Abstract
Background
The neuroendocrine cells can cause a variety of malignancies throughout the human body known as the neuroendocrine tumors (NETs) or carcinoid tumors. The primary testicular carcinoid tumor (PTCT) accounts for less than 1% of the testicular neoplasms and for only 0.2% of all carcinoid tumors representing already a very rare neoplastic entity. Here, we present a patient with a history of an exceptionally rare primary testicular carcinoid tumor, staining positive for Cdx-2 along with a literature review.
Case presentation
A 44-year old patient without significant past medical history was diagnosed in September 2009 with primary testicular carcinoid tumor, which was surprisingly staining positively for Cdx-2, too. At the time of the initial diagnosis the tumor was already showing histopathological infiltration of veins. DOTA-TATE-PET/CT imaging and endoscopy studies did not show any signs of distant metastases and in particular no gastrointestinal manifestation following no further medical indication for systemic chemotherapy. The continuous and close follow-up of the patient has reached a total of over 10 years at the time of publication remaining in complete remission.
Conclusion
The diagnosis of primary testicular carcinoid is based on histopathology. The detailed histopathologic assessment of biomarkers based on immunohistochemistry is very important for the classification and the prognosis of the primary testicular carcinoid tumor. Primary testicular carcinoid tumor with Cdx-2 positive stain outlines an exceptionally rare neoplastic entity without a consensus about general follow-up guidelines, requiring close clinical and imaging aftercare and consideration in Cdx-2 positive metastatic tumor of unknown origin.
Similar content being viewed by others
Background
The neuroendocrine cells can cause a variety of malignancies throughout the human body known as the neuroendocrine tumors (NETs). These types of tumors, likewise called carcinoid tumors, are able to produce hormone-like molecules, which can mimic characteristic hormonal syndromes [1]. Carcinoid tumors occur predominantly in the gastrointestinal tract (67.5%) and in the bronchopulmonary system (25.3%) [2]. The primary testicular carcinoid tumor (PTCT) accounts for less than 1% of the testicular neoplasms [3] and for only 0.2% of all carcinoid tumors representing a very rare neoplastic entity [4, 5]. The distinction of the origin in primary or metastatic circumstance is of the outmost importance for the prognosis of the testicular carcinoid tumor and the treatment [6]. Here, we present a case history of a primary testicular carcinoid tumor with exceptionally rare Cdx-2 positive stain and complete remission along with 10 years recurrence-free follow-up and a literature review.
Case presentation
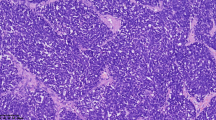
We report a 44-year old patient, who saw his urologist in September 2009 due to a painless and for approximately 6 month continuously growing left testicular swelling. The patient did not report any further clinical signs or symptoms of general disease especially no history of sudden hot flushes. The past medical history reveals solely strumectomy due to Grave’s disease and atopic diathesis. On clinical exam no additional noticeable problems aside the one-sided testicular mass, especially no inguinal lymphadenopathy, were detected. The complete blood count and metabolic panel studies were all in normal range. Due to suspected testicular malignancy on clinical exam the patient underwent a near-time radical inguinal left-sided orchiectomy. The histological analysis of the testicular tissue revealed the diagnosis of a primary testicular carcinoid tumor, which was positive for chromogranin A, CD56, Ep4 and Cdx-2. The nuclear MIB-1 expression was detected in patches of the tumor cells with an MIB-1 index of approximately 2% (Fig. 1). At the time of the initial diagnosis the tumor was already showing histopathological infiltration of veins (cN0, cM0, R0 and V1). However the 24-h urine study showed a normal level of 5-Hydroxyindolacetic acid. Based on these findings the patient subsequently underwent DOTA-TATE-PET/CT imaging and endoscopy studies showing no signs of distant metastases and in particular no gastrointestinal manifestation following no further medical indication for systemic chemotherapy. Furthermore the patient was undergoing continuous clinical, abdominal sonography and imaging postsurgical care (Fig. 2). The follow-up of the patient has reached a total of over 10 years at the time of publication remaining in complete remission.
Histological and immunohistochemical analysis of primary testicular carcinoid tumor tissue. Histological analysis (H&E staining) shows nested cuboidal cells with prominent round nuclei and reduced amount of cytoplasm, arranged in a ribbon-like structure and surrounded by moderate fibrotic stroma (a), with a positive immunohistochemical staining for Chromogranin A (b), CD 56 (c), Ep-4 (d), Cdx-2 (e) and Mib-1(f) pointed out by arrows. Scale bars 100 µm
Discussion
Historically, the nomenclature of “carcinoid” was describing the tumor entity of neuroendocrine cells with low malignancy in the gastrointestinal tract (GI) [7]. However the histopathogenesis of the primary testicular carcinoid remains under debate suggesting respective hypothesis: originating from the same precursor cell as the Leydig cells do or resulting from chromosomal irregularity [8, 9]. The diagnosis of primary testicular carcinoid is based on histopathology. The detailed histopathologic assessment is very important for the classification and the prognosis of the primary testicular carcinoid tumor [3]. Mitotic activity and vascular or tunica albuginea invasion were found not to increase the malignancy of the carcinoid tumors. However the occurrence of a low-degree of tumor differentiation, symptoms of a carcinoid syndrome as well as a tumor size correlate with increased metastatic potential [10, 11]. A precise detection of biomarkers assessed by immunohistochemistry (IHC) enables the subtyping and accurate classification of PTCT [12]. In general it is considered and it was described by Abbosh et al. that caudal type homeobox 2 (Cdx-2), a marker for neuroendocrine tumor cells originating from GI tract, is negative in PTCT [9, 13]. Lee et al. and Bing et al. described malignant germ cell tumors of the testes stained positive for Cdx-2 suggesting precaution in making a diagnosis in metastatic tumor with unknown origin and thereby considering an occult testicular malignancy rather than of GI origin [14, 15]. Albeit Atalay et al. demonstrated a strong significant Cdx-2 staining, as it is observed in tumor cells with GI origin, merely in testicular teratoma [16]. To the best of our knowledge, there is in the literature only one reported case of Cdx-2 positve PTCT [17]. In our case, the exceptionally rare Cdx-2 stain positivity was found as well, albeit no GI origin of carcinoid tumor cells was detected. This data suggests that the analytic specificity of Cdx-2 marker needs to be assessed critically and distinct in each case. The standard treatment of PTCT remains the radical inguinal orchiectomy [6]. The recurrence of PTCT may occur up to 17 years after the initial diagnosis and treatment requiring close clinical and imaging aftercare [18]. Since the data is based on single cases there is no consensus about general follow-up guidelines [6, 19]. In summary PTCT has a good prognosis with the 5-year overall survival rate of 78.7% and the 5-year specific survival rate of 84.3% and should be alternatively considered in Cdx-2 positive metastatic tumor of unknown origin [19].
Conclusion
Primary testicular carcinoid tumor with Cdx-2 positive stain outlines an exceptionally rare neoplastic entity. The standard treatment of PTCT remains the radical inguinal orchiectomy. PTCT have a good prognosis albeit some prognostic factors increase metastatic potential. The recurrence can appear almost 2 decades after initial diagnosis requiring close clinical and imaging aftercare.
Availability of data and materials
Not applicable.
Abbreviations
- CD56:
-
Cluster of differentiation 56
- Cdx-2:
-
Caudal type homeobox 2
- DOTA-TATE-PET/CT:
-
Tetraazacyclododecanetetraacetic acid–DPhe1-Tyr3-octreotate positron emission tomography/computed tomography
- Ep4:
-
Prostaglandin E receptor 4
- GI:
-
Gastrointestinal tract
- IHC:
-
Immunohistochemistry
- MIB-1:
-
Marker of proliferation Ki-67
- NET:
-
Neuroendocrine tumor
- PTCT:
-
Primary testicular carcinoid tumor
References
Yao JC, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J ClinOncol. 2008;26:3063–72.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97:934–59.
Wang WP, et al. Primary carcinoid tumors of the testis: a clinicopathologic study of 29 cases. Am J SurgPathol. 2010;34:519–24.
Kato N, et al. Primary carcinoid tumor of the testis: Immunohistochemical, ultrastructural and FISH analysis with review of the literature. PatholInt. 2003;53:680–5.
Berdjis CC, Mostofi FK. Carcinoid tumors of the testis. J Urol. 1977;118:777–82.
Stroosma OB, Delaere KP. Carcinoid tumours of the testis. BJU Int. 2008;101:1101–5.
D’Arrigo L, et al. Primary carcinoid tumour of the testis: a case-report. Arch ItalUrolAndrol. 2014;86:231–2.
Mai KT, Park PC, Yazdi HM, Carlier M. Leydig cell origin of testicular carcinoid tumour: immunohistochemical and electron microscopic evidence. Histopathology. 2006;49:548–9.
Abbosh PH, et al. Germ cell origin of testicular carcinoid tumors. Clin Cancer Res. 2008;14:1393–6.
Zavala-Pompa A, et al. Primary carcinoid tumor of testis: immunohistochemical, ultrastructural, and DNA flow cytometric study of three cases with a review of the literature. Cancer. 1993;72:1726–32.
Penke M. Primary neuroendocrine tumor of the testis and osseous, cardiac, and lymph node metastases in a young patient. Case Rep Oncol. 2014;7:815–8.
Duan K, Mete O. Algorithmic approach to neuroendocrine tumors in targeted biopsies: practical applications of immunohistochemical markers. Cancer Cytopathol. 2016;124:871–84.
Lin F, Liu H. Immunohistochemistry in undifferentiated neoplasm/tumor of uncertain origin. Arch Pathol Lab Med. 2014;138:1583–610.
Lee MJ, Vogt AP, Hsiao W, Osunkoya AO. CDX-2 expression in malignant germ cell tumors of the testes, intratubular germ cell neoplasia, and normal seminiferous tubules. Tumour Biol. 2012;33:2185–8.
Bing Z, Pasha T, Tomaszewski JE, Zhang P. CDX2 expression in yolk sac component of testicular germ cell tumors. Int J SurgPathol. 2009;17:373–7.
Oz Atalay F, AytacVuruskan B, Vuruskan H. CDX2 immunostaining in primary and metastatic germ cell tumours of the testis. J Int Med Res. 2016;44:1323–30.
AbouZahr R, et al. Primary carcinoid tumor of the testis: a case report and review of the literature. Case Rep Urol. 2018;2018:3614387.
Hayashi T, et al. Primary carcinoid of the testis associated with carcinoid syndrome. Int J Urol. 2001;8:522–4.
Amine MM, et al. Neuroendocrine testicular tumors: a systematic review and meta-analysis. CurrUrol. 2017;10:15–25.
Acknowledgements
We are grateful to the patient for his contribution.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
E.W. and C.F.W. were involved in patient’s medical care. A.F performed and analyzed pathological studies. E.W. and C.F.W. gathered detailed clinical information and analyzed data. E.W. and C.F.W. wrote the paper. E.W. and C.F.W. Conceived of and directed the project. The manuscript was critically reviewed by all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics Committee approval was not required for individual anonymized data.
Consent for publication
The written informed consent was obtained from the patient for publication of anonymized data and accompanying images. A copy of the written consent was uploaded and is available for review by the Editor.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Widmeier, E., Füllgraf, H. & Waller, C.F. Complete remission of Cdx-2 positive primary testicular carcinoid tumor: 10-years follow-up and literature review. BMC Urol 20, 197 (2020). https://doi.org/10.1186/s12894-020-00768-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-020-00768-2