Abstract
Background
Urinary incontinence (UI) is one of the most common problems in old age that is often seen in women, which causes not only physical problems but also psychological, social, economic problems and poor quality of life. The aim of the present study was to evaluate the UI and related quality of life (QoL) in elderly women.
Methods
This cross-sectional study enrolled 369 women over 60 years old and living in Tabas city, Iran who were selected by cluster random sampling method. The instruments included the International Consultation on Incontinence Questionnaire-Short Form, the International Consultation on Incontinence Questionnaire Urinary Incontinence Quality of Life Module, and a demographic questionnaire. Data analysis was carried out using independent t-test, chi-square, and logistic regression in SPSS software.
Results
The UI prevalence among participants was 24.9% and stress urinary incontinence was the most common type (40.2% of all elderly patients). The mean UI-related QoL score was 38.04 ± 11.67 from the score range of 22–76. There was a significant positive correlation between UI-related QoL score and UI score (r = 0.585, p < 0.001). Age, body mass index (BMI), constipation, history of cesarean section, hypertension, and the use of angiotensin receptor blockers are factors increasing the odds of having UI in this study population.
Conclusion
Aging, some chronic diseases, high BMI, and the use of some drugs are related to UI prevalence. Also, it is associated with lower QOL among elderly women. Designing appropriate intervention programs, controlling chronic diseases, training in the proper use of drugs, and also some physical exercises can be effective in controlling and improving this common syndrome of old age and promoting their QoL.
Similar content being viewed by others
Introduction
Urinary incontinence (UI)—the complaint of any involuntary leakage of urine-is common in women that increases with age and may decrease quality of life [1]. Therefore, UI is one of the most common syndromes in old age, and depending on different populations, its prevalence has been reported between 2.8% in Nigeria and 57.7% in Iran [2]. The World Health Organization (WHO) has identified the UI as one of the priorities in the health field as impacts the quality of life of older people because it affects different aspects of life and leads to psychological, physical, and social consequences [3]. Negative psychological effects of UI include anxiety, worry, frustration, tension and stress, bad temper, low self-esteem, and self-confidence. The prevalence of depression and anxiety among people with UI is reported to be about 20–40% and 56%, respectively [4]. According to previous studies, the UI prevalence among older adults has been estimated between 30 and 70% [5,6,7]. The UI prevalence is different in different regions of Iran so the prevalence of this syndrome in the Iranian female community is reported between 20 and 60%, this wide range can be attributed to the methodology or the age range of the participants in different studies [8,9,10,11].
It is difficult to assess the true prevalence of UI for cultural and social reasons. This syndrome is commonly underreported because most elderly people regard it as a consequence of aging and may even feel embarrassed to express it [12]. The three most common types of UI in women are stress urinary incontinence (SUI), urge urinary incontinence (UUI), or a combination of both, mixed urinary incontinence (MUI) [13]. In people with SUI, complaints of involuntary loss of urine during coughing, sneezing, and other physical exertions (e.g., sporting activities) increase intra-abdominal pressure, whereas the person with UUI suddenly feels the need to urinate (loss of urine associated with urgency). MUI is a combination of the symptoms of SUI and UUI. Other types of UIs that require more specialized detection include overflow and functional UIs [14].
Previous studies have reported numerous factors for the incidence or exacerbation of UI, including aging [11, 15,16,17], female gender [16,17,18], childbirth [11, 19, 20], obesity [18, 19, 21, 22], chronic diseases [17, 18, 23, 24], menopause [25, 26], polypharmacy [17, 27, 28] and movement limitations [17, 18, 25].
One of the main UI consequences is a decrease in the quality of life (QoL) of older adults [27, 29]. Evidence shows that UI affects QOL in a variety of ways, as there are many differences in people's perceptions and responses to UI symptoms. First, people with UI usually have more chronic illnesses than non-affected ones. In addition, fluid intake, mobility, and diuretic therapy may affect the UI [29]. Therefore, UI has negative effects on various aspects of life, especially QOL and the physical, social and psychological dimensions of health [29, 30].
It is difficult to assess the true prevalence of UI for cultural and social reasons. This syndrome is commonly underreported because most elderly people regard it as a consequence of aging and may even feel embarrassed to express it [12]. The three most common types of UI in women are stress urinary incontinence (SUI), urge urinary incontinence (UUI), or a combination of both, mixed urinary incontinence (MUI) [13]. In people with SUI, complaint of involuntary loss of urine during coughing, sneezing, and other physical exertion (e.g., sporting activities) increase intra-abdominal pressure, whereas the person with UUI suddenly feels the need to urinate (loss of urine associated with urgency). MUI is a combination of the symptoms of SUI and UUI. Other types of UIs that require more specialized detection include overflow and functional UIs [14].
Previous studies have reported numerous factors for the incidence or exacerbation of UI, including aging [11, 15,16,17], female gender [16,17,18], childbirth [11, 19, 20], obesity [18, 19, 21, 22], chronic diseases [17, 18, 23, 24], menopause [25, 26], polypharmacy [17, 27, 28] and movement limitations [17, 18, 25].
One of the main UI consequences is a decrease in the quality of life (QoL) of older adults [27, 29]. Evidence shows that UI affects QOL in a variety of ways, as there are many differences in people's perceptions and responses to UI symptoms. First, people with UI usually have more chronic illnesses than non-affected ones. In addition, fluid intake, mobility, and diuretic therapy may affect the UI [29]. Therefore, UI has negative effects on various aspects of life, especially QOL and the physical, social and psychological dimensions of health [29, 30].
On the other hand, women are more susceptible to this syndrome due to their anatomical, social, and cultural conditions, as well as due to pregnancy and childbirth, and menopause. UI causes many serious problems for the patient physically, mentally, and socially. It may affect relatives even more severely, and at the same time, this syndrome imposes huge economic costs. Due to the importance of this common syndrome in older adults and the fact that there has been no study on the relationship between the prevalence of UI and QOL among older adults, the present study aimed to determine the status of UI and related QOL in elderly women of Tabas, South Khorasan Province, Iran.
Methods
Study design and participants
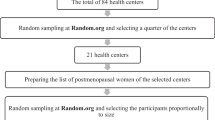
This cross-sectional study was conducted in Tabas city of South Khorasan province, Iran in 2020. The study population included 369 elderly women who were randomly selected. Inclusion criteria included age of 60 years and older living in urban areas of Tabas, and absence of cognitive problems based on the Persian version of the Mini-Mental State Examination (MMSE) test [31]. Exclusion criteria also included elderly women with deafness, severe disability, and lack of consent to participate in the study.
The required sample size was estimated at 369 people using 5% accuracy and the type I error = 0.05 using Cochran's formula. To select the participants, individuals were selected as a category in proportion to the number of people registered in the Iranian National Health System (INHS), in three urban of Tabas city (Kowsar, Golshan, and Golestan) after coordination with Tabas city health center. Tabas city has three comprehensive health centers. The total population of elderly women in Kosar, Golshan, and Golestan health centers is 879, 392, and 448 people, respectively. A total of 188, 85, and 96 people were randomly selected from Kowsar, Golshan, and Golestan health centers, respectively. They were invited to participate in the study and in person at healthcare centers. At first, the study purpose and method were explained to the participants, and after obtaining their consent, the questionnaires were completed in the form of face-to-face interviews in a private room where the elderly felt comfortable. The elderly women who were not able to come to the health center, the first author, referred to their homes and did the interviews for completing the questionnaires. All methods were carried out in accordance with relevant guidelines and regulations.
Instruments
The first section of the questionnaire includes demographic and background information including age, level of education, place of residence, weight, height, smoking, employment status, history of abortion, marital status, living situation, disability status, and having chronic diseases or common problems. Weight and height were measured by standard protocol. Body Mass Index (BMI) is a person’s weight in kilograms (or pounds) divided by the square of height in meters (or feet). The next sections of the questionnaire included the following instruments.
International consultation on incontinence questionnaire-short form (ICIQ-UI SF)
The ICIQ-UI-short form is a brief and psychometrically robust patient-completed questionnaire that evaluates the frequency, severity, and QOL-related impacts of UI in men and women in research and clinical practice across the world. It contains six questions that investigate a person's condition over the past four weeks. Questions 1 and 2 are demographic questions and question 3 includes the frequency of UI, question 4 measures the amount of leakage, and question 5 measure UI-related QOL impact. The scores obtained from questions 3, 4, and 5 represent the actual score. Question 6 focuses on the time and type of leakage. The possible score range is 0–21 with higher scores indicating increased severity [32]. The reliability and validity of the Persian version of ICIQ-SF have been approved in a study by Hajebrahimi et al. [33].
International consultation on incontinence questionnaire urinary incontinence quality of life module (ICIQ-LUTSqol)
The ICIQ-LUTSqol [34] is a psychometrically robust patient-completed questionnaire evaluating the quality of life (QoL) in UI patients in research and clinical practice. The ICIQ-LUTSqol consists of 20 items and each item has two sections. Section "a" of each item is entered into the outcomes calculator and contributes to the overall score. Section "b" of each item is a visual analog scale to assess the bother score (score range:0–10), which does not contribute to the overall score but is intended as a guide to clinicians to indicate the overall bother experienced by the patient. Bother scores, including question 22, have not been entered into the outcome calculator. The possible score range is 19 and 76, with lower scores indicating a better QoL status. However, sections of b are assessed on a 0–10 scale, where 0 means no bother and 10 means maximum bother/maximum impact on section a, i.e. QoL [35]. The reliability and validity of the Persian version of ICIQ-LUTSqol have been evaluated and approved by Pourmomeny et al. [35].
Statistical analysis
Data were collected and coded and then entered into SPSS and analyzed using descriptive tests. In descriptive statistics, mean, standard deviation, frequency and percentage, and minimum and maximum were used. Independent t-test and chi-square test were used to investigate the relationship between the studied variables and the UI, and the odds ratio of UI in terms of each variable when controlling other variables was determined using a logistic regression model.
Results
The mean ± SD of participants' age was 70.86 ± 8.27 years (range of 60–95 years). The majority of the participants had elementary education (57.5%) and were married. Of them, 36.3% had joint pain. Approximately, 66% of participants suffered from hypertension. Also, 35.8% of them had hyperlipidemia and 30% had diabetes (Tables 2 and 3, total column).
The prevalence of UI among the participants was 24.9%. The mean UI score was 6.29 ± 2.75 from the score range of 3 to 15. The most common UI was SUI among participants (40.2%). The least common UI in both groups was nighttime incontinence or nocturnal enuresis (Table 1).
The mean ± SD of the UI-QoL score was 38.04 ± 11.67 from the score range of 22–76. There was a positive and significant correlation between UI-related QoL score and UI score (r = 0.585, p < 0.001). There was also no significant difference between different UI types in terms of UI-related QoL (Table 2).
There was a statistically significant relationship between the prevalence of UI types with age, history of cesarean section, lifestyle, and regular drug use (p < 0.05). The prevalence of UI was 30% in people aged 80 years and older and 26.2% in the participants without a history of cesarean section. Also, the prevalence of this syndrome was 35% among elderly women who lived with their single children and 28.2% among those who were taking medication (Table 3).
There was also a statistically significant relationship between the prevalence of UI with cardiovascular diseases, respiratory diseases, arthritis and bone diseases, constipation, imbalance, joint pain, hypertension, digestive problems, sleep problems, and anorexia (P < 0.05) (Table 4).
According to the results of raw model regression analysis, the odds ratio of developing UI in elderly women with constipation was 2.7 times higher than those without constipation. Also, the odds ratio of developing UI increased by 6% with a one-unit increase in BMI. The odds ratio of developing UI in the elderly with hypertension was almost twice. According to the results of regression analysis in the adjusted model based on age, BMI, constipation, cesarean section, hypertension, and angiotensin receptor blockers, the odds ratio of developing UI in elderly women with constipation were 2.6 times higher than those without constipation. Also, the odds ratio of developing UI increased by 6% with a one-unit increase in BMI (Table 5).
Discussion
UI is one of the most common problems in old age that not only causes physical problems but also causes psychological, social, and economic problems as well as poor quality of life. The aim of the present study was to determine the status of UI and UI-related QoL in elderly women living in Tabas, South Khorasan Province, Iran. The prevalence of UI in elderly women was 24.9%. The UI prevalence was 33% and 25% in Amirkola city, Mazandaran province [8], and Khorasan, respectively [9]. The overall UI prevalence in Iranian women is estimated at 46% [10]. The prevalence of UI varies by country and in elderly women in the world was 37.1% based on a meta-analysis [36]. It can be stated that wide differences in the UI prevalence can be due to differences in research methods used, different cultures or races of study populations or the existence of different predisposing factors in those areas. Also, after observing the prevalence in different regions, it can be stated that the UI prevalence is quite diverse in different populations, which can be due to cultural and social differences. Estimating the UI incidence rate requires proven definitions of UI to prevent misinterpretation. It is shown that the different UI incidence rate in women is largely due to different UI definitions in each study. It also explains our problem when comparing the present data with the existing literature [37]. Following the current ICS definition, we used a validated questionnaire to standardize the UI definition and its diagnosis.
The most common type of UI in the present study was SUI which is consistent with the results of many studies [10, 11, 19, 38]. SUI following an increase in abdominal pressure is to such an extent that it overcomes the bladder blockage pressure. Abdominal pressure increases when coughing, sneezing, laughing, climbing stairs, or lifting objects. SUI is more prevalent among women due to pregnancy and childbirth, and also the decrease in estrogen production during the postmenopausal period also leads to muscle atrophy and consequent UI [39]. Also, the higher SUI incidence can also be due to various factors [10]. However, there are studies that have reported that other types of UI are more prevalent. For example, Pathiraja et al. [40] reported that UUI was more prevalent and Agarwal et al. also showed that UUI and mixed UI were more common [41] were the most common.
The results showed a statistically significant relationship between the UI prevalence with age, history of cesarean section, lifestyle, and drug use. That is, the UI prevalence was 30% in people aged 80 years and older and 26.2% in elderly women with a history of cesarean section. Also, the prevalence of this disorder was 35% among the elderly who lived with their single children. The majority of previous relevant studies revealed that UI prevalence in women increased with age [11, 19, 37, 42]. With age, anatomical and physiological changes of the urogenital system such as muscle and axon degeneration, decrease in bladder capacity, increase in detrusor activity and consequent decrease in detrusor contractile strength occur and as a result, elderly women are prone to UI [43]. Overall, increased UI prevalence in elderly women may be due to the relaxation of the pelvic floor muscles and connective tissue supporting the urethra.
Only 26% of the participants who had a history of cesarean section reported that they are suffering from UI, and the prevalence of UI was higher among women who had no history of cesarean section. The results of previous studies also have shown that vaginal delivery may be related to UI and not cesarean Section [44, 45]. Some other studies have not reported a definitive relationship between the mode of delivery and UI [46].
There was a statistically significant relationship between the prevalence of UI and drug use. The results of other studies also indicate the relationship between drug use and UI prevalence [8, 17, 27, 28]. “In principle, drugs could cause incontinence by lowering bladder outlet resistance and/or by increasing intravesical pressure, which disrupts the normal pressure relationship between the bladder and urethra and leads to urinary leakage; other possibilities include disturbances of the central nervous control of voiding or an overproduction of urine [47].”
The highest prevalence of UI was reported in the elderly with respiratory diseases was imbalance, anorexia, arthritis and bone diseases, and constipation, which is consistent with the results of other studies. Studies on the relationship between various diseases and UI have identified chronic respiratory patients as a risk factor for UI [17, 23, 48]. Increased abdominal pressure in chronic respiratory diseases associated with chronic cough, increases the pressure on the urethra, which in turn affects the supporting tissues of the pelvis, which ultimately can cause a UI in the individual. Constipation, arthritis, rheumatism, imbalance, and heart disease in various studies have been considered as risk factors for UI [8, 24, 49,50,51]. Constipation is strongly associated with UI due to high abdominal pressure, which increases urethra pressure and affects the pelvic supporting tissue. A fecal impaction can change the position of the pelvic organs and put pressure on the bladder, thereby reducing its ability to hold urine. UI also occurs due to an overactive bladder, urinary retention, and loss of sphincter control due to constipation [52, 53].
According to the results of regression analysis in the adjusted model based on age, BMI, constipation, cesarean section, hypertension and use of angiotensin receptor blockers, the odds ratio of developing UI in the women with constipation was 2.6 times higher than those without constipation. Also, the odds ratio of developing UI increases by 6% with a one-unit increase in BMI. The results of the present study are consistent with the results of other research. For example, in a meta-analysis of the relationship between constipation and UI risk [53], results showed that constipation was a major risk factor for UI. Obesity and high BMI [18, 19, 21] and chronic diseases [17, 18, 23, 24] are other predictors and risk factors for UI in elderly women.
UI-related QoL was low and had a significant positive correlation with the UI score. There was also no significant difference in the UI- related QoL in the affected elderly based on the types of UI. Coyne et al. [30] also reported poorer QoL in elderly people with SUI and mixed UI. The results of most studies indicate a relationship between UI and QoL and the elderly people had poorer QoL [19, 37, 41, 54]. People with UI usually have more chronic illnesses than non-affected ones. Many patients are reluctant to seek medical help or treatment because they think the disease is incurable, and feeling ashamed or scared. These patients usually avoid meeting friends, traveling, and participating in other social activities. As a result, they experience social isolation, psychological and physical consequences, and subsequent poor QoL [27, 55].
Conclusion
The prevalence of UI indicates this is a common condition and SUI is the most common type of IU among older women in the Iranian community that should be addressed by health care centers. Interventional programs for elderly people and their families about UI, risk factors such as aging, some chronic diseases, high BMI, and the use of some drugs and their management are essential for promoting their QoL.
Study limitations
The present study has been performed on a number of elderly women in Tabas, therefore, the present study imposes limitations in the field of generalizations, interpretations, and etiological citations of the studied variables due to its study population and the methodology that should be considered. The impossibility of matching the members of the research group in terms of variables, which affected the structures studied in the present study, was another limitation of the present study. For example, the participants were not selected from families with the same socioeconomic status. Elderly women may not reflect their true feelings when answering questions for reasons and attempts were made to minimize this limitation by emphasizing the confidentiality of the information sought. It is likely that the elderly’s situation affected their responses when filling out the questionnaires, which was beyond the researcher's control. All data were collected via patient interview (not patient recall by independently completing the surveys or by consulting with the medical record). Additionally, the educational level attained by the population is low. For these reasons, should be cautious about interpreting relationships between the findings.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318(16):1592–604.
Mostafaei H, Sadeghi-Bazargani H, Hajebrahimi S, Salehi-Pourmehr H, Ghojazadeh M, Onur R, et al. Prevalence of female urinary incontinence in the developing world: a systematic review and meta-analysis—a report from the developing world committee of the international continence society and Iranian research center for evidence based medicine. Neurourol Urodyn. 2020;39(4):1063–86.
Organization WH. Integrated care for older people (ICOPE) Guidelines on community-level interventions to manage declines in intrinsic capacity Evidence profile: urinary incontinence: World Health Organization 2017 [Available from: file:///C:/Users/Administrator/Downloads/WHO-MCA-17.06.08-eng%20(1).pdf.
Bilgic D, Beji NK, Ozbas A, Cavdar İ, Yalcin O. Approaches to cope with stress and depression in individuals with urinary incontinence. Gynecol Obstet Invest. 2017;82(2):181–7.
Roe B, Flanagan L, Jack B, Barrett J, Chung A, Shaw C, et al. Systematic review of the management of incontinence and promotion of continence in older people in care homes: descriptive studies with urinary incontinence as primary focus. J Adv Nurs. 2011;67(2):228–50.
Silay K, Akinci S, Ulas A, Yalcin A, Silay Y, Akinci M, et al. Occult urinary incontinence in elderly women and its association with geriatric condition. Eur Rev Med Pharmacol Sci. 2016;20(3):447–51.
Stenzelius K, Molander U, Odeberg J, Hammarström M, Franzen K, Midlöv P, et al. The effect of conservative treatment of urinary incontinence among older and frail older people: a systematic review. Age Ageing. 2015;44(5):736–44.
Moudi E, Samadi F, Hosseini S, Bijani A, Ghadimi R. Urinary incontinency in elderly women and the potential risk factors: a cohort study among the elderly women of Amirkola. J Babol Univ Med Sci. 2017;19(2):14–9.
Tashakori M, Moghimi A, Pilevaryan AA, Moghimian M. Study of severity and prevalence of stress incontinent in menopausal working women in Khorasan. Iran J Obstet Gynecol Infertil. 2006;9(2):47–52.
Rashidi F, Hajian S, Darvish S, Alavi MH. Prevalence of urinary incontinence in Iranian women: systematic review and meta-analysis. Iran J Obstet Gynecol Infertil. 2019;21(12):94–102.
Morowatisharifabad MA, Rezaeipandari H, Mazyaki A, Bandak Z. Prevalence of urinary incontinence among elderly women in Yazd, Iran: a population-based study. Elderly Health Journal. 2015;1(1):27–31.
Elenskaia K, Haidvogel K, Heidinger C, Doerfler D, Umek W, Hanzal E. The greatest taboo: urinary incontinence as a source of shame and embarrassment. Wien Klin Wochenschr. 2011;123(19):607–10.
Åström Y, Asklund I, Lindam A, Sjöström M. Quality of life in women with urinary incontinence seeking care using e-health. BMC Womens Health. 2021;21(1):1–9.
Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Ho C, Teo C, Phang L, Azizi N, Darwin F, Mohd Ghazi N, et al. Prevalence and risk factors associated with overactive bladder. Urotoday Int J. 2012;5(1):88.
Wu JM, Matthews CA, Vaughan CP, Markland AD. Urinary, fecal, and dual incontinence in older US Adults. J Am Geriatr Soc. 2015;63(5):947–53.
Marques LP, Schneider IJC, Giehl MWC, Antes DL, d’Orsi E. Demographic, health conditions, and lifestyle factors associated with urinary incontinence in elderly from Florianópolis, Santa Catarina, Brazil. Rev Bras Epidemiol. 2015;18:595–606.
Tamanini JTN, Lebrão ML, Duarte YA, Santos JL, Laurenti R. Analysis of the prevalence of and factors associated with urinary incontinence among elderly people in the Municipality of São Paulo, Brazil: SABE study (Health, Wellbeing and Aging). Cad Saude Publica. 2009;25:1756–62.
Al Kiyumi MH, Al Belushi ZI, Jaju S, Al Mahrezi AM. Urinary incontinence among omani women: prevalence, risk factors and impact on quality of life. Sultan Qaboos Univ Med J. 2020;20(1): e45.
Dehghan Manshadi F, Ghanbari Z, Jabbari Z, Miri E. Urinary incontinence, its related disorders and risk factors in women. J Sch Public Health Inst Public Health Res. 2013;11(2):53–63.
Erekson EA, Cong X, Townsend MK, Ciarleglio MM. Ten-year prevalence and incidence of urinary incontinence in older women: a longitudinal analysis of the health and retirement study. J Am Geriatr Soc. 2016;64(6):1274–80.
Bolina AF, Dias FA, de Freitas Santos NM, dos Santos Tavares DM. Self-reported urinary incontinence in elderly and its associated factors. Rev Rene. 2013;14(2).
Park J, Hong G-RS, Yang W. Factors associated with self-reported and medically diagnosed urinary incontinence among community-dwelling older women in Korea. Int Neurourol J. 2015;19(2):99.
Asemota O, Eldemire-Shearer D, Waldron NK, Standard-Goldson A. Prevalence of Self-reported urinary incontinence in community-dwelling older adults of Westmoreland. Jam MEDICC Rev. 2016;18:41–5.
Silva JCPd, Soler ZASG, DominguesWysocki A. Associated factors to urinary incontinence in women undergoing urodynamic testing. Rev Escola Enferm USP. 2017. https://doi.org/10.1590/s1980-220x2016140903209.
Townsend M, Lajous M, Medina-Campos R, Catzin-Kuhlmann A, López-Ridaura R, Rice M. Risk factors for urinary incontinence among postmenopausal Mexican women. Int Urogynecol J. 2017. https://doi.org/10.1007/s00192-016-3196-0.
Kim KJ, Shin J, Choi J, Park J-M, Park HK, Lee J, et al. Association of geriatric syndromes with urinary incontinence according to sex and urinary-incontinence–related quality of life in older inpatients: a cross-sectional study of an acute care hospital. Korean J Fam Med. 2019;40(4):235.
Reigota RB, Pedro AO, de Souza Santos Machado V, Costa-Paiva L, Pinto-Neto AM. Prevalence of urinary incontinence and its association with multimorbidity in women aged 50 years or older: a population-based study. Neurourol Urodyn. 2016;35(1):62–8.
Pizzol D, Demurtas J, Celotto S, Maggi S, Smith L, Angiolelli G, et al. Urinary incontinence and quality of life: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33(1):25–35.
Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101(11):1388–95.
Seyedian MFM, Nowroozian M, Nejat S, Delavar A, Ghasemzadeh H. Preparing and determining the validity of the persian version of the mini mental state examination. J Med Council Iran. 2007;25(4):408–14.
Avery KDJ, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure forevaluating the symptoms and impact of urinaryincontinence. Neurourol Urodyn. 2004;23(4):322–30.
Hajebrahimi S, Nourizadeh D, Hamedani R, Pezeshki MZ. Validity and reliability of the international consultation on incontinence questionnaire-urinary incontinence short form and its correlation with urodynamic findings. Urol J. 2012;9(4):685–90.
Kelleher C, Cardozo L, Khullar V, Salvatore S. A new questionnaire to assess the qualityof life of urinary incontinent women. BJOG. 1997;104:1374–9.
Pourmomeny AA, Zargham M, Fani M. Reliability and validity of the quality of life questionnaire in Iranian patients with lower urinary tract symptoms. LUTS Lower Urin Tract Symptoms. 2018;10(1):93–100.
Batmani S, Jalali R, Mohammadi M, Bokaee S. Prevalence and factors related to urinary incontinence in older adults women worldwide: a comprehensive systematic review and meta-analysis of observational studies. BMC Geriatr. 2021;21(1):1–17.
Tamanini JTN, Pallone LV, Sartori MGF, Girão MJBC, Dos Santos JLF, de Oliveira Duarte YA, et al. A populational—based survey on the prevalence, incidence, and risk factors of urinary incontinence in older adults—results from the “SABE STUDY.” Neurourol Urodyn. 2018;37(1):466–77.
Altaweel W, Alharbi M. Urinary incontinence: prevalence, risk factors, and impact on health related quality of life in Saudi women. Neurourol Urodyn. 2012;31(5):642–5.
Fillit HM, Rockwood K, Young JB. Brocklehurst's textbook of geriatric medicine and gerontology E-book: Elsevier Health Sciences; 2016.
Pathiraja R, Prathapan S, Goonawardena S. Urinary incontinence of women in a nationwide study in Sri Lanka prevalence and risk factors. Urol J. 2017;14(3):3075–80.
Agarwal BK, Agarwal N. Urinary incontinence: prevalence, risk factors, impact on quality of life and treatment seeking behaviour among middle aged women. Int Surg J. 2017;4(6):1953–8.
Murukesu RR, Singh DK, Shahar S. Urinary incontinence among urban and rural community dwelling older women: prevalence, risk factors and quality of life. BMC Public Health. 2019;19(4):1–11.
Abrams P, Andersson K-E, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth international consultation on incontinence recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn Off J Int Cont Soc. 2010;29(1):213–40.
Van Brummen HJ, Bruinse HW, Van De Pol G, Heintz APM, Van Der Vaart CH. Bothersome lower urinary tract symptoms 1 year after first delivery: prevalence and the effect of childbirth. BJU Int. 2006;98(1):89–95.
Parashi S, Kashanian M, Niknafs F. Evaluation of the relationship between the mode of first delivery and stress urinary incontinence after 1 year. Razi J Med Sci. 2009;15:47–53.
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348(10):900–7.
Tsakiris POM, Michel MC. Drug-induced urinary incontinence. Drugs Aging. 2008;25(7):541–9.
Abrams P, Andersson K-E, Apostolidis A, Birder L, Bliss D, Brubaker L, et al. 6th international consultation on incontinence. recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2.
Carneiro JA, Ramos GCF, Barbosa ATF, Medeiros SM, Lima CDA, Costa FMD, et al. Prevalência e fatores associados à incontinência urinária em idosos não institucionalizados. Cadernos Saúde Coletiva. 2017;25:268–77.
Bresee C, Dubina ED, Khan AA, Sevilla C, Grant D, Eilber KS, et al. Prevalence and correlates of urinary incontinence among older, community-dwelling women. Female Pelvic Med Reconstr Surg. 2014;20(6):328.
Sensoy N, Dogan N, Ozek B, Karaaslan L. Urinary incontinence in women: prevalence rates, risk factors and impact on quality of life. Pak J Med Sci. 2013;29(3):818.
Eshkoor S, Hamid TA, Shahar S, Mun C. Factors related to urinary incontinence among the Malaysian elderly. J Nutr Health Aging. 2017;21(2):220–6.
Lian W-Q, Li F-J, Huang H-X, Zheng Y-Q, Chen L-H. Constipation and risk of urinary incontinence in women: a meta-analysis. Int Urogynecol J. 2019;30(10):1629–34.
Kessler M, Facchini LA, Soares MU, Nunes BP, França SM, Thumé E. Prevalence of urinary incontinence among the elderly and relationship with physical and mental health indicators. Rev Bras Geriatr Gerontol. 2018;21:397–407.
Göral Türkcü S, Kukulu K. Urinary incontinence and quality of life of women living in nursing homes in the Mediterranean region of Turkey. Psychogeriatrics. 2017;17(6):446–52.
Acknowledgements
The present study is the result of the master's thesis of the International Campus of Shahid Sadoughi University of Medical Sciences in Yazd. Hereby, the authors would like to express their thanks to the managers of Tabas health centers and all the elderly women who participated in the present study.
Funding
This study was not funded by any organization.
Author information
Authors and Affiliations
Contributions
ZN, MAM, HR and RH contributed to the study conception and design. Material preparation, data collection and analysis were performed by ZN, HR, SJ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of the School of Public Health in Shahid Sadoughi University of Medical Sciences, Yazd, Iran (IR.SSU.SPH.REC.1399.035). The aim, methodology and voluntary participation were explained to the participants and they were assured that all their information would was kept confidential. Informed consent was also obtained from all older adults (from legal representative/guardians of the illiterate participants).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Najafi, Z., Morowatisharifabad, M.A., Jambarsang, S. et al. Urinary incontinence and related quality of life among elderly women in Tabas, South Khorasan, Iran. BMC Urol 22, 214 (2022). https://doi.org/10.1186/s12894-022-01171-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-022-01171-9