Abstract
Background
Hibernoma is a rare soft tissue tumor stem from persistent fetal brown fat tissue. This benign tumor may occasionally occur in head and neck area and, in most cases, is characterized by an asymptomatic slow growth.
Case presentation
We presented an uncommon case of hibernoma of the posterior cervical triangle occurring in a 30-year-old man referred to the department of otolaryngology. The patient suffered from a right, very painful, and rapidly growing mass since 3 months. MRI examination reported both an infiltrating mass and a homogenous enhancement of an underlying vascularization after the injection of intravenous contrast. According to the risk of sarcoma, a surgical procedure was made to completely excise the mass that was a hibernoma.
Conclusions
Hibernoma may occur with an uncommon clinical presentation imitating malignancy. MRI plays a key role in the differential diagnosis and surgery remains the better therapeutic approach.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Hibernoma is a rare benign tumor originating from persistent fetal brown fat tissue [1]. The brown fat has a thermogenesis function, especially in the first years of a child’s life, but it regresses with age [1]. In adults, the most common residual areas of brown fat are usually located in the inter-scapular region, mediastinum, retroperitoneum, back, thigh and, sometimes, in head and neck [2,3,4]. Widely, the remaining of brown fat still remains asymptomatic and has no impact on the homeostasis. In rare cases, the remaining tissue can slowly grow, leading to the occurrence of a soft-tissue tumor. Thus, some cases of hibernoma are well described in the current literature and they are commonly found in chest, abdominal cavity and head and neck [3, 4]. In this paper, we reported an unusual case of hibernoma in a patient with a painless mass at the base of the neck. The current literature was reviewed about epidemiology, clinical course, diagnosis and treatment.
Case presentation
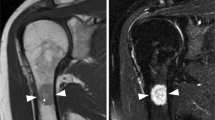
A 30-year-old man was referred to the Department of Otolaryngology and Head and Neck Surgery for mass located in the right posterior cervical triangle of the neck. The patient had this mass since several months but it recently started to grow in a context of substantial neck pain. The patient had no difficulty to breathe and swallow. Clinical examination exhibited a relatively mobile, soft mass located in the supraclavicular area. No cervical node was found. Both clinical and ultrasound examinations led to suspect a soft tissue mass, and the magnetic resonance imaging (MRI) revealed a 38 mm along the axis tumor (Fig. 1) between the elevator scapulae and the right scalene muscles. The tumor infiltrated the scalene muscles and the injection of intravenous contrast (gadolinium) reported a homogenous enhancement of an important underlying vascularization, a nodular structure of the tissue, and the presence of septa > 2 mm. According to the clinical features and the MRI characteristics (especially T1 sequence), we highly suspected liposarcoma of the neck. The fine needle aspiration biopsy was made but non-contributory. Thus, a surgical procedure was made to completely excise the mass and the macroscopic examination revealed an encapsulated taned-brown polylobulated tumor. The immediate post-operative follow-up was unremarkable. The definitive histopathological examination retained the diagnosis of a hibernoma, which was characterized by mature fat cells, abundant eosinophilic cells with small cytoplasmic vacuoles and regular, small, round cell nuclei (Fig. 2). The 4-years follow-up was unremarkable and the patient had no recurrence.
Discussion
Since the first case described in 1906 [5], approximately ten cases of cervical hibernoma have been reported [6]. Among these, only three patients had hibernoma in the posterior cervical triangle but it seems highly probable that the diagnosis is widely underestimated [7, 8]. Indeed, with the contribution of modern technological advancements in positron emission tomography, some recent research supports the theory that the true prevalence of brown fat in adult is between 30 and 100%, suggesting an increased possibility to develop hibernoma, though often misdiagnosed or confused with lipoma [9]. Yet, it is important to make the difference between lipoma and hibernoma since, to date, no case of malignant transformation of hibernoma has been reported, which is not the case of lipoma. From an epidemiological standpoint, hibernoma is mostly seen in the third, fourth and fifth decades of life with a slightly higher female prevalence [6, 10].
Clinically, most patients with neck hibernoma are usually asymptomatic over time even if the slow growth of the tumor may, at some point, compress the adjacent structures [7, 8]. In our patient, the rapid growth and the related pain are uncommon manifestations and prompted us to quickly carry out additional examinations to exclude malignancy. To the best of our knowledge, only one reported case was characterized by similar clinical findings [6]. Among the complementary examinations, computed tomography (CT), MRI, and angiography can provide additional usefulness informations. So, hibernomas are usually depicted as well-circumscribed and variably homogeneous tumors with marked contrast enhancement. The differentiation with lipoma is possible with MR imaging because hibernoma still remains more vascularized, with large septa (>2 mm; easily seen with contrast agent), and, unlike to lipoma, the hibernoma tissue can be differentiated to the fat with MRI STIR or T2 Fat Sar sequences [11, 12]. Table 1 summarizes the clinical and imaging characteristics of lipoma, liposarcoma and hibernoma.
In our patient, the MRI examination showed a 38 mm along the axis, relatively well circumscribed tumor with intermediate signal intensity between subcutaneous fat and muscle. Moreover, the observed tumor was homogenous, relatively well circumscribed, with septa > 2 mm and some nodular areas. All of these features led us to exclude lipoma but the critical point concerned the differential diagnosis with liposarcoma. Indeed, the high vascularization, the large septa, and the fast arteriovenous contrast enhancement may mislead to liposarcoma diagnosis. Thus, as reported in the current literature, even with imaging, the characteristics of this tumor remain difficult to differentiate from malignant fat tumors and some very rare tumors such as angiolipoma and malignant fibrous histocytoma [6, 13, 14].
The final diagnosis is made after a fine needle aspiration procedure or after the surgical excision [6]. As showed in our patient, the histopathological findings include small, round, brown fat-like cells, variable numbers of mature fat cells with i) uniform, small eosinophilic cytoplasmic vacuoles, ii) regular, small, and round cell nuclei; and iii) delicate branching capillaries. Hypervascularization combined with abundant mitochondria give hibernomas their color. Concerning the histopathological differential diagnosis with liposarcoma, some cytology features (i.e. admixture of multivacuolated and univacuolated fat cells; a rich, delicate, capillary-like vasculature) are known to lead to a misdiagnosis of liposarcoma and the pathologists must take into consideration these similar characteristics. To date, hibernoma can be classified by morphologic or histological characteristics such as the presence of multivacuolated or univacuolated cells found in brown fat or normal fat [6]. Morphological, four variants of hibernoma are described: typical, myxoid, spindle cell, and lipoma-like [15]. Typical hibernoma included eosinophilic, pale, and mixed cell types. The myxoid variant contained a loose basophilic matrix while the spindle cell hibernoma had features of spindle cell lipoma. The lipoma-like variant only contained scattered cells. The present histopathological case corresponds to the typical variant. The 4-years follow-up of our patient did not report recurrence that seems to be in line with the other cases reported in the literature [6].
Conclusion
Hibernoma is a rare benign tumor that can mimic malignant lesion of the soft tissue such as liposarcoma. In this paper, we report an unusual presentation of hibernoma of the posterior cervical triangle characterized by both severe pain and rapid growth. MRI plays a key role in the differential diagnosis, especially with other benign tumors but still remains limited for the differential diagnosis with malignancy. The biopsy and the surgery procedure correspond to the gold standard approaches for the final diagnosis, the exclusion of liposarcoma, and to select the appropriate treatment. To date, there is no described case of recurrence or malignant transformation.
Abbreviations
- CT :
-
Computed tomography
- MRI:
-
Magnetic resonance imaging.
References.
Cannon B, Nedergaard J. Brown Adipose Tissue: Function and Physiological. Significance. Physiol Rev. 2004;84:277–359.
Chen CL, Chen WC, Chiang JH, Ho CF. Intercapsular hibernoma-Case report and literature review. Kaohsiung J Med Sci. 2011;27:348–52.
Della Volpe C, Salazard B, Casanova D, Vacheret H, Bartoli JF, Magalon G. Hibernoma of the antero-lateral thigh. Br J Plast Surg. 2005;58:859–61.
Hertoghs M, Van Schil P, Rutsaert R, Van Marck E, Vallaeys J. Intrathoracic hibernoma: Report of two cases. Lung Cancer. 2009:367–70.
Merkel H. Über ein Pseudolipon der Mamma. Beitr Path Anat Allge Path. 1906; 39:152–157. [article in German].
Trujillo O, Cui IH, Malone M, Suurna M. An unusual presentation of a rare benign tumor in the head and neck: A review of hibernomas. Laryngoscope. 2015;125(7):1656–9.
Florio G, Cicia S, Del Papa M, Carnì D. Neck hibernoma: case report and literature review. G Chir. 2000;21(8–9):339–41.
Arsa J. Minié. Hibernoma: unusual location in the submental space. J Craniomaxillofac Surg. 1992;20:264–5.
Nedergaard J, Bengtsson T, Cannon B. Three years with adult human brown adipose tissue. Ann N Y. Acad Sci. 2010;1212:E20–36.
Khattala K, Elmadi A, Bouamama H, Rami M, Bouabdallah Y. Cervical hibernoma in a two year old boy. Pan Afr Med J. 2013;16:27.
Papathanassiou ZG, Alberghini M, Taieb S, Errani C, Picci P, Vanel D. Imaging of hibernomas: A retrospective study on twelve cases. Clin Sarcoma Res. 2011;1(1):3.
DeRosa DC, Lim RB, Lin-Hurtubise K, Johnson EA. Symptomatic hibernoma: a rare soft tissue tumor. Hawaii J Med Public Health. 2012;71(12):342–5.
Jaroszewski DE, Petris GD. Giant hibernoma of the thoracic pleura and chest wall. World J Clin Cases. 2013;1(4):143–5.
Salim B, Belkacem C. Hibernoma of the thigh: a report of four cases. J Orthop Surg. 2014;22(1):118–21.
Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: a clinicopathologic study of 170 cases. Am J Surg Pathol. 2001;25(6):809–14.
Acknowledgments
Dr. Sarah Saxena, MD, native English speaker for the collaboration in proofreading of the article. Dr. Stelianos Kampouridis for the MRI pictures.
Competing Interests.
The authors declare that they have no competing interests.
Funding
None.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Authors contributions.
AR wrote the paper et realized the surgical approach with TD. SS and JRL reviewed and corrected the paper. All authors read and approved the final manuscript.
Consent for publication.
The patient accepted the publication of the case and gave his consent.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rodriguez Ruiz, A., Saussez, S., Demaesschalck, T. et al. Hibernoma: a rare case of adipocytic tumor in head and neck.. BMC Ear Nose Throat Disord 17, 13 (2017). https://doi.org/10.1186/s12901-017-0046-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12901-017-0046-8