Abstract
Background
Recently, presepsin has been reported to be a useful biomarker for early diagnosis of sepsis and evaluation of prognosis in septic patients. However, few reports have evaluated its usefulness in patients with urinary tract infections (UTI). This study aimed to evaluate whether presepsin could be a valuable marker for detecting severe sepsis, and whether it could predict the therapeutic course in patients with UTI compared with markers already used: procalcitonin (PCT) and C-reactive protein (CRP).
Methods
From April 2014 to December 2016, a total of 50 patients with urinary tract infections admitted to Gunma university hospital were enrolled in this study. Vital signs, presepsin, PCT, CRP, white blood cell (WBC) count, causative agents of urinary-tract infections, and other data were evaluated on the enrollment, third, and fifth days. The patients were divided into two groups: with (n = 11) or without (n = 39) septic shock on the enrollment day, and with (n = 7) or without (n = 43) sepsis on the fifth day, respectively. Presepsin was evaluated as a biomarker for systemic inflammatory response syndrome (SIRS) or septic shock.
Results
Regarding the enrollment day, there was no significant difference of presepsin between the SIRS and non-SIRS groups (p = 0.276). The median value of presepsin (pg/mL) was significantly higher in the septic shock group (p < 0.001). Multivariate logistic regression analysis showed that presepsin (≥ 500 pg/ml) was an independent risk factor for septic shock (p = 0.007). ROC curve for diagnosing septic shock indicated an area under the curve (AUC) of 0.881 for presepsin (vs. 0.690, 0.583, and 0.527 for PCT, CRP and WBC, respectively). Regarding the 5th day after admission, the median presepsin value on the enrollment day was significantly higher in the SIRS groups than in the non-SIRS groups (p = 0.006). On the other hand, PCT (≥ 2 ng/ml) on the enrollment day was an independent risk factor for SIRS. ROC curve for diagnosing sepsis on the fifth day indicated an AUC of 0.837 for PCT (vs. 0.817, 0.811, and 0.802 for presepsin, CRP, and WBC, respectively).
Conclusions
This study showed that presepsin may be a good marker for diagnosing septic shock based on admission data in patients with UTI.
Similar content being viewed by others
Background
Urinary tract infections (UTI) are common, and sometimes progress to sepsis or septic shock, which can be lethal. Mortality rate due to severe sepsis and septic shock has been reported to be between 20 and 50% [1, 2], and 9–31% of all cases of severe sepsis and septic shock has been reported to arise from UTI [2]. Therefore, diagnosis and evaluation of severity of sepsis or septic shock are important at the beginning of treatment of UTI.
Clinically, C-reactive protein (CRP) and procalcitonin (PCT) are used as markers for disease severity in patients with UTI. However, both CRP and PCT have some limitations. The response time to bacterial infections is delayed (CRP, 6 h; PCT, 2–3 h), production triggers might not be living bacteria (CRP, cytokine; PCT, endotoxin and cytokine), and serum half-time is long (CRP, 4–6 h; PCT, 20–24 h) [3, 4]. Therefore, a novel biomarker for bacterial infection, which reflects clinical condition at the time of measurement, is required.
Presepsin is a 13KDa N-terminal fragment of soluble CD14 [5]. Granulated leukocytes phagocytose both bacteria and CD14 and expel presepsin into the blood after enzymatic digestion of bacteria within two hours [5, 6]. Recently, presepsin has been reported to have a high sensitivity in detecting sepsis and be a biomarker for early diagnosis of sepsis [7]. Moreover, elevated presepsin levels on day one might evaluate prognosis of patients with sepsis in intensive-care units [8, 9]. However, there are a few reports on the use of presepsin as a biomarker in patients with UTI.
This study aimed to evaluate whether presepsin could be a useful marker for detecting sepsis or severe sepsis, and whether it could predict therapeutic courses in patients with UTI compared with other markers, such as PCT or CRP.
Methods
Patients
We performed a prospective observational study. From April 2014 to December 2016, a total of 57 patients with UTI, who were admitted into Gunma university hospital, were enrolled in this study. Seven patients were excluded from this study due to data unavailability. The urologist diagnosed UTI based on urinary sediment (≥ 5 leucocytes/high power field) and symptoms (fever and/or micturition pain and/or flank pain). Data of patient age, sex, medical history, oral medicine, blood pressure, body temperature, heart rate, respiratory rate, urine and blood culture results, surgical procedure for UTI after admission, causative agents of UTI, presepsin, PCT, CRP, white blood cell (WBC), Aspartate transaminase (ALT), Alanine transaminase (AST), γ-glutamyl transpeptidase (γGPT), and Creatinine (Cr) were collected. Vital signs and blood test results were evaluated at enrollment, and on the 3rd and 5th day after admission. The written informed consent was obtained from all of the enrolled patients. This study was approved by the Institutional Review Board of Gunma University Hospital (No.1650).
Assessment of systemic inflammatory response syndrome (SIRS) and septic shock
Diagnosis of SIRS and septic shock were established according to the criteria set by the American College of Chest Physicians/Society of Critical Care Medicine (ACCP/SCCM) [10].
Outcomes
Three outcome variables: SIRS and septic shock on the enrollment day and SIRS on the 5th day after admission were evaluated by dividing the participants into two groups for each of these variables; with (n = 39) or without (n = 11) SIRS on the enrollment day, with (n = 11) or without (n = 39) septic shock on the enrollment day, and with (n = 7) or without (n = 43) SIRS on the 5th day after admission, respectively.
Statistical analysis
Mann–Whitney U-test was used for continuous variables (age, CRP, presepsin, PCT, ALT, AST, γGPT, and Cr). We estimated independence using the chi-squared test or Fisher`s exact test for categorical variables (sex, placement of urinary catheter, urological cancer, urinary calculi, diabetes mellitus, and internal use of steroids). Independent predictors were evaluated using logistic regression analysis. The predictive accuracy of presepsin, PCT, CRP and WBC for septic shock or SIRS was evaluated by the area under the curve (AUC) of receiver operating characteristics (ROC) analysis. The Youden's index (sensitivity + specificity—1) was used to calculate optimal cutoff values for presepsin. P values ≤ 0.05 were considered statistically significant. SPSS Statistics Ver. 25 (IBM Corp. IL, USA) was used for statistical analyses.
Results
Patients characteristic
Table 1 shows the clinical characteristics of the 50 patients. On the enrollment day, septic shock was detected in 22% (n = 11) and SIRS in 78% (n = 39) of the patients. The mean age was 66.5 years, and 33 patients (66%) were men and 17 (34%) were women. Urine and blood cultures were positive and revealed bacterial growth in in 90% (n = 45) and 48% (n = 24) of samples, respectively. Forty-eight% (n = 24), 30% (n = 15), 24% (n = 12), 18% (n = 9), 56% (n = 28), and 18% (n = 9) were with placement of urinary catheter, urological cancer, urinary calculi, diabetes mellitus, surgical procedure after admission, and internal use of steroids, respectively.
Prediction of SIRS on the enrollment day
The overall median baseline presepsin, PCT, and CRP levels were 483 pg/mL, 0.87 ng/mL, and 10.45 mg/L, respectively, with no significant difference between the SIRS and non-SIRS groups (Additional file 1: Table S1).”
Prediction of septic shock on the enrollment day
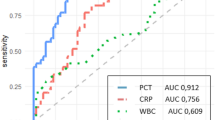
The median presepsin level (pg/mL) was significantly higher in the septic shock group (1380 vs. 399, p < 0.001). The PCT and CRP levels were not significantly different between the septic shock and non-septic shock groups. Other blood test results that were significantly higher in the septic group included: AST (p = 0.003), ALT (p = 0.049), γGTP (p = 0.002 and Cr (p = 0.02), respectively (Table 1). Logistic regression analysis for evaluating factors associated with septic shock on the enrollment day is shown in Table 2. The factors associated with septic shock on univariate analysis included presepsin (≥ 500 pg/mL), PCT (≥ 2 ng/ml), AST (≥ 34 U/L) and γGTP (≥ 47 U/L). Only presepsin level retained a significant value after adjusting for confounders using multivariate logistic regression analysis (Table 2). ROC curve for diagnosing septic shock indicated an AUC of 0.881 for presepsin, which was greater than these for other markers (Fig. 1). The Cutoff level of presepsin with the optimum diagnostic efficiency by the ROC curves was 492 ng/ml, which was broadly similar to the clinical cut off value (500 pg/mL).
Prediction of SIRS on the 5th day after admission
The median presepsin level (pg/mL) was significantly higher in the SIRS group on the 5th day after admission (day1; 1167 vs. 419, p < 0.001, day3; 633 vs. 311, p = 0.027). The PCT (day1: 73.1 vs. 0.55, p = 0.003; day3: 20.34 vs. 1.35, p = 0.005)) and CRP (day1: 25.63 vs. 8.23, p = 0.007; day3: 25.58 vs. 10.71, p < 0.001) levels were also significantly different between the SIRS and non-SIRS groups on the 5th day after admission. Other blood test results that were significantly higher in the SIRS group on the 5th day after admission included: day1/AST (34 vs. 24, P = 0.013); day1/Cr (2.3 vs. 1.05, p = 0.007); day1/WBC (18,200 vs. 13,600, p = 0.009); and day3/WBC (11,900 vs. 8400, p = 0.021) (Table 3). The ratio of positive blood culture (86% vs. 42%, p = 0.039) and urinary calculi (57% vs. 19%, p = 0.048) significantly differed between the SIRS and non-SIRS groups on the 5th day after admission. Logistic regression analysis to evaluate factors associated with SIRS on the 5th day after admission is shown in Table 4. These factors included day1/presepsin (≥ 500 pg/mL), day1/PCT (≥ 2 ng/ml) and urinary calculi. Only day1/PCT level retained statistical significance after adjusting for confounders using multivariate logistic regression analysis (Table 4). ROC curve in patients with definitive diagnosis of SIRS on the 5th day after admission indicated an AUC of 0.837 for PCT, which is larger than these for other markers (Fig. 1). Regarding presepsin, the cutoff level with the optimum diagnostic efficiency using the ROC curves was 492 ng/ml, which was broadly similar to the clinical cut off value (500 pg/mL).
Discussion
In this study, elevated presepsin level on admission was an independent risk factor for septic shock, while elevated PCT on admission was independently associated with SIRS on the 5th day after admission in patients with UTI. Presepsin and PCT originate from different sources [3,4,5]. These results support our hypothesis that presepsin could be a useful marker for detecting severe sepsis in patients with UTI. On the other hand, PCT could predict therapeutic courses in patients with UTI better than did presepsin.
Presepsin is one of the biomarkers that increase after bacterial infections [11]. Its levels are increased in acute pyelonephritis patients with bacteremia [12]. Moreover, elevation of presepsin levels before initiating treatment might predict the development of sepsis in patients with obstructive acute pyelonephritis [13]. In this study, we evaluated the patients who needed hospitalization due to not only pyelonephritis, but also prostatitis. Additionally, elevation of presepsin levels on the enrollment day was a predictor of septic shock. Therefore, presepsin might be a useful for detecting severe urosepsis that needs vasopressor therapy.
Sever sepsis and septic shock can be fatal, with mortality rates: 28.3% in the United States and 41.1% in Europe [2]. Clinically, it is very useful to predict septic shock on admission. Therefore, it is essential that biomarkers increase immediately after infections and have high sensitivity for sepsis to be reliable. Presepsin levels have been shown to increase within 2 h together with blood bacterial counts, and peak at 3 h after infection [6]. On the other hand, elevated PCT and CRP levels are detected within 3–6 and 6 h, and peak at 6–8 and 36–50 h, respectively [14, 15]. It has also been reported that patients with severe sepsis had significantly higher presepsin levels than did those with sepsis, local infection, or SIRS [16]. In this study, elevation of presepsin levels on the enrollment day was a predictor of septic shock, not of SIRS. These results suggest that presepsin may be used to identify patients at increased risk of more severe infections at early stages.
One important characteristic of biomarkers is their prognostic values. Presepsin levels on day 1 were reported to be correlated with 60-day in-hospital mortality in patients with sepsis, severe sepsis, or septic shock [17]; a longer intensive-care unit stay; and a lower degree of resolution of primary infection [8, 9]. Mortality is one of the prognostic variables. Since there were no mortalities in this current study, we used presence or absence of SIRS on day 5 for prognosis. In this study, the levels of presepsin were significantly higher in the SIRS group than in the non-SIRS group on day 5 after admission. However, the levels of PCT on day1 were only identified as a predictor of SIRS on day5 using multivariate logistic regression analysis. Regarding PCT, the AUC for PCT to predict 30-day mortality in patients with febrile UTI was reported to be 0.71 (95% CI: 0.56–0.85) [18]. There are a few reports that compared between presepsin and PCT for evaluating their prognostic values in patients with UTI. Further research that includes a large sample size of patients with severe urosepsis than does this study is needed to evaluate the reliability of each of these biomarkers for predicting treatment outcomes.
This study has several limitations. First, since 2016, sepsis has been defined according to the Sequential (Sepsis-Related) Organ Failure Assessment (SOFA) [19]. This study began in 2014, and we did not assess the level of consciousness, which is a requirement for the SOFA scoring. Therefore, instead of the SOFA, SIRS criteria [10] were used for defining sepsis and septic shock. Second, this study might have been limited by its single-center design and small sample size. Third, we did not consider renal function in setting the reference values of presepsin and PCT. The levels of presepsin and PCT have been previously reported to be affected by renal function [20, 21]. It would have been ideal to set the reference values depending on assessment of renal function. However, these adjustments are yet to be clarified. Fourth, all patients were discharged from our hospital alive in this study. However, it has been reported that severe sepsis and septic shock could be fatal, with mortality rate of 28.3%-41.1% [2]. Regarding 11 patients with septic shock on the enrollment day, seven patients were without SIRS on the fifth day. Six patients underwent surgical procedures out of these seven patients, and it seems that the combination of antibiotics and surgical procedures might have been quite effective. There is a possibility that these patients might have not needed any vasopressors infusion in the course of treatments. Moreover, the number of patients was not enough to evaluate presepsin for detecting severe sepsis and predicting the therapeutic course in comparison with PCT and CRP. Further research with a larger number of patients is needed.
Conclusions
This study showed that, in patients with UTI, presepsin may be a good marker for diagnosis of septic shock based on the data of admission.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALT:
-
Aspartate transaminase
- AST:
-
Alanine transaminase
- AUC:
-
The area under the curve
- Cr:
-
Creatinine
- CRP:
-
C-reactive protein
- γGPT:
-
γ-Glutamyl transpeptidase
- PCT:
-
Procalcitonin
- ROC:
-
A receiver operating characteristics
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
The Sequential Organ Failure Assessment
- UTI:
-
Urinary tract infections
- WBC:
-
White blood cell
References
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Levy MM, Artigas A, Phillips GS, Rhodes A, Beale R, Osborn T, et al. Outcomes of the surviving sepsis campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 2012;12:919–24.
Brunkhorst FM, Heinz U, Forycki ZF. Kinetics of procalcitonin in iatrogenic sepsis. Intensive Care Med. 1998;24:888–9.
Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994;79:1605–8.
Yaegashi Y, Shirakawa K, Sato N, Suzuki Y, Kojika M, Imai S, et al. Evaluation of a newly identified soluble CD14 subtype as a marker for sepsis. J Infect Chemother. 2005;11:234–8.
Nakamura M, Takeuchi T, Naito K, Shirakawa K, Hosaka Y, Yamasaki F, et al. Early elevation of plasma soluble CD14 subtype, a novel biomarker for sepsis, in a rabbit cecal ligation and puncture model. Crit Care. 2008;12(Suppl 2):194.
Zou Q, Wen W, Zhang XC. Presepsin as a novel sepsis biomarker. World J Emerg Med. 2014;5:16–9.
Masson S, Caironi P, Fanizza C, Thomae R, Bernasconi R, Noto A, et al. Circulating presepsin (soluble CD14 subtype) as a marker of host response in patients with severe sepsis or septic shock: data from the multicenter, randomized ALBIOS trial. Intensive Care Med. 2015;41:12–20.
Kim H, Hur M, Moon HW, Yun YM, Di Somma S. Multi-marker approach using procalcitonin, presepsin, galectin-3, and soluble suppression of tumorigenicity 2 for the prediction of mortality in sepsis. Ann Intensive Care. 2017;7:27.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644–55.
Memar MY, Baghi HB. Presepsin: a promising biomarker for the detection of bacterial infections. Biomed Pharmacother. 2019;111:649–56.
Claessens Y-E, Trabattoni E, Grabar S, Quinguis L, Sahakian G, Anselmo M, et al. Plasmatic presepsin (sCD14-ST) concentrations in acute pyelonephritis in adult patients. Clin Chim Acta. 2017;464:182–8.
Tambo M, Taguchi S, Nakamura Y, Okegawa T, Fukuhara H. Presepsin and procalcitonin as predictors of sepsis based on the new sepsis-3 definitions in obstructive acute pyelonephritis. BMC Urol. 2020;20:23.
Maruna P, Nedelníková K, Gürlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000;49(Suppl 1):57–61.
Lelubre C, Anselin S, Boudjeltia KZ, Biston P, Piagnerelli M. Interpretation of C-reactive protein concentrations in critically ill patients. Biomed Res Int. 2013;2013:124021.
Shozushima T, Takahashi G, Matsumoto N, Kojika M, Okamura Y, Endo S. Usefulness of presepsin (sCD14-ST) measurements as a marker for the diagnosis and severity of sepsis that satisfied diagnostic criteria of systemic inflammatory response syndrome. J Infect Chemother. 2011;17:764–9.
Ulla M, Pizzolato E, Lucchiari M, Loiacono M, Soardo F, Forno D, et al. Diagnostic and prognostic value of presepsin in the management of sepsis in the emergency department: a multicenter prospective study. Crit Care. 2013;17:R168.
Starre WE, Zunder SM, Vollaard AM, Nieuwkoop CV, Stalenhoef JE, Delfos NM, et al. Prognostic value of pro-adrenomedullin, procalcitonin and C-reactive protein in predicting outcome of febrile urinary tract infection. Clin Microbiol Infect. 2014;20:1048–54.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Nakamura Y, Ishikura H, Nishida T, Kawano Y, Yuge R, Ichiki R, et al. Usefulness of presepsin in the diagnosis of sepsis in patients with or without acute kidney injury. BMC Anesthesiol. 2014;14:88.
Amour J, Birenbaum A, Langeron O, Le Manach Y, Bertrand M, Coriat P, et al. Influence of renal dysfunction on the accuracy of procalcitonin for the diagnosis of postoperative infection after vascular surgery. Crit Care Med. 2008;36:1147–54.
Acknowledgements
We thank Ms. Atsuko Oyama, and Ms. Rie Suzuki for their technical assistance.
Funding
No funding sources.
Author information
Authors and Affiliations
Contributions
YSe perfomed project development, data collection, data analysis and manuscript writing. KK contributed to project development and manuscript editing. DO, HN, YM, TS, SA, MN, HK, HM and YSh contributed to data collection. MM contributed to data analysis. KS contributed to project developments. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study was approved by the Ethical Committee of Gunma University (Approval No. 1650), and written informed consent was obtained from all of the enrolled patients to use their tissues. It was performed in accordance with the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Supplemental Table 1.
Characteristics of Patients with or without SIRS on the enrollment day.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sekine, Y., Kotani, K., Oka, D. et al. Presepsin as a predictor of septic shock in patients with urinary tract infection. BMC Urol 21, 144 (2021). https://doi.org/10.1186/s12894-021-00906-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-021-00906-4