Abstract
Background
The weight-adjusted waist circumference index (WWI) is a novel obesity indicator that offers improved accuracy in assessing both muscle and fat mass compared to traditional measures. This study aimed to investigate the association between WWI and bone mineral density (BMD) in adults.
Methods
Weighted multivariate logistic regression, subgroup analysis, interaction tests and restricted cubic spline (RCS) curves were used to explore the relationship between WWI and BMD based on data from the National Health and Nutrition Examination Survey (NHANES).
Results
This study had 40,568 individuals in total. At all four measurement sites, we detected a negative linear correlation between WWI and BMD. Even when quartile factors for WWI were created, this unfavorable connection maintained. In comparison to those in the lowest quartile, those in the highest percentile of WWI showed declines in lumbar BMD of 0.08 g/cm2 and femoral neck BMD of 0.03 g/cm2, respectively. This adverse correlation, nevertheless, differed among several categories.
Conclusions
Our findings suggest an adverse correlation between WWI and BMD among US adults. Employing WWI as a tool for osteoporosis prevention in the general population may enhance interventions.
Similar content being viewed by others
Background
Osteoporosis is a pervasive public health problem characterized by low Bone Mineral Density (BMD), making early prevention and risk factor identification crucial [1, 2]. Population-based research advances have resulted in more accurate evaluations of fracture risk and a broader choice of fracture prevention methods [3, 4].
Obesity is a complicated metabolic disorder [5]. Obesity prevalence has increased significantly globally, with roughly 30% of the world’s individuals currently afflicted [6, 7]. Traditional obesity markers, such as BMI and waist circumference (WC), have limitations, notably in their capacity to distinguish between muscle and fat mass, which may lead to less accurate estimates of an individual’s health risk [8,9,10]. As a result, it has been suggested that body composition and body fat distribution more closely reflect negative metabolic features [11, 12].
In contrast, the weight-adjusted waist circumference index (WWI) has emerged as a potentially more reliable and informative obesity indicator [13, 14]. It has been associated with age-related changes in body composition and has been linked to various health conditions, suggesting its potential as a valuable tool in evaluating health risks [15,16,17,18,19].
Despite the promise that WWI holds as an obesity indicator, the relationship between WWI and bone metabolism has not been previously explored in the scientific literature. In response to this knowledge gap, the present study aims to explore the association between WWI and BMD by analyzing data from the National Health and Nutrition Examination Survey (NHANES), which was conducted between 1999 and 2018.
Methods
Study participants
The National Center for Health Statistics (NCHS) conducts the well-known National Health and Nutrition Examination study (NHANES), a cross-sectional study that is nationally representative [20,21,22]. All research participants provided written agreement at the time of recruitment, and the NCHS Research Ethics Review Board approved the study’s methodology. Over 10 survey cycles in a period of twenty years (1999–2018), the survey was carried out. We removed 31,452 people under the age of 20, 23,796 participants with insufficient WWI data, and 5,500 participants without relevant BMD data. The final number of participants in the research was 40,568 (Fig. 1).
WWI
The WWI is determined by dividing waist circumference (cm) by the square root of body weight (kg), is a tool for assessing body fat mass and muscle mass [23]. Certified health professionals took participants’ weights and waist circumferences at the mobile examination facility. By taking off their shoes and bulky clothing, the participants’ weights were calculated. The waist circumference was estimated by drawing a horizontal line above the highest lateral border of the right iliac bone and then inserting a tape measure at the junction of the two lines [24].
BMD
BMD values were evaluated using a dual-energy X-ray absorptiometry scan in four separate areas, including the lumbar, pelvic, femoral neck, and total BMD, as in prior research, to reduce bias across diverse populations [25]. Supplementary file 1 details from which file the BMD of the different parts was extracted.
Covariables
Covariates included age, sex, smoking status, dietary inflammatory index, low-density lipoprotein cholesterol (LDL-C), race, cancer, high blood pressure, use of hormone medication, take prescription for cholesterol, diabetes, income-to-poverty ratio (PIR), triglycerides, education level, and history of bone fracture.
Statistical analysis
Considering that NHANES uses a complex multi-stage probability sampling design. To assess participant demographics by WWI quartile, we employed the chi-square test and t-test. For examining the linear relationship between WWI and BMD, we used weighted multivariate logistic regression analysis. After categorizing WWI into quartiles, we utilized a trend test to analyze the linear association trend between WWI and BMD. Additionally, subgroup analysis was carried out to investigate the relationship between WWI and BMD in various subpopulations based on factors such as sex, race, education, high blood pressure, and diabetes status. We also conducted interaction tests to assess the consistency of the associations across subgroups. To investigate the nonlinear association between WWI and BMD, we used restricted cubic spline (RCS) curve. We established statistical significance at two-sided P < 0.05 [26, 27]. The statistical software packages used were R (version 4.2), Python (version 3.10.4) and Empowerstats (version 5.0).
Results
Baseline characteristics
The study included 40,568 participants, with a mean (SD) age of 48.74 (18.01) years, and 51.56% of participants were female. The mean (SD) BMI and WWI for all participants were 28.49 (6.31) kg/m2 and 11.01 (0.85) cm/√kg. Compared with participants in the lowest WWI quartile, those in the highest quartile were more likely to be female, Mexican American, and elderly. Participants with higher WWI had lower education and income levels, higher smoking rates, higher use of hormone and lower cholesterol medication, greater dietary inflammatory potential, a greater history of diabetes, high blood pressure, cancer, and fractures, as well as higher cholesterol levels and lower BMD (Table 1).
Association between WWI and BMD
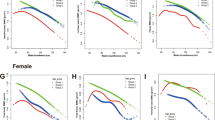
The associations between WWI and BMD are presented in Table 2. In the crude and adjusted models, WWI was negatively correlated with BMD at all four sites. Thank you for your clarification. We appreciate your attention to detail and recognize the importance of conveying our findings clearly. In the fully adjusted model, each one-unit increase in WWI was associated with a decrease in BMD, measured in g/cm2, at all four sites. Specifically, we observed a decrease of 0.03 g/cm2 in lumbar BMD, 0.04 g/cm2 in pelvis BMD, 0.02 g/cm2 in femoral neck BMD, and 0.02 g/cm2 in total BMD. When comparing those in the highest quartile of WWI to those in the lowest quartile, we observed decreases in lumbar, pelvis, femoral neck, and total BMD by 0.08 g/cm2, 0.06 g/cm2, 0.03 g/cm2, and 0.05 g/cm2, respectively. Hexbin plots showing the relationship between the WWI and various bone mineral densities (Fig. 2). Smoothed curve fitting findings confirmed the nonlinear negative connection between WWI and BMD at all four sites (Fig. 3).
Hexbin Plots of weight-adjusted waist index and various bone mineral densities. Each subplot represents a different bone mineral density: Lumbar BMD (top left), Pelvis BMD (top right), Femoral Neck BMD (bottom left), and Total BMD (bottom right). The color of each hexbin represents the number of data points within that area, with darker colors indicating a higher count. Note that due to missing values in the dataset, not all potential data points are shown
The nonlinear associations between weight-adjusted waist index and bone mineral density. The solid line represents the smooth curve fit between variables. Blue bands represent the 95% of confidence interval from the fit. A WWI and lumbar BMD; B WWI and pelvis BMD; C WWI and femoral neck BMD; D WWI and total BMD. WWI, weight-adjusted waist index; BMD, bone mineral density
The relationship between WWI and BMD at all four sites was inconsistent across subgroups, as presented in Table 3. The association between WWI and BMD differed significantly across different genders at the total BMD site (P for interaction = 0.016), but did not show significant difference at the lumbar, pelvis, and femoral neck BMD sites (P for interaction > 0.05). The negative correlation between WWI and BMD was constant across different education levels at all sites (P for interaction > 0.05). In the subgroups of race/ethnicity, the associations between WWI and BMD did not show a statistically significant interaction at any of the sites (P for interaction > 0.05). The correlation varied in the subgroups of high blood pressure, with a significant interaction observed at the lumbar BMD site (P for interaction = 0.040) and total BMD site (P for interaction = 0.050), but no significant interaction at the pelvis and femoral neck BMD sites (P for interaction > 0.05). In the diabetes subgroups, the associations between WWI and BMD did not differ significantly at any of the sites (P for interaction > 0.05).
Discussion
In our cross-sectional study, which enrolled 40,568 eligible participants, we observed a negative association between WWI and BMD. Interestingly, there was a significant gender dependence on this association, indicating that a higher WWI may lead to a decrease in BMD among U.S. adults. These findings suggest that managing visceral fat distribution is important for bone metabolism.
This research is the first to examine the connection between BMD and WWI. Obesity and being overweight have always been seen as protective factors. BMI and BMD have a favorable correlation that has been shown in several research dating back at least 20 years [28, 29]. Researchers found that BMI, particularly in gender-specific populations and groups of menopausal women, decreased the incidence of bone loss and fractures [30, 31]. However, as a consequence of epidemiological research that refutes this idea, there has been a paradigm shift regarding obesity as a protective factor for osteoporotic fractures [32].
Numerous research has discovered nonlinear relationships and saturation effects between BMI and BMD in individuals of all ages, sexes, and ethnic backgrounds as a result of improvements in research methodology. These findings demonstrate that a simple linear positive correlation cannot adequately capture the relationship between BMI and BMD [8, 20, 33]. Additionally, research from various nations and locations has revealed considerable variations in BMI and fracture risk at various sites [34,35,36]. A prospective research of more than 800,000 middle-aged and older Spanish women, for instance, revealed that obesity reduced the risk of hip and pelvic fractures but raised the risk of proximal humeral fracture by 30% relative to the population at large [37].
However, the majority of studies investigating the relationship between obesity and BMD use the BMI and WC to assess obesity and are unable to distinguish between muscle mass, fat mass, and fat distribution. However, research examining bone metabolism must take body composition into account. According to Gnudi et al., there is only a connection between BMD and muscle mass in women who do not have osteoporosis, highlighting the significance of differentiating between various forms of body mass [38]. The WWI anthropometric measure is thought to be a marker of both high-fat mass and low-muscle mass [39]. There is a less substantial “obesity paradox” in WWI in the relationship between traditional indicators and metabolic diseases [40]. According to the most recent research, the obesity paradox may not actually exist, but rather, it is caused by the BMI’s inability to discern between muscle mass and fat mass [41]. Recent epidemiological research reveals that when assessing obesity and other illnesses, WWI performs better than several traditional indicators [13, 41,42,43].
According to the findings of the subgroup analysis, there were variations in the relationships between WWI and BMD at various sites depending on subgroups of gender, age, and race. The relationships between bone metabolism and several contributing variables vary by gender and race [26, 44]. For instance, a recent cross-sectional study indicated that non-Hispanic black women had a substantially stronger negative connection between metal exposure and BMD than did other groups [25]. Although it is believed that the relationship between WWI and abdominal fat and muscle mass is more sex- and race-specific [18, 45], the considerable age disparities in the NHANES for assessing BMD at various locations may be the cause of the subgroup discrepancies.
Uncertainty exists regarding the fundamental causes of this adverse relationship between BMD and WWI. Visceral fat has different metabolic properties from subcutaneous fat, and pro-inflammatory cytokines can speed up bone resorption and negatively affect BMD [46]. Additionally, there is strong proof that mesenchymal stromal/stem cells (MSC) have a negative correlation with osteoblast and adipocyte commitment. The systemic linkages between peripheral adipose depots and trabecular and cortical bone might be mediated by the same mechanisms that regulate MSC development locally within the marrow microenvironment [47, 48].
The adoption of a complicated multi-stage random sampling strategy and a high sample size are two of our study’s strengths, since they boost the reliability and representativeness of our findings [49, 50]. However, there are some limitations to our study that must be noted. For starters, because to the cross-sectional design, we were unable to establish a causal relationship between WWI and BMD. Due to database constraints, we were unable to incorporate data on all factors that influence bone metabolism, such as menopause and medication usage. This was done in order to keep the sample size large enough. Despite these restrictions, the present association between WWI and BMD was steady enough that it was less likely to be considerably impacted by characteristics that were not included.
Conclusion
Our study provides new evidence for a complex link between obesity and bone metabolism, as we found a significant and negative association between WWI and BMD in US adults. This highlights the importance of managing visceral fat distribution in bone metabolism and sheds light on the limitations of using traditional obesity measurements, such as BMI and WC, to assess bone health.
Availability of data and materials
The survey data are publicly available on the internet for data users and researchers throughout the world ( www.cdc.gov/nchs/nhanes/ ).
Abbreviations
- WWI:
-
Weight-adjusted waist circumference index
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- LDL-C:
-
Low-density lipoprotein cholesterol
- PIR:
-
Income-to-Poverty Ratio
- MSC:
-
Mesenchymal stromal/stem cells
- RCS:
-
Restricted cubic spline
References
Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367(9527):2010–8.
Black DM, Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2016;374(3):254–62.
Xie R, Huang X, Zhang Y, Liu Q, Liu M. High low-density lipoprotein cholesterol levels are Associated with osteoporosis among adults 20–59 years of age. Int J Gen Med. 2022;15:2261–70.
Xie R, Huang X, Liu Q, Liu M. Positive association between high-density lipoprotein cholesterol and bone mineral density in U.S. adults: the NHANES 2011–2018. J Orthop Surg Res. 2022;17(1):92.
Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399(10322):394–405.
Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, Mozaffarian D, Swinburn B, Ezzati M. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–40.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13–27.
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16(11):1330–8.
Compston JE, Flahive J, Hosmer DW, Watts NB, Siris ES, Silverman S, Saag KG, Roux C, Rossini M, Pfeilschifter J, et al. Relationship of weight, height, and body mass index with fracture risk at different sites in postmenopausal women: the global longitudinal study of osteoporosis in women (GLOW). J Bone Miner Res. 2014;29(2):487–93.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32(6):959–66.
Shieh A, Karlamangla AS, Karvonen-Guttierez C, Greendale GA. Menopause-related changes in body composition are associated with subsequent bone mineral density and fractures: Study of Women’s Health Across the Nation. J Bone Miner Res 2022.
Ma M, Liu X, Jia G, Geng B, Xia Y. The association between body fat distribution and bone mineral density: evidence from the US population. BMC Endocr Disord. 2022;22(1):170.
Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8(1):16753.
Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. 2021;50(3):780–6.
Zhang D, Shi W, Ding Z, Park J, Wu S, Zhang J. Association between weight-adjusted-waist index and heart failure: results from National Health and Nutrition Examination Survey 1999–2018. Front Cardiovasc Med. 2022;9:1069146.
Qin Z, Du D, Li Y, Chang K, Yang Q, Zhang Z, Liao R, Su B. The association between weight-adjusted-waist index and abdominal aortic calcification in adults aged ≥ 40 years: results from NHANES 2013–2014. Sci Rep. 2022;12(1):20354.
Cai S, Zhu T, Ding Y, Cheng B, Zhang A, Bao Q, Sun J, Li M, Liu X, Wang S. The relationship between the weight-adjusted-waist index and left ventricular hypertrophy in chinese hypertension adults. Hypertens Res. 2023;46(1):253–60.
Qin Z, Chang K, Yang Q, Yu Q, Liao R, Su B. The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: a population-based study. Front Nutr. 2022;9:941926.
Cai S, Zhou L, Zhang Y, Cheng B, Zhang A, Sun J, Li M, Su Y, Bao Q, Zhang Y, et al. Association of the weight-Adjusted-Waist Index with risk of all-cause mortality: a 10-Year Follow-Up study. Front Nutr. 2022;9:894686.
Xie R, Zhang Y, Yan T, Huang X, Xie S, Liu C, Liu M. Relationship between nonalcoholic fatty liver disease and bone mineral density in adolescents. Med (Baltim). 2022;101(41):e31164.
Xie R, Zhang Y. Is assessing the degree of hepatic steatosis and fibrosis based on index calculations the best choice for epidemiological studies? Environ Pollut. 2023;317:120783.
Xie R, Zhang Y. Index-based calculation or transient elastography to assess the degree of hepatic steatosis and fibrosis. J Nutr. 2023;153(3):909.
Zierfuss B, Höbaus C, Herz CT, Pesau G, Koppensteiner R, Schernthaner GH. Predictive power of novel and established obesity indices for outcome in PAD during a five-year follow-up. Nutr Metab Cardiovasc Dis. 2020;30(7):1179–87.
Ouyang Y, Quan Y, Guo C, Xie S, Liu C, Huang X, Huang X, Chen Y, Xiao X, Ma N, et al. Saturation effect of body Mass Index on Bone Mineral density in adolescents of different Ages: a Population-Based study. Front Endocrinol (Lausanne). 2022;13:922903.
Xie R, Liu Y, Wang J, Zhang C, Xiao M, Liu M, Zhang Y. Race and Gender Differences in the Associations Between Cadmium Exposure and Bone Mineral Density in US Adults. Biol Trace Elem Res. 2023;201(9):4254–61.
Xie R, Zhang Y. Association between 19 dietary fatty acids intake and rheumatoid arthritis: Results of a nationwide survey. Prostaglandins Leukot Essent Fatty Acids. 2023;188:102530.
Xie R, Zhang Y. Associations between dietary flavonoid intake with hepatic steatosis and fibrosis quantified by VCTE: Evidence from NHANES and FNDDS. Nutr Metab Cardiovasc Dis. 2023;33(6):1179–89.
Khosla S, Atkinson EJ, Riggs BL, Melton LJ. 3rd: relationship between body composition and bone mass in women. J Bone Miner Res. 1996;11(6):857–63.
Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res. 1993;8(5):567–73.
Paganini-Hill A, Chao A, Ross RK, Henderson BE. Exercise and other factors in the prevention of hip fracture: the Leisure World study. Epidemiology. 1991;2(1):16–25.
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of osteoporotic fractures Research Group. N Engl J Med. 1995;332(12):767–73.
Piñar-Gutierrez A, García-Fontana C, García-Fontana B, Muñoz-Torres M. Obesity and bone health: a complex relationship. Int J Mol Sci. 2022;23(15):8303–23.
Xie R, Liu M. Relationship between non-alcoholic fatty liver disease and degree of hepatic steatosis and bone Mineral Density. Front Endocrinol (Lausanne). 2022;13:857110.
Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z. Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women’s health initiative-observational study. J Bone Miner Res. 2009;24(8):1369–79.
Premaor MO, Pilbrow L, Tonkin C, Parker RA, Compston J. Obesity and fractures in postmenopausal women. J Bone Miner Res. 2010;25(2):292–7.
Compston JE, Watts NB, Chapurlat R, Cooper C, Boonen S, Greenspan S, Pfeilschifter J, Silverman S, Díez-Pérez A, Lindsay R, et al. Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med. 2011;124(11):1043–50.
Prieto-Alhambra D, Premaor MO, Fina Avilés F, Hermosilla E, Martinez-Laguna D, Carbonell-Abella C, Nogués X, Compston JE, Díez-Pérez A. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res. 2012;27(2):294–300.
Gnudi S, Sitta E, Lisi L. Relationship of body mass index with main limb fragility fractures in postmenopausal women. J Bone Miner Metab. 2009;27(4):479–84.
Zhao P, Shi W, Shi Y, Xiong Y, Ding C, Song X, Qiu G, Li J, Zhou W, Yu C, et al. Positive association between weight-adjusted-waist index and hyperuricemia in patients with hypertension: the China H-type hypertension registry study. Front Endocrinol (Lausanne). 2022;13:1007557.
Fassio A, Idolazzi L, Rossini M, Gatti D, Adami G, Giollo A, Viapiana O. The obesity paradox and osteoporosis. Eat Weight Disord. 2018;23(3):293–302.
Kim JE, Choi J, Kim M, Won CW. Assessment of existing anthropometric indices for screening sarcopenic obesity in older adults. Br J Nutr. 2022;(129):1–13.
Li Q, Qie R, Qin P, Zhang D, Guo C, Zhou Q, Tian G, Liu D, Chen X, Liu L, et al. Association of weight-adjusted-waist index with incident hypertension: the rural chinese cohort study. Nutr Metab Cardiovasc Dis. 2020;30(10):1732–41.
Ding C, Shi Y, Li J, Li M, Hu L, Rao J, Liu L, Zhao P, Xie C, Zhan B, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: a prospective cohort study. Nutr Metab Cardiovasc Dis. 2022;32(5):1210–7.
Ning HT, Du Y, Zhao LJ, Tian Q, Feng H, Deng HW. Racial and gender differences in the relationship between sarcopenia and bone mineral density among older adults. Osteoporos Int. 2021;32(5):841–51.
Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH. Associations between Weight-Adjusted Waist Index and Abdominal Fat and muscle Mass: multi-ethnic study of atherosclerosis. Diabetes Metab J. 2022;46(5):747–55.
Morley JE, Baumgartner RN. Cytokine-related aging process. J Gerontol A Biol Sci Med Sci. 2004;59(9):M924–929.
Gimble JM, Zvonic S, Floyd ZE, Kassem M, Nuttall ME. Playing with bone and fat. J Cell Biochem. 2006;98(2):251–66.
Katzmarzyk PT, Barreira TV, Harrington DM, Staiano AE, Heymsfield SB, Gimble JM. Relationship between abdominal fat and bone mineral density in white and african american adults. Bone. 2012;50(2):576–9.
Xie R, Ning Z, Xiao M, Li L, Liu M, Zhang Y. Dietary inflammatory potential and biological aging among US adults: a population-based study. Aging Clin Exp Res. 2023;35(6):1273–81.
Xie R, Liu X, Wu H, Liu M, Zhang Y. Associations between systemic immune-inflammation index and abdominal aortic calcification: Results of a nationwide survey. Nutr Metab Cardiovasc Dis. 2023;33(7):1437–43.
Acknowledgements
We would like to thank all participants in this study.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
YZ, HW, XL, [CL]2 and RX designed the research. YZ, HW, [CL]1, ML, XL, and RX collected, analyzed the data, and drafted the manuscript. XL, QY and RX revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The portions of this study involving human participants, human materials, or human data were conducted in accordance with the Declaration of Helsinki and were approved by the National Center for Health Statistics (NCHS) Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Y., Wu, H., Li, C. et al. Associations between weight-adjusted waist index and bone mineral density: results of a nationwide survey. BMC Endocr Disord 23, 162 (2023). https://doi.org/10.1186/s12902-023-01418-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01418-y