Abstract
Background
To preliminary investigate the effects of silodosin 8 mg once daily on obstruction urodynamic parameters and subjective symptoms in Caucasian patients with lower urinary tract symptoms suggestive of benign prostatic enlargement.
Methods
We performed a single-center, open-label, single-arm, post-marketing interventional clinical trial. Inclusion criteria were: Caucasian subjects aged ≥50 years waiting to undergo surgery for lower urinary tract symptoms suggestive of benign prostatic enlargement, international prostate symptom total score ≥ 13, international prostate symptom-quality of life score ≥ 3, prostate volume ≥ 30 ml, maximum urine flow rate ≤ 15 mL/s, bladder outlet obstruction index > 40. Eligible subjects received one capsule of silodosin 8 mg once daily for 8 weeks. Invasive urodynamic evaluations were performed at baseline and at 8-weeks follow-up. International prostate symptom questionnaire was administered at baseline, after 4-weeks and 8-weeks of treatment.
Results
Overall, 34 subjects were included. Mean bladder outlet obstruction index significantly decreased from 70.6 to 39.2 and bladder outlet obstruction index class improved in 16 patients (53.3%). Statistically significant improvements of mean total international prostate symptom score, mean storage sub-score, mean voiding sub-score and mean quality of life sub-score were evident after 4-weeks of treatment with further improvements after 8-weeks. At the end of the treatment, all patients declared that their condition improved enough to spare or delay surgery.
Conclusions
Silodosin 8 mg once daily significantly improves benign prostatic obstruction in Caucasian patients with lower urinary tract symptoms suggestive of benign prostatic enlargement waiting for surgery.
Trial registration
EudraCT n. 2015-002277-38 Date of registration: 15th December 2017.
Similar content being viewed by others
Background
Silodosin is a new, highly selective α1-blocker (AB) approved in Japan in 2006 and recently in more than 50 countries including United States and Europe for the treatment of Lower Urinary Tract Symptoms suggestive of Benign Prostatic Enlargement (LUTS/BPE) [1]. This agent has a very strong affinity for the AR, the predominant α1A Adrenergic Receptor (α1-AR) subtype expressed in human prostate where it mediates smooth muscle contraction and therefore functional obstruction of the lower urinary tract [2,3,4,5,6,7]. Phase III randomized controlled trials as well as post hoc analyses of these studies performed in Japan, US and Europe demonstrated that silodosin provides clinically relevant benefits in terms of storage and voiding LUTS as well as in terms of Quality of Life (QoL) as assessed by the International Prostate Symptom Score (IPSS) [8,9,10,11]. Benign Prostatic Obstruction (BPO) is considered a key pathophysiological link between Benign Prostatic Enlargement (BPE) and LUTS [12, 13]. Moreover, long lasting BPO may activate pathways leading to progressive remodeling of both lower and upper urinary tract with subsequent functional impairments [12]. Therefore, BPO relief represents a major goal of LUTS/BPE treatment. A diagnosis of BPO requires an invasive Pressure/Flow studies (PFS) that allows to calculate the Bladder Outlet Obstruction Index (BOOI) [12]. Clinical studies investigating invasive urodynamic measures of BPO in LUTS/BPE patients receiving silodosin demonstrated that this agent, as other ABs, significantly improves BOOI [11,12,13]. Based on indirect comparisons, the magnitude of BPO improvement with silodosin appears to be greater if compared to other ABs [12,13,14]. Until now, however, urodynamic data on silodosin in terms of BPO mainly derive from three major studies involving Japanese LUTS/BPH patients [15,16,17]. It is widely recognized that ethnic and even population differences exist in the pharmacokinetics and pharmacodynamics of drugs [18]. Moreover, in two of these studies, silodosin was administered at the dosage of 4 mg twice daily whereas the dose of silodosin recommended by both the Food and Drug Administration and EMA is 8 mg once a day [15, 17, 19]. We aimed to preliminary investigate the effects of silodosin 8 mg once daily in Caucasian patients with LUTS/BPE in terms of invasive BPO urodynamic parameters and subjective symptoms.
Methods
We performed a single-center, open-label, single-arm, post-marketing interventional clinical trial (EudraCT n. 2015-002277-38). The local ethics committee approved the study protocol. The study was carried out according to the Declaration of.
Helsinki. All patients enrolled complained with LUTS severe enough to require surgery and reported poor results with previous pharmacological treatments.
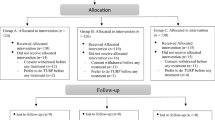
Study inclusion criteria were: Caucasian subjects aged ≥50 years waiting to undergo surgical intervention for LUTS/BPH, IPSS total score ≥ 13, IPSS-QoL score ≥ 3, prostate volume ≥ 30 ml, maximum urine flow rate (Qmax) ≤ 15 mL/s, BOOI > 40. Exclusion criteria were: pharmacological treatment for LUTS/BPH in the last 4 weeks or 6 months in case of previous assumption of 5alpha-reductase inhibitors, absolute indication for surgery therapy, hypersensitivity to the active substance or to any of the excipients, neurological causes of detrusor overactivity, active urinary tract infections, presence or history of bladder calculi, presence of prostate cancer, Post-Void Residual Volume (PVR) > 300 mL, clinically significant cardiovascular and cerebrovascular disease within 6 months prior to screening, renal or hepatic impairment, patients for whom cataract surgery was scheduled, history of orthostatic hypotension or syncope. After a washout period of 6 months, in patients taking 5-alpha reductase inhibitors, or of 4 weeks in patient taking any other drug or herbal remedy for LUTS/BPH, four visits were foreseen: at screening (Visit 1, week − 1), at baseline (Visit 2) and after 4 (Visit 3) and 8 (Visit 4) weeks of treatment. Screening procedures consisted of: medical history collection, check of prior and concomitant medications, symptom assessment by IPSS questionnaire, physical examination, measurement of vital signs (sitting blood pressure and heart rate), evaluation of prostate volume and PVR by suprapubic ultrasound, measurement of Qmax, 12-lead ECG, laboratory tests, including Prostate Specific Antigen value. Each patient signed an informed consent. Inclusion and exclusion criteria were preliminarily evaluated. At baseline, the following evaluations were performed: vital signs, urodynamic study. A final evaluation of inclusion and exclusion criteria was performed at this stage and patients with a BOOI< 40 were excluded. Eligible subjects received one capsule of silodosin 8 mg once daily for 8 weeks. They agreed not to use any other approved or experimental medication for LUTS/BPE or overactive bladder anytime during the study. At the end of the 4-weeks treatment period, patients underwent the following evaluations: IPSS questionnaire and patient-reported Treatment-Emergent Adverse Events (TEAEs) evaluated based on the terminology of the Medical Dictionary for Regulatory Activities. At the end of the 8-weeks treatment period, patients underwent the following evaluations: physical examination, IPSS questionnaire, vital signs, laboratory tests, PVR, urodynamic study. Moreover, TEAEs were evaluated again. All urodynamic studies were performed by the same operator based on standard International Continence Society (ICS) procedure [20]. A 6-F double lumen catheter was inserted transurethrally, and a balloon catheter was inserted from the anus to measure abdominal pressure. The test was done with the patient standing. Physiological saline solution was injected into the bladder at 50 ml per minute after evacuating the bladder. Intravesical pressure, abdominal pressure and detrusor pressure in the storage phase were simultaneously measured and recorded. Detrusor pressure was measured by electrically subtracting the abdominal pressure from the intravesical pressure. Detrusor Overactivity (DO) was defined as involuntary detrusor contractions during the filling phase which may be spontaneous or provoked. At maximum cystometric capacity the pressure/flow study was performed. The BOOI was defined as Detrusor Pressure at Qmax (PdetQmax) - 2Qmax [21]. According to BOOI value, subjects were classified as obstructed (BOOI > 40), equivocal (BOOI 20 − 40), or unobstructed (BOOI < 20) [21]. The primary objective of the study was to evaluate BOOI variations with respect to baseline. The followings were considered secondary outcomes: variations of other urodynamic parameters, improvement from baseline in obstruction class on the ICS BOOI nomogram, PVR variations, IPSS variations, percentage of subjects considering their condition improved enough to spare or delay the surgical intervention for LUTS/BPE, safety profile of the drug. Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as number and percentages. Changes from baseline for continuous data were compared using the paired Student’s T test. McNemar’s or Bowker’s Symmetry tests were used for shift tables assessment P values of less than 0.05 were regarded as statistically significant. Statistical analysis was performed using SAS software (SAS Institute Inc., Cary, N.C.).
Results
Overall, 34 subjects were screened. Of them, 4 were excluded after PFS indicated that they were unobstructed. Demographic and clinical characteristics of the 30 subjects enrolled into the study are summarized in Table 1.
All patients completed the study protocol and were available for follow-up evaluations. Table 2 and Fig. 1 summarizes the variations of main urodynamic parameters from baseline to the end of the study.
Mean BOOI significantly decreased from 70.6 to 39.2 and BOOI class improved in 16 patients (53.3%). Obstruction persisted in 14/30 subjects (46.7%). Statistically significant improvements were observed in terms of Detrusor opening pressure, PdetQmax, Maximum Detrusor Pressure (Pdetmax), Qmax, and Bladder Contractility Index. No statistically significant variations in terms of incidence of DO and amplitude of the largest DO contraction were observed. Total IPSS score, IPSS storage and voiding sub-scores as well as IPSS QoL sub-score improved in a statistically significant manner after 4-weeks of treatment and further improvements were evident after 8-weeks (Table 3).
Mean total IPSS score improved by 6.7 points and by 10.7 points after 4 and 8 weeks of treatment, respectively. Mean IPSS storage sub-score improved by 2.2 points and 4.0 points after 4 and 8 weeks of treatment, respectively. Mean IPSS voiding sub-score improved by 4.5 points and 6.7 points after 4 and 8 weeks of treatment, respectively. Mean IPSS QoL sub-score improved by 1.7 points and 3.0 points after 4 and 8 weeks of treatment, respectively. At the end of the treatment all patients answered “yes” to the question: “After the treatment with silodosin, is your condition improved enough to spare or, delay the surgical intervention for BPH/LUTS?”. In total, 11/30 patients (36.7%) experienced TEAEs. All TEAEs were drug related. The most frequently reported TEAE was retrograde ejaculation occurring in 8/30 patients (26.7%). Other TEAEs were asthenia (1/30, 3.3%), fatigue (1/30, 3.3%), and nasal congestion (1/30, 3.3%). There were no serious adverse events and all adverse evets were of mild intensity. There were no TEAEs leading to drug discontinuation. No clinical changes were found in terms of vital signs and laboratory parameters.
Discussion
ABs aim to inhibit the effect of endogenously released noradrenaline on smooth muscle cells in the prostate and thereby reduce prostate tone and BPO [21, 22]. To date, six ABs (terazosin, doxazosin, tamsulosin, naftopidil, alfuzosin, and silodosin) have been approved for the treatment of LUTS/BPE. Although all ABs improve BPO, the magnitude of improvement varies according to the type of AB and is greater after silodosin with values comparable to that obtained after transurethral microwave thermotherapy [12, 13]. To our knowledge, this is the first study investigating the urodynamic efficacy of silodosin 8 mg once a day in terms of BPO in Caucasian patients with LUTS/BPE waiting for surgery. We demonstrated that silodosin significantly improves BOOI in this selected subset of patients characterized by significant subjective and objective impairments. The magnitude of BOOI improvement (31.4 points) was both statistically and clinically significant and in line with published ranges for silodosin (21.2 - 37.6). To date, the rationale behind the urodynamic profile of silodosin is not completely understood. Based on published data, however, the existence of a positive relationship between α-1A/ α-1B receptor affinity ratio and BPO improvement has been hypothesized [12]. Moreover, the magnitude of BOOI improvement with ABs has been reported to increase also with the percentage of patients with obstruction at baseline [13]. Nevertheless, direct comparisons among ABs in terms of BPO improvement are lacking thus limiting the value of current evidences. We found that obstruction class improved in 53.3% of patients. This finding is in line with published data. In the study by Yamanishi et al., the obstruction grade was improved in 15 patients (56%) (obstructed to unobstructed in 5, obstructed to equivocal in 8, and equivocal to unobstructed in 2) and unchanged in 12 (44%) (obstructed to obstructed in 9, and equivocal to equivocal in 3) [16]. The BOOI value is obtained from Qmax and PdetQmax values. Results from the present study show statistically significant improvements of both PdetQmax and Qmax. However, although mean PdetQmax variation was clinically robust, mean Qmax improvement was clinically marginal (only 1.8 mL/s). This finding is coherent with published urodynamic data obtained in LUTS/BPE patients treated with ABs in general as well as in the subgroup of Japanese patients treated with silodosin at the dosages of both 4 mg twice daily and 8 mg once a day [13,14,15,16,17]. From a pathophysiological point of view, we can hypothesize that the reduction of detrusor pressure represents a priority with respect to urinary flow improvement and, when the relief of outflow resistances is small as after therapy with ABs, the lower urinary tract mainly adapts by reducing detrusor pressures thus potentially preserving the integrity of the bladder itself and of the upper urinary tract [12]. Therefore, in everyday clinical practice, Qmax improvement alone may underestimate the urodynamic benefits deriving from ABs therapy. Unlike some published data, our study did not demonstrate statistically significant variations of urodynamic parameters relative to DO [15,16,17]. However, the number of patients with DO at baseline in the present study was very low and further studies are needed to specifically address this issue.
In line with published data, we observed a statistically and clinically significant therapeutic effect, including improvements in both obstructive and irritative sub-scores, which was reflected by improvements in QoL. Interestingly, the magnitude of improvement we found in all these domains after 8 weeks of treatment was higher if compared to results from phase III clinical studies on silodosin as well as to results obtained in the urodynamic studies involving mainly obstructed patients after a 12 weeks treatment period [1, 15,16,17]. Matsukawa et al. reported mean improvements of total IPSS, voiding IPSS sub-score, storage IPSS sub-score and QoL sub-score of 6.2, 3.6, 2.6, and 1.6 points, respectively [17]. Yamanishi et al. reported mean improvement of total IPSS, voiding IPSS sub-score, storage IPSS sub-score and QoL sub-score were 7.9, 3.8, 2.0, and 1.1 points, respectively [16]. In the study by Chapple et al., mean improvement of total IPSS, voiding IPSS sub-score, storage IPSS sub-score and QoL sub-score were 7.0, 4.5, 2.5, and 1.1 points, respectively [10]. The rationale behind the differences observed between our results and published ones is unknown. Although we can hypothesize that baseline characteristics of subjects may have a role and that subjects with a moderate-to-high compromised baseline level, such that involved into the present study, may have a greater margin of improvement if compared to subjects that are less compromised at baseline, further studies are needed to confirm this hypothesis. At the end of the treatment, all patients declared that their condition had improved enough to spare or delay surgery. Results from the present study have relevant clinical implications. Indeed, therapy with ABs may represent an interesting “rescue treatment” option for patients with BPO waiting for surgical treatment.
Although a timely indication to surgery is crucial to prevent bladder decompensation leading to surgical failure, this treatment may postpone the need to perform a surgical treatment in patients showing an improvement of BPO and LUTS and/or an improvement of their QoL due to LUTS while waiting for surgery. Moreover, this treatment may cause a reduction in the waiting list for the other patients confirming the need to perform surgery. The urodynamic profile of silodosin characterized by the highest level of BOOI improvement with respect to other ABs, makes it a drug of greatest interest in this subset of patients. We confirmed the good safety profile of silodosin. In line with published data, retrograde ejaculation was the more frequently reported adverse event. However, none of subjects interrupted the treatment due to this event. We acknowledge potential limitations of the present study. First, it was a single arm, open-label study using neither a placebo nor a control group. Although a placebo-effect cannot be excluded in terms of changes of both subjective and urodynamic parameters, results from a previous meta-analysis suggested the absence of significant placebo effects on urodynamic parameters of BPO after therapy with ABs [13]. Moreover, our study sample voluntarily included patients with urodynamic proven BPO thus making questionable the generalizability of our results to subjects that in the everyday clinical practice do not routinely undergo invasive urodynamic investigations. However, the combination of the clinical criteria we adopted in the pre-screening procedure (age ≥ 50 years, IPSS total score ≥ 13, prostate volume of ≥ 30 ml, Qmax ≤ 15 mL/s) represented a good proxy of BPO as it allowed us to identify a population of subjects with a high prevalence of urodynamic proven BPO (88.2%, n = 30/34). Therefore, in every day clinical practice, findings from the present study can be generalizable to subjects with the aforementioned clinical features even in the absence of urodynamic confirmation of BPO. Overall, results from the present study should be considered as preliminary and confirmatory randomized placebo controlled trials with adequate follow-up are needed. In conclusions, silodosin 8 mg once daily provides statistically and clinically significant improvement of BPO and symptoms in LUTS/BPE Caucasian men with confirmed BPO waiting for surgery.
Conclusions
In conclusions, based on these preliminary data, silodosin 8 mg once daily significantly improves BPO in Caucasian patients with LUTS/BPE waiting for surgery.
Abbreviations
- AB:
-
Alpha Blocker
- AR:
-
Adrenergic Receptor
- BOOI:
-
Bladder Outlet Obstruction Index
- BPE:
-
Benign Prostatic Enlargement
- BPO:
-
Benign Prostatic Obstruction
- DO:
-
Detrusor Overactivity
- ICS:
-
International Continence Society
- IPSS:
-
International Prostate Symptom Score
- LUTS:
-
Lower Urinary Tract Symptoms
- PdetQmax :
-
Detrusor Pressure at Qmax
- PFS:
-
Pressure/Flow studies
- PVR:
-
Post-Void Residual Volume
- Qmax :
-
Maximum Urine Flow Rate
- QoL:
-
Quality of Life
- SD:
-
Standard Deviation
- TEAEs:
-
Treatment-Emergent Adverse Events
References
Osman NI, Chapple CR, Cruz F, Desgrandchamps F, Llorente C, Montorsi F. Silodosin: a new subtype selective alpha-1 antagonist for the treatment of lower urinary tract symptoms in patients with benign prostatic hyperplasia. Expert Opin Pharmacother. 2012 Oct;13(14):2085–96.
Lepor H, Shapiro E. Characterization of alpha1 adrenergic receptors in human benign prostatic hyperplasia. J Urol. 1984;132(6):1226–9.
Lepor H, Tang R, Meretyk S, Shapiro E. Alpha 1 adrenoceptor subtypes in the human prostate. J Urol. 1993;149(3):640–2.
Kobayashi S, Tang R, Shapiro E, Lepor H. Characterization and localization of prostatic alpha 1 adrenoceptors using radioligand receptor binding on slide-mounted tissue section. J Urol. 1993;150(6):2002–6.
Walden PD, Gerardi C, Lepor H. Localization and expression of the alpha1A-1, alpha1B and alpha1D-adrenoceptors in hyperplastic and non-hyperplastic human prostate. J Urol. 1999;161(2):635–40.
Forray C, Bard JA, Wetzel JM, et al. The alpha 1-adrenergic receptor that mediates smooth muscle contraction in human prostate has the pharmacological properties of the cloned human alpha 1c subtype. Mol Pharmacol. 1994;45(4):703–8.
Imperatore V, Fusco F, Creta M, et al. Medical expulsive therapy for distal ureteric stones: tamsulosin versus silodosin. Arch Ital Urol Androl. 2014 Jun 30;86(2):103–7.
Kawabe K, Yoshida M, Homma Y, Silodosin Clinical Study Group. Silodosin, a new alpha1A-adrenoceptor-selective antagonist for treating benign prostatic hyperplasia: results of a phase III randomized, placebo-controlled, double-blind study in Japanese men. BJU Int. 2006 Nov;98(5):1019–24.
Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G. Silodosin in the treatment of the signs and symptoms of benign prostatic hyperplasia: a 9-month, open-label extension study. Urology. 2009 Dec;74(6):1318–22.
Chapple CR, Montorsi F, Tammela TL, et al. Silodosin therapy for lower urinary tract symptoms in men with suspected benign prostatic hyperplasia: results of an international, randomized, double-blind, placebo- and active-controlled clinical trial performed in Europe. Eur Urol. 2011 Mar;59(3):342–52.
Osman NI, Chapple CR, Tammela TL, Eisenhardt A, Oelke M. Open-label, 9-month extension study investigating the uro-selective alpha-blocker silodosin in men with LUTS associated with BPH. World J Urol. 2015 May;33(5):697–706.
Fusco F, Creta M, Imperatore V, et al. Benign prostatic obstruction relief in patients with lower urinary tract symptoms suggestive of benign prostatic enlargement undergoing endoscopic surgical procedures or therapy with alpha-blockers: a review of urodynamic studies. Adv Ther. 2017 Apr;34(4):773–83.
Fusco F, Palmieri A, Ficarra V, et al. α1-blockers improve benign prostatic obstruction in men with lower urinary tract symptoms: a systematic review and meta-analysis of urodynamic studies. Eur Urol. 2016 Jun;69(6):1091–101.
Creta M, Bottone F, Sannino S, et al. Effects of alpha1-blockers on urodynamic parameters of bladder outlet obstruction in patients with lower urinary tract symptoms suggestive of benign prostatic enlargement: a review. Minerva Urol Nefrol. 2016;68(2):209–21.
Matsukawa Y, Gotoh M, Komatsu T, Funahashi Y, Sassa N, Hattori R. Efficacy of silodosin for relieving benign prostatic obstruction: prospective pressure flow study. J Urol. 2009;182:2831–5.
Yamanishi T, Mizuno T, Tatsumiya K, Watanabe M, Kamai T, Yoshida K. Urodynamic effects of silodosin, a new alpha 1A-adrenoceptor selective antagonist, for the treatment of benign prostatic hyperplasia. Neurourol Urodyn. 2010;29:558–62.
Matsukawa Y, Takai S, Funahashi Y, Kato M, Yamamoto T, Gotoh M. Long-term efficacy of a combination therapy with an anticholinergic agent and an α1-blocker for patients with benign prostatic enlargement complaining both voiding and overactive bladder symptoms: a randomized, prospective, comparative trial using a urodynamic study. Neurourol Urodyn. 2017 Mar;36(3):748–54.
Kurose K, Sugiyama E, Saito Y. Population differences in major functional polymorphisms of pharmacokinetics/pharmacodynamics-related genes in Eastern Asians and Europeans: implications in the clinical trials for novel drug development. Drug Metab Pharmacokinet. 2012;27(1):9–54. Epub 2011 Nov 29.
Rossi M, Roumeguère T. Silodosin in the treatment of benign prostatic hyperplasia. Drug Des Devel Ther. 2010 Oct 27;4:291–7.
Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the Standardisation Subcommittee of the International Continence Society. Urology. 2003;61:37.
Nitti VW. Pressure flow urodynamic studies: the gold standard for diagnosing bladder outlet obstruction. Rev Urol. 2005;7(Suppl 6):S14–21.
Gratzke C, Bachmann A, Descazeaud A, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015;67:1099–109.
Acknowledgements
We have no acknowledgements for this study.
Funding
This work was supported by Recordati S.p.A. Recordati contributed in the study design definition and was involved in the collection and analysis of the data.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Conception and design: FF, MC and VM; enrollment of patients and acquisition of data: FF, NL, FP and MF; drafting of the manuscript: FF and MC; statistical analysis: FF, FP; analysis and interpretation of data: MC, MF, NL; supervision: NL, VM. We confirm that all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of the University of Naples Federico II (Institutional review board approval No.143/15). All patients gave their written informed consent to participate in the study.
Consent for publication
Informed consent was obtained from the patients for publication of this study.
Competing interests
Ferdinando Fusco, Massimiliano Creta and Vincenzo Mirone have been consultants for Recordati S.p.A.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fusco, F., Creta, M., Longo, N. et al. Silodosin 8 mg improves benign prostatic obstruction in Caucasian patients with lower urinary tract symptoms suggestive of benign prostatic enlargement: results from an explorative clinical study. BMC Urol 18, 12 (2018). https://doi.org/10.1186/s12894-018-0326-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-018-0326-7