Abstract
Background
Postoperative delirium (POD) is a common complication after major surgery and can cause a variety of adverse effects. However, no large-scale national database was used to assess the occurrence and factors associated with postoperative delirium (POD) following hepatic resection.
Methods
Patients who underwent hepatic resection from 2015 to 2019 were screened using the International Classification of Diseases (ICD) 10th edition clinical modification code from the National Inpatient Sample (NIS) Database. Peri-operative factors associated with delirium were screened and underwent statistical analysis to identify independent predictors for delirium following hepatic resection.
Results
A total of 80,070 patients underwent hepatic resection over a five-year period from 2015 to 2019. The overall occurrence of POD after hepatic resection was 1.46% (1039 cases), with a slight upward trend every year. The incidence of elective admission was 6.66% lower (88.60% vs. 81.94%) than that of patients without POD after hepatic resection and 2.34% (45.53% vs. 43.19%) higher than that of patients without POD in teaching hospitals (P < 0.001). In addition, POD patients were 6 years older (67 vs. 61 years) and comprised 9.27% (56.69% vs. 47.42%) more male patients (P < 0.001) compared to the unaffected population. In addition, the occurrence of POD was associated with longer hospitalization duration (13 vs. 5 days; P < 0.001), higher total cost ($1,481,89 vs. $683,90; P < 0.001), and higher in-hospital mortality (12.61% vs. 4.11%; P < 0.001). Multivariate logistic regression identified hepatic resection-independent risk factors for POD, including non-elective hospital admission, teaching hospital, older age, male sex, depression, fluid and electrolyte disorders, coagulopathy, other neurological disorders, psychoses, and weight loss. In addition, the POD after hepatic resection has been associated with sepsis, dementia, urinary retention, gastrointestinal complications, acute renal failure, pneumonia, continuous invasive mechanical ventilation, blood transfusion, respiratory failure, and wound dehiscence / non-healing.
Conclusion
Although the occurrence of POD after hepatic resection is relatively low, it is beneficial to investigate factors predisposing to POD to allow optimal care management and improve the outcomes of this patient population.
Similar content being viewed by others
Background
Most people with liver cancer have liver dysfunction caused by other liver diseases, alcoholism, or hepatitis virus infections [1]. In the United States, hepatic resection is increasingly used for resection of biliary tract malignancies, primary liver cancer, and metastases [2]. Major hepatic resection is an extremely risky procedure, especially in cases with poor liver condition, with complications occurring after surgery in 41-50% of patients [3,4,5]. It is now understood that there is a high risk of postoperative delirium (POD) after hepatic resection [6].
POD is a multifactorial and heterogeneous syndrome defined as an acute alteration of consciousness associated with an underlying physiological disorder [7, 8]. POD is common postoperatively, with the incidence of POD varying between 4% and 61%, depending on the type of surgery [9,10,11]. The occurrence of POD leads to higher complication rates, longer recovery times, additional care, prolonged intensive care unit (ICU) stays, and greater costs [12, 13]. Although the pathophysiology of POD is unknown, risk factors for POD include the patient’s age, drug-related factors, medical condition, postoperative analgesic regimen, and surgical factors [14,15,16].
Recently, it has been reported that POD after hepatic resection in the elderly is associated with serum albumin concentration and age [6, 17, 18]. However, to date, few studies have elucidated POD in patients undergoing hepatic resection. Therefore, it is important to investigate the factors that contribute to POD in hepatic resection cases and identify factors that increase the risk of developing POD. This will provide a theoretical basis for the prevention of POD. Herein, the clinical data of hepatic resection inpatients were retrospectively analyzed with the aim of providing an overview of the frequency of occurrence of POD events in this patient cohort and an in-depth study of potential risk factors associated with POD.
Methods
Data source
The National Inpatient Sample (NIS) database, conducted by the Healthcare Cost and Utilization Project and sponsored by the Agency for Healthcare Research and Quality, provided data for your research. In the United States, NIS is the largest database of all payers for hospitalization admissions. NIS collects stratified samples from more than 1,000 hospitals, accounting for about 20% of annual hospitalizations in the U.S [19]. Data collected from the NIS database, including hospital characteristics, type of insurance, patient demographics, length of stay (LOS), in-hospital mortality, total cost, and diagnostic and procedure codes for the International Classification of Diseases (10th Revision) Clinical Revision (ICD-10-CM). This study utilized anonymized data from public sources and is thus classified as exempt from requiring ethical approval according to established research guidelines.
Data collection
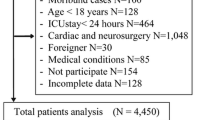
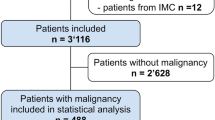
The cohort under investigation comprised individuals for whom hospitalization information was accessible in the National Inpatient Sample database spanning the years 2015 to 2019. The focus was on patients undergoing hepatic resection, identified through specific ICD-10-CM procedural codes: 0FB00ZZ, 0FB03ZX, 0FB03ZZ, 0FB04ZX, 0FB04ZZ, 0FB10ZX, 0FB13ZX, 0FB13ZZ, 0FB14ZX, 0FB14ZZ, 0FB20ZX, 0FB23ZX, 0FB23ZZ, 0FB24Z, 0FB24ZZ, 0FC00ZZ, 0FC03ZZ, 0FC04ZZ, 0FC10ZZ, 0FC13ZZ, 0FC14ZZ, 0FC20ZZ, 0FC23ZZ, 0FC24ZZ, 0FP000Z, 0FP002Z, 0FP003Z, 0FT00ZZ, 0FT04ZZ, 0FT10ZZ, 0FT14ZZ, 0FT20ZZ, and 0FT24ZZ (n = 80,070). The exclusion criteria were as follows: (1) patients with missing data; (2) less than 18 years of age (Fig. 1). Ultimately, a total of 71,348 patients meeting the specified criteria and possessing comprehensive data were identified through the screening process.
Depending on the occurrence of POD, selected cases were divided into two groups. POD is defined by ICD-10-CM diagnostic code 4181, R4182, R4183, 4184, R41841, R41842, R41843, 41,844, R4189, F060, F062, F10121, F11921, F13921, F05, F11121.
The primary outcome of the study was POD. Surgery-related complications during hospitalization were collected from the National Inpatient Sample database by ICD-10-CM diagnostic code. Complications included sepsis, dementia, urinary retention, gastrointestinal complications, cardiac arrest, acute renal failure, pneumonia, continuous invasive mechanical ventilation, blood transfusion, respiratory failure, and acute myocardial infarction. Surgical complications included bile leakage, Intra-abdominal abscess, liver ascites, wound infection, and wound dehiscence / non-healing. If other comorbidities were identified in previous studies as important risk factors for any kind of POD, these comorbidities may be analyzed at the discretion of the authors.
Data analysis
We began by examining the data distribution and calculating the basic descriptive statistics for all the variables included in the analysis. Afterwards, the continuous variable data were compared using a T-test, while the categorical data were compared using either χ2 test or Fisher exact test. To identify the factors that independently predict POD following hepatic resection, we conducted univariate and multivariate regression analyses. In order to evaluate the impact of various pre-surgery factors on the requirement for POD, we computed the adjusted odds ratio. These factors included patient characteristics like age, race, and teaching status of hospitals, as well as patient comorbidities and concurrent operations such as wound infection, hemorrhage, and pulmonary embolism. We used the R software (v3.5.3) to carry out all statistical analyses on the NIS database. Due to the large sample size, a P-value ≤ 0.001 was statistically significant.
Results
Occurrence of POD in hepatic resection cases
Patient demographics, hospital characteristics, and comorbidities are among the categories of variables outlined in Table 1. 71,348 hepatic resections were screened from the National Inpatient Sample database from 2015 to 2019. The incidence of POD was 1.46% (n = 1,039/71,348) (Table 2) and exhibited a growing trend from 2015 to 2019 (from 1.04 to 1.53%) (Fig. 2).
Patient demographics
POD cases tended to be 6 years older (67 years vs. 61 years) and comprised 13.38% (56.69% vs. 43.31%) more males than unaffected populations (P < 0.001) (Table 2; Figs. 3C, D and 4C, D). Besides, the two groups exhibited comparable age distributions, and a lower occurrence of POD was observed among patients younger than 65 years (P < 0.001) (Table 2). Whites constituted the predominant race (nearly 66.59%) of the study population. However, the two groups were comparable in terms of race (P = 0.007) (Table 2).
Patient demographics and hospital characteristics between the two surgical groups. A Type of insurance analysis of postoperative delirium patients. B Type of insurance analysis of patients without postoperative delirium. C Age distribution analysis of postoperative delirium patients. D Analysis of age distribution of patients without postoperative delirium
Hospital characteristics
Individuals who experienced POD following hepatic resection were 14.23% less likely to undergo elective admission compared to those who did not encounter such complications (35.60% vs. 21.37%, P < 0.001) (Table 2). Additionally, in-hospital POD was predominantly observed in teaching hospitals (88.61% vs. 88.91%, P < 0.001) (Table 2). Regarding hospital bed capacity, the occurrence of in-hospital POD was 3.18% higher in facilities categorized as Medium or large (24.30% vs. 27.48%, 67.28% vs. 59.67%, P < 0.001) (Table 2; Fig. 4A & B). In addition, the incidence of in-hospital POD was 78.35% higher with open hepatectomy (10.68% vs. 89.03%, P < 0.001) (Table 2). Besides, there was no significant difference in the hospital region between the two groups (P = 0.004) (Table 2).
Patient demographics and hospital characteristics between the two surgical groups. A Racial distribution analysis of postoperative delirium patients. B Racial distribution analysis of patients without postoperative delirium. C Gender distribution analysis of postoperative delirium patients. D Gender distribution of patients without postoperative delirium
Adverse outcomes of POD after hepatic resection
Unsurprisingly, patients with POD had significantly three times higher in-hospital mortality compared with those with undiagnosed POD (12.61% vs. 4.11%; P < 0.001) (Table 2). POD cases had an 8-day longer hospitalization (13 vs. 5 days; P < 0.001) (Table 2). As a result, POD increases medical spending. The study found that the total hospitalization expenses were raised significantly by $79,799 after POD ($148,189 vs. $68,390, P < 0.001) (Table 2). In terms of the type of insurance, the proportion of individuals with private insurance in the POD group was lower by 14.48% (21.31% vs. 35.79%, P < 0.001) (Table 2; Fig. 3A & B). The number of comorbidities was significantly higher in patients with POD (95.67% vs. 75.35%, P < 0.001), which represented more comorbidities (Table 2).
Risk factors of POD following hepatic resection
Logistic regression analysis was used to determine factors predisposing to POD (Tables 3 and 4), which included patients older than 65 years (OR = 1.30; CI = 1.22–1.39), teaching hospital (odds ratio [OR] = 1.85; CI = 1.52–2.25), Medium hospital bed size capacity (OR = 1.54; CI = 0.91–1.45), large hospital bed size capacity (OR = 1.64; CI = 1.34–2.02), depression (OR = 1.45; CI = 1.21–1.74), fluid and electrolyte disorders (OR = 1.27; CI = 1.11–1.47), coagulopathy (OR = 1.36; CI = 1.17–1.59), other neurological disorders (OR = 36.58; CI = 31.46–42.53), psychoses(OR = 1.77; CI = 1.34–2.34), weight loss(OR = 1.59; CI = 1.38–1.83).
Additional comorbidities and complications associated with POD following hepatic resection
Univariate analysis showed that POD cases experienced more perioperative complications during hospital stay, encompassing sepsis, dementia, acute myocardial infarction, urinary retention, gastrointestinal complication, cardiac arrest, acute renal failure, pneumonia, continuous invasive mechanical ventilation, blood transfusion, respiratory failure, intra-abdominal abscess, liver ascites, wound infection, wound dehiscence/non-healing (P < 0.001) (Table 5). Multivariate analysis revealed that POD after hepatic resection may be associated with perioperative complications: sepsis (OR = 1.61; CI = 36-1.91), dementia(OR = 3.46; CI = 2.74–4.37), urinary retention (OR = 1.80; CI = 1.43–2.34), gastrointestinal complication (OR = 1.70; CI = 1.23–2.35), acute renal failure (OR = 1.89; CI = 1.65–2.17), pneumonia (OR = 1.43; CI = 1.19–1.73), continuous invasive mechanical ventilation (OR = 1.82; CI = 1.33–2.49), blood transfusion (OR = 1.62; CI = 1.37–1.89), respiratory failure (OR = 1.50; CI = 1.19–1.9), wound dehiscence/ non-healing (OR = 2.53; CI = 1.57–4.09).
Discussion
Postoperative delirium often presents 24 to 96 h after surgery and presents with acute confusion, disorganized attention, and decreased perception of the environment, with symptoms that may or may not be related to organic disease and usually resolves during hospitalization [20]. It is estimated that about 4–61% of patients develop POD after surgery [21], which may lead to a cascade of adverse outcomes, such as lengthy hospitalization, loss of functional independence, and cognitive decline [6, 11, 22]. This investigation presents an extensive health-economic analysis of delirium following hepatic resection. Over the period spanning 2015 to 2019, the incidence of POD exhibited an upward trend, rising from approximately 1.04–1.53%. The comparatively low rates observed in 2015 may be attributed to the implementation of the ICD-10-CM coding system (Fig. 2). Our study revealed an overall occurrence of 1.46% following hepatic resection, significantly lower than the rates reported in the literature, which ranged from 8.4–22.4% [17, 23, 24]. Several possible reasons can also explain this apparent discrepancy. First, limitations of the National Inpatient Sample database, such as providing only in-hospital POD, high specificity (low false-positive rate), and low sensitivity (high false-negative rate), might result in an underestimation of the actual rates [19]. Secondly, the definition and diagnosis of delirium varies from agency to institution, depending on the criteria employed, which can also contribute to this discrepancy [16, 25, 26]. Third, the previous literature has observed a small and selective presence in older patients, resulting in a high incidence [17, 18, 24]. Fourth, differences in study design interpretation and diagnostic criteria could potentially account for the difference in the documented occurrence of postoperative delirium, whose clinical diagnosis can be prone to oversight [27]. Accordingly, larger, prospective case-control studies are warranted to understand the broader picture.
Advanced age is a well-known risk factor for POD [17, 18]. In accordance with previous reports, our findings revealed that advanced age was a robust predictor of POD after hepatic resection. Patients with POD tended to be 6 years older than those who were not affected. In addition, in terms of age distribution, patients over 65 years of age make up a larger proportion of the POD group. A potential explanation for this observation is that age-related factors, such as brain atrophy, diminished neuron density, decreased blood flow, and neurotransmitter level reductions, have been demonstrated to render the elderly population particularly susceptible to delirium [27, 28]. Additionally, we found that a smaller proportion of females were present in patients with POD, which was also found to be protective during logistic regression.
As expected, patients who underwent hepatic resections during elective surgery were associated with lower rates of POD, given that most patients admitted for elective surgery are in good health or have been adequately evaluated and prepared prior to surgery [29]. This finding was further confirmed by the finding that elective admission was a protective factor for POD. One possible reason why teaching hospitals are a predictor of in-hospital POD risk is that cases in these hospitals often have complex complications [30]. In addition, laparoscopic hepatectomy has developed rapidly [31], and many studies have shown that laparoscopic hepatectomy is safer and more feasible than open hepatectomy [31, 32]. In particular, the postoperative recovery was faster in the laparoscopic hepatectomy group than in the open hepatectomy group. These results are further validated by our findings that the incidence of in-hospital POD is significantly reduced with laparoscopic hepatectomy. In terms of the hospital bed capacity, hospitals categorized as medium or large capacity correlated with increased rates of POD, although the cause is unclear and may be due to multiple factors.
Several studies on POD after hepatic resection have shown that risk stratification, pre-screening, and optimal care are essential to improve prognosis [17, 18, 24]. Therefore, in order to prevent the occurrence of POD, emphasis should be placed on comprehending the preoperative risk factors. Logistic regression analysis results were consistent with the literature; the OR value was highest for psychosis due to other neurological disorders before surgery (36.58) (Table 4), indicating that these medical comorbidities were strongly correlated with POD and should be addressed preoperatively. Patients with a history of other neuropsychiatric disorders, such as depression (OR = 1.45) and psychoses (OR = 1.77), were identified as having an elevated risk of developing POD [17, 33]. Other comorbidities such as fluid and electrolyte disorders (OR = 1.27), coagulopathy (OR = 1.36), weight loss (OR = 1.59), and coagulopathy (OR = 1.53) had been documented as factors predisposing to POD [33, 34]. Interestingly, female (OR = 0.79), elective admission (OR = 0.61), and Private insurance (OR = 0.69) yielded a protective effect against POD, although the reasons are unknown and could be multifaceted. Several previous findings may be relevant and worth discussing. Melatonin is a hormone released by the pineal gland and associated with female hormones [34]. Previous studies have documented that changes in melatonin metabolism or disrupted circadian patterns may participate in POD pathogenesis [35].
Consistent with previous studies [36, 37], our data analysis showed that patients with POD had a median length of stay of six days longer and an increase in total hospital costs of $79,799 compared to patients who did not develop POD. POD may be associated with perioperative complications (sepsis, dementia, urinary retention, gastrointestinal complications, acute renal failure, pneumonia, continuous invasive mechanical ventilation, blood transfusion, respiratory failure) (Table 5). Besides, people with POD often have impairments in consciousness, perception, or cognitive function and are unable to follow guidance for care and rehabilitation [33, 38]. Patients with POD are more often paid through Medicare than those without POD. In addition, private insurance is a protective factor for POD, underscoring the significant influence of medical insurance type in this context. As a result, the increase in complications can result in more than three times the in-hospital mortality rate in delirium cases compared to those who are not affected. Therefore, the number of comorbidities was significantly higher in patients with POD since a higher number of comorbidities is indicative of poorer preoperative general conditions, and more comorbidities may contribute to heightened postoperative complications comprising delirium.
Although certain preoperative risk factors like advanced age, psychosis, depression, and neurological disorders are non-modifiable, it is beneficial for clinicians to engage in consultations with patients, obtain informed consent, and proactively manage those identified as being at a heightened risk of POD. Other factors predisposing to POD, including coagulopathy, weight loss, and fluid and electrolyte imbalances, are amenable to modification to some extent. Patients presenting with one or more of these comorbidities can undergo optimization to enhance their readiness for elective procedures. This optimization may involve interventions such as transfusions for patients with coagulopathy and effective management of fluid and electrolyte balance. Consequently, these findings hold significant importance and offer potential benefits in the treatment of POD following hepatic resection [33, 39]. Furthermore, Sensory deficit correction, it encourages the use of correctors and technical aids such as glasses, hearing aids, and dentures, among others; environmental management, installation of a clock and other orientation elements in the patient’s room to promote orientation, in addition to minimizing environmental stressors; sleep protocol, lowering of lights, noise, and administration of nighttime drugs; hydration protocol, monitoring of the patient’s hydration and access to it; and reduction of medication, which have proven to be highly effective in preventing POD [40, 41].
Our study offers notable strengths, encompassing a substantial sample size, national representativeness, and the application of multivariate regression models to mitigate confounding variables. However, it is imperative to recognize inherent shortcomings associated with the use of the National Inpatient Sample database. Firstly, the collection of each case data was confined to the duration of their hospital stay, thereby omitting complications or outcomes post-discharge, including readmission rates and long-term follow-up data from this database. Since only early-stage hospitalized cases are included, this limitation may lead to an underestimation of the incidence of POD [19, 23, 24]. Secondly, akin to any extensive administrative dataset, coding, and documentation discrepancies or misclassifications may occur [16, 19]. In addition, the evaluation is constrained to variables documented in the NIS database. Notably, the relevant surgical types and anesthetic factors that could potentially influence POD, such as no record of the duration of surgery, size of liver cancer, and invasion, and some indications for surgery (hepatocellular carcinoma, intrahepatic cholangiocarcinoma, metastatic cancer, and Others.) are not strictly defined, operation duration, anesthesia duration, anesthesia mode, and the selection of anesthetic agents, were not captured in the NIS database [17, 18]. This was a weakness of this study, but it did not affect the analysis of risk factors. The advantage of the NIS database is that the sample size is larger and the data is more convincing. The results of this study provide a better treatment strategy for the development of liver resection.
Conclusions
POD that occurs after hepatic resection is a costly complication, with an overall incidence of 1.46%. From 2015 to 2019, the annual incidence of POD gradually increased. This study identified several risk factors for POD after hepatic resection, including teaching hospitals, non-selective admissions, older male patients, depression, fluid and electrolyte disorders, coagulation disorders, and weight loss. In addition, POD is associated with sepsis, dementia, urinary retention, gastrointestinal complications, acute renal failure, pneumonia, continuous invasive mechanical ventilation, blood transfusion, respiratory failure, and wound dehiscence / non-healing. Young female patients, elective admissions, and private insurance were identified as protective factors. The incidence of POD following hepatic resection surgery is associated with higher total hospitalization costs, longer LOS, and higher in-hospital mortality.
Data availability
The datasets are available at https://www.ahrq.gov/data/hcup/index.html.
Abbreviations
- POD:
-
Postoperative Delirium
- ICD:
-
International Classification of Diseases
- NIS:
-
National Inpatient Sample
- ICU:
-
Intensive Care Unit
- LOS:
-
Length of Stay
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Chauhan K, Scaife S, Rosenbaum JT. Uveitis and health disparities: results from the National Inpatient Sample. Br J Ophthalmol. 2019;103(9):1301–5.
Gani F, Thompson VM, Bentrem DJ, Hall BL, Pitt HA, Pawlik TM. Patterns of hepatic resections in North America: use of concurrent partial resections and ablations. HPB: Official J Int Hepato Pancreato Biliary Association. 2016;18(10):813–20.
Fan ST, Lai EC, Lo CM, Ng IO, Wong J. Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis. Archives Surg (Chicago Ill : 1960). 1995;130(2):198–203.
Pol B, Campan P, Hardwigsen J, Botti G, Pons J, Le Treut YP. Morbidity of major hepatic resections: a 100-case prospective study. Eur J Surg = Acta Chir. 1999;165(5):446–53.
Jin S, Fu Q, Wuyun G, Wuyun T. Management of post-hepatectomy complications. World J Gastroenterol. 2013;19(44):7983–91.
Park SA, Tomimaru Y, Shibata A, Miyagawa S, Noguchi K, Dono K. Incidence and risk factors for postoperative delirium in patients after Hepatectomy. World J Surg. 2017;41(11):2847–53.
Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27–32.
Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443–51.
Milstein A, Pollack A, Kleinman G, Barak Y. Confusion/delirium following cataract surgery: an incidence study of 1-year duration. Int Psychogeriatr. 2002;14(3):301–6.
Scholz AF, Oldroyd C, McCarthy K, Quinn TJ, Hewitt J. Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. Br J Surg. 2016;103(2):e21–8.
Andrási TB, Talipov I, Dinges G, Arndt C, Rastan AJ. Risk factors for postoperative delirium after cardiac surgical procedures with cardioplegic arrest. Eur J cardio-thoracic Surgery: Official J Eur Association Cardio-thoracic Surg 62(1) (2022).
Bilotta F, Lauretta MP, Borozdina A, Mizikov VM, Rosa G. Postoperative delirium: risk factors, diagnosis and perioperative care. Minerva Anestesiol. 2013;79(9):1066–76.
Aranake-Chrisinger A, Avidan MS. Postoperative delirium portends descent to dementia. Br J Anaesth. 2017;119(2):285–8.
Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–74.
Wang E, Belley-Côté EP, Young J, He H, Saud H, D’Aragon F, Um K, Alhazzani W, Piticaru J, Hedden M, Whitlock R, Mazer CD, Kashani HH, Zhang SY, Lucas A, Timmerman N, Nishi C, Jain D, Kugler A, Beaver C, Kloppenburg S, Schulman S, Borges FK, Kavosh M, Wada C, Lin S, Sibilio S, Lauw M, Benz A, Szczeklik W, Mokhtari A, Jacobsohn E, Spence J. Effect of perioperative benzodiazepine use on intraoperative awareness and postoperative delirium: a systematic review and meta-analysis of randomised controlled trials and observational studies. Br J Anaesth. 2023;131(2):302–13.
Oh ST, Park JY. Postoperative delirium. Korean J Anesthesiology. 2019;72(1):4–12.
Ishihara A, Tanaka S, Ueno M, Iida H, Kaibori M, Nomi T, Hirokawa F, Ikoma H, Nakai T, Eguchi H, Shinkawa H, Hayami S, Maehira H, Shibata T, Kubo S. Preoperative risk Assessment for Delirium after hepatic resection in the Elderly: a prospective Multicenter Study. J Gastrointest Surgery: Official J Soc Surg Aliment Tract. 2021;25(1):134–44.
Nomi T, Kaibori M, Hirokawa F, Ueno M, Hokuto D, Noda T, Nakai T, Ikoma H, Iida H, Kubo S. Effect of laparoscopic liver resection on postoperative delirium in elderly patients with hepatocellular carcinoma. J Hepato-Biliary-Pancreat Sci. 2023;30(9):1111–8.
Edigin E, Kaul S, Eseaton PO. Analysis of hidradenitis suppurativa hospitalizations: a report from the National Inpatient Sample database. J Am Acad Dermatol. 2021;85(5):1357–60.
Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment, Nature reviews. Neurology. 2009;5(4):210–20.
Gleason LJ, Schmitt EM, Kosar CM, Tabloski P, Saczynski JS, Robinson T, Cooper Z, Rogers SO Jr., Jones RN, Marcantonio ER, Inouye SK. Effect of Delirium and other Major complications on outcomes after elective surgery in older adults. JAMA Surg. 2015;150(12):1134–40.
Sprung J, Roberts RO, Weingarten TN, Nunes Cavalcante A, Knopman DS, Petersen RC, Hanson AC, Schroeder DR, Warner DO. Postoperative delirium in elderly patients is associated with subsequent cognitive impairment. Br J Anaesth. 2017;119(2):316–23.
Chen YL, Lin HC, Lin KH, Lin LS, Hsieh CE, Ko CJ, Hung YJ, Lin PY. Low hemoglobin level is associated with the development of delirium after hepatectomy for hepatocellular carcinoma patients. PLoS ONE. 2015;10(3):e0119199.
Yoshimura Y, Kubo S, Shirata K, Hirohashi K, Tanaka H, Shuto T, Takemura S, Kinoshita H. Risk factors for postoperative delirium after liver resection for hepatocellular carcinoma. World J Surg. 2004;28(10):982–6.
Sun Z, Yang D. Postoperative delirium in geriatric patients. Anesth Analg. 2023;137(4):e38–9.
Yürek F, Lachmann C. [Postoperative Delirium], Anasthesiologie, Intensivmedizin, Notfallmedizin. Schmerztherapie: AINS. 2023;58(9):480–1.
Soundhar A, Udesh R, Mehta A, Schindler J, Jeevanantham V, Gleason T, Thirumala PD. Delirium following transcatheter aortic valve replacement: National Inpatient Sample Analysis. J Cardiothorac Vasc Anesth. 2017;31(6):1977–84.
Turner RC, Lucke-Wold BP, Robson MJ, Lee JM, Bailes JE. Alzheimer’s disease and chronic traumatic encephalopathy: distinct but possibly overlapping disease entities. Brain Injury. 2016;30(11):1279–92.
Yang QF, Lin ZM, Yang S, Wang PK, Chen R, Wang J. Incidence and risk factors of In-Hospital prosthesis-related complications following total knee arthroplasty: a Retrospective Nationwide Inpatient Sample Database Study. Orthop Surg. 2021;13(5):1579–86.
Reeves RA, Schairer WW, Jevsevar DS. The national burden of periprosthetic hip fractures in the US: costs and risk factors for hospital readmission. Hip International: J Clin Experimental Res hip Pathol Therapy. 2019;29(5):550–7.
Fretland A, Dagenborg ÅVJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, Hausken J, Tønnessen TI, Abildgaard A, Barkhatov L, Yaqub S, Røsok BI, Bjørnbeth BA, Andersen MH, Flatmark K, Aas E, Edwin B. Laparoscopic Versus Open Resection for Colorectal Liver metastases: the OSLO-COMET Randomized Controlled Trial. Ann Surg. 2018;267(2):199–207.
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, OʼRourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29.
Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Aceto P, Audisio R, Cherubini A, Cunningham C, Dabrowski W, Forookhi A, Gitti N, Immonen K, Kehlet H, Koch S, Kotfis K, Latronico N, MacLullich AMJ, Mevorach L, Mueller A, Neuner B, Piva S, Radtke F, Blaser AR, Renzi S, Romagnoli S, Schubert M, Slooter AJC, Tommasino C, Vasiljewa L, Weiss B, Yuerek F, Spies CD. Update of the European Society of Anaesthesiology and Intensive Care Medicine evidence-based and consensus-based guideline on postoperative delirium in adult patients, European journal of anaesthesiology (2023).
Fineberg SJ, Nandyala SV, Marquez-Lara A, Oglesby M, Patel AA, Singh K. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine. 2013;38(20):1790–6.
de Jonghe A, van Munster BC, van Oosten HE, Goslings JC, Kloen P, van Rees C, Wolvius R, van Velde R, Levi MM, Korevaar JC, de Rooij SE. The effects of melatonin versus placebo on delirium in hip fracture patients: study protocol of a randomised, placebo-controlled, double blind trial. BMC Geriatr. 2011;11:34.
Marcantonio ER, Simon SE, Bergmann MA, Jones RN, Murphy KM, Morris JN. Delirium symptoms in post-acute care: prevalent, persistent, and associated with poor functional recovery. J Am Geriatr Soc. 2003;51(1):4–9.
Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Aceto P, Audisio R, Cherubini A, Cunningham C, Dabrowski W, Forookhi A, Gitti N, Immonen K, Kehlet H, Koch S, Kotfis K, Latronico N, MacLullich AMJ, Mevorach L, Mueller A, Neuner B, Piva S, Radtke F, Blaser AR, Renzi S, Romagnoli S, Schubert M, Slooter AJC, Tommasino C, Vasiljewa L, Weiss B, Yuerek F, Spies CD. Update of the European Society of Anaesthesiology and Intensive Care Medicine evidence-based and consensus-based guideline on postoperative delirium in adult patients. Eur J Anaesthesiol. 2024;41(2):81–108.
Rai D, Garg RK, Malhotra HS, Verma R, Jain A, Tiwari SC, Singh MK. Acute confusional state/delirium: an etiological and prognostic evaluation. Ann Indian Acad Neurol. 2014;17(1):30–4.
van der Zanden V, Beishuizen SJ, Scholtens RM, de Jonghe A, de Rooij SE, van Munster BC. The effects of blood transfusion on Delirium Incidence. J Am Med Dir Assoc. 2016;17(8):748–53.
Alvarez EA, Rojas VA, Caipo LI, Galaz MM, Ponce DP, Gutierrez RG, Salech F, Tobar E, Reyes FI, Vergara RC, Egaña JI, Briceño CA, Penna A. Non-pharmacological prevention of postoperative delirium by occupational therapy teams: a randomized clinical trial. Front Med. 2023;10:1099594.
Deeken F, Sánchez A, Rapp MA, Denkinger M, Brefka S, Spank J, Bruns C, von Arnim CAF, Küster OC, Conzelmann LO, Metz BR, Maurer C, Skrobik Y, Forkavets O, Eschweiler GW, Thomas C. Outcomes of a Delirium Prevention Program in older persons after elective surgery: a stepped-Wedge Cluster Randomized Clinical Trial. JAMA Surg. 2022;157(2):e216370.
Funding
This study was funded by the Natural Science Foundation of Gansu Province (20JR10RA730 to Min Wang).
Author information
Authors and Affiliations
Contributions
RL, SS and NL contributed to the study design, data acquisition and analysis, interpretation of results, and writing and revising the manuscript. WF and MW contributed to the study design, interpretation of results, and reviewing the manuscript. ZD contributed to data acquisition, data analysis, and reviewing of the manuscript. QY contributed to the study design, interpretation of results, and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable. Administrative permissions were required to access the raw data used in this study and the corresponding author’s (Zhen Deng) work unit (The First School of Clinical Medicine, Southern Medical University, Guangzhou, Guangdong, 510515, China.) has already granted permission from Agency for Healthcare Research and Quality (AHRQ) to access Healthcare Cost and Utilization Project (HCUP) Nationwide Databases. However, this observational study used deidentifed publicly available data, hence there was no requirement for consent to participate and it was deemed exempt by the ethics committee. So there is no need to grant permission in the Ethics approval and consent to participate section. What is more, the data used in this study were no need anonymized before its use. All methods are carried out following relevant guidelines and regulations. The data used in this study were not need anonymized before its use.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, R., Liu, N., Suo, S. et al. Incidence and risk factors of postoperative delirium following hepatic resection: a retrospective national inpatient sample database study. BMC Surg 24, 151 (2024). https://doi.org/10.1186/s12893-024-02436-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-024-02436-w