Abstract
Background
Mamushi bites are the most common venomous snake bites in Japan, with known complications including rhabdomyolysis and acute kidney injury; however, adrenal insufficiency as a result of snake bites has not been previously reported. We report a case of empty sella with transient adrenal insufficiency during hospitalization for a Mamushi bite.
Case presentation
An 84-year-old man was admitted to our hospital with a Mamushi bite on the right fifth finger. Serum sodium (Na) level remained in the normal range. On the ninth day of admission, he developed hyponatremia, with a serum Na level of 114 mEq/L and serum cortisol level of 4.0 μg/dL (reference value 4.5–21.1 μg/dL). His serum Na level was restored within the normal range after administration of corticosteroids with 3% NaCl solution. Both rapid adrenocorticotrophin and corticotropin-releasing hormone loading tests showed low cortisol response. Based on the results of the hormone loading tests, a diagnosis of pituitary adrenal insufficiency was made. Contrast-enhanced pituitary magnetic resonance imaging (MRI) showed primary empty sella. After discontinuation of corticosteroids, the hyponatremia did not recur, and the patient was discharged on the 24th day of hospitalization. After discharge, the patient visited an outpatient clinic, but hyponatremia recurrence was not observed.
Conclusions
This is the first report of hyponatremia due to pituitary adrenal insufficiency during hospitalization for a Mamushi bite in a patient with empty sella. When hyponatremia occurs during hospitalization for a Mamushi bite, cortisol measurement, hormone loading test, and head MRI should be performed to search for pituitary lesions because of the possibility of adrenal insufficiency caused by snake venom.
Similar content being viewed by others
Background
Mamushi (Gloydius blomhoffii), the most common venomous snake in Japan, is found throughout Japan, except in Okinawa. Approximately 1000 cases of Mamushi bites are reported annually, with an estimated mortality rate of approximately 1% [1]. Known complications of Mamushi bites include acute kidney injury, hypovolemic shock, and rhabdomyolysis [2]. Although rare, fatal complications such as respiratory failure, gastrointestinal hemorrhage, and intestinal necrosis have also been reported [3].
To date, there have been no case reports of adrenal insufficiency following a Mamushi bite. Empty sella is defined as an enlarged subarachnoid space within the sella turcica [4] and is associated with various degrees of hormone deficiency [5]. In this report, we present a case of empty sella with transient adrenal insufficiency during hospitalization for a Mamushi bite.
Case presentation
Case
An 84-year-old Japanese man was bitten by a Mamushi on the right fifth finger and presented to our emergency department. He had a history of benign prostatic hyperplasia and an overactive bladder. He was taking mirabegron at a dosage of 50 mg/day and had an oxybutynin patch that delivered a dose of 73.5 mg/day. The patient was treated on surgical admission. On the second day of hospitalization, the bite reached Grade 4 (redness and swelling of the whole extremity) [6]. Creatine kinase (CK) level was maximal at 1770 U/L on the fourth day of admission. Cephalantin (10 mg/day), acetate ringer (1000 mL/day), and maintenance fluid (sodium 35 mEq/L, potassium 20 mEq/L, and glucose 4.3% isotonic solution [1000 mL/day]) had been administered since the second day of admission. The total in–out balance had roughly passed zero.
On the eighth day of hospitalization, vomiting occurred. In the early hours of the ninth day of hospitalization, the patient experienced restlessness, and blood tests revealed hyponatremia. The patient was transferred to the department of internal medicine.
Investigations
At the time of transfer to the department of internal medicine, the patient’s vital signs were as follows: consciousness level of 13 points (E3V4M6) on the Glasgow Coma Scale, blood pressure of 142/79 mmHg, pulse rate of 59 beats/min, respiratory rate of 24 breaths/min, SpO2 of 97% (room air), and body temperature of 37.2 °C in the axilla. Physical examination revealed no rigidity of the neck, no enlarged cervical lymph nodes, and clear respiratory sounds and no heart murmur on chest auscultation. The abdomen was flat and soft with no tenderness. No edema of the lower legs was observed, and tenderness, swelling, and heat were present from the right upper arm to the dorsum of the right hand. The findings in the right upper extremity remained unchanged from those on the previous day.
Table 1 shows the laboratory findings at the time of transfer to the department of internal medicine. Blood tests showed that the CK level was elevated again to 2267 U/L. The serum Na level was 114 mE/L, and serum osmolality was 237 mOsm/L. Urinalysis revealed a urine specific gravity of 1.020, urinary Na level of 195 mEq/L, and urine osmolality of 613 mOsm/L. Despite the hyponatremia, the urine was hypertonic.
Differential diagnosis
Figure 1 shows the clinical course of the patient after admission. We determined that the CK re-elevation was due to hyponatremia. Severe symptomatic hyponatremia was corrected with administration of 3% sodium chloride solution. On the 10th day of admission, the serum Na level improved to 120 mEq/L, and the level of consciousness improved as the serum Na level improved. Since the blood cortisol level was low at 4.0 µg/dL (reference value 4.5–21.11 µg/dL), adrenal insufficiency was suspected, and administration of corticosteroids (dexamethasone 6.6 mg/day, then hydrocortisone 100 mg/day) was initiated on the 10th day of admission. On the 11th day of admission, the 3% sodium chloride solution was discontinued, and on the 15th day of admission, the corticosteroids were discontinued; however, the serum Na level did not decrease. An adrenocorticotrophin hormone (ACTH) loading test was performed on the 16th day of admission. Pituitary contrast-enhanced magnetic resonance imaging (MRI) and a corticotropin-releasing hormone / growth hormone-releasing factor / thyrotropin-releasing hormone / luteinizing hormone-releasing hormone (CRH/GRF/TRH/LHRH) stimulation test was performed on the 19th and 23rd day of admission, respectively. The results of the ACTH loading test and CRH/GRF/TRH/LHRH stimulation test are shown in Table 2. The peak blood cortisol levels after the ACTH loading and CRH/GRF/TRH/LHRH stimulation tests were below 18 µg/dL, and the peak ACTH level after the CRH/GRF/TRH/LHRH stimulation test was less than two-folds the basal value; thus, a diagnosis of pituitary adrenal insufficiency was made [7].
Chart showing the patient’s clinical course. DEXA: dexamethasone 6.6 mg/day, HDC: hydrocortisone 100 mg/day, NaCl: sodium chloride, CK, creatine kinase, ACTH: adrenocorticotropic hormone, CRH: corticotropin-releasing hormone, GRF: growth hormone-releasing factor, TRH: thyrotropin-releasing hormone, LHRH: luteinizing hormone-releasing hormone
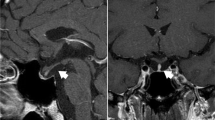
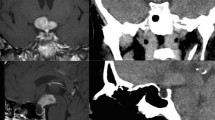
Contrast-enhanced MRI of the pituitary gland is shown in Fig. 2. The sella turcica was markedly enlarged and filled with cerebrospinal fluid.
Outcome and follow-up
After discontinuation of corticosteroids, the hyponatremia did not recur, and the swelling in the right upper extremity improved. The patient was discharged on the 24th day of admission. He visited the outpatient clinic 9 and 16 days after discharge, and there was no hyponatremia relapse. The patient has not experienced hyponatremia in the three years since the Mamushi bite.
Discussion and conclusions
This is the first report of a case of hyponatremia due to pituitary adrenal insufficiency after a Mamushi bite, and close examination revealed empty sella. To the best of our knowledge, this is the first report of adrenal insufficiency after a Mamushi bite in the global literature.
In the present case, the onset of hyponatremia occurred notably later than did the peak swelling of the right upper limb and the peak CK level. The timing of hyponatremia manifestation does not align with the severity of the disease due to a Mamushi bite. The patient's cortisol response during the CRH/GRF/TRH/LHRH stimulation test conducted on the 23rd day of admission, when symptoms from the Mamushi bite had already improved, was low. Therefore, we concluded that the adrenal insufficiency in this case represents a distinct condition unrelated to the relative adrenal insufficiency seen in critically ill patients. Regarding the results of the ACTH loading test performed on the 16th day of admission, adrenal function could possibly be underestimated due to administration of dexamethasone on the previous day. However, given the significantly low initial cortisol levels and the fact that the CRH stimulation test was conducted more than one week after the last steroid administration, we believe that even if the ACTH loading test results were underestimated, it does not change the current diagnosis.
Hypopituitarism has been reported as a rare complication of Russell’s viper bites [8]. In a case series of acute hypopituitarism following a Russell’s viper bite [9], the median time from the bite to the onset of hypopituitarism was 9 days, which is similar to the onset time in our case. The mechanism of acute hypopituitarism after a Russell’s viper bite is described as follows: in the first stage, the pituitary gland becomes more vulnerable due to irritation from the direct action of the snake venom and swells due to capillary leak syndrome. In the second stage, microthrombosis due to disseminated intravascular coagulation (DIC), hypotension, and intracranial hypertension occurs, resulting in pituitary gland infarction and bleeding [10]. In general, the detailed components and physiological effects of snake venom are unknown, but because many components, such as phospholipase A2 and L-amino acid oxidase, are shared across species [2, 11], Mamushi bites can cause the same pathological conditions as Russell’s viper bites.
In this case, the patient’s condition was accompanied by primary empty sella, but there was no history of trauma, intracranial surgery, or radiotherapy, and the condition was judged to be primary empty sella [4]. We concluded that the empty sella was present prior to the Mamushi bite. The etiology of a primary empty sella is not clearly understood, and various hypotheses have been proposed [4]. The causes include a defect in the sellar diaphragm, increased intracranial pressure, and changes in the pituitary gland volume. Increased intracranial pressure is reportedly involved in the development of empty sella, and a mechanism in which the subarachnoid space fits into the sella turcica due to increased intracranial pressure against the background of a defective or hypoplastic sellar diaphragm has been postulated [4, 12]. In the present case, there were no signs of hypotension, hemorrhage, or DIC; however, the swelling of the pituitary gland and the increased intracranial pressure caused by the snake venom may have further increased the pressure on the pituitary gland, which was already pressurized within the sella turcica, leading to hypopituitarism. The pituitary gland is one of the most vascularized tissues in the human body [13], and as part of the mechanism of Sheehan’s syndrome, which also causes hypopituitarism, a mechanism in which the pituitary gland, enlarged by pregnancy, presses on the superior pituitary artery has been postulated [14]. Based on the above considerations, we hypothesize that the patient with empty sella was originally vulnerable to compression and ischemia.
In the present case, the patient developed hypopituitarism after a Mamushi bite, but only a transient decrease in pituitary adrenal insufficiency was observed. The majority of patients who develop hypopituitarism in the acute phase of a Russell’s viper bite are reported to have hypopituitarism in the chronic phase [15, 16]. Russell’s viper bites have been reported to be 2.6–23 times more fatal than Mamushi bites [17, 18]. Since a Mamushi bite is milder than a Russell’s viper bite, we consider that the hypopituitarism in our case was transient. The prevalence of primary empty sella is reported to be 2–20% [19], and it is a fairly common condition; therefore, explaining this rare condition entirely by the presence of primary empty sella may be difficult [19]. Intraspecific geographic variation [17] and changes in venom composition with individual snake maturity [20] have also been reported, and the composition of the Mamushi venom in our case may be associated with the pathogenesis of the disease.
Adrenal insufficiency during hospitalization for Mamushi bite is very rare, but pituitary adrenal insufficiency may develop by the same mechanism as that involved in Russell’s viper bite, especially in patients with a fragile pituitary gland. If hyponatremia develops during hospitalization for Mamushi bite, pituitary adrenal insufficiency should be considered, and appropriate correction, corticosteroid-related tests, and head MRI should be performed.
In conclusion, we report for the first time a case of hyponatremia due to pituitary adrenal insufficiency following a Mamushi bite in a patient with empty sella. When hyponatremia develops during the course of a Mamushi bite, considering the possibility of adrenal insufficiency due to snake venom, cortisol measurement and loading tests should be performed, and head MRI should be performed to search for pituitary lesions.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ACTH:
-
Adrenocorticotrophin hormone
- CK:
-
Creatine kinase
- CRH/GRF/TRH/LHRH:
-
Corticotropin-releasing hormone / growth hormone-releasing factor / thyrotropin-releasing hormone / luteinizing hormone-releasing hormone
- DIC:
-
Disseminated intravascular coagulation
- MRI:
-
Magnetic resonance imaging
- Na:
-
Sodium
References
Hifumi T, Yamamoto A, Morokuma K, Ogasawara T, Kiriu N, Hasegawa E, et al. Surveillance of the clinical use of mamushi (Gloydius blomhoffii) antivenom in tertiary care centers in Japan. Jpn J Infect Dis. 2011;64:373–6.
Ando T, Nakashima S, Abe S, Watanabe D, Iwasaki K, Shinohara M, et al. Mamushi bites in a kidney transplant recipient. IJU Case Rep. 2022;5:297–9.
Okamoto O, Nakashima R, Yamamoto S, Hashimoto T, Takasaki T, Tokuda H, et al. A lethal case of mamushi (Gloydius blomhoffii) bite: severe bowel symptoms as a lethal sign. Acute Med Surg. 2016;4:135–9.
Chiloiro S, Giampietro A, Bianchi A, Tartaglione T, Capobianco A, Anile C, et al. Diagnosis of endocrine disease: primary empty sella: a comprehensive review. Eur J Endocrinol. 2017;177:R275–85.
Ahamed MAA, Shetty S, Hegde S, Prasannan P. The emptiness within: a case of empty sella syndrome. Cureus. 2022;14:e28941.
Hifumi T, Sakai A, Kondo Y, Yamamoto A, Morine N, Ato M, et al. Venomous snake bites: clinical diagnosis and treatment. J Intensive Care. 2015;3:16.
Yanase T, Tajima T, Katabami T, Iwasaki Y, Tanahashi Y, Sugawara A, et al. Diagnosis and treatment of adrenal insufficiency including adrenal crisis: a Japan Endocrine Society clinical practice guideline [Opinion]. Endocr J. 2016;63:765–84.
Tun-Pe, Phillips RE, Warrell DA, Moore RA, Tin-Nu-Swe, Myint-Lwin, et al. Acute and chronic pituitary failure resembling Sheehan’s syndrome following bites by Russell's viper in Burma. Lancet. 1987;2:763–7.
Rajagopala S, Thabah MM, Ariga KK, Gopalakrishnan M. Acute hypopituitarism complicating Russell’s viper envenomation: case series and systematic review. QJM. 2015;108:719–28.
Bhattacharya S, Krishnamurthy A, Gopalakrishnan M, Kalra S, Kantroo V, Aggarwal S, et al. Endocrine and metabolic manifestations of snakebite envenoming. Am J Trop Med Hyg. 2020;103:1388–96.
Damm M, Hempel BF, Süssmuth RD. Old world vipers-a review about snake venom proteomics of viperinae and their variations. Toxins (Basel). 2021;13:427.
Guitelman M, Garcia Basavilbaso N, Vitale M, Chervin A, Katz D, Miragaya K, et al. Primary empty sella (PES): a review of 175 cases. Pituitary. 2013;16:270–4.
Rolih CA, Ober KP. Pituitary apoplexy. Endocrinol Metab Clin North Am. 1993;22:291–302.
Dejager S, Gerber S, Foubert L, Turpin G. Sheehan’s syndrome: differential diagnosis in the acute phase. J Intern Med. 1998;244:261–6.
Naik BN, Bhalla A, Sharma N, Mokta J, Singh S, Gupta P, et al. Pituitary dysfunction in survivors of Russell’s viper snake bite envenomation: a prospective study. Neurol India. 2018;66:1351–8.
Proby C, Tha-Aung, Thet-Win, Hla-Mon, Burrin JM, Joplin GF. Immediate and long-term effects on hormone levels following bites by the Burmese Russell’s viper. Q J Med. 1990;75:399–411.
Kularatne SA. Epidemiology and clinical picture of the Russell’s viper (Daboia russelii russelii) bite in Anuradhapura, Sri Lanka: a prospective study of 336 patients. Southeast Asian J Trop Med Public Health. 2003;34:855–62.
Gopalakrishnan M, Vinod KV, Dutta TK, Shaha KK, Sridhar MG, Saurabh S. Exploring circulatory shock and mortality in viper envenomation: a prospective observational study from India. QJM. 2018;111:799–806.
Auer MK, Stieg MR, Crispin A, Sievers C, Stalla GK, Kopczak A. Primary empty sella syndrome and the prevalence of hormonal dysregulation. Dtsch Arztebl Int. 2018;115:99–105.
Chaiyabutr N, Chanhome L, Vasaruchapong T, Laoungbua P, Khow O, Rungsipipat A, et al. Comparative compositional and functional venomic profiles among venom specimens from juvenile, subadult and adult Russell’s viper (Daboia siamensis): correlation with renal pathophysiology in experimental rabbits. J Venom Anim Toxins Incl Trop Dis. 2022;28:20210111.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
RS managed the case and wrote and revised the manuscript. HN and TK assisted in the preparation and revision of the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work. All authors take full responsibility for the integrity of the study and final manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was not required because this was a case report. Therefore, the need for ethics approval was waived by the Ethics Committee of Hyogo Prefectural Tamba Medical Center.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Journal Editor.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sugimoto, R., Kenzaka, T. & Nishisaki, H. Hyponatremia due to adrenal insufficiency after a Mamushi bite: a case report. BMC Endocr Disord 23, 219 (2023). https://doi.org/10.1186/s12902-023-01466-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01466-4