Abstract
Background
Diabetes is a well-known risk factor for tuberculosis and poorly glycemic control may increase the risk of tuberculosis. We performed a meta-analysis to explore the association of glycemic control in diabetic patients and their tuberculosis prevalence.
Methods
We included observational studies that investigated the prevalence of tuberculosis associated with glycemic control. The markers of glycated hemoglobin A1c (HbA1c) and fasting plasma glucose were used to evaluate the exposure of interest in the study. We searched related articles in PubMed, EMBASE and Web of Science through 14 December 2019. The Newcastle-Ottawa scale was used to assess the risk of bias of included studies.
Results
Seventeen studies (four cohort studies, five case-control studies and eight cross-sectional studies) were included, involving 1,027,074 participants. The meta-analysis found the pooled odds ratio of prevalent tuberculosis increased a 2.05-fold (95%CI: 1.65, 2.55) for the patients with HbA1c ≥7.0% compared to those with HbA1c concentration < 7.0%. Furthermore, we found the mean of HbA1c was higher in the diabetes mellitus with tuberculosis group than the diabetes-only group (P = 0.002). In the sensitivity analysis, the finding remains consistent.
Conclusion
Our study provides the evidence that poorly controlled diabetes in diabetics may be associated with increased prevalence of tuberculosis. More efforts should focus on screening tuberculosis in uncontrolled diabetes.
Similar content being viewed by others
Background
Tuberculosis (TB) remains one of the most common infectious diseases in the world. The World Health Organization (WHO) has published that an estimated of approximately 10.0 million people fell ill with TB in 2019 from 202 countries and territories, suggesting a high burden of TB [1]. It is necessary to identify potential high-risk factors for TB screening. Besides HIV infection, poverty, undernutrition, and smoking, diabetes mellitus (DM) has received recent recognition as a risk factor for TB [2].
Epidemiological studies have elucidated the relationship of DM with the prevalence of TB disease [3,4,5]. In a recent systematic review among 13 observational studies, people with DM had about tripled the prevalence of developing TB than people without DM [3]. Additionally, in the two nationwide population-based studies, there was a higher underlying prevalence of tuberculosis infection at baseline in diabetics patients compared to the healthy population [4, 5]. One explanation for these results is that dysglycemia in diabetic patients may impair their innate immune system that seems to provide a favorable environment for acute intracellular bacterial infections in diabetic patients [6, 7]. Furthermore, the intracellular bacterial infections (e.g. TB) are one of the common complications of DM [8, 9]. Dysglycemia may be a key factor that impact the relationship of DM and TB.
A great number of studies have focused on the role of dysglycemia on the prevalence of TB [10,11,12,13,14]. Patients with poorly controlled diabetic are related to an increased prevalence of developing TB compared to those with controlled blood glucose [10,11,12]. In a cohort study of older individuals in China, DM subjects with baseline glycated hemoglobin A1c (HbA1c) ≥7% had higher prevalences of developing active pulmonary TB than patients with HbA1c < 7% (adjusted hazard ratio [HR]: 3.11) [10]. Similarly, Lin et al. showed that diabetics patients with poor glucose control were especially vulnerable to developing TB compared to the controlled DM [12]. However, there are inconsistent findings [13, 14]. The cohort study in U.K. by Pealing et al. indicated that patients with poorly controlled DM did not increase the prevalence of TB compared with diabetic patients with controlled glucose [13]. A case-control study in Denmark also reported that the level of HbA1c was not significantly related to the prevalence of TB [14]. Therefore, whether glycemic control mediates the relationship between DM and TB infection is unknown.
Considering the increasing prevalence of DM over time and greater susceptibility to infections [15], in the present study, we conducted a meta-analysis to examine the association between glycemic level and TB prevalence among patients with diabetes.
Methods
Search strategy and eligibility criteria
In the present study, we searched PubMed, Embase, and Web of Science to identify all relevant articles exploring the association of poor glycemic control and TB prevalence before December 14, 2019, without language restrictions. We searched the main keywords included “diabetes mellitus”, “DM”, “Glycated Hemoglobin A”, “hemoglobin A1c”, “HbA1c”, “fasting plasma glucose”, “FPG”, “glycemic control”, “Tuberculosis”, “TB”, and “mycobacterium”. Medical subject headings (MeSH) terms were used to efficiently search PubMed, and similar key words were used to search Embase and Web of Science. The search strategy for each database is available in the Additional file (Additional file 1).
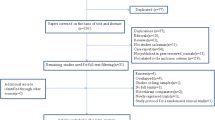
To include as many studies as possible, searches were not restricted by publication date or study type. We included articles that met the following three inclusion criteria: published up to December 14, 2019, published in English; included exposure of interest which evaluated glycaemia control status in diabetes patients; included outcome of interest which investigated the prevalence of pulmonary tuberculosis. We included the study that restricted to patients with diabetes only. Case reports, meeting abstracts, news items, articles without available comparison and outcome, articles not published in English, and articles exploring extrapulmonary tuberculosis were excluded. To evaluate the selection process, the study selection flowchart outlines records at each step (Fig. 1).
Data extraction and analysis
The value of HbA1c was used as a predictor for monitoring glycemic control in DM patients. Poor glycemic control was defined as HbA1c > 7% [16]. In addition, fasting plasma glucose (FPG) was also used as an interesting marker for reflecting impaired glucose regulation under basal conditions. We used a preconceived and standardized data extraction form to collect basic information on the first author’s name, year of publication, country, the recruitment period, study design, number of participants, outcomes of studies. The reported estimated effect (e.g., Relative Risk [RR], Odds Ratio [OR], Hazard Ratio [HR]) of the association between TB prevalence and poor diabetes control was obtained from the study. As counting data, we extracted the frequency of TB patients in each exposure group to calculate the odds ratio (or) and 95% confidence interval (CI). We also extracted the mean with standard deviation (SD) or median with inter-quartile range (IQR) to examine the distribution differences in the two groups of TB-DM and DM-only groups. Relevant citations were screened by two reviewers independently and disagreements were resolved through discussion.
A meta-analysis was performed to explore the effect of blood glucose levels-on TB in DM patients. First, HbA1c is the most commonly used index for reflecting blood glucose status. We examined the relationship between HbA1c and the prevalence of pulmonary TB in DM patients: grouped by HbA1c ≥ 7% and HbA1c < 7%; Then, HbA1c was taken as a continuous variable to observe the difference of its mean value between TB-DM group and DM only group; finally, we focused on the fasting blood glucose index, and explored the mean difference between the two groups (TB-DM group and simple DM group). The observed OR of TB among persons with various glycemic control within each study was presented in forest plots. Furthermore, we observed the mean difference in the two groups (TB-DM group vs. DM-only group). Relative risk of publication bias was evaluated by visual examination of funnel plots and assessed by Egger’s test. All statistical analyses were performed with Review Manager 5.3.
The quality of included study was assessed by using the Newcastle-Ottawa Scale for case-control study and cohort study in scientific research (Table S1). Newcastle-Ottawa Scale assigns a maximum of 9 stars (4 for selection of study population, 2 for comparability, 3 for robustness of outcome or exposure).
Results
Potentially 2252 relevant articles were identified through a comprehensive search of the databases. After removal of duplicates, 1637 articles were included. Full-text screening was performed in 49 potential eligible articles, of which 33 studies were excluded for various reasons mentioned in Fig. 1. Considering the related articles, seventeen studies (four cohort studies, five case-control studies and eight cross-sectional studies) including 1,027,074 participants met the eligibility criteria for the final review.
Baseline characteristics of the seventeen included studies are summarized in Tables 1-2. There were four cohort studies published between 2008 and 2019 in Asia. Three studies were conducted in general populations, and one was among the elderly. Study sample size of cohort studies ranged from 6444 to 819,051. Of the five case-control studies, four were conducted in high prevalence populations of developing countries. In regard of cross-sectional studies, the majority of study sample size were less than 700 (6 out of 8).
Results of quality assessment are listed in the appendix. The ascertainment of DM was mostly based on medical record in seven studies, and laboratory testing in one study. Similarly, the diagnosis of TB was based on medical record in seven studies, laboratory testing in one study, and self-reported in one study.
Glycated haemoglobin A1c
There were seven studies involved 20,857 participants to explore the relationship between glycemic control and TB [10, 11, 14, 17,18,19,20]. We conducted a meta-analysis to investigate the effect of poorly controlled glucose (HbA1c > 7.0%) on the prevalence of tuberculosis, and found that the pooled odds ratio of prevalent TB increased 2.05-fold (95%CI: 1.65–2.55) compared to good glycemic control (HbA1c < 7.0%) (Fig. 2). The crude OR from the observational studies revealed no substantial statistical heterogeneity (I2 = 18%, P = 0.29). Funnel plot was shown in Fig. 3. In the sensitivity analysis, we excluded the study (Leung 2008), which focused on the elderly, and found consistent results (Fig. S1).
Table 3 exhibits the distribution of HbA1c concentrations in DM-TB patients and DM-only patients. Ten studies were included, and an increasing trend between non-DM and DM patients was observed in regard to their mean or median HbA1c concentrations [9, 14, 19,20,21,22,23,24,25,26]. Furthermore, there was a statistically significant difference in HbA1c concentrations between the two groups, and the mean of HbA1c was higher in the DM-TB than the DM-only group (P = 0.002, Fig. 4). Effect estimates were heterogeneous within studies (I2 = 81%, P < 0.0001). Then we restricted our study to the case-control studies, and observed consistent results. The funnel plot of the mean difference from three case-control studies revealed no statistical evidence of substantial heterogeneity (I2 = 34%, P = 0.22, Fig. S2).
Fasting plasma glucose
Table 4 lists the distribution of FPG concentrations in TB-DM group and DM group. The seven studies involved 656 TB-DM patients and 8127 DM patient from five countries [14, 18,19,20, 22,23,24]. In statistical analysis, we focused on the fasting blood glucose index to explore the distribution of fasting blood glucose concentrations in TB-DM group and DM group. Due to the small sample sizes and the skewed data, means and medians can be very different from each other, so only means were used for meta-analyses. Therefore, we further conducted analysis in four articles for meta-analysis to explore the difference of mean FPG concentrations in the two groups (Fig. 5). The statistical analysis showed similar levels of FPG between TB-DM and DM-only groups (P = 0.26). There was significant heterogeneity of effect estimates, and 93% of the total variance among those studies. We further conducted analysis in case-control studies. The results showed no substantial statistical heterogeneity (I2 = 42%, P = 0.19), and observed significant difference in the two groups of TB-DM and DM-only patients (Fig. S3).
Discussion
In the present study, we conducted a meta-analysis that included seventeen studies and revealed that uncontrolled high levels of blood glucose of diabetic patients may be associated with an increased prevalence of tuberculosis. It suggests that tuberculosis screening among uncontrolled diabetic patients is necessary.
As the great burden of TB globally, it is important to identify potential high-prevalence populations appropriate for TB screening. Several studies have demonstrated that DM patients are at a greater risk for active TB disease, and poor glycemic control could also exacerbate this risk [10,11,12,13,14, 27]. As reported, 422 million people currently have diabetes, and 1.6 million deaths are directly attributed to diabetes each year (World Health Organization, Diabetes, https://www.who.int/health-topics/diabetes#tab=tab_1). The overlap between the diabetes and tuberculosis epidemics could adversely affect global tuberculosis control efforts. Then we conducted a meta-analysis to explore the relationship between uncontrolled DM and TB prevalence. Assessing glycemic control in DM patients, however, is still a challenge. Several recent approaches include the use of self-monitoring of blood glucose and HbA1c [16]. HbA1c testing was recommended as a simple and convenient method for evaluating average glycemia level over the preceding several months. In this study, we found the pooled odds ratio of prevalent tuberculosis increased a 2.05-fold (95%CI: 1.65, 2.55) for the patients with HbA1c ≥7.0% compared to those with HbA1c concentration < 7.0%. We also observed higher HbA1c levels in the TB-DM group compared to DM-only patients.
Glycated hemoglobin A1c is the product of glucose binding to hemoglobin in red blood cells. It is a gold standard for evaluating blood glucose control. Since most of the hemoglobin of human body exists in the red blood cell, which has a biological half-life of approximately 3–4 months. Thus, HbA1c concentrations reflects the controlling status of blood glucose over a relatively long-term peroid [28]. According to the American Diabetes Association (ADA) and the Canadian Diabetes Association (CDA) guidelines, HbA1c was accepted as an approved indicator for the assessment of glycemic control state in DM patients [29, 30]. In the present study, after evaluating plasma glucose levels through laboratory tests, there was a statistically significant difference in the mean of HbA1c between the two groups (TB-DM vs. DM-only group), suggesting these diabetics with poor glucose control may also have increased susceptibility to TB infection. Furthermore, diabetic patients with an HbA1c > 7.0 (%) had a twofold higher prevalence of TB than those with an HbA1c < 7.0 (%). Results of two studies reported that chronic hyperglycemia with HbA1c values of > 7%, had a 2.52–3.07 risk of developing pulmonary TB when compared with a group with better glycemic control [18, 20]. There are several possible explanations for the discrepancy. First, different tuberculin-skin-test thresholds are proposed for different countries and risk groups, which may affect the prevalence of tuberculosis. Moreover, tuberculosis are chronic wasting diseases and closely related to external factors, such as age, gender, BMI, nutrition, and contact history with binding patients. These factors may cause different results among a large number of existing studies, which also suggests that it is necessary for us to adopt a unified diagnosis and treatment standard to explore the relationship between glucose control and tuberculosis prevalence in a larger sample size meta-analysis or original literature.
Fasting plasma glucose is measured after overnight fasting or not eating anything for at least eight hours, which is the preferred method of screening test for DM in primary care. In the study, we included four studies for meta-analysis and found no statistically significant differences of FPG level between the DM-only group and TB-DM group. That may be due to the substantial statistical heterogeneity among studies. We further conducted analysis restricted to the two case-control studies. The results show no publication bias, and observed a high concentration of FPG in the TB-DM group. Consistent with previous studies, the strong association between heightened values of FPG and the prevalence of TB was claimed [31, 32]. In a Taiwanese cohort with five years of follow-up among 120,000 participants, Lee et al. reported 7.5% of incident TB could be attributed to poor glycemic control in the study population [32]. In the future, more researches are recommended to strengthen and explore the relationship between DM control and TB in the field.
The mechanisms that may underlie this association between TB infection and uncontrolled DM remain uncertain. Dysglycemia in DM patients was postulated to damage their innate or adaptive immunity and could trigger a hyperinflammatory state [26, 33]. It was reported that the synthesis of cytokines in pulmonary TB with DM patients shown significant changes compared to pulmonary TB without DM, such as IL-2, IL-6, IL-17, TNF-α and IFN-γ [34, 35]. In addition, Sanchez-Jimenez et al. showed the plasmatic increment of IL-15 could be related to the inflammatory state characteristic among DM and TB patients [24]. Further, a hyperinflammatory state of diabetic patients may favour the re-activation of TB [36, 37]. Despite of the potential association, policy on screening for TB infection among diabetic patients is not adopted by global health organizations [38]. The results of our study may provide more evidence that cost-effectiveness screening for tuberculosis in uncontrolled DM patients is needed and should be a high priority.
This study had some limitations. First, in the study, we pooled raw data to explore the prevalence of TB in uncontrolled DM patient. We could not control for potential confounding, such as alcohol consumption, nutrition, smoking status, and history of Bacillus Calmette-Guerin vaccination, diabetes duration [39], although we stratified by participant’s age in the sensitivity analysis. Second, most of studies that we have included are cross-sectional or case-control design, and as such we were unable to determine the temporal relationship between tuberculosis and diabetes. It restricts the popularization and application in this study. Moreover, it should be noted that the relationship between diabetes glycemic control and pulmonary tuberculosis may be complex or nonlinear, and more relevant studies are needed to explore. Third, the differences in the characteristics of the diabetes group and the control group, and different clinical evaluation markers for blood glucose control also bring difficulties to meta-analysis. There is need for well-designed prospective and larger studies in the future.
Conclusion
In conclusion, we revealed that uncontrolled high levels of blood glucose of diabetic patients might be especially vulnerable to developing tuberculosis. Our findings suggested that tuberculosis controls strategies should consider jointly targeting diabetes patients with poorly controlled glucose. We also recommended further studies for more thorough understanding of the relationship that could deliver a clear public health message.
Availability of data and materials
The data used in the analyses described in this study are available from the author (QL, liuqihust2016@126.com) on reasonable request.
Abbreviations
- HbA1c:
-
hemoglobin A1c
- CI:
-
confidence interval
- TB:
-
tuberculosis
- DM:
-
diabetes mellitus
- HR:
-
hazard ratio
- FPG:
-
fasting plasma glucose
- IQR:
-
inter-quartile range
- RR:
-
relative risk
- SD:
-
standard deviation
References
World Health Organization. Global tuberculosis report 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf. [Accessed 10 June 2021].
Hayashi S, Chandramohan D. Risk of active tuberculosis among people with diabetes mellitus: systematic review and meta-analysis [J]. Tropical Med Int Health. 2018;23(10):1058–70. https://doi.org/10.1111/tmi.13133.
Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies [J]. PLoS Med. 2008;5(7):e152. https://doi.org/10.1371/journal.pmed.0050152.
Dobler CC, Flack JR, Marks GB. Risk of tuberculosis among people with diabetes mellitus: an Australian nationwide cohort study [J]. BMJ Open. 2012;2(1):e666.
Ko PY, Lin SD, Tu ST, Hsieh MC, Su SL, Hsu SR, et al. High diabetes mellitus prevalence with increasing trend among newly-diagnosed tuberculosis patients in an Asian population: a nationwide population-based study. Prim Care Diabetes. 2016;10(2):148–55. https://doi.org/10.1016/j.pcd.2015.09.005.
Peleg AY, Weerarathna T, McCarthy JS, et al. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab Res Rev. 2007;23(1):3–13. https://doi.org/10.1002/dmrr.682.
Stegenga ME, van der Crabben SN, Blumer RM, et al. Hyperglycemia enhances coagulation and reduces neutrophil degranulation, whereas hyperinsulinemia inhibits fibrinolysis during human endotoxemia. BLOOD. 2008;112(1):82–9. https://doi.org/10.1182/blood-2007-11-121723.
Perez A, Brown HR, Restrepo BI. Association between tuberculosis and diabetes in the Mexican border and non-border regions of Texas. Am J Trop Med Hyg. 2006;74(4):604–11. https://doi.org/10.4269/ajtmh.2006.74.604.
Widjaja SS, Rusdiana, Savira M. CD4 and its relevance to advanced glycation end products in tuberculosis patients with co-morbidity diabetes. Open Access Maced J Med Sci. 2018;6(11):2115–8. https://doi.org/10.3889/oamjms.2018.347.
Leung CC, Lam TH, Chan WM, Yew WW, Ho KS, Leung GM, et al. Diabetic control and risk of tuberculosis: a cohort study. Am J Epidemiol. 2008;167(12):1486–94. https://doi.org/10.1093/aje/kwn075.
Leegaard A, Riis A, Kornum JB, Prahl JB, Thomsen VO, Sorensen HT, et al. Diabetes, glycemic control, and risk of tuberculosis: a population-based case-control study. Diabetes Care. 2011;34(12):2530–5. https://doi.org/10.2337/dc11-0902.
Lin C, Kuo S, Hsieh M, et al. Effect of diabetes mellitus on risk of latent TB infection in a high TB incidence area: a community-based study in Taiwan [J]. BMJ Open. 2019;9(10):e29948.
Pealing L, Wing K, Mathur R, et al. Risk of tuberculosis in patients with diabetes: Population based cohort study using the UK Clinical Practice Research Datalink. BMC Med. 2015;13:135. https://doi.org/10.1186/s12916-015-0381-9.
Kumpatla S, Sekar A, Achanta S, Sharath BN, Kumar AM, Harries AD, et al. Characteristics of patients with diabetes screened for tuberculosis in a tertiary care hospital in South India. Public Health Action. 2013;3(Suppl 1):S23–8. https://doi.org/10.5588/pha.13.0035.
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nat Rev Endocrinol. 2011;8(4):228–36. https://doi.org/10.1038/nrendo.2011.183.
Saudek CD, Derr RL, Kalyani RR. Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA. 2006;295(14):1688–97. https://doi.org/10.1001/jama.295.14.1688.
Almeida-Junior JL, Gil-Santana L, Oliveira CAM, et al. Glucose metabolism disorder is associated with pulmonary tuberculosis in individuals with respiratory symptoms from Brazil. PLoS One. 2016;11(4):e153590.
Berkowitz N, Okorie A, Goliath R, Levitt N, Wilkinson RJ, Oni T. The prevalence and determinants of active tuberculosis among diabetes patients in Cape Town, South Africa, a high HIV/TB burden setting. Diabetes Res Clin Pract. 2018;138:16–25. https://doi.org/10.1016/j.diabres.2018.01.018.
Marupuru S, Senapati P, Pathadka S, Miraj SS, Unnikrishnan MK, Manu MK. Protective effect of metformin against tuberculosis infections in diabetic patients: an observational study of south Indian tertiary healthcare facility. Braz J Infect Dis. 2017;21(3):312–6. https://doi.org/10.1016/j.bjid.2017.01.001.
Martínez-Aguilar G, Serrano CJ, Castañeda-Delgado JE, Macías-Segura N, Hernández-Delgadillo N, Enciso-Moreno L, et al. Associated risk factors for latent tuberculosis infection in subjects with diabetes. Arch Med Res. 2015;46(3):221–7. https://doi.org/10.1016/j.arcmed.2015.03.009.
Chan MW, Kow FP, Tang WS, et al. A cross sectional survey of pulmonary tuberculosis among elderly diabetics attending primary care clinics in Penang, Malaysia. Southeast Asian J Trop Med Public Health, 2019:50(2):325–34.
Khalil NH, Ramadan RA. Study of risk factors for pulmonary tuberculosis among diabetes mellitus patients. Egypt J Chest Dis Tuberc. 2016;65(4):817–23. https://doi.org/10.1016/j.ejcdt.2016.05.009.
Leal ML, Maciel ELN, Cade NV. Factors associated with tuberculosis in a population of diabetics: A case-control study. Cien Saude Colet. 2019;24(9):3247–56. https://doi.org/10.1590/1413-81232018249.30392017.
Sanchez-Jimenez R, Ceron E, Bernal-Alcantara D, et al. Association between IL-15 and insulin plasmatic concentrations in patients with pulmonary tuberculosis and type 2 diabetes. Tuberculosis (Edinb). 2018;111:114–20. https://doi.org/10.1016/j.tube.2018.06.009.
Webb EA, Hesseling AC, Schaaf HS, Gie RP, Lombard CJ, Spitaels A, et al. High prevalence of Mycobacterium tuberculosis infection and disease in children and adolescents with type 1 diabetes mellitus. Int J Tuberc Lung Dis. 2009;13(7):868–74.
Hensel RL, Kempker RR, Tapia J, Oladele A, Blumberg HM, Magee MJ. Increased risk of latent tuberculous infection among persons with pre-diabetes and diabetes mellitus. Int J Tuberc Lung Dis. 2016;20(1):71–8. https://doi.org/10.5588/ijtld.15.0457.
Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med. 2008;5(7):e152. https://doi.org/10.1371/journal.pmed.0050152.
Roohk HV, Zaidi AR. A review of glycated albumin as an intermediate glycation index for controlling diabetes [J]. J Diabetes Sci Technol. 2008;2(6):1114–21. https://doi.org/10.1177/193229680800200620.
Basevi V, Di Mario S, Morciano C, et al. Comment on: American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care 2011;34(Suppl. 1): S11-S61[J]. Diabetes Care. 2011;34(5):e53–4.
Cohen MP, Hud E. Measurement of plasma glycoalbumin levels with a monoclonal antibody based ELISA. J Immunol Methods. 1989;122(2):279–83. https://doi.org/10.1016/0022-1759(89)90275-5.
Qiu H, Shi Y, Li Y, Shen X, Li R, Yang Q, et al. Incident rate and risk factors for tuberculosis among patients with type 2 diabetes: retrospective cohort study in Shanghai, China. Tropical Med Int Health. 2017;22(7):830–8. https://doi.org/10.1111/tmi.12884.
Lee P, Fu H, Lai T, et al. Glycemic control and the risk of tuberculosis: a cohort study. PLoS Med. 2016;13(8):e1002072. https://doi.org/10.1371/journal.pmed.1002072.
Stevenson CR, Critchley JA, Forouhi NG, Roglic G, Williams BG, Dye C, et al. Diabetes and the risk of tuberculosis: a neglected threat to public health? Chronic Illn. 2007;3(3):228–45. https://doi.org/10.1177/1742395307081502.
Restrepo BI, Fisher Hoch SP, Pino PA, et al. Tuberculosis in poorly controlled type 2 diabetes: altered cytokine expression in peripheral white blood cells [J]. Clin Infect Dis. 2008;47(5):634–41. https://doi.org/10.1086/590565.
Kassa D, Ran L, Geberemeskel W, Tebeje M, Alemu A, Selase A, et al. Analysis of immune responses against a wide range of Mycobacterium tuberculosis antigens in patients with active pulmonary tuberculosis. Clin Vaccine Immunol. 2012;19(12):1907–15. https://doi.org/10.1128/CVI.00482-12.
Hodgson K, Morris J, Bridson T, Govan B, Rush C, Ketheesan N. Immunological mechanisms contributing to the double burden of diabetes and intracellular bacterial infections. IMMUNOLOGY. 2015;144(2):171–85. https://doi.org/10.1111/imm.12394.
Delgado JC, Baena A, Thim S, Goldfeld AE. Aspartic acid homozygosity at codon 57 of HLA-DQ beta is associated with susceptibility to pulmonary tuberculosis in Cambodia. J Immunol. 2006;176(2):1090–7. https://doi.org/10.4049/jimmunol.176.2.1090.
Collaborative framework for care and control of tuberculosis and diabetes. Geneva: World Health Organization, 2011. PMID: 26290931. Available from:https://www.ncbi.nlm.nih.gov/books/NBK310833/. [Accessed 10 June 2021].
Jabbar A, Hussain SF, Khan AA. Clinical characteristics of pulmonary tuberculosis in adult Pakistani patients with co-existing diabetes mellitus. East Mediterr Health J. 2006;12(5):522–7.
Acknowledgements
We would like to thank Prof. Shunqing Xu, Yuanyuan Li and Wei Xia, from Huazhong University of Science and Technology, China, for providing suggestive comments on an early draft.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
ZFC drafted the protocol. QL performed the searches, analyzed the data. ZFC and QL drafted the manuscript. RRS and WXZ critically reviewed the manuscript and provided valuable comments. TPW, ZL, XZS, and YLL provided valuable suggestions in data analysis and manuscript writing. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No needed for this meta-analysis of already published data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy for the systematic review.
Additional file 2 Table S1
. Results of quality assessment for 9 studies.
Additional file 3 Fig. S1
. Forest plot of observational studies on poorly controlled DM and tuberculosis infection excluded the study with the elderly. Fig. S2. Forest plot of observational studies on glycated haemoglobin A1c concentrations and tuberculosis infection with restricting to the case-control studies. Fig. S3. Forest plot of observational studies on fasting plasma glucose concentrations and tuberculosis infection with restricting to the case-control studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Z., Liu, Q., Song, R. et al. The association of glycemic level and prevalence of tuberculosis: a meta-analysis. BMC Endocr Disord 21, 123 (2021). https://doi.org/10.1186/s12902-021-00779-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-021-00779-6