Abstract
Background
Osteoporosis is a prevalent condition characterized by low bone density and increased risk of fractures, resulting in a significant healthcare burden. Previous research has suggested that serum ferritin levels may be related to the risk of developing osteoporosis. The aim of this study was to investigate the relationship between dietary iron intake and the development of osteoporosis.
Methods
Using data from the National Health and Nutrition Examination Survey (NHANES) conducted between 2005 and 2018, a total of 11,690 adults aged over 20 were evaluated. Bone mineral density (BMD) measurements of the femoral neck and lumbar spine were used to assess osteoporosis and osteopenia. Dietary iron intake was determined using food intake interviews and the Food and Nutrient Database for Dietary Studies. Logistic regression models were applied to investigate the association between dietary iron consumption and osteopenia and osteoporosis.
Results
After adjusting for sociodemographic factors, compared with those who had the first quartile (Q1) of dietary iron intake, the odds ratio (OR) for osteopenia across the quartiles of dietary iron intake levels was 0.88 (95%CI: 0.79–0.98), 0.80 (95%CI: 0.72–0.89), and 0.74 (95%CI: 0.67–0.83) for Q2, Q3, and Q4, respectively. And the OR for osteoporosis across the quartiles of dietary iron intake levels was 1.00, 0.77 (95%CI: 0.50–1.19), 0.54 (95%CI: 0.34–0.89), and 0.83 (95%CI: 0.54–1.29) for Q1, Q2, Q3, and Q4, respectively. Notably, the observed association was significant among females but not males.
Conclusion
The risk of osteopenia/osteoporosis in females decreases with a moderate increase in dietary iron consumption. For females to preserve bone health, moderately increasing their dietary iron intake without overindulging should be seen as a key approach. Our study provides useful insights for developing dietary strategies to prevent and manage osteoporosis in vulnerable populations.
Similar content being viewed by others
Background
Osteoporosis, a systemic bone disease characterized by osteopenia and bone microstructure deterioration, has emerged as a significant public health concern in the middle-aged and elderly population due to the aging of the population [1, 2]. The prevalence of osteoporosis increases with age, affecting 36% of Chinese people over the age of 60, with higher rates among women (49%) than men (23%) [3]. Osteoporosis-related fractures are common among people aged over 50 years old, with 50% of females and 20% of males suffering from such fractures [3]. These fractures have a substantial impact on patients’ quality of life, resulting in disability and even mortality. One-year mortality rates following hip fractures have been reported to be as high as 20%, with approximately 50% of patients becoming disabled [4]. The economic burden of fractures is also substantial, with medical expenditures for fractures in China totaling $10.2 billion in 2010 and expected to reach $275 billion by 2050 [5].
Diet plays a crucial role in preserving bone mass and maintaining bone health throughout life, as the bone is an active and dynamic tissue that requires adequate nutrients during remodeling and mineralization [6, 7]. Dietary nutrients, such as protein, vitamin D, and calcium, have been shown to affect bone remodeling regulation [8], while micronutrients such as iron and zinc are associated with bone homeostasis [9]. Iron deficiency has been identified as an important factor affecting bone health, with plasma iron levels found to be associated with the risk of osteoporosis in a U-shaped exposure-response relationship [10]. In addition to plasma iron levels, studies have also demonstrated that both iron excess and a lack of iron in the diet can harm bone mass and mineral content [11,12,13]. Iron deficiency may impact bone health by affecting vitamin D metabolism and collagen synthesis, and iron overload suppresses osteoblast proliferation and differentiation while promoting osteoclast differentiation [14, 15].
Despite the potential importance of iron intake in maintaining bone health, research on the association between dietary iron consumption and adult osteoporosis is limited. Therefore, the aim of the current study is to investigate the relationship between dietary iron intake and osteopenia and osteoporosis in adults.
Methods
Study design and population
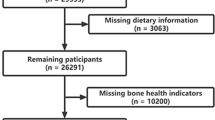
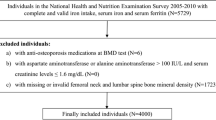
In the US, NHANES is an ongoing health examination study and nutritional status survey that includes adults and children. Initiating from 1998, five data components are included in the project: demographic, dietary, examination, laboratory, and questionnaire. Participants were interviewed at home, and examinations and laboratory tests were conducted at mobile examination centers. The continuous NHANES survey design can be found at http://www.cdc.gov/nchs/nhanes/index.htm. Informed consent was obtained from all participants before data collection by the ethics review board of the National Center for Health Statistics. Seven survey cycles were used in the present study (2005–2006, 2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, 2017–2018). Collectively, there were 70,190 participants in the pooled cycles. Participants with missing values for dietary iron intake and/or osteopenia/osteoporosis, or aged < 20 years, were removed from the sample pool. The final sample for multiple cross-sectional analyses comprised 11,690 participants.
Assessment of osteopenia and osteoporosis
The osteopenia was assessed via bone mineral density (BMD) measurement for the femoral neck and lumbar spine. Firstly, all data for BMD were standardized for eliminating bias from units. Secondly, osteopenia was defined as BMD of femoral neck lower than − 1 and greater than − 2.5, and BMD of lumbar spine lower than − 1 and great than − 2.5. Thirdly, osteoporosis was detected while BMD of the femoral neck or lumbar spine was lower than − 2.5 [16].
Assessment of dietary iron intake
NHANES interviewed food intake on two non-consecutive days, the first in person and the second by telephone. Due to the much missing in the second-wave interview, we used the first-wave food intake in this analysis, and an estimation of dietary iron-nutrient was made using the Food and Nutrient Database for Dietary Studies published by the United States Department of Agriculture [17].
Covariates
The confirmed age was recorded at the time of screening. Sex was dichotomized into male and female. Covariates definition refers to the previous study [18]. Races were grouped into Mexican American, non-Hispanic Black, non-Hispanic White, other Hispanic, and other race. Educational attainment was divided as less than high school, high school, and above high school. The ratio of family income to poverty was an income index estimated household socioeconomic status, which was graded as < 1.5, 1.5–3.5, or > 3.5 [19]. Alcohol intake was defined as mild, moderate, and heavy [20, 21]. Heavy alcohol use was defined as ≥ 3 drinks per day for females or ≥ 4 drinks per day for males, or binge drinking on five or more days per month. Moderate alcohol use was defined as ≥ 2 drinks per day for females and ≥ 3 drinks per day for males, or binge drinking ≥ 2 days per month. Mild alcohol use was regarded as others. Smoking status was defined as never, former, and current. Never smokers were those who smoked < 100 cigarettes in their lifetime; former smokers smoked > 100 cigarettes in their lifetime but currently did not smoke at all, and current smokers smoked > 100 cigarettes in their lifetime and currently smoked some days or every day. Cardiovascular disease (CVD) was defined as a report of CVD diagnosed by a physician, or taking anti-CVD medicine. Physical activity level was calculated using the metabolic equivalent (MET, min/week) [22]. The body mass index (BMI) was classified as underweight (< 20 kg/m2), normal (≥ 20 kg/m2 to < 25 kg/m2), overweight (≥ 25 kg/m2 to < 30 kg/m2), and obese (≥ 30 kg/m2) [23]. Diabetes mellitus was defined as reporting a diabetes diagnosis, glycohemoglobin HbA1c (%) > 6.5, or fasting glucose (mmol/L) ≥ 7.0, random blood glucose (mmol/L) ≥ 11.1, two-hour OGTT blood glucose (mmol/L) ≥ 11.1, or use of diabetes medication or insulin [24].
Statistical analysis
The mean dietary iron intake was grouped into quartiles from the lowest (first quartile, Q1) to the highest (fourth quartile, Q4). We summarized continuous variables by means and standard deviations and categorical variables with numbers and proportions. Analyzing data for normally distributed data using one-way ANOVA and categorical data using Chi-square tests determined differences among quartiles in dietary iron intake. To account for oversampling and non-responses, a seven-cycle sample weight (2005–2018) was used. Using tutorials on the NHANES website, we defined primary sample units and strata based on complex multistage probability sampling. An analysis of the associations between dietary iron intake quartiles and osteopenia or osteoporosis was conducted using three logistic regression models. Model 1 was no covariate; Model 2 was adjusted for age, sex, race, education, the ratio of family income to poverty, educational level, alcohol intake, smoking status, and MET. Model 3 was further adjusted for cardiovascular disease, BMI, and diabetes. Odds ratio (OR) and 95% confidence interval (CI) were used to assess the strength of the association.
Additionally, some additional analyses were conducted. As a first step, dietary iron intake was included as continuous variables in three logistic models with osteopenia and osteoporosis, not as quartiles. The second step was to perform interactive analyses with osteopenia and osteoporosis stratified by sex, races, education, alcohol intake, smoking status, the ratio of family poverty, CVD, and diabetes. Statistical analyses were conducted using STATA software (Version 17, Stata Corporation). Two-tailed P < 0.05 was defined as the significant threshold.
Results
There were 11,690 participants included in the final analysis across the quartiles of dietary iron intake levels, as shown in Table 1. Participants in the Q4 group tended to be younger, male, non-Hispanic White, above high school attainment, mild alcohol consumption, never smokers, overweight, with highest MET levels, the ratio of family income to poverty > 3.5, no diabetes, and cardiovascular disease, no osteopenia, and osteoporosis. There was a significant difference among the dietary iron intake quartiles in terms of age, sex, education, race, alcohol intake, smoking status, BMI, the MET, the ratio of family income to poverty, diabetes, osteopenia and osteoporosis except for CVD (P < 0.05).
High dietary iron intake levels were negatively associated with osteopenia in the null model, and the OR for osteopenia across the quartiles of dietary iron intake levels was 1.00, 0.88 (95%CI: 0.79–0.98), 0.80 (95%CI: 0.72–0.89), and 0.74 (95%CI: 0.67–0.83) for Q1, Q2, Q3, and Q4, respectively. After adjusting for demographic variables, the association was not significantly changed, and the OR of the dietary iron intake level quartiles was 1.00, 0.77 (95% CI: 0.64–0.93), 0.74 (95% CI: 0.61–0.89), and 0.79 (95% CI: 0.65–0.95) for Q1, Q2, Q3, and Q4, respectively. In the full mode, after further adjusting for CVD, BMI, and diabetes, the OR for osteopenia across the dietary iron intake level quartiles were 1.00, 0.78 (95%CI: 0.65–0.95), 0.75 (95%CI: 0.62–0.91), and 0.78 (95%CI: 0.65–0.95) for Q1, Q2, Q3, and Q4, respectively (Table 2). In the full model, the mean dietary iron intake was associated with a lower risk of osteopenia (OR 0.99, 95%CI: 0.98–0.99). A significant linear association was found between the quartiles of dietary iron intake levels and osteopenia (P for trend < 0.001) (Table 2). No significant moderating effect was found in the subgroup analysis stratified by sex, race, education, alcohol intake, smoking status, the ratio of family income to poverty, CVD, and diabetes (P > 0.05) (Table 3).
High dietary iron intake levels had a close reverse relation with osteoporosis in quartile 3 not quartile 4 in the full model, and the OR for osteoporosis across the quartiles of dietary iron intake levels was 1.00, 0.77 (95%CI: 0.50–1.19), 0.54 (95%CI: 0.34–0.89), and 0.83 (95%CI: 0.54–1.29) for Q1, Q2, Q3, and Q4, respectively. Stratification analyses by gender showed that the association was significant in women, but not men. Additionally, the mean dietary iron intake was not associated with the occurrence of osteoporosis in the final model (OR 0.99, 95%CI: 0.97–1.01) (Table 4). There was no significant between-group difference in dietary iron intake quartiles in the subgroup analysis stratified by races, education, alcohol intake, smoking status, the ratio of family income to poverty, CVD, and diabetes (P > 0.05) (Table 5).
Discussion
In this national prospective cohort study, we found a significant association between dietary iron intake and the risk of osteopenia/osteoporosis. Specifically, we observed a U-shaped relationship between dietary iron intake and decreased osteoporosis risk, which was independent of sociodemographic factors. Our findings highlight the importance of considering dietary iron intake as a potential preventive factor for osteopenia/osteoporosis .
The effects of diet on bone cells can be divided into pro-anabolic effects, which promote bone formation, and anti-catabolic effects, which inhibit bone resorption [25, 26].Pro-anabolic effects can be achieved through the intake of nutrients that support bone formation. For example, calcium, vitamin D, and phosphorus are essential for bone mineralization, while protein and amino acids provide the building blocks for bone tissue[27]. In addition, certain micronutrients such as magnesium, zinc, and copper are important cofactors in bone formation [28]. Anti-catabolic effects can be achieved through the intake of nutrients that inhibit bone resorption. For example, vitamin K has been shown to reduce the activity of osteoclasts, the cells responsible for bone resorption [29]. Similarly, certain phytoestrogens found in soy and other plants have been shown to inhibit osteoclast activity and promote bone formation [30]. Conversely, excessive intake of caffeine, alcohol, and sodium can lead to increased calcium excretion and bone loss [31].
Although there have been some investigations into the correlation between dietary micronutrients and osteoporosis, limited research has been conducted on the association between iron intake and osteoporosis, particularly in healthy adults. A U-shaped relationship between iron intake and osteoporosis, which is consistent with previous animal studies [32]. Population studies have discovered that excessive iron intake or iron metabolism-related diseases (e.g., hemochromatosis) can lead to reduced BMD [19, 33]. Iron deficiency anemia is positively related to BMD and an increased risk of osteoporosis and fractures [34]. Our research demonstrates that adequate iron intake is linked to a lower risk of osteoporosis in the healthy population. Even in those who have already had a fragility fracture, osteoporosis may be preventable and treated, and the moderate physical activity can significantly lower the risk of fracture and refracture [35]. Early screening, identification of populations at high risk for osteopenia, and prompt preventive action are all part of good public health practice. Our research indicates that increasing dietary iron intake is a useful strategy, but caution should be exercised to avoid excessive consuming.
The results of our study hold significant implications for public health. While the existing literature on dietary iron consumption in the general population remains limited, the relationship between iron levels in the blood and bone mineral density (BMD) has been extensively investigated. The association between serum ferritin and BMD in healthy individuals has yielded controversial findings. For example, one study found a positive correlation between serum ferritin and BMD in elderly men, but not women [36], while another study found an inverse correlation between BMD and either ferritin saturation or transferring in women over the age of 45, but not men [37]. In contrast to males, women’s dietary iron consumption was associated with osteoporosis/osteopenia at certain levels, according to our study. Women appear to be more susceptible to osteoporosis/osteopenia than males; for instance, osteoporosis is thought to afflict one-third of postmenopausal women globally, and women with osteopenia have a 1.8-fold higher chance of breaking a bone than do healthy women [38, 39]. To more accurately identify postmenopausal women with low BMD and to provide targeted recommendations for increasing dietary iron intake to replenish the iron loss in the body and reduce the risk of osteoporosis, additional biomarkers are necessary.
There are several mechanisms that could explain the association between iron intake and osteoporosis/osteopenia. Iron deficiency can negatively affect bone health by impairing bone, protein production and vitamin D metabolism. Iron is involved in the activation of the cytochrome P450 family and the catalysis of prolyl-4-hydroxylase and lysyl-hydroxylase, which are necessary for collagen synthesis [40, 41]. Collagen makes up approximately 90% of the protein in bone tissue, and hydroxylation of proline in pro-collagen is crucial for its synthesis [42,43,44]. Additionally, vitamin D plays a crucial role in maintaining bone health by enhancing calcium absorption in the stomach and maintaining the equilibrium of serum calcium and phosphate concentrations. The cytochrome P450 family is responsible for mediating and regulating these actions [45, 46]. Iron overload, on the other hand, has been found to promote osteoclast differentiation while impairing osteoblast proliferation and differentiation, thus leading to a decline in bone density [13, 15, 47]. In addition, the process of bone remodeling involves a close communication between osteoclasts and osteoblasts, which is regulated by intricate autocrine and paracrine mechanisms involving various regulatory proteins [48]. Previous mouse model suggested that iron overload has the potential to adversely affect the bone marrow microenvironment, leading to a decrease in both the quantity and quality of mesenchymal stem cells [49]. Another population study demonstrated that excessive iron accumulation can harm hematopoiesis by damaging both hematopoietic cells and the microenvironment in which they function. This process is facilitated by signaling proteins that are associated with ROS [50]. The above evidence provides important proof of the role of dietary iron intake in bone development and remodeling.
There were some strengths in the current study. Firstly, this study comprehensively assessed dietary iron intake. Firstly, our study comprehensively assessed dietary iron intake, which was estimated using the Food and Nutrient Database for Dietary Studies published by the United States Department of Agriculture. This database provides a reliable source of dietary intake data for the US population, and allowed us to evaluate the associations between iron intake and osteoporosis in a more precise and accurate manner. Secondly, the large sample size of our national study provided sufficient power to perform subgroup analyses, and allowed us to explore the potential differences in the association between iron intake and osteoporosis across different subpopulations. Thirdly, our study included participants over 20 years old, which is more applicable to health populations, compared with the research that focuses only on the elderly and postmenopausal women.
However, our study also has certain limitations that should be taken into consideration when interpreting our results. Firstly, the cross-sectional study design restricts our ability to establish causal associations between dietary iron intake and osteoporosis. Secondly, the dietary iron is the only micronutrient we included in all dietary intakes. It may be difficult to examine the synergistic effects of many nutrients. Thirdly, some covariates were self-reported, which might introduce recall error and affect the accuracy of our results. Finally, some potential covariates, such as genetic factors, Vitamin D, and blood iron levels, were not included in this study, which may affect the interpretation of our findings. Further longitudinal research is needed to confirm and extend our findings, and to address these limitations.
Conclusion
In summary, moderate increases in dietary iron intake without overconsumption were substantially associated with a lower risk of osteopenia/osteoporosis in women. This study highlights the essential role of dietary iron intake in osteoporosis among women. To increase or maintain bone mass and reduce the risk of osteoporosis, public health and clinical interventions should take into account moderate increasing dietary iron intake without overconsumption as an important strategy for the individual and population levels.
Data Availability
The data presented in this study are from publicly available data in NHANES (website: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm).
References
Jandu J, et al. Osteopenia - StatPearls - NCBI Bookshelf. NCBI Bookshelf- StatPearls; 2020.
Xu W et al. Risk of osteoporosis and fracture after hysterectomies without oophorectomies: a systematic review and pooled analysis 2022: p. 1–10.
Liying HE et al. The prevalence rate of osteoporosis in the elderly in China between 2010 and 2016:a metaanalysis of single rate. 2016.
Lahtinen A et al. No major differences in recovery after hip fracture between Home-Dwelling Female and male patients. 2020. 109(3): p. 250–64.
Si L et al. Projection of osteoporosis-related fractures and costs in China: 2010–2050 2015.
Moran JM. Nutrition and Women’s Bone Health. Nutrients, 2022. 14(4).
Knurick JR, et al. Comparison of correlates of bone mineral density in individuals adhering to lacto-ovo, vegan, or omnivore diets: a cross-sectional investigation. Nutrients. 2015;7(5):3416–26.
Reed JA et al. Comparative changes in radial-bone density of elderly female lacto-ovovegetarians and omnivores. 1994. 59(5 Suppl): p. 1197S.
Ann R, J.T.A.J.o.C M, Nutrition. Bone nutrients for vegetarians. 2014;100(1S):469S–75.
Yan C, et al. Research Progress of Ferroptosis Regulatory Network and Bone remodeling in osteoporosis. Front Public Health. 2022;10:910675.
Katsumata SI et al. Dietary Iron Deficiency decreases serum osteocalcin concentration and bone Mineral density in rats. 2006. 70(10): p. 2547–50.
Denis et al. Iron Deficiency negatively affects vertebrae and femurs of rats independently of Energy Intake and Body Weight1. 2004. 134(11): p. 3061–7.
Katsumata SI, et al. Severe iron deficiency decreases both bone formation and bone resorption in rats. 2009;139(2):238–43.
Jia P et al. Ferric ion could facilitate osteoclast differentiation and bone resorption through the production of reactive oxygen species. 2012. 30(11): p. 1843–52.
Doyard M et al. Iron excess limits HHIPL-2 gene expression and decreases osteoblastic activity in human MG-63 cells. 2012. 23(10): p. 2435–45.
Bone Mass Measurement: What the Numbers Mean. 2022; Available from: https://www.bones.nih.gov/health-info/bone/bone-health/bone-mass-measure.
Ahluwalia N et al. update on nhanes dietary data: focus on collection, release, analytical considerations, and uses to inform public policy 1,2
You Y, et al. The association between sedentary behavior, exercise, and sleep disturbance: a mediation analysis of inflammatory biomarkers. Front Immunol. 2022;13:1080782.
Rahman HH et al. Association of albumin to creatinine ratio with urinary arsenic and metal exposure: evidence from NHANES 2015–2016 2022(54 – 6).
Naimi TS et al. Binge Drinking Among US Adults 2003. 289(1).
Phillips JA. Dietary guidelines for Americans, 2020–2025. Workplace Health Saf. 2021;69(8):395.
Ainsworth et al. Compendium of physical activities: classification of energy costs of human physical activities. 1993. 93(6): p. 710–0.
Seidell JC, et al. Obesity and fat distribution in relation to health -. Curr insights recommendations. 1987;50:57.
Association AD. Understanding A1c Diagnosis (2022). 2022 [cited 2022 26 Aug]; Available from: https://www.diabetes.org/diabetes/a1c/diagnosis.
Wang T, et al. Therapeutic potential and Outlook of Alternative Medicine for osteoporosis. Curr Drug Targets. 2017;18(9):1051–68.
He J, et al. Therapeutic anabolic and anticatabolic benefits of Natural Chinese Medicines for the treatment of osteoporosis. Front Pharmacol. 2019;10:1344.
Trautvetter U, et al. Effect of calcium phosphate and vitamin D(3) supplementation on bone remodelling and metabolism of calcium, phosphorus, magnesium and iron. Nutr J. 2014;13:6.
Mahdavi-Roshan M, Ebrahimi M, Ebrahimi A. Copper, magnesium, zinc and calcium status in osteopenic and osteoporotic post-menopausal women. Clin Cases Miner Bone Metab. 2015;12(1):18–21.
Alonso N, et al. Role of vitamin K in bone and muscle metabolism. Calcif Tissue Int. 2023;112(2):178–96.
Lisco G, et al. Endocrine, metabolic, and Immune Pathogenesis of Postmenopausal osteoporosis. Is there a therapeutic role in Natural Products? Endocr Metab Immune Disord Drug Targets; 2023.
Body JJ, et al. Non-pharmacological management of osteoporosis: a consensus of the belgian bone club. Osteoporos Int. 2011;22(11):2769–88.
Wei M, et al. Manganese, iron, copper, and selenium co-exposure and osteoporosis risk in chinese adults. J Trace Elem Med Biol. 2022;72:126989.
Guggenbuhl P et al. Bone mineral density in men with genetic hemochromatosis and HFE gene mutation. 2005. 16(12): p. 1809–14.
Pan ML et al. Iron Deficiency Anemia as a Risk Factor for Osteoporosis in Taiwan: A Nationwide Population-Based Study 2017(6).
Lorenc R, et al. Guidelines for the diagnosis and management of osteoporosis in Poland: Update 2017. Endokrynol Pol. 2017;68(5):604–9.
Lee KS et al. Serum ferritin levels are positively associated with bone mineral density in elderly Korean men: the 2008–2010 Korea National Health and Nutrition Examination Surveys 2014. 32(6).
Iron overload accelerates bone loss in healthy postmenopausal women and middle-aged men: a 3 year retrospective longitudinal study %J J Bone Miner Res. 2012. 27.
Organization WH. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992] 1994.
Siris ES, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National. Osteoporos Risk Assess. 2001;286(22):2815–22.
Toxqui L, Vaquero MP. Chronic iron deficiency as an emerging risk factor for osteoporosis: a hypothesis. Nutrients. 2015;7(4):2324–44.
Che J, et al. The Effect of Abnormal Iron Metabolism on Osteoporosis. 2020;195(2):353–65.
Vasta JD, Raines RT. Human collagen prolyl 4-Hydroxylase is activated by ligands for its Iron Center. Biochemistry. 2016;55(23):3224–33.
Suokas M, et al. Retrieval-independent localization of lysyl hydroxylase in the endoplasmic reticulum via a peptide fold in its iron-binding domain. Biochem J. 2003;370(Pt 3):913–20.
Shoulders M, R.T.J.A.R.o B, Raines. Collagen Struct Stab. 2010;78(1):929–58.
Wang P et al. The burgeoning role of cytochrome P450-mediated vitamin D metabolites against colorectal cancer. 2018. 133: p. 9–20.
Gil A, et al. Vitam D: Classic Novel Actions. 2018;72(2):87.
Wang et al. Iron overload increases osteoclastogenesis and aggravates the effects of ovariectomy on bone mass 2015.
Kular J, et al. An overview of the regulation of bone remodelling at the cellular level. Clin Biochem. 2012;45(12):863–73.
Zhang Y, et al. Effects of iron overload on the bone marrow microenvironment in mice. PLoS ONE. 2015;10(3):e0120219.
Lu W, et al. Free iron catalyzes oxidative damage to hematopoietic cells/mesenchymal stem cells in vitro and suppresses hematopoiesis in iron overload patients. Eur J Haematol. 2013;91(3):249–61.
Acknowledgements
Thanks to the National Health and Nutrition Examination Survey team for collecting and sharing original datasets.
Funding
None.
Author information
Authors and Affiliations
Contributions
XL writes the manuscript; XL and JJA revise and review the manuscript; JJA drafts the study design and supervises all process.
Corresponding author
Ethics declarations
Competing interests
All authors declare that they have no competing financial interests.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Review Board of National Center for Health Statistics and all participants provided written informed consent. All methods were performed in accordance with the relevant the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, X., An, J. Dietary iron intake and its impact on osteopenia/osteoporosis. BMC Endocr Disord 23, 154 (2023). https://doi.org/10.1186/s12902-023-01389-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-023-01389-0