Abstract
Background
To investigate the prevalence of euthyroid sick syndrome (ESS) and to evaluate the outcomes and risk factors associated with ESS among hospitalized patients with diabetic ketosis (DK) or diabetic ketoacidosis (DKA).
Methods
Laboratory and clinical data of 396 adult hospitalized DK/DKA patients with or without ESS were collected and analyzed. Spearman linear analysis and multivariable logistic regression analyses were used to evaluate correlated factors of thyroid hormones and risk factors of ESS.
Results
Most of the individuals were diagnosed with type 2 diabetes (359/396, 90.7%). The prevalence of ESS was 57.8% (229/396). Patients in ESS group were older and had a longer course of diabetes. Levels of thyroid hormones, serum lipids, and parameters reflecting acidosis were significantly decreased in ESS group. The proportion of patients with infection, acute renal injury and DKA was significantly higher in ESS group than in control group, accompanied by longer hospitalization stay and higher hospitalization costs. Free triiodothyronine positively correlates with albumin, eGFR, parameters reflecting acidosis and lipid profiles (All P < 0.001), and negatively correlates with age, onset age, 24-h urine albumin, hsCRP and WBC count (All P < 0.001). Hypoalbuminemia, low level of carbon dioxide combining power, high level of HbA1c and WBC, and co-infection are shown to be risk factors for ESS (OR = 0.866, 0.933, 1.112, 1.146, 1.929, respectively; All P < 0.05).
Conclusions
The prevalence of ESS was high in adult DK/DKA patients. Patients with ESS had inferior clinical and socioeconomic outcomes. Early recognition and management of patients with ESS may be necessary to improve outcome.
Similar content being viewed by others
Background
Over the past decades, the prevalence of diabetes mellitus (DM) is increasing with the global booming of obesity and metabolic syndrome. According to recent estimates, about 536.6 million adults (10.5% of the population) suffered from diabetes globally in 2021 and the number was expected to rise to 783.2 million (12.2% of the population) in 2045 [1]. Impaired insulin secretion and varied degrees of peripheral insulin resistance is the major pathogenesis mechanism of diabetes. Insulin deficiency can increase lipolysis and along with it is the accelerated process of beta oxidation which can produce ketone bodies [2] and thus cause diabetic ketosis (DK) or diabetic ketoacidosis (DKA). Characterized as an acute complication of diabetes, DKA usually occurs in young patients with type 1 DM (T1DM) and used to be fatal in pre-insulin era. With the advancement in diagnosis and treatment, DKA is now a treatable condition. The mortality of DKA has declined dramatically these years, especially in the developed countries [3]. However, previous studies depicted that the morbidity and mortality of DKA remains high in developing countries [4]. Of note, almost one-fourth of DKA was found to be the first behaving of diabetes in older patients with type 2 DM (T2DM) [5]. A large proportion of Chinese population is still in high risk of DKA [6], which is in line with our clinical experiences. Despite of the extensively improved cure rate, DKA remains to be a significant cause of mortality in patients, especially in children and young adults. Also, DKA poses heavy burdens on health-care system. DKA is responsible for over 500,000 hospital days per year and the treatment of DKA accounts for an estimated total cost of $2.4 billion annually [2].
Euthyroid sick syndrome (ESS), also named non-thyroidal illness syndrome (NTIS) or low T3 syndrome, is characterized mainly by a reduced level of serum triiodothyronine (T3), normal or decreased level of serum thyroxine (T4) and thyroid stimulating hormone (TSH), and elevated reverse triiodothyronine (rT3) levels [7]. ESS has been reported in patients with acute and chronic illnesses such as acute myocardial infarction, trauma, postoperative and acute infection, as well as in critically ill patients [8, 9]. The scale of the decrease in serum concentration of thyroid hormones is indicated to reflect the severity of the disorder and as a result, is associated with prognosis [9]. Previously, some researchers have pointed out that the reduction of serum FT3 is positively associated with the severity of DKA in children with T1DM [10, 11]. However, fewer studies investigated the thyroid status and the associated verified outcomes in older patients and in patients with T2DM during DK/DKA, while these patients constitute the majority in our clinical practice. Therefore, we aimed to investigate the prevalence of ESS and to evaluate the outcomes and risk factors associated with ESS among adult patients with DK/DKA, not only in patients with T1DM, but also in those with T2DM.
Methods
Study population and design
Hospitalized patients with DK/DKA were enrolled retrospectively from the Department of Endocrinology of The Second Affiliated Hospital of Guangzhou Medical University, from January 2017 to January 2020. The study followed the Declaration of Helsinki and was approved by the Ethics Committee of The Second Affiliated Hospital of Guangzhou Medical University (Approval number 2021-hg-ks-10). Written informed consent was waived due to the retrospective nature of the study. All patients were admitted to the ward due to uncontrolled hyperglycemia complicated with DK/DKA. The diagnosis of diabetes was based on the World Health Organization (WHO) criteria [12]. DK was diagnosed in diabetic patients with blood ketone body > 3 mmol/L or positive urine ketone body, blood glucose > 11 mmol/L, and bicarbonate ion (HCO3−) ≥ 15 mmol/L or arterial power of hydrogen (pH) ≥ 7.3 [2]. The diagnosis of DKA was made if serum HCO3− level was under 15 mmol/L and/or arterial pH level was under 7.3, and blood glucose was ranged from 16.7 to 33.3 mmol/L [2, 13]. We did not include euglycaemic ketosis or euglycaemic ketoacidosis in the study. Patients were excluded if they met one of the following exclusion criteria: (1) diagnosed with primary thyroid disease, including thyroid cancer, hyperthyroidism, and hypothyroidism; (2) severe hepatic dysfunction or chronic kidney dysfunction; (3) with history of malignant tumor; (4) with history of pituitary disease; (5) pregnancy.
Measurement and data collection
Demographic characteristics including gender, age, onset age, duration of diabetes, previous antidiabetic medications, smoking history, and family history of diabetes were collected through the review of medical records. Body mass index (BMI) was calculated as the body weight (kg) divided by body square height (m). Blood pressure was measured in the sitting position on the right arm in line with the heart after taking a 10-min break and was recorded as an average of three times. We also collected information about the duration and cost of hospitalization of the patients. Venous blood samples were collected in the morning after an overnight fast at the second day of admission. Arterial blood sampling was performed by experienced nurses. Thyroid function tests including serum free triiodothyronine (FT3), free thyroxine (FT4), thyroid stimulating hormone (TSH), and thyroid antibodies were routinely measured, using electrochemiluminescence immunoassays. Normal ranges of thyroid hormones were as follows: TSH 0.27–4.2 mIU/L, FT3 3.10–6.80 pmol/L, and FT4 12.00–22.00 pmol/L. Patients with the serum FT3 less than 3.1 pmol/L, combined with or without a reduction of FT4 or TSH, were included in the ESS group [14, 15]. Serum analysis including fasting plasma glucose, HbA1c, fasting C-peptide, arterial gas test, blood routine test, electrolytes, hepatic and renal function, and lipid profiles were accomplished by routine laboratory methods at the Department of Clinical Laboratory. The estimated glomerular filtration rate (eGFR) was calculated according to Modification of Diet in Renal Disease equation: eGFR (mL/min/1.73 m2) = 186 × (SCr/88.4)−1.154 × (age)−0.203 × (0.742 if female) [16]. Urine samples of 24 h were collected to measure urine albumin levels by the biuret method. The diagnostic criteria of acute kidney injury (AKI) is a sudden increase in serum creatinine concentration by ≥ 50% within 7 days or ≥ 0.3 mg/dL (26.5 μmol/L) within 48 h, or urine volume < 0.5 ml/kg/h for > 6 h [17]. Infections (pneumonia, urinary tract infection, gastrointestinal tract infection, etc.) were diagnosed according to the clinical manifestations, laboratory and imaging examinations.
Statistical analyses
All statistical analyses were performed using IBM SPSS software version 25.0 (IBM Corp., Armonk, New York, USA). Normally distributed data were presented as mean ± standard deviation (SD) and non-normally distributed data were presented as median (interquartile range). Categorical data were expressed as number (%). Independent sample two-tail t-test was applied for the comparisons of numeric variables with normality while the Mann–Whitney U-test was applied for the comparisons of non-normally variables. Chi-squared test was used for comparisons of categorical variables. Spearman correlation tests were conducted to evaluate associations between FT3, FT4 and other variables. Multiple logistic regression analysis was performed to identify the risk factors for ESS in DK/DKA patients. A two-tail P value < 0.05 was regarded as statistically significant.
Results
Baseline demographic and clinical characteristics of participants with and without ESS
Figure 1 shows the flowchart of subject selection. The study enrolled 396 patients with DK/DKA, including 216 males and 180 females, with a mean age of 57.5 ± 18.3 years. Table 1 displays the demographic and clinical characteristics of the patients. Patients with T2DM constituted the majority (359/396, 90.7%). No significant difference was observed in the incidence of ESS between T1DM and T2DM. Of the 396 patients, 57.8% (n = 229) were found to be complicated with ESS (165 with DK, 64 with DKA). Compared with subjects without ESS, individuals with ESS were older and had a longer course of diabetes. The levels of white blood cell count (WBC), neutrophil absolute value, neutrophil/lymphocyte (N/L) ratio, high sensitivity C-reactive protein (hsCRP) and creatinine were significantly higher in the ESS group than in the euthyroid group, whereas eGFR, pressure of carbon dioxide (PaCO2), HCO3−, carbon dioxide combining power (CO2CP), FT3, FT4, FT3/FT4 ratio, total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) levels were significantly lower in ESS group than in euthyroid group.
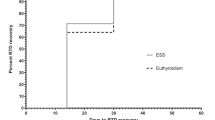
Clinical and socioeconomic outcomes of DK/DKA patients in ESS group and without ESS group
Considering the possible negative impact of ESS, we compared clinical and socioeconomic outcomes in the two groups. As shown in Table 2, the duration of hospital stay (9 (7, 11) day vs. 8 (7, 10) day, P = 0.018) and hospitalization costs (11,833 (9598, 15,974) yuan vs. 10,272 (8456, 11,718) yuan, P < 0.001) were significantly higher in individuals with ESS than in euthyroid individuals. Importantly, the occurrence of comorbidities including co-infection, the prevalence of AKI and DKA was also significantly higher in the ESS group (P < 0.001, P = 0.009, P = 0.021, respectively).
Analysis of correlated factors of thyroid hormones
The relationships between FT3, FT4 levels and clinical factors were presented in Table 3. Both FT3 and FT4 positively correlated with levels of BMI, serum albumin, pH, PaCO2, CO2CP, and HCO3−, and negatively correlated with WBC, neutrophils, and N/L ratio (All P < 0.05). FT3 was also positively related to eGFR, lymphocyte, TC, LDL-C, and HDL-C, and was negatively related to age, onset age, diabetes duration, HbA1c, creatinine, 24-h urine albumin, and hsCRP (All P < 0.05). But FT4 correlated with none of these parameters. The associations between FT3 and represented factors including CO2CP, albumin, WBC, and HbA1c were shown in Fig. 2 (r = 0.236, 0.480, -0.502, -0.119, respectively; All P < 0.05).
Correlations between FT3 and albumin (a), CO2CP (b), WBC (c), HbA1c (d). Within patients, there were significantly correlations between FT3 and albumin, CO2CP, WBC, HbA1c, respectively (r = 0.477, 0.235, -0.504, -0.117, P < 0.05). Abbreviations: HbA1c, glycated hemoglobin; WBC, white blood cell count; FT3, free triiodothyronine
Risk factors for ESS patients with DK/DKA
After adjusting various confounding factors, multiple logistic regression presented associated factors of ESS including HbA1c (OR = 1.112, P = 0.040, 95%CI 1.005 ~ 1.231), CO2CP (OR = 0.933, P = 0.007, 95%CI 0.888 ~ 0.981), albumin (OR = 0.866, P < 0.001, 95%CI 0.814 ~ 0.921), WBC (OR = 1.146, P = 0.002, 95%CI 1.052 ~ 1.248), and co-infection (OR = 1.929, P = 0.031, 95%CI 1.063 ~ 3.500) (Table 4). Patients with severe acidosis, hypoalbuminemia, high WBC count and co-infection were more likely to present ESS.
Discussion
As expected, the present study revealed a high prevalence of ESS in hospitalized patients with DK/DKA. Different from previous studies which mainly focused on young patients with T1DM [10, 11, 18], most of the patients were middle-aged and elderly patients with T2DM in this research. Moreover, patients with ESS were older in age and had a longer course of diabetes. But the prevalence of ESS in our study was comparable to the ones in previous reports.
ESS is considered to be an independent risk factor for the severity of illness and its prognosis [9, 19,20,21]. Previous studies have shown that the reduction of FT3 and FT4 predicted the severity of illness and hospital mortality rates of patients [22]. The changes of thyroid hormone levels in ESS are not associated with primary thyroid disease [19,20,21, 23]. The reduction of FT3 is an adaptive response to stress during the acute phase response in critical illness [24, 25] and the serum level of FT3 could return to normal with treatment and recovery of illness [26]. Shao et al. found that the ESS patients with DKA in children had lower serum FT3, FT4 and TSH, accompanied with worse glucose control [11]. Previous studies demonstrated high prevalence of thyroid dysfunction in DKA patients [22, 27]. These findings were in accordance with our study. In the present research, patients with ESS had lower levels of serum FT3 and FT4, and higher levels of HbA1c. As for the hospitalized outcomes, all the patients got recovered from DK/DKA and thus the mortality rate was 0% in the study. However, much heavier socioeconomic burdens were indicated in the ESS group by a longer hospital stay and higher hospitalization costs. Also, the occurrence of comorbidities including AKI and co-infection were significantly higher in patients with ESS.
The changes in thyroid function can affect renal function directly, as well as make indirect alterations by affecting systemic hemodynamics, metabolism, and cardiac function [28, 29]. The relationships between thyroid hormones and renal function have been broadly recognized these years. But most of the evidences came from patients with chronic renal impairment [28,29,30,31]. Previously, a study reported a high prevalence of ESS (about 70%) in patients with AKI [29]. As known, DK/DKA is a direct imposing factor for AKI. Other studies also documented the high prevalence of AKI in DK/DKA [32, 33]. But few researches explored the the correlation between ESS and AKI in DK/DKA. In our study, we found a higher occurrence of AKI in patients with ESS compared with euthyroid patients. Serum creatinine, eGFR and 24-h urine albumin was significantly associated with serum FT3 level. However, due to the complicated systemic alterations (hemodynamics, metabolism, etc.), the cause-and-effect relationship between changes of thyroid hormones and kidney function in acute diseases has not been well-established based on current evidences. Further studies are needed to elucidate the associations.
In the present study, we assessed parameters reflecting the extent of acidosis, including pH, PaCO2, HCO3− and CO2CP, to evaluate the association between acidosis and the levels of thyroid hormones. We noticed that DK/DKA patients with ESS have higher levels of acidosis. The values of pH and CO2CP were positively associated with both FT3 and FT4 levels. And the prevalence of ESS increased with higher degree of acidosis. Previous studies described similar changes of thyroid hormones in DKA patients [10, 26]. Rashidi et al. pointed out that the lower level of pH in DKA patients, the lower level FT3 [26]. The metabolic acidosis may play important role in the formation of ESS by affecting the thyroid hormone metabolism [34]. Also, CO2CP was manifested as a significant independent risk factor for ESS in DK/DKA patients in our study. Together, these results indicated a connection between acidosis state and the alterations in thyroid hormones in DK/DKA patients.
Serum albumin was suggested to strongly positively correlate with thyroid hormone (FT3 and FT4) levels in DK/DKA patients in the present study. Albumin is known as a major plasma protein. T3 levels decline in the early stage of ESS, and the decrease of T4 to T3 conversion is related to the reduction in albumin levels [35]. Low albumin level is widely used as a predictor of malnutrition. According to previous researches, malnutrition may be one of the factors affecting thyroid hormones [36, 37]. But in our study, most of the patients were in fine nutritional status. In fact, serum albumin levels may also be influenced by various factors such as liver diseases and changes of intravascular volume [38]. They may decrease as a result of inflammation due to acute or chronic diseases [39]. Therefore, serum albumin has been validated as a measurement of disease severity in the Acute Physiology and Chronic Health Evaluation scoring system [40]. The degradation of albumin level was shown to be an independent predictor of ICU mortality in previous studies [37]. Hypoalbuminemia was also found to be associated with ESS in various kinds of diseases (rheumatoid arthritis [41], COVID-19 infection [42], acute pancreatitis [43], etc.). Serum albumin levels were shown to be reduced in ESS pediatric patients with DK/DKA [27]. Besides the aforementioned influencing factors, the deficiency of insulin can also cause a drop in albumin in DK/DKA, since albumin synthesis in hepatocytes depends on sufficient insulin secretion [11, 44]. In the present research, albumin deficiency was also indicated to be an independent risk factor for ESS, and its reduction might present a worse prognosis in DK/DKA patients.
Inflammation is considered as one of the precipitating factors for many pathological circumstances including DK/DKA [45, 46]. It has been reported that DKA correlated with active systemic inflammatory response and oxidative stress [47, 48]. Elevations in nonspecific inflammatory cytokines were found to correlate strongly and positively with DK/DKA [49,50,51]. Previous studies also pointed out that serum levels of thyroid hormones were negatively associated with the serum concentrations of inflammatory cytokines [52]. In the present study, inflammatory indicators, including WBC, neutrophils, hsCRP and N/L ratio, were significantly higher in individuals with ESS, and were negatively associated with FT3. Moreover, elevated WBC and co-infection were risk factors for ESS in DK/DKA. Previous studies have also proposed other factors associated with ESS, including uric acid, serum lipids and other metabolic indicators [53,54,55]. But in this study, we did not have similar findings.
This study has several limitations. First, it was single-center research with a relatively small number of patients. Second, the cause-and-effect relationship could not be built due to the retrospective nature of the study. Third, follow-up was not done to evaluate the dynamic change of thyroid hormones in ESS patients after recovering of DK/DKA. Therefore, the results need to be cautiously interpreted.
Conclusion
This study demonstrated a high prevalence of ESS in adult DK/DKA patients with elder ages, most of whom were with T2DM. Patients with ESS had inferior clinical and socioeconomic outcomes. Low albumin levels, high WBC counts, poor glycemic control, co-infection, and higher levels of acidosis were risk factors of ESS in DK/DKA patients. Diabetic education, early detection and treatment of DK/DKA is necessary not only for patients with T1DM, but also for patients with T2DM. Early interventions for patients with the identified risk factors for ESS might be helpful to improve hospitalization outcomes.
Availability of data and materials
The data used for the current study are available from the corresponding author on reasonable request.
Abbreviations
- ESS:
-
Euthyroid sick syndrome
- DK:
-
Diabetic ketosis
- DKA:
-
Diabetic ketoacidosis
- DM:
-
Diabetes mellitus
- T1DM:
-
Type 1 DM
- T2DM:
-
Type 2 DM
- NTIS:
-
Non-thyroidal illness syndrome
- T3:
-
Triiodothyronine
- T4:
-
Thyroxine
- TSH:
-
Thyroid stimulating hormone
- FT3:
-
Free triiodothyronine
- FT4:
-
Free thyroxine
- rT3:
-
Reverse triiodothyronine
- WHO:
-
World Health Organization
- HCO3− :
-
Bicarbonate ion
- pH:
-
Power of hydrogen
- BMI:
-
Body mass index
- eGFR:
-
Estimated glomerular filtration rate
- AKI:
-
Acute kidney injury
- SD:
-
Standard deviation
- WBC:
-
White blood cell count
- N/L ratio:
-
Neutrophil/lymphocyte ratio
- hsCRP:
-
High sensitivity C-reactive protein
- PaCO2:
-
Pressure of carbon dioxide
- CO2CP:
-
Carbon dioxide combining power
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183: 109119.
Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335–43.
Gibb FW, Teoh WL, Graham J, Lockman KA. Risk of death following admission to a UK hospital with diabetic ketoacidosis. Diabetologia. 2016;59(10):2082–7.
Nyenwe EA, Kitabchi A. The evolution of diabetic ketoacidosis: An update of its etiology, pathogenesis and management. Metabolism. 2016;65(4):507–21.
Ooi E, Nash K, Rengarajan L, Melson E, Thomas L, Johnson A, et al. Clinical and biochemical profile of 786 sequential episodes of diabetic ketoacidosis in adults with type 1 and type 2 diabetes mellitus. BMJ Open Diabetes Res Care. 2021;9(2): e002451.
Li J, Yang D, Yan J, Huang B, Zhang Y, Weng J. Secondary diabetic ketoacidosis and severe hypoglycaemia in patients with established type 1 diabetes mellitus in China: A multicentre registration study. Diabetes Metab Res Rev. 2014;30(6):497–504.
Boelen A, Kwakkel J, Fliers E. Beyond low plasma T3: Local thyroid hormone metabolism during inflammation and infection. Endocr Rev. 2011;32(5):670–93.
Pappa TA, Vagenakis AG, Alevizaki M. The nonthyroidal illness syndrome in the non-critically ill patient. Eur J Clin Invest. 2011;41(2):212–20.
Fliers E, Bianco AC, Langouche L, Boelen A. Thyroid function in critically ill patients. Lancet Diabetes Endocrinol. 2015;3(10):816–25.
Hu Y, Li G, Wang W. Euthyroid sick syndrome in children with diabetic ketoacidosis. Saudi Med J. 2015;36(2):243–7.
Shao P, Guo S, Li G, Qin D, Li S, Luan Y. Determinants of deranged thyroid function parameters in children admitted for management of diabetic ketoacidosis/diabetic ketosis. BMC Endocr Disord. 2020;20(1):135.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–53.
Vellanki P, Umpierrez GE. Diabetic ketoacidosis: A common debut of diabetes among African with type 2 diabetes. Endocr Pract. 2017;23(8):971–8.
Mebis L, Van den Berghe G. Thyroid axis function and dysfunction in critical illness. Best Pract Res Clin Endocrinol Metab. 2011;25(5):745–57.
Economidou F, Douka E, Tzanela M, Nanas S, Kotanidou A. Thyroid function during critical illness. Hormones (Athens). 2011;10(2):117–24.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–70.
Levey AS, James MT. Acute kidney injury. Ann Intern Med. 2017;167(9):ITC66–80.
Bogale KT, Hale DT, Schaefer E, Bangalore KB. Prevalence and factors associated with diabetic ketoacidosis at diagnosis of type 1 diabetes: A report from a tertiary medical center in Central Pennsylvania. Endocrinol Diabetes Metab. 2020;4(2): e00186.
Van den Berghe G. Non-thyroidal illness in the ICU: A syndrome with different faces. Thyroid. 2014;24(10):1456–65.
Wang F, Pan W, Wang H, Wang S, Pan S, Ge J. Relationship between thyroid function and ICU mortality: A prospective observation study. Crit Care. 2012;16(1):R11.
Ataoğlu HE, Ahbab S, Serez MK, Yamak M, Kayaş D, Canbaz ET, Çetin F, Seçmeler S, Şar D, Yenigün M. Prognostic significance of high free T4 and low free T3 levels in non-thyroidal illness syndrome. Eur J Intern Med. 2018;57:91–5.
Mirboluk AA, Rohani F, Asadi R, Eslamian MR. Thyroid function test in diabetic ketoacidosis. Diabetes Metab Syndr. 2017;11(Suppl 2):S623–5.
Maiden MJ, Torpy DJ. Thyroid hormones in critical illness. Crit Care Clin. 2019;35(2):375–88.
Bello G, Ceaichisciuc I, Silva S, Antonelli M. The role of thyroid dysfunction in the critically ill: A review of the literature. Minerva Anestesiol. 2010;76(11):919–28.
Ranasinghe AM, Bonser RS. Thyroid hormone in cardiac surgery. Vasc Pharmacol. 2010;52(3–4):131–7.
Rashidi H, Ghaderian SB, Latifi SM, Hoseini F. Impact of diabetic ketoacidosis on thyroid function tests in type 1 diabetes mellitus patients. Diabetes Metab Syndr. 2017;11(Suppl 1):S57–9.
Joseph J, Saroha V, Payne H, Paul P, Didi M, Isherwood D, Blair J. Thyroid function at diagnosis of type I diabetes. Arch Dis Child. 2011;96(8):777–9.
Han Q, Zhang J, Wang Y, Li H, Zhang R, Guo R, Li L, Teng G, Wang J, Wang T, Liu F. Thyroid hormones and diabetic nephropathy: An essential relationship to recognize. Nephrology (Carlton). 2019;24(2):160–9.
Iglesias P, Olea T, Vega-Cabrera C, Heras M, Bajo MA, del Peso G, Arias MJ, Selgas R, Díez JJ. Thyroid function tests in acute kidney injury. J Nephrol. 2013;26(1):164–72.
Chen Y, Zhang W, Wang N, Wang Y, Wang C, Wan H, Lu Y. Thyroid parameters and kidney disorder in type 2 diabetes: result from the METAL Study. J Diabetes Res. 2020;2020:4798947.
Zhao W, Li X, Liu X, Lu L, Gao Z. Thyroid function in patients with type 2 diabetes mellitus and diabetic nephropathy: a single center study. J Thyroid Res. 2018;2018:9507028.
Woodrow G, Brownjohn AM, Turney JH. Acute renal failure in patients with type 1 diabetes mellitus. Postgrad Med J. 1994;70(821):192–4.
Huang S, Huang C, Lin C, Cheng B, Chiang Y, Lee Y, Yeh S, Chan C, Chua W, Lee Y, Ting W. Acute kidney injury is a common complication in children and adolescents hospitalized for diabetic ketoacidosis. PLoS ONE. 2020;15(10): e0239160.
Tahirović HF. Thyroid hormones changes in infants and children with metabolic acidosis. J Endocrinol Invest. 1991;14(9):723–6.
Guo J, Hong Y, Wang Z, Li Y. Analysis of the incidence of Euthyroid Sick Syndrome in comprehensive intensive care units and related risk factors. Front Endocrinol (Lausanne). 2021;12: 656641.
Douyon L, Schteingart DE. Effect of obesity and starvation on thyroid hormone, growth hormone, and cortisol secretion. Endocrin Metab Clin. 2002;31(1):173–89.
Aschettino-Manevitz DL, Ornstein RM, Meyer Sterling W, Kohn N, Fisher M. Triiodothyronine (T3) and metabolic rate in adolescents with eating disorders: Is there a correlation? Eat Weight Disord. 2012;17(4):e252–8.
Takagi K, Umeda Y, Yoshida R, Nobuoka D, Kuise T, Fushimi T, Fujiwara T, Yagi T. Preoperative controlling nutritional status score predicts mortality after hepatectomy for hepatocellular carcinoma. Dig Surg. 2019;36(3):226–32.
Maimaiti Z, Xu C, Fu J, Li WT, Chai W, Zhou Y, Chen J. A novel biomarker to screen for malnutrition: Albumin/fibrinogen ratio predicts septic failure and acute infection in patients who underwent revision total joint arthroplasty. J Arthroplasty. 2021;36(9):8.
Vincent JL, Moreno R. Clinical review: scoring systems in the critically ill. Crit Care. 2010;14(2):207.
Tsuji H, Hashimoto M, Harada T, Tanaka M, Ito H, Murakami K, Ohmura K, Fujii T, Mimori T. Persistent anemia and hypoalbuminemia in rheumatoid arthritis patients with low serum triiodothyronine level. Mod Rheumatol. 2020;30(4):640–7.
Baldelli R, Nicastri E, Petrosillo N, Marchioni L, Gubbiotti A, Sperduti I, Giacinto PD, Rizza L, Rota F, Franco M, Lania A, Aimaretti G, Ippolito G, Zuppi P. Thyroid dysfunction in COVID-19 patients. J Endocrinol Invest. 2021;44(12):2735–9.
Qu C, Duan Z, Xiao X, Wei M, Gao K, Yu X, Ke L, Tong Z, Li W. Nonthyroidal illness syndrome in acute pancreatitis patients: an 8-year cohort study. BMC Gastroenterol. 2022;22(1):40.
Cheng PC, Hsu SR, Cheng YC. Association between serum albumin concentration and ketosis risk in hospitalized individuals with type 2 diabetes mellitus. J Diabetes Res. 2016;2016:1269706.
Koh C, Bhoo-Pathy N, Ng K, Jabir RS, Tan G, See M, Jamaris S, Taib NA. Utility of pre-treatment neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as prognostic factors in breast cancer. Brit J Cancer. 2015;113(1):150–8.
Umpierrez GE, Kitabchi AE. Diabetic ketoacidosis: Risk factors and management strategies. Treat Endocrinol. 2003;2(2):95–108.
Ma S, Jin Y, Xu W, Hu W, Bai F, Wu X. Increased serum levels of ischemia-modified albumin and C-reactive protein in type 1 diabetes patients with ketoacidosis. Endocrine. 2012;42(3):570–6.
Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Diabetes. 2004;53(8):2079–86.
Xu W, Wu H, Ma S, Bai F, Hu W, Jin Y, Liu H. Correlation between peripheral white blood cell counts and hyperglycemic emergencies. Int J Med Sci. 2013;10(6):758–65.
Karavanaki K, Kakleas K, Georga S, Bartzeliotou A, Mavropoulos G, Tsouvalas M, Vogiatzi A, Papassotiriou I, Karayianni C. Plasma high sensitivity C-reactive protein and its relationship with cytokine levels in children with newly diagnosed type 1 diabetes and ketoacidosis. Clin Biochem. 2012;45(16–17):1383–8.
Du S, Yang X, Shi D, Su Q. Characteristics of type 2 diabetes with ketosis in Baoshan. Yunnan of China J Diabetes Res. 2016;2016:7854294.
Mönig H, Arendt T, Meyer M, Kloehn S, Bewig B. Activation of the hypothalamo-pituitary-adrenal axis in response to septic or non-septic diseases–implications for the Euthyroid Sick Syndrome. Intens Care Med. 1999;25(12):1402–6.
Kota SK, Meher LK, Krishna S, Modi K. Hypothyroidism in metabolic syndrome. Indian J Endocrinol Metab. 2012;16(Suppl 2):S332–3.
Li J, Wang X, Xie T, Lin W, Yang H, Li T, Xu K, Zhang B, Qu X, Zhang H, Ning W, Liu S, Li T, Zuo X, Liu S, Zhang W. Hypothyroidism and its association with systemic lupus erythematosus: A cross sectional study in Chinese patients. Am J Med Sci. 2021;361(1):63–8.
Taneichi H, Sasai T, Ohara M, Honma H, Nagasawa K, Takahashi T, Ishii M, Fujiwara F, Yamashina M, Kajiwara T, Takabe N, Takahashi K, Satoh J. Higher serum free triiodothyronine levels within the normal range are associated with metabolic syndrome components in type 2 diabetic subjects with euthyroidism. Tohoku J Exp Med. 2011;224(3):173–8.
Acknowledgements
Not applicable.
Funding
The present study was supported by grant from National Natural Science Foundation of China (grant number 81800726) to ZXD.
Author information
Authors and Affiliations
Contributions
DXY and YM contributed equally to this manuscript. DXY analyzed the data and drafted the manuscript. YM helped with the data analyse and interpretation. LWG provided the clinical information. YHY and CZS participated in the collection of clinical material. ZXD conceived and designed the project and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Review Board for Human Investigation and the Ethics Committee of The Second Affiliated Hospital of Guangzhou Medical University (Approval number 2021-hg-ks-10). The investigations were performed in accordance with the principles of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Deng, Xy., Yi, M., Li, Wg. et al. The prevalence, hospitalization outcomes and risk factors of euthyroid sick syndrome in patients with diabetic ketosis/ketoacidosis. BMC Endocr Disord 23, 195 (2023). https://doi.org/10.1186/s12902-023-01451-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01451-x