5 mg. These factors contribute to the robustness of our study.
In conclusion, we have established a correlation between circulating sclerostin levels and marrow adiposity in postmenopausal females with GIO. These findings imply that sclerostin may play significant roles in the pathogenesis of GIO.
Availability of data and materials
The datasets generated during and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
- BMAT:
-
Bone marrow adipose tissue
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- BMSCs:
-
Bone marrow mesenchymal stem cells
- eGFR:
-
Stimated glomerular filtration rate
- GIO:
-
Glucocorticoid-induced osteoporosis
References
Courtalin M, Bertheaume N, Badr S, During A, Lombardo D, Deken V, Cortet B, Clabaut A, Paccou J. Relationships between circulating sclerostin, bone marrow adiposity, other adipose deposits and lean mass in post-menopausal women. Int J Mol Sci. 2023;24(6):5922.
Patalong-Wojcik M, Golara A, Zajac K, Sokolowska A, Kozlowski M, Toloczko-Grabarek A, Krzyscin M, Brodowska A, Janiec A, Myszka A, et al. Influence of muscle mass and strength on bone mineralisation with consideration of sclerostin concentration. Biomedicines. 2023;11(6):1574.
Iolascon G, Liguori S, Paoletta M, Toro G, Moretti A. Anti-sclerostin antibodies: a new frontier in fragility fractures treatment. Ther Adv Musculoskelet Dis. 2023;15:1759720X231197094.
Poutoglidou F, Samoladas E, Raikos N, Kouvelas D. Efficacy and safety of anti-sclerostin antibodies in the treatment of osteoporosis: A meta-analysis and systematic review. J Clin Densitom. 2022;25(3):401–15.
Fairfield H, Falank C, Harris E, Demambro V, McDonald M, Pettitt JA, Mohanty ST, Croucher P, Kramer I, Kneissel M, et al. The skeletal cell-derived molecule sclerostin drives bone marrow adipogenesis. J Cell Physiol. 2018;233(2):1156–67.
Sorensen NN, Andreasen CM, Jensen PR, Hauge EM, Bollerslev J, Delaisse JM, Kassem M, Jafari A, Diaz-delCastillo M, Andersen TL. Disturbed bone marrow adiposity in patients with Cushing’s syndrome and glucocorticoid- and postmenopausal- induced osteoporosis. Front Endocrinol (Lausanne). 2023;14:1232574.
Pierce JL, Sharma AK, Roberts RL, Yu K, Irsik DL, Choudhary V, Dorn JS, Bensreti H, Benson RD Jr, Kaiser H, et al. The glucocorticoid receptor in osterix-expressing cells regulates bone mass, bone marrow adipose tissue, and systemic metabolism in female mice during aging. J Bone Miner Res. 2022;37(2):285–302.
Guanabens N, Gifre L, Peris P. The role of Wnt signaling and sclerostin in the pathogenesis of glucocorticoid-induced osteoporosis. Curr Osteoporos Rep. 2014;12(1):90–7.
Bhattacharyya S, Pal S, Chattopadhyay N. Targeted inhibition of sclerostin for post-menopausal osteoporosis therapy: a critical assessment of the mechanism of action. Eur J Pharmacol. 2018;826:39–47.
Costa S, Fairfield H, Reagan MR. Inverse correlation between trabecular bone volume and bone marrow adipose tissue in rats treated with osteoanabolic agents. Bone. 2019;123:211–23.
Ma YH, Schwartz AV, Sigurdsson S, Hue TF, Lang TF, Harris TB, Rosen CJ, Vittinghoff E, Eiriksdottir G, Hauksdottir AM, et al. Circulating sclerostin associated with vertebral bone marrow fat in older men but not women. J Clin Endocrinol Metab. 2014;99(12):E2584–2590.
Kim JA, Roh E, Hong SH, Lee YB, Kim NH, Yoo HJ, Seo JA, Kim NH, Kim SG, Baik SH, et al. Association of serum sclerostin levels with low skeletal muscle mass: The Korean Sarcopenic Obesity Study (KSOS). Bone. 2019;128: 115053.
Urano T, Shiraki M, Ouchi Y, Inoue S. Association of circulating sclerostin levels with fat mass and metabolic disease–related markers in Japanese postmenopausal women. J Clin Endocrinol Metab. 2012;97(8):E1473–1477.
Thiele S, Hannemann A, Winzer M, Baschant U, Weidner H, Nauck M, Thakker RV, Bornhauser M, Hofbauer LC, Rauner M. Regulation of sclerostin in glucocorticoid-induced osteoporosis (GIO) in mice and humans. Endocr Connect. 2019;8(7):923–34.
Gifre L, Ruiz-Gaspa S, Monegal A, Nomdedeu B, Filella X, Guanabens N, Peris P. Effect of glucocorticoid treatment on Wnt signalling antagonists (sclerostin and Dkk-1) and their relationship with bone turnover. Bone. 2013;57(1):272–6.
Florez H, Hernandez-Rodriguez J, Muxi A, Carrasco JL, Prieto-Gonzalez S, Cid MC, Espinosa G, Gomez-Puerta JA, Monegal A, Guanabens N, et al. Trabecular bone score improves fracture risk assessment in glucocorticoid-induced osteoporosis. Rheumatology (Oxford). 2020;59(7):1574–80.
Li S, Wang B, Liang W, Chen Q, Wang W, Mei J, Zhang H, Liu Q, Yuan M. Associations Between Vertebral Marrow Proton Density Fat Fraction and Risk of Prostate Cancer. Front Endocrinol (Lausanne). 2022;13:874904.
Li G, Xu Z, Lin H, Chen Y, Li X, Chang S. Association between insulin resistance and the magnetic resonance spectroscopy-determined marrow fat fraction in nondiabetic postmenopausal women. Menopause. 2018;25(6):676–82.
Janik M, Stuss M, Michalska-Kasiczak M, Jegier A, Sewerynek E. Effects of physical activity on sclerostin concentrations. Endokrynol Pol. 2018;69(2):142–9.
Mödder UI, Hoey KA, Amin S, McCready LK, Achenbach SJ, Riggs BL, Melton LJ 3rd, Khosla S. Relation of age, gender, and bone mass to circulating sclerostin levels in women and men. J Bone Miner Res. 2011;26(2):373–9.
Amrein K, Amrein S, Drexler C, Dimai HP, Dobnig H, Pfeifer K, Tomaschitz A, Pieber TR, Fahrleitner-Pammer A. Sclerostin and its association with physical activity, age, gender, body composition, and bone mineral content in healthy adults. J Clin Endocrinol Metab. 2012;97(1):148–54.
Li X, Ominsky MS, Villasenor KS, Niu QT, Asuncion FJ, Xia X, Grisanti M, Wronski TJ, Simonet WS, Ke HZ. Sclerostin antibody reverses bone loss by increasing bone formation and decreasing bone resorption in a rat model of male osteoporosis. Endocrinology. 2018;159(1):260–71.
Invernizzi M, Carda S, Rizzi M, Grana E, Squarzanti DF, Cisari C, Molinari C, Renò F. Evaluation of serum myostatin and sclerostin levels in chronic spinal cord injured patients. Spinal Cord. 2015;53(8):615–20.
Ardawi MS, Al-Kadi HA, Rouzi AA, Qari MH. Determinants of serum sclerostin in healthy pre- and postmenopausal women. J Bone Miner Res. 2011;26(12):2812–22.
Durosier C, van Lierop A, Ferrari S, Chevalley T, Papapoulos S, Rizzoli R. Association of circulating sclerostin with bone mineral mass, microstructure, and turnover biochemical markers in healthy elderly men and women. J Clin Endocrinol Metab. 2013;98(9):3873–83.
Wanby P, Nobin R, Von SP, Brudin L, Carlsson M. Serum levels of the bone turnover markers dickkopf-1, sclerostin, osteoprotegerin, osteopontin, osteocalcin and 25-hydroxyvitamin D in Swedish geriatric patients aged 75 years or older with a fresh hip fracture and in healthy controls. J Endocrinol Invest. 2016;39(8):855–63.
Wang YP, Khelifi N, Halleux C, Ung RV, Samson F, Gagnon C, Mac-Way F. Bone marrow adiposity, bone mineral density and wnt/beta-catenin pathway inhibitors levels in hemodialysis patients. J Bone Metab. 2022;29(2):113–22.
Kawazoe M, Kaneko K, Shikano K, Kusunoki N, Nanki T, Kawai S. Glucocorticoid therapy causes contradictory changes of serum Wnt signaling-related molecules in systemic autoimmune diseases. Clin Rheumatol. 2018;37(8):2169–78.
Braz NFT, Rocha NP, Vieira ÉLM, Gomez RS, Barbosa IG, Malheiro OB, Kakehasi AM, Teixeira AL. Negative impact of high cumulative glucocorticoid dose on bone metabolism of patients with myasthenia gravis. Neurol Sci. 2017;38(8):1405–13.
van Lierop AH, van der Eerden AW, Hamdy NA, Hermus AR, den Heijer M, Papapoulos SE. Circulating sclerostin levels are decreased in patients with endogenous hypercortisolism and increase after treatment. J Clin Endocrinol Metab. 2012;97(10):E1953–1957.
Belaya ZE, Rozhinskaya LY, Melnichenko GA, Solodovnikov AG, Dragunova NV, Iljin AV, Dzeranova LK, Dedov II. Serum extracellular secreted antagonists of the canonical Wnt/β-catenin signaling pathway in patients with Cushing’s syndrome. Osteoporos Int. 2013;24(8):2191–9.
Gaudio A, Pennisi P, Bratengeier C, Torrisi V, Lindner B, Mangiafico RA, Pulvirenti I, Hawa G, Tringali G, Fiore CE. Increased sclerostin serum levels associated with bone formation and resorption markers in patients with immobilization-induced bone loss. J Clin Endocrinol Metab. 2010;95(5):2248–53.
Sharma-Ghimire P, Buchanan S, Bemben MG, Knehans A, Campbell J, Bemben DA. Sclerostin and Dickkopf-1 characteristics according to age and physical activity levels in premenopausal women. J Clin Densitom. 2022;25(2):168–77.
Liu X, Gu Y, Kumar S, Amin S, Guo Q, Wang J, Fang CL, Cao X, Wan M. Oxylipin-PPARgamma-initiated adipocyte senescence propagates secondary senescence in the bone marrow. Cell Metab. 2023;35(4):667–84 e666.
Fan J, Zhang D, Jiang Y, Yu L, Han B, Qian Z. The effects of PPARγ inhibitor on bones and bone marrow fat in aged glucocorticoid-treated female rats. Exp Gerontol. 2023;181:112281.
Li GW, Xu Z, Chen QW, Chang SX, Tian YN, Fan JZ. The temporal characterization of marrow lipids and adipocytes in a rabbit model of glucocorticoid-induced osteoporosis. Skeletal Radiol. 2013;42(9):1235–44.
Brent MB, Brüel A, Thomsen JS. Sparse dose-dependent difference in skeletal effects of short-term glucocorticoid excess in outbred Swiss mice. Endoc Metab Sci. 2021;5:100114.
Beier EE, Sheu TJ, Resseguie EA, Takahata M, Awad HA, Cory-Slechta DA, Puzas JE. Sclerostin activity plays a key role in the negative effect of glucocorticoid signaling on osteoblast function in mice. Bone Res. 2017;5:17013.
Sato AY, Cregor M, Delgado-Calle J, Condon KW, Allen MR, Peacock M, Plotkin LI, Bellido T. Protection From Glucocorticoid-Induced Osteoporosis by Anti-Catabolic Signaling in the Absence of Sost/Sclerostin. J Bone Miner Res. 2016;31(10):1791–802.
Ren H, Liang D, Jiang X, Tang J, Cui J, Wei Q, Zhang S, Yao Z, Shen G, Lin S. Variance of spinal osteoporosis induced by dexamethasone and methylprednisolone and its associated mechanism. Steroids. 2015;102:65–75.
Belaya ZE, Grebennikova TA, Melnichenko GA, Nikitin AG, Solodovnikov AG, Brovkina OI, Grigoriev AU, Rozhinskaya LY, Dedov II. Effects of endogenous hypercortisolism on bone mRNA and microRNA expression in humans. Osteoporos Int. 2018;29(1):211–21.
Acknowledgements
Not applicable.
Funding
This work was supported by the funds for Training Project of Academic Leaders of Health System in Pudong New Area of Shanghai (NO. PWRd2021-07).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Shaojun Li obtained funding. Wei Li and Wei Wang completed experiments. Minlan Zhang collected the data. Qi Chen and Fengyi Li analyzed the data. The first draft of the manuscript was written by Wei Li and all authors commented on previous versions of the manuscript. Critical revisions were made by Shaojun Li. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol underwent a comprehensive review and obtained approval from the Institutional Review Board at Zhoupu Hospital, affiliated with Shanghai University of Medicine & Health Sciences. Before participating in the study, all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, W., Wang, W., Zhang, M. et al. Association of serum sclerostin levels with marrow adiposity in postmenopausal women with glucocorticoid-induced osteoporosis. BMC Endocr Disord 24, 55 (2024). https://doi.org/10.1186/s12902-024-01591-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-024-01591-8