Abstract
Background
Multi-step testing might enhance performance of the prostate cancer diagnostic pipeline. Using PSA >1 ng/ml for first-line risk stratification and the Stockholm 3 Model (S3M) blood-test >10% risk of Gleason Score > 7 prostate cancer to inform biopsy decisions has been suggested. We aimed to determine the effects of changing the PSA cutoff to perform reflex testing with S3M and the subsequent S3M cutoff to recommend prostate biopsy while maintaining the sensitivity to detect Gleason Score ≥ 7 prostate cancer.
Methods
We used data from the prospective, population-based, paired, diagnostic Stockholm 3 (STHLM3) study with participants invited by date of birth from the Swedish Population Register during 2012–2014. All participants underwent testing with PSA and S3M (a combination of plasma protein biomarkers [PSA, free PSA, intact PSA, hK2, MSMB, MIC1], genetic polymorphisms, and clinical variables [age, family, history, previous prostate biopsy, prostate exam]). Of 47,688 men in the STHLM3 main study, we used data from 3133 men with S3M >10% and prostate biopsy data. Logistic regression models were used to calculate prostate cancer detection rates and proportion saved biopsies.
Results
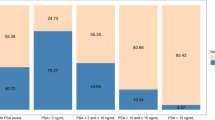
44.2%, 62.5% and 67.9% of the participants had PSA <1, <1.5 and <1.7 ng/ml, respectively. Increasing the PSA cut-off for additional work-up from 1 ng/ml to 1.5 ng/ml would thus save 18.3% of the performed tests, 4.9% of the biopsies and 1.3% (10/765) of Gleason Grade ≥ 7 cancers would be un-detected. By lowering the S3M cutoff to recommend biopsy, sensitivity to high-grade prostate cancer can be restored, to the cost of increasing the number of performed biopsies modestly.
Conclusion
The sensitivity to detect prostate cancer can be maintained when using different PSA cutoffs to perform additional testing. Biomarker cut-offs have implications on number of tests and prostate biopsies performed. A PSA cutoff of 1.5 ng/ml to perform additional testing such as the S3M test might be considered.
Trial registration
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Recently, Crawford and colleagues proposed an approach of using PSA 1.5 ng/ml as first-line testing before using biomarker-based tests to inform prostate biopsy decisions [1]. Such a multi-step work-up is an attractive approach for improving prostate cancer diagnostics. Men with PSA below the population median carries a low risk to develop metastatic or lethal disease also during long follow-up [2]. Since testing with PSA has high availability and low cost, base-line PSA testing is a attractive for efficient first-line risk stratification [2].
For second-line testing, the S3M (Stockholm3 Model) blood-test has been developed, including data on proteins, a genetic score and clinical information (age, digital rectal examination, prostate volume, and previous biopsy) [3]. Compared with both organized PSA-screening and current prostate cancer testing (without organized screening but with high rates of PSA testing), the STHLM3 studies have shown that use of the S3M test may decrease both the number of prostate biopsies and over-diagnosis, while maintaining sensitivity to high-grade disease [3, 4]. This was done using PSA >1 ng/ml as cutoff for performing the S3M blood-test and a risk of high-grade disease exceeding that of PSA = 3 ng/ml to indicate recommendation for prostate biopsies.
With the approach suggested by Crawford et al. [1], two thirds of men would be identified as having a very low risk of developing high-grade disease. Compared with a lower PSA cutoff, using 1.5 ng/ml would decrease the number of performed biomarker tests. However, while performing the biomarker test for fewer men, it would also yield a smaller pool of men in which to identify prostate cancer cases, potentially affecting overall sensitivity.
It is unknown how changing the PSA cut-off for performing a reflex test affects the overall diagnostic sensitivity, the number of performed biopsies, and number of performed biomarker tests. We therefore illustrate such effects for the first-line test PSA and the second-line biomarker test S3M.
Methods
STHLM3 (ISRCTN84445406) is a prospective and population-based prostate cancer diagnostic study conducted 2012–2014 including men between 50 and 69 years of age [3]. The S3M test is a blood test based on a model including a combination of plasma protein biomarkers (PSA, free PSA, intact PSA, hK2, MSMB, MIC1), genetic polymorphisms (232 SNPs), and clinical variables (age, family, history, previous prostate biopsy, prostate exam). The test gives a prediction on the individual risk of finding Gleason Score ≥ 7 on prostate biopsies, where ≥10% risk was considered increased risk in the main study. The 10% risk cutoff was choosen because it represent equal sensitivity to detect Gleason Score ≥ 7 cancer as PSA = 3 ng/ml, used in major screening studies [5]. The exact cut-off used can be chosen to fit different individuals and healthcare systems [6]. As for September 2017, the S3M test is clinically availiable for analysis at Karolinska University Laboratory, Stockholm, Sweden.
Of 47,688 participants in the STHLM3 study, 26,458 men had a PSA ≥ 1 ng/ml and underwent further testing with S3M. By design, a prostate biopsy was recommended to men with ≥10% risk of high-grade prostate cancer as predicted by PSA (≥3 ng/ml) or the S3M test. Gleason Score ≥ 7 (ISUP ≥2) defined high-grade cancer. 65.0% of participants with high risk followed the recommendation to undergo prostate biopsy during the main study period. For this analysis we included 3133 men in the STHLM3 validation cohort with biopsy data and an S3M test ≥10%.
We calculated detection rates and proportion saved biopsies when S3M was used as a reflex test after a range of a priori choosen PSA cutoff levels, keeping overall sensitivity fixed at the same level as PSA ≥ 3 (or, equivalently, S3M ≥ 10% as a reflex test in men with PSA ≥ 1). Data on men with less than 10% risk of Gleason Score ≥ 7 prostate cancer was thus incomplete. To calculate results for this group of men, we imputed case status of each non-biopsied man using Bernoulli experiments with the risk prediction from the S3M as parameter [7].
Results
44.2%, 62.5% and 67.9% of the participants in the population-based STHLM3 study had PSA <1, <1.5 and <1.7 ng/ml, respectively. Solely increasing the cut-off for additional work-up from 1 ng/ml to 1.5 ng/ml would thus save 18.3% of the performed tests, 4.8% of the biopsies and only 1.3% (10/765) of Gleason Grade ≥ 7 cancers would be un-detected (Table 1). Participant characteristics in men with PSA ≥ 3 or S3M ≥ 10% risk of Gleason Score ≥ 7 cancer and thus undergoing a prostate biopsy are described in Table 2.
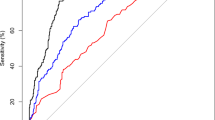
To infer the mortality benefit of early detection of prostate cancer reported in ERSPC, the sensitivity to detect high-grade disease needs to be at least as high as when performing systematic prostate biopsies with a PSA cut-off of 3 ng/ml, being the threshold primarily used for biopsy in ERSPC [5]. To adjust for the slightly decreased cancer detection when increasing the first-line PSA threshold from 1 to 1.5 ng/ml, the S3M cutoff to recommend biopsy can be tuned, as previously illustrated [7]. Figure 1 illustrates how the PSA cutoff to perform the S3M test and the S3M cutoff to recommend biopsy are inter-related to maintain sensitivity to high-grade disease. For example, the total number of biopsies would increase slightly by 4% if increasing the cutoff for performing the S3M test from PSA 1.0 ng/ml to 1.5 ng/ml while maintaining sensitivity to high-grade prostate cancer (Fig. 1). A small number of Glason Score ≥ 4 + 3 were detected in low PSA ranges (Table 1). If choosing PSA 2 ng/ml for threshold to perform S3 M testing, only 1.0% (3/197) of Gleason Score ≥ 4 + 3 cancers would be undetected, but missing also 3.8% (18/472) of Gleason Score 3 + 4 cancers. Availiable number of higher-grade cases were to small in low PSA ranges for additional analyses such as in Fig. 1 on this endpoint.
The minimum PSA used to perform the S3 M test by the minimum risk of high-grade prostate cancer as predicted by the S3 M test used to recommend prostate biopsy in order to maintain relative sensitivity compared to when using PSA = 3 ng/ml. Shaded area indicates 95% confidence interval. Data from 3133 men in the STHLM3 study with a S3 M test >10% and a subsequent prostate biopsy
Discussion
With a possibly increasing complexity of the diagnostic chain including a multi-step approach with PSA, additional biomarker-based algorithms, and imaging before deciding to recommend further work-up, several cut-offs need to be adjusted to optimize performance. Here, we illustrate the effects of simultaneously tuning both the PSA cut-off for performing the reflex test S3M and the S3M cutoff for recommending a prostate biopsy. Using this approach, the sensitivity to detect high-grade disease can be maintained, while the number of prostate biopsies is slightly affected.
From a health-economical point of view, it is efficient to maximize the use of cheap tools such as PSA early in the diagnostic chain, with the more expensive and specialized tests used downstream. Further, as many men with low risk of high-grade disease as possible should be identified early in the process, without being subjected to additional tests or extended workup. Thus, it is interesting both from the perspective of an individual and from the healthcare system to explore how an increased cut-off to perform e.g. the S3M test might be done without compromising the overall diagnostic performance.
This analysis was based on prospective, population-based data from the STHLM3 study. It illustrates the relationship between two sequential diagnostic tests when maintaining sensitivity to detect high-grade disease. The detection rates in low PSA intervals are well comparable with previously presented data [8] and the internal validity of these data is high. While extrapolation outside the STHLM3 context is hard, corresponding analyses regarding other suggested reflex tests are warranted. Limitations of this work include lack of external validation, lack of true disease prevalence while men with <10% risk of Gleason Score ≥ 7 cancer as predicted by both PSA and S3M did not undergo prostate biopsy, and lack of long-term follow-up.
Conclusion
We conclude that the sensitivity to detect prostate cancer can be maintained while avoiding a substantial proportion of reflex tests and biopsies by carefully choosing the PSA cutoff to perform additional testing. For instance, a PSA cutoff of 1.5 ng/ml to perform additional biomarker tests such as the S3 M test might be considered.
Abbreviations
- 5-ARI:
-
5-alfa reductase inhibithor
- ERSPC:
-
European Randomized Study of Screening for Prostate Cancer
- PSA:
-
prostate-specific antigen
- S3 M:
-
stockholm3 model
- STHLM3:
-
Stockholm3 study
References
Crawford ED, Rosenberg MT, Partin AW, Cooperberg MR, Maccini M, Loeb S, et al. An approach using PSA levels of 1.5 ng/mL as the cutoff for prostate cancer screening in primary care. Urology. 2016;96:116–20.
Vickers AJ, Cronin AM, Bjork T, Manjer J, Nilsson PM, Dahlin A, et al. Prostate specific antigen concentration at age 60 and death or metastasis from prostate cancer: case-control study. BMJ. 2010 ed. 2010;341:c4521.
Grönberg H, Adolfsson J, Aly M, Nordström T, Wiklund P, Brandberg Y, et al. Prostate cancer screening in men aged 50-69 years (STHLM3): a prospective population-based diagnostic study. Lancet Oncol. 2015;16:1667–76.
Eklund M, Nordström T, Aly M, Adolfsson J, Wiklund P, Brandberg Y, et al. The Stockholm-3 (STHLM3) Model can Improve Prostate Cancer Diagnostics in Men Aged 50–69 yr Compared with Current Prostate Cancer Testing. European Urology Focus [Internet]. 2016. Available from: http://www.eu-focus.europeanurology.com/article/S2405-4569(16)30156-0/fulltext.
Schröder FH, Hugosson J, Roobol MJ, Tammela TLJ, Zappa M, Nelen V, et al. Screening and prostate cancer mortality: results of the European randomised study of screening for prostate cancer (ERSPC) at 13 years of follow-up. Lancet. 2014;384:2027–35.
Nordström T, Grönberg H, Adolfsson J, Aly M, Eklund M. Balancing Overdiagnosis and early detection of prostate cancer using the Stockholm-3 model. European Urology Focus. 2016;
Nordström T, Grönberg H, Adolfsson J, Aly M, Eklund M. Balancing Overdiagnosis and Early Detection of Prostate Cancer using the Stockholm-3 Model. Catto J, editor. European Urology Focus. 2016.
Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level. N. Engl. J. Med. 2004 ed. 2004;350:2239–46.
Acknowledgements
We thank all study participants, the STHLM3 core management group, STHLM3 outpatient urologists, KI Biobank, Karolinska University Hospital Laboratory, Unilabs AB Stockholm, and Histocenter Gothenburg for dedicated work with all aspects of the STHLM3 study.
Availability of data and materials
The datasets analysed during the current study might be available from the corresponding author on request.
Funding
The main funder of the STHLM3 study is the Stockholm County Council (Stockholms Läns Landsting) who is the main healthcare provider in Stockholm. Martin Eklund is supported by the Swedish Research Council for Health, Working Life and Welfare, the Swedish Research Council, and the Swedish Cancer Society. The funding sources had no role in the study design; the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
HG is principal investigator for the STHLM3 study. TN, HG and ME designed the study. TN and ME performed statistical analyses and drafted the manuscript. TN, HG, JA and ME interpreted study results and finalized the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The STHLM3 study was approved by the Stockholm County regional ethics committee, number 2012/572:31/1.
Consent for publication
Not applicable.
Competing interests
TN and JA declare nor conflict of interest. HG has five prostate cancer diagnostic-related patents pending, has patent applications licensed to Thermo-Fisher Scientific, and might receive royalties from sales related to these patents. ME is named on four of these five patent applications. Karolinska Institutet collaborates with Thermo-Fisher Scientific in developing the technology for STHLM3.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nordström, T., Adolfsson, J., Grönberg, H. et al. Effects of increasing the PSA cutoff to perform additional biomarker tests before prostate biopsy. BMC Urol 17, 92 (2017). https://doi.org/10.1186/s12894-017-0281-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-017-0281-8