Abstract
Background
To investigate the role of antimicrobial prophylaxis in laparoscopic nephrectomy for renal cell carcinoma.
Methods
We retrospectively enrolled 1000 patients who underwent laparoscopic nephrectomy from August 2019 to November 2021 in the Peking Union Medical College Hospital. Patients were divided into group without antimicrobial prophylaxis (n = 444) and group with antimicrobial prophylaxis (n = 556). Outcomes including 30-day postoperative infection rate, the increase rate of pre- and post-operative white blood cell counts and hospital stay were analyzed.
Results
The overall infection rate was 5.0% (28/556) in the group with antimicrobial prophylaxis, which was similar to 4.1% (18/444) in the group without antimicrobial prophylaxis (P = 0.461). The increase rate of pre- and post-operative white blood cell counts was significantly lower (85.5% versus 97.0%) in the group with antimicrobial prophylaxis (P = 0.004). The postoperative hospital stay was 5 (4, 6) days in both groups (P = 0.483). Logistic regression analyses identified the use of antimicrobial prophylaxis had no influence on the occurrence of infection events (odds ratio = 0.797; 95% confidence interval, 0.435–1.460; P = 0.462). Hemoglobin (odds ratio = 0.430; 95% confidence interval, 0.257–0.719; P = 0.001) and partial nephrectomy (odds ratio = 2.292; 95% confidence interval, 1.724–3.046; P < 0.001) influenced the use of antimicrobial prophylaxis independently.
Conclusions
The use of antimicrobial prophylaxis had no impact on postoperative infection in patients receiving laparoscopic nephrectomy for renal cell carcinoma.
Similar content being viewed by others
Background
Antimicrobial prophylaxis (AMP) is widely used to prevent postoperative infection. In terms of urologic surgery, the European Association of Urology published a guideline for AMP in various surgical procedures [1]. However, little was demonstrated on laparoscopic urologic procedures. With the advantage of low invasiveness, laparoscopic surgery is popular in urologic field. Much evidence supports that the incidence of infection following laparoscopic surgery is lower than that of open surgery in either urologic field [2, 3] or non-urologic field [4,5,6,7]. Therefore, the protocols of perioperative AMP may be different between laparoscopic and open urologic surgery.
The Japanese Urological Association guideline recommends 1-day AMP protocol for clean operations and 3-day AMP protocol for clean-contaminated operations [8]. However, the guideline recommends the same AMP protocol for both laparoscopic and open urologic surgery. Yamamoto et al. pointed that more solid evidence is needed to establish a consensus for AMP use in laparoscopic procedures alone [9]. As early as 2004, Takeyama et al. demonstrated that the prophylactic efficacy of 1-day AMP was similar to that of 3-day AMP for clean or clean-contaminated urologic laparoscopic surgery [10]. Furtherly, Toshiki et al. prospectively investigated 373 cases undergoing gasless laparoendoscopic single-port surgery for renal or adrenal tumors without AMP use. It turned out that non-use of AMP and the on-demand use of antibiotics was efficient for minimally invasive renal and adrenal surgery [11]. In recent years, Aditya et al. presented that single‑dose cefuroxime was adequate for clean or clean-contaminated urologic surgery. However, only 65 patients underwent laparoscopic surgery in the study [12]. Therefore, it is possible that short-time AMP or even no AMP is sufficient to prevent postoperative infection for laparoscopic urologic surgery.
The incidence of renal cell carcinoma (RCC) is increasing, with approximately 400,000 new cases per year worldwide [13]. Laparoscopic nephrectomy is the standard treatment for localized RCC [14]. Radical nephrectomy is considered as clean surgery while partial nephrectomy is categorized as clean-contaminated surgery due to the possibility of urine contamination in the surgical field [9]. Until now, no standard AMP regimen for laparoscopic nephrectomy for RCC has been established. Inappropriate application of antibiotics during the perioperative period of RCC may result in the emergence of antimicrobial resistant bacteria, adverse events from administered drugs and the increase of hospital cost and stay [15, 16]. Therefore, there is an urgent need to demonstrate the role of AMP in laparoscopic nephrectomy for RCC.
Thus, we performed an investigation on the role of AMP in a Chinese tertiary center and tried to provide more evidence for deciding an optimal AMP regimen in laparoscopic nephrectomy for RCC.
Methods
Patients
We retrospectively enrolled 1000 patients who underwent laparoscopic nephrectomy from August 2019 to November 2021 in the Peking Union Medical College Hospital. The inclusion criteria were as follows: (1) patients were diagnosed as primary RCC by pathology; (2) patients underwent laparoscopic nephrectomy successfully, without conversion to open surgery; (3) patients were aged between 18 and 85 years. Patients were excluded if they had signs of infection prior to the operation, contaminated operation site or a history of autoimmune diseases requiring long-term immunosuppressant or steroid therapy. Patients were classified into AMP group and non-AMP group according to the use of AMP.
Data collection
Patients’ clinical characteristics including sex, age, body mass index (BMI), history of smoking, hypertension, diabetes, cardiovascular disease, cerebral infarction and other malignancies, American Society of Anesthesiologists (ASA) score, hemoglobin (Hb), platelet (PLT), alanine aminotransferase (ALT), albumin (ALB), creatinine (CREA), side and size of the tumor lesion, surgical approach (radical or partial nephrectomy, retroperitoneal or transperitoneal), operation time and blood loss were collected. For patients in the AMP group, the duration of AMP and the type of the antibiotics were also collected.
Operations and perioperative care
Robot-assisted or pure laparoscopic nephrectomy was performed via retroperitoneal or transperitoneal approach depending on the location and size of the tumor lesion. Usually three to five ports with skin incisions were needed. The maximum length of the incisions depended on the size of specimen. For radical nephrectomy, a skin incision approximately 8 cm in length was made to ensure enough space for hand insertion. All operations were performed under standard sterilization of the surgical sites. At the end of an operation, the surgical wound was closed by absorbable stitches, thereafter disinfected with iodine complex and then covered with sterile gauzes. Dressings were changed regularly after the operation.
Outcomes
The primary outcome was 30-day postoperative infection rate, including surgical site infection (SSI) and remote infection (RI). SSI was categorized into superficial infection, deep infection and infection of organs/space, based on the guideline of SSI prevention [17]. RI was defined as systemic infection involving respiratory, urinary tract or gastrointestinal tract system. RI was featured by high fever (body temperature over 38.5℃), elevation of white blood cell (WBC) count and positive pathogenic tests, or no pathogenic evidence, but over two senior physicians reached an agreement of RI [18]. Secondary outcomes included the increase rate of pre- and post-operative WBC counts and hospital stay. For patients in the non-AMP group, the unplanned addition of antibiotics was also analyzed.
Statistical analysis
Continuous variables including age, BMI, Hb, PLT, ALT, ALB, CREA, tumor size, operation time and blood loss were transformed into categorical variables based on normal reference values or clinical judgment. All categorical variables were presented as frequency and percentage. Difference test was conducted using the chi-square or Fisher’s exact test. The duration of AMP, increase rate of pre- and post-operative WBC counts and postoperative hospital stay were presented as median and interquartile range. The increase rate of WBC and postoperative hospital stay were compared using Mann-Whitney U test. Univariable and multivariable logistic regression analyses were used to determine factors influencing AMP using and postoperative infection. Statistical analyses were conducted using SPSS software (version 25, IBM). All tests were two-sided, and P < 0.05 indicated statistical significance.
Results
Patient characteristics
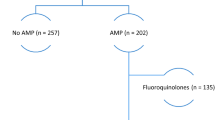
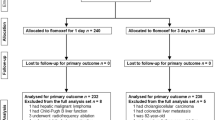
A total of 1000 patients were included in the study, in which 556 patients received AMP and 444 patients did not. Baseline characteristics of the two groups were shown in Table 1. Patients in the AMP group were more likely to have anemia (for Hb less than reference value, 9.7% versus 5.4%, P = 0.012), smaller tumor lesions (for tumor size ≤ 7 cm, 94.8% versus 91.4%, P = 0.036), undergo partial nephrectomy (72.7% versus 54.3%, P < 0.001) and adopt transperitoneal approach (7.0% versus 4.1%, P = 0.045). Other characteristics were comparable between the two groups. For patients in the AMP group, the duration of AMP was 3 (3, 4) days. A proportion of 29.1% patients received AMP more than 3 days (Fig. 1). The types of antibiotics were shown in Table 2. Nearly 70% patients received second-generation cephalosporins.
Factors influencing the use of AMP
As shown in Table 3, univariable logistic regression analysis revealed that Hb, tumor size, partial nephrectomy and surgical approach were influencing factors for AMP. However, following multivariable logistic regression analysis indicated that only Hb [odds ratio (OR) = 0.430; 95% confidence interval (CI), 0.257–0.719; P = 0.001] and partial nephrectomy (OR = 2.292; 95% CI, 1.724–3.046; P < 0.001) influenced the use of AMP independently. Patients who had lower Hb and partial nephrectomy tended to receive AMP.
Outcomes
The overall 30-day postoperative infection rate was 5.0% (28/556) in the AMP group and 4.1% (18/444) in the non-AMP group. The difference of infection rates was not significant (P = 0.461). In the AMP group, 3 patients experienced SSI and 25 patients had RI. In the non-AMP group, 3 patients underwent SSI and 15 patients had RI. The detailed infection events were shown in Table 4. In terms of the secondary outcomes, the increase rate of pre- and post-operative WBC counts was 85.5% (58.0%, 121.8%) in the AMP group, significantly lower than 97.0% (67.3%, 124.8%) in the non-AMP group (P = 0.004). The postoperative hospital stay was 5 (4, 6) days in either AMP or non-AMP group (P = 0.483). For patients in the non-AMP group, the unplanned addition of antibiotics occurred in 5.0% (22/444) cases, in which 2 patients underwent SSI and 7 patients had RI. All the infection events were well-controlled by antibiotics. Of note, in the AMP group, the antibiotics was upgraded to control infection events in 1 patient with SSI and 4 patients with RI.
Additionally, we performed further subgroup analysis. In patients undergoing partial nephrectomy, the overall infection rate was 6.4% (26/404) in the AMP group and 5.0% (12/241) in the non-AMP group (P = 0.447). In patients undergoing radical nephrectomy, the overall infection rate was 1.3% (2/152) in the AMP group and 3.0% (6/203) in the non-AMP group (P = 0.504). In patients with operation time more than 120 min, the overall infection rate was 8.3% (10/120) in the AMP group and 5.2% (6/116) in the non-AMP group (P = 0.334). In patients with operation time within 120 min, the overall infection rate was 4.1% (18/436) in the AMP group and 3.7% (12/328) in the non-AMP group (P = 0.741). In patients with ASA 1, the overall infection rate was 3.5% (8/230) in the AMP group and 3.0% (6/200) in the non-AMP group (P = 0.780). In patients with ASA 2, the overall infection rate was 6.1% (20/326) in the AMP group and 4.9% (12/244) in the non-AMP group (P = 0.532). In the AMP group, the overall infection rate was 6.2% (10/162) in patients who received AMP more than 3 days and 4.6% (18/394) in patients who received AMP within 3 days (P = 0.432). Besides, the overall infection rate was 4.8% (19/395) in patients who received second-generation cephalosporins and 5.6% (9/161) in patients who received other types of antibiotics (P = 0.703).
Factors influencing the occurrence of infection events
As shown in Table 5, univariable logistic regression analysis revealed that partial nephrectomy was the only influencing factor for the occurrence of infection events (OR = 2.715; 95% CI, 1.253–5.887; P = 0.011). Patients who underwent partial nephrectomy tended to experience infection events. The use of AMP had no influence on the occurrence of infection events (OR = 0.797; 95% CI, 0.435–1.460; P = 0.462).
Discussion
There has been inadequate evidence on the AMP use for laparoscopic nephrectomy up till now. Using a large-scale Chinese patient data, our study found that the nonuse of AMP had an equivalent effect on postoperative infection compared to AMP use in patients receiving laparoscopic nephrectomy for RCC.
We focused on a consecutive cohort undergoing laparoscopic nephrectomy and found that 44.4% patients received no AMP. The median duration of AMP was 3 days in AMP group, similar to the Japanese Urological Association guideline recommendation. The overall infection rate was 4.6% in the whole cohort, similar to the infection rates reported in previous studies [11, 19]. Our following analysis revealed that the infection rates of AMP and non-AMP groups were similar and AMP use had no effect on the occurrence of infection events, despite a less increase of pre- and post-operative WBC counts in the AMP group. Subgroup analysis showed that AMP use did not decrease infection rates in patients undergoing either partial nephrectomy or radical nephrectomy, despite partial nephrectomy was a risk factor for the occurrence of infection events. Besides, the addition and upgrade of antibiotics were adequate to control postoperative infection. Therefore, AMP may be not a necessary perioperative procedure in laparoscopic nephrectomy for RCC.
The possibility of eliminating AMP was also demonstrated in Toshiki’s study, though they only incorporated clean urologic surgeries [11]. The underlying reasons for the no impact of AMP on postoperative infection may lie in following aspects. First, except AMP use, measures including removal of hair, applying an incise drape to the surgical site, use of antimicrobial sutures and clean operating room environment also play an important role to prevent postoperative infection [15, 20]. Second, the smaller incision and less exposure of intracorporal oragans/tissues to the air in laparoscopic surgery may contribute to less infection events. Third, AMP was intended for prevention of SSI [21]. However, the incidence of RI was higher than that of SSI in our study. Therefore, the effect of AMP may be less obvious under above circumstances.
The nonuse of AMP for laparoscopic nephrectomy has several benefits. First, it may exert a preventive effect on the development of bacterial resistance. Misuse of antibiotics may increase bacterial resistance [22, 23]. Calvert et al. reported that extended AMP beyond 24 h for partial or radical nephrectomy was associated with a 3.79 times higher possibility of Clostridium difficile infection [24]. In our study, nearly 30% patients in the AMP group received AMP for more than 3 days and AMP regimens varied in different types of antibiotics, which to some extent mirrors the abuse of antibiotics. Therefore, there is an urgent need to cut down unnecessary AMP use in laparoscopic nephrectomy. Second, the reduced use of AMP may help lower the risk of adverse events associated with antibiotics, such as allergic reaction, gastrointestinal reaction and damage to hepatic/renal function. Although the adverse events following antibiotics administration are relatively uncommon, it remains valuable to prevent the occurrence of adverse events since it’s difficult to evaluate and predict the degree of each adverse event [25]. Third, the reduced use of AMP can relieve the socioeconomic burden caused by the expense of antibiotics, instruments used for administration, as well as labor cost [22, 26,27,28]. This benefit is even prominent in China owing to its large population and relatively limited medical resources.
Our analysis also revealed that patients with patients who had lower Hb and partial nephrectomy tended to receive AMP. It’s reasonable for physicians to apply AMP in patients undergoing partial nephrectomy since partial nephrectomy is seen as clean-contaminated. Anemia usually reflects a status of malnutrition, which is a risk factor for perioperative infections [8]. Therefore, physicians tended to use AMP in patients with lower Hb.
To our knowledge, this is the largest cohort study focusing on the AMP use in laparoscopic nephrectomy for RCC. Our study indicated that in patients undergoing laparoscopic nephrectomy for RCC, eliminating AMP use may be possible. However, there are several limitations in our study. First, the study is retrospective and non-randomized. There remains a risk of selection and confounding bias. Randomized controlled trials are needed to provide more solid evidence on this issue. Second, our study is only suitable for patients with relatively good general conditions. For patients with high-risk factors for infection, such as severe diabetes, immunocompromised status and other severe comorbidities, the use of AMP should be cautiously assessed.
Conclusions
In conclusion, the nonuse of AMP had an equivalent effect on postoperative infection compared to AMP use in patients receiving laparoscopic nephrectomy for RCC. AMP may be not a necessary perioperative procedure in laparoscopic nephrectomy for RCC.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMP:
-
Antimicrobial prophylaxis
- ALB:
-
Albumin
- ALT:
-
Alanine aminotransferase
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CREA:
-
Creatinine
- Hb:
-
Hemoglobin
- OR:
-
Odds ratio
- PLT:
-
Platelet
- RCC:
-
Renal cell carcinoma
- RI:
-
Remote infection
- SSI:
-
Surgical site infection
- WBC:
-
White blood cell
References
Naber KG, Bergman B, Bishop MC, Bjerklund-Johansen TE, Botto H, Lobel B, et al. EAU guidelines for the management of urinary and male genital tract infections. Urinary tract infection (UTI) Working Group of the Health Care Office (HCO) of the European Association of Urology (EAU). Eur Urol. 2001;40(5):576–88.
Rassweiler J, Seemann O, Schulze M, Teber D, Hatzinger M, Frede T. Laparoscopic versus open radical prostatectomy: a comparative study at a single institution. J Urol. 2003;169(5):1689–93.
Soulié M, Salomon L, Seguin P, Mervant C, Mouly P, Hoznek A, et al. Multi-institutional study of complications in 1085 laparoscopic urologic procedures. Urology. 2001;58(6):899–903.
Richards C, Edwards J, Culver D, Emori TG, Tolson J, Gaynes R. Does using a laparoscopic approach to cholecystectomy decrease the risk of surgical site infection? Ann Surg. 2003;237(3):358–62.
McCall JL, Sharples K, Jadallah F. Systematic review of randomized controlled trials comparing laparoscopic with open appendicectomy. Br J Surg. 1997;84(8):1045–50.
Meltomaa SS, Mäkinen JI, Taalikka MO, Helenius HY. Incidence, risk factors and outcome of infection in a 1-year hysterectomy cohort: a prospective follow-up study. J Hosp Infect. 2000;45(3):211–7.
Boni L, Benevento A, Rovera F, Dionigi G, Di Giuseppe M, Bertoglio C, et al. Infective complications in laparoscopic surgery. Surg Infect (Larchmt). 2006;7(Suppl 2):S109–11.
Matsumoto T, Kiyota H, Matsukawa M, Yasuda M, Arakawa S, Monden K. Japanese guidelines for prevention of perioperative infections in urological field. Int J Urol. 2007;14(10):890–909.
Yamamoto S, Shima H, Matsumoto T. Controversies in perioperative management and antimicrobial prophylaxis in urologic surgery. Int J Urol. 2008;15(6):467–71.
Takeyama K, Shimizu T, Mutoh M, Nishiyama N, Kunishima Y, Matsukawa M, et al. Prophylactic antimicrobial agents in urologic laparoscopic surgery: 1-day versus 3-day treatments. J Infect Chemother. 2004;10(3):168–71.
Kijima T, Masuda H, Yoshida S, Tatokoro M, Yokoyama M, Numao N, et al. Antimicrobial prophylaxis is not necessary in clean category minimally invasive surgery for renal and adrenal tumors: a prospective study of 373 consecutive patients. Urology. 2012;80(3):570–5.
Sharma AP, Devana SK, Bora GS, Mavuduru RS, Mohan B, Taneja N, et al. Protocol-based perioperative antimicrobial prophylaxis in urologic surgeries: feasibility and lessons learned. Indian J Urol. 2019;35(2):141–6.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Ljungberg B, Cowan NC, Hanbury DC, Hora M, Kuczyk MA, Merseburger AS, et al. EAU guidelines on renal cell carcinoma: the 2010 update. Eur Urol. 2010;58(3):398–406.
Alexander JW. When should prophylactic antibiotics be given? Ann Surg. 2009;249(4):557–8.
Rogues AM, Dumartin C, Amadéo B, Venier AG, Marty N, Parneix P, et al. Relationship between rates of antimicrobial consumption and the incidence of antimicrobial resistance in Staphylococcus aureus and Pseudomonas aeruginosa isolates from 47 French hospitals. Infect Control Hosp Epidemiol. 2007;28(12):1389–95.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017;152(8):784–91.
Hirokawa F, Hayashi M, Miyamoto Y, Asakuma M, Shimizu T, Komeda K, et al. Evaluation of postoperative antibiotic prophylaxis after liver resection: a randomized controlled trial. Am J Surg. 2013;206(1):8–15.
Cai T, Verze P, Brugnolli A, Tiscione D, Luciani LG, Eccher C, et al. Adherence to European Association of Urology Guidelines on prophylactic antibiotics: an important step in Antimicrobial Stewardship. Eur Urol. 2016;69(2):276–83.
Dohmen PM. Antibiotic resistance in common pathogens reinforces the need to minimise surgical site infections. J Hosp Infect. 2008;70(Suppl 2):15–20.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Guideline for Prevention of Surgical Site infection, 1999. Am J Infect Control. 1999;27(2):97–132. quiz 3–4; discussion 96.
Moslemi MK, Movahed SM, Heidari A, Saghafi H, Abedinzadeh M. Comparative evaluation of prophylactic single-dose intravenous antibiotic with postoperative antibiotics in elective urologic surgery. Ther Clin Risk Manag. 2010;6:551–6.
Monroe S, Polk R. Antimicrobial use and bacterial resistance. Curr Opin Microbiol. 2000;3(5):496–501.
Calvert JK, Holt SK, Mossanen M, James AC, Wright JL, Porter MP, et al. Use and outcomes of extended antibiotic prophylaxis in urological cancer surgery. J Urol. 2014;192(2):425–9.
Wolf JS Jr., Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179(4):1379–90.
Spelman D, Harrington G, Russo P, Wesselingh S. Clinical, microbiological, and economic benefit of a change in antibiotic prophylaxis for cardiac surgery. Infect Control Hosp Epidemiol. 2002;23(7):402–4.
Woodfield JC, Van Rij AM, Pettigrew RA, van der Linden A, Bolt D. Using cost of infection as a tool to demonstrate a difference in prophylactic antibiotic efficacy: a prospective randomized comparison of the pharmacoeconomic effectiveness of ceftriaxone and cefotaxime prophylaxis in abdominal surgery. World J Surg. 2005;29(1):18–24.
Su HY, Ding DC, Chen DC, Lu MF, Liu JY, Chang FY. Prospective randomized comparison of single-dose versus 1-day cefazolin for prophylaxis in gynecologic surgery. Acta Obstet Gynecol Scand. 2005;84(4):384–9.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the National High Level Hospital Clinical Research Funding (No. 2022-PUMCH-B-008).
Author information
Authors and Affiliations
Contributions
MW, JD and ZJ performed study concept and design; MW, WY and WX provided acquisition, analysis and interpretation of data, and statistical analysis; GL and YX provided technical and material support; MW, JD and ZJ performed development of methodology and writing, review and revision of the paper. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the institutional review board of the Ethic Committee of the Peking Union Medical College Hospital and it conforms to the provisions of the Declaration of Helsinki. The informed consent was waived due to the retrospective design of the study by the institutional review board of the Ethic Committee of the Peking Union Medical College Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, M., Yang, W., Xu, W. et al. The role of antimicrobial prophylaxis in laparoscopic nephrectomy for renal cell carcinoma. BMC Urol 24, 60 (2024). https://doi.org/10.1186/s12894-024-01447-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-024-01447-2