Abstract
Background
Anaplastic thyroid cancer (ATC) is a rare and aggressive malignancy with a poor prognosis, particularly in patients presenting with distant metastasis (DM). This study aimed to assess the effect of combination treatment strategies on survival in ATC patients with DM.
Methods
A retrospective analysis was conducted using data from the Surveillance, Epidemiology, and End Results (SEER) database to identify primary ATC cases with DM at diagnosis. Univariate and multivariate Cox proportional hazards regression analyses were performed to identify independent risk factors for survival.
Results
Of the 315 ATC patients with DM included in the study, surgery to the primary tumor, radiotherapy, chemotherapy, and lung metastasis were identified as independent risk factors for survival. Patients who received primary tumor surgery plus chemotherapy or surgery plus chemoradiation exhibited a superior outcome compared to those who received only one treatment modality.
Conclusion
Our findings suggest that a combination treatment approach, particularly surgery combined with radiotherapy or surgery combined with chemoradiotherapy, may provide the most optimal treatment option for ATC patients with DM. These results may provide some evidence for clinical decision making, but larger sample cohorts are still needed for validation.
Similar content being viewed by others
Introduction
Thyroid cancer is the most prevalent type of endocrine cancer, and its incidence has tripled over the last three decades [1]. Among thyroid cancers, anaplastic thyroid carcinoma (ATC) is the most aggressive cancer type [2], with a median survival of only four months and less than half of patients surviving beyond six months [3]. Distant metastasis (DM) occurs in approximately 50% of patients at the time of diagnosis and is a crucial prognostic factor for disease-specific mortality [4].
Various anti-cancer treatments, including surgery to the primary tumor, radiotherapy, and chemotherapy, have been associated with improved survival in ATC patients [5]. Current guidelines recommend both aggressive therapy and palliative care for ATC patients with DM. However, the effectiveness of combination therapy in patients with DM is still uncertain [6, 7]. This study aimed to evaluate the effectiveness of multimodal treatment strategies for ATC patients with DM using the Surveillance, Epidemiology, and End Results (SEER) program.
Methods
Database and case selection
Population-based data for this study were obtained from the SEER 17 database, which covers approximately 26.5% of the US population. Patients diagnosed with metastatic ATC diagnosed in 2010 and 2020 were identified using SEER*Stat software (version 8.4.1; seer.cancer.gov/seerstat). Thyroid cancer was identified using ICD-O-3 codes (C79.3), and ATC was identified using ICD-O-3 histology codes (8021–8035) [8]. Squamous cell carcinoma (8070–8076) was also included as ATC according to the latest WHO classification [9]. The following demographic and clinical variables were collected: age, gender, race, year of diagnosis, TNM stage, distant metastatic sites (bone, brain, liver, lung, distant lymph node), treatment (surgery to primary site, radiotherapy, and chemotherapy), overall survival (OS), cancer-specific survival (CSS), and survival time. Tumor diameter and extension were recorded based on the “Collaborative Stage (CS) tumor size” and “CS extension” for patients diagnosed before 2015, and “Tumor size summary” and “Extent of Disease (EOD) primary tumor” were recorded for patients diagnosed after 2015. The T stage of patients was adjusted to AJCC 8th edition according to tumor size and extension [10]. The surgical approach on the primary site was defined according to “Site-Specific Surgery of Primary Site Codes,” with code 40 (subtotal or near-total thyroidectomy), 50 (total thyroidectomy), and 80 (thyroidectomy, not otherwise specified) defined as thyroidectomy. Code 00 was defined as no surgical treatment on thyroid, and other codes were defined as non-thyroidectomy. According to the SEER manual, ‘beam radiation’ is defined as ‘beam radiation directed to cancer tissue’. Therefore, patients coded as “beam radiation” in this database were considered to have received radiotherapy. Only patients diagnosed with their first malignancy were included, and those without distant metastasis at initial diagnosis, unknown demographic characteristics and treatment data, or unknown involvement of distant sites were excluded.
Statistical analysis
The primary outcomes of this study were cancer-specific survival (CSS) and overall survival (OS). Kaplan-Meier survival curves and the log-rank test were employed to compare the CSS and OS between groups. Multivariate Cox regression analysis was used to identify independent prognostic factors, with hazard ratios (HRs) calculated along with 95% confidence intervals (CIs).
All statistical tests were two-sided, with P values of < 0.05 considered statistically significant unless otherwise stated. Kaplan-Meier analysis was performed using Graphpad Prism 9 (Dotmatics). Multivariate Cox regression analysis was conducted using R version 4.2.1 (R Foundation for Statistical Computing).
Results
The basic characteristics of patients
Table 1 presents the baseline clinical characteristics of the 315 patients included in this study. The median age at diagnosis was 70 years, and approximately half of the patients were female (50.79%) and non-Hispanic white (57.78%). The majority of patients were at T4 (73.65%) and N1 (74.92%) stage, with 250 (79.37%) exhibiting extrathyroidal extension. The most common metastatic site was the lung, identified in 266 (84.44%) patients, and 71 (22.54%) patients exhibited multiple organ metastases. Of the 315 patients, 113 (35.87%) underwent a surgical procedure, 183 (58.10%) received radiotherapy, and 149 (47.30%) received chemotherapy.
The metastatic pattern and survival of patients
Among the 315 patients included in this study, 297 had distant organ metastasis, while 18 (5.71%) had only distant lymph node (LN) metastasis (Fig. 1A). Of the 71 patients with multiple organ metastases, 58 (81.69%) had two distant organ metastases, 12 (16.90%) had three distant organ metastases, and only one (1.41%) had four organ metastases (Fig. 1B). Among the 226 patients with single organ metastasis, lung metastasis was the most common, with 199 (88.05%) presenting with lung metastasis, 21 (9.29%) with bone metastasis, and 3 (1.33%) each with brain and liver metastasis (Fig. 1C).
Pie charts showing the metastatic patterns of ATC patients. (A) Metastatic pattern of distant lymph node and distant organ in all 315 patients. (B) Number of organs involved of 71 patients with multiple organ metastases. (C) Metastatic site of 226 patients with one organ metastasis. LN: lymph node. Met/Mets: metastasis/metastases
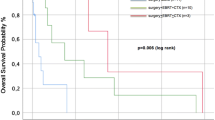
We subsequently assessed the survival of patients with different metastatic patterns. Our analysis revealed no significant difference in OS and CSS among patients with only distant LN metastasis, single distant organ metastasis, and multiple distant organ metastases (Fig. 2A-B). The number of multi-organ metastases was not significantly associated with patient prognosis (Fig. 2C-D). However, among patients with single distant organ metastasis, OS was worse in those with lung metastasis (Fig. 2E), and this trend was also reflected in CSS (Fig. 2F).
Overall survival (OS) and cancer-specific survival (CSS) of patients with different metastatic patterns. (A-B): OS and CSS of patients with distant lymph node or organ metastasis. (C-D): OS and CSS of patients with multiple organ metastases. (E-F): OS and CSS of patients with single organ metastasis
Analysis of prognostic factors for OS and CSS in ATC patients with DM
We performed univariate Cox regression analysis on all variables to examine the impact of different factors on OS in ATC patients with DM. Our data indicated that being male, younger than 65 years old, having a tumor diameter less than 6 cm, no lung metastasis, undergoing surgery to the primary site, and receiving radiotherapy or chemotherapy were associated with favorable OS. In multivariate Cox regression analysis, all factors except gender were found to be independent prognostic factors affecting OS in ATC patients with DM (Table 2). The factors affecting CSS were similar to those affecting OS, with age, tumor diameter, lung metastasis, surgery, radiotherapy, and chemotherapy identified as independent risk factors (Table 3).
The treatment strategy of ATC patients with DM
We further investigated the prognosis of patients receiving different treatment regimens, given that surgery on the primary site, radiotherapy, and chemotherapy were all associated with better survival. Patients who received treatment had better OS and CSS than those who did not receive treatment, and those who received multimodal therapy had better outcomes than those who received single therapy. The median OS and CSS of patients who received no treatment, single treatment, two treatments, and three treatments were both 0.1, 2, 4, and 7 months, respectively (Fig. 3A-B).
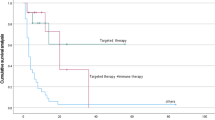
We then examined whether there were prognostic differences between the different treatment strategies. Our data showed no differences in patients who received single treatment (Fig. 3C-D). However, among patients who received multimodal therapy, surgery on the primary site plus chemotherapy (median OS and CSS were 8 months) had a prognosis comparable to that of patients who received surgery on the primary site plus chemoradiotherapy and better than those who received surgery on the primary site combined with radiotherapy (median OS and CSS were 2 months) as well as those in the chemoradiotherapy group (median OS and CSS were 4 months) (Fig. 3E-F).
Discussion
ATC is a rare form of thyroid tumor with an extremely poor prognosis and a high rate of distant metastasis. Previous studies have shown that nearly half of the patients present with DM [8, 11]. Current guidelines recommend surgery, radiotherapy, and chemotherapy for patients with DM from ATC, but it remains unclear whether combination therapy can further improve patient prognosis [6, 7]. In this study, we retrospectively analyzed a large cohort from the SEER database to demonstrate the value of multimodal treatment for the survival of ATC patients with DM.
The impact of metastatic patterns on thyroid cancer prognosis is still controversial. Some studies have reported that the lung is the most common metastatic site for thyroid cancer [12, 13], Matsuzu and colleagues found that patients with lung metastasis had a worse prognosis than those with metastasis to other organs in papillary thyroid carcinoma [14], while Sampson et al. reported that patients with lung metastasis had a better survival than those with bone metastasis [15]. Studies by Vuong and Shao et al. concluded that patients with multiple distant organ metastases had a worse prognosis [8, 16]. However, these studies often include multiple pathological types in the analysis, with varying prognoses. No study has been conducted to evaluate whether metastatic patterns affect the prognosis of patients with ATC. Our study found that lung metastasis was the most common in patients with ATC, with 71 patients (22.54%) having multiple organ metastases and 18 patients (5.71%) having only distant lymph node metastasis. Our analysis showed that patients with lung metastasis had worse OS than those with metastasis to other organs, while other distant metastatic patterns were not significantly associated with survival. This may be due to the small number of patients with different distant metastasis patterns, making it difficult to reach statistically significant differences in subgroup analysis, given the median survival of ATC with DM is only 3 months [17].
Non-treatment factors, such as age, gender, tumor size, and treatment factors, have been reported as predictive factors in ATC patients [5, 18, 19]. Age has been associated with thyroid cancer-specific survival and is included in the AJCC staging system for patients with differentiated thyroid cancer [20]. In our study, being older than 65 years was a negative prognostic factor, which was consistent with the findings of Gui and Wang et al. [19, 21]. The predictive value of tumor diameter was controversial in different studies [5, 21, 22], potentially due to the different cutoff values used in those studies. Our analysis showed that tumor diameter greater than 6 cm was an unfavorable indicator in ATC patients with DM, which confirmed the results of Glaser et al. [5]. Lung metastasis, which was correlated with shorter OS, was confirmed as an independent risk factor. Treatment factors, including surgery to the primary tumor, radiotherapy, and chemotherapy, were all protective factors for OS and CSS, consistent with previous studies [5, 23].
Given that all treatments were shown to be protective factors for patient survival, our study aimed to investigate the impact of different treatment combinations on patient prognosis. Previous studies have suggested that chemoradiotherapy is more effective than radiotherapy alone in patients with ATC [24], a and data by Song et al. has also suggested that surgery-based multimodal therapy improves patients’ prognosis [25], indicating the potential benefit of multimodal treatment compared to monotherapy for patients with ATC. Our results demonstrated that patients who received a combination of two to three treatments had significantly better OS and CSS than those who received only a single treatment, and that the survival of patients who received any treatment was better than that of untreated patients. We then analyzed different treatment combinations and found that chemoradiotherapy was not as effective as other combinations, while surgery plus chemotherapy had comparable survival to patients receiving all three treatments. Surgical treatment is generally not suitable for all patients due to extensive disease, but complete surgical resection is recommended for tumors limited to the thyroid parenchyma [26]. Although our study concluded that the prognosis of patients is not significantly affected by the status of the surgical margins [27], the determination of the extent of surgical resection remains a key concern, considering the widespread invasion of adjacent organs by ATC. Regarding chemotherapy, doxorubicin combined with taxanes and/or platins has been the standard of care for many years [28], and paclitaxel-based regimens are also recommended for ATC patients [29, 30]. Recent clinical trials have demonstrated that for patients with the BRAF V600E mutation, dabrafenib plus trametinib significantly improved survival [31]. Despite the fact that new chemotherapeutic agents and regimens continue to be proposed, the response rate in ATC patients is relatively low, and further research is needed on the pharmacological treatment of ATC patients. Radiotherapy could reduce the risk of local recurrence and regional complications [32], but its benefits to patients with DM remains unclear [33]. The acute toxicity induced by radiotherapy may affect its benefits, and future studies should investigate ways to improve the dose and modality of radiotherapy to reduce its toxic effects while retaining local control.
Our study is the largest study to date providing data on the value of multimodal treatment in ATC patients with DM. Despite its clinical significance, there are also limitations to this study. Firstly, the selection biases of retrospective studies cannot be avoided. Secondly, the SEER database only presents data at the time of diagnosis, and the efficacy of different treatments and changes in tumor parameters during follow-up are not available, which limits further evaluation of the effects of different treatment options. In addition, the SEER database is unable to provide specific regimens for radiotherapy or chemotherapy, including the specific areas targeted by radiation and the chemotherapy regimens. So, it was not clear that all of the radiotherapy was directed at primary thyroid tumor, which also compromises data completeness. Therefore, our findings need to be further validated in real-world data.
Conclusions
Our study included 315 ATC patients with DM, and the analysis showed no significant difference in OS and CSS between the different metastatic patterns. All treatment regimens were identified as independent protective factors for OS and CSS. Specifically, surgery combined with chemotherapy or surgery combined with chemoradiotherapy was associated with better survival compared to monotherapy or other combination treatment modalities. The study was based on a retrospective analysis of the SEER database, and these findings still need to be validated by a larger sample of cohort studies.
Data availability
The SEER database analyzed in the current study are available at https://seer.cancer.gov/.
Abbreviations
- ATC:
-
Anaplastic thyroid cancer
- CS:
-
Collaborative stage
- CSS:
-
Cancer-specific survival
- DM:
-
Distant metastasis
- EOD:
-
Extent of disease
- HR:
-
Hazard ratio
- OS:
-
Overall survival
- RT:
-
Radiotherapy
- SEER:
-
The surveillance, epidemiology, and end results
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71:209–49.
Smallridge RC, Ain KB, Asa SL, Bible KC, Brierley JD, Burman KD, et al. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012;22:1104–39.
Lin B, Ma H, Ma M, Zhang Z, Sun Z, Hsieh IY, et al. The incidence and survival analysis for anaplastic thyroid cancer: a SEER database analysis. Am J Transl Res. 2019;11:5888–96.
Nixon IJ, Whitcher MM, Palmer FL, Tuttle RM, Shaha AR, Shah JP, et al. The impact of distant metastases at presentation on prognosis in patients with differentiated carcinoma of the thyroid gland. Thyroid. 2012;22:884–9.
Glaser SM, Mandish SF, Gill BS, Balasubramani GK, Clump DA, Beriwal S. Anaplastic thyroid cancer: prognostic factors, patterns of care, and overall survival. Head Neck. 2016;38(Suppl 1):E2083–90.
Bible KC, Kebebew E, Brierley J, Brito JP, Cabanillas ME, Clark TJ, et al. 2021 American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2021;31:337–86.
Haddad RI, Bischoff L, Ball D, Bernet V, Blomain E, Busaidy NL, et al. Thyroid carcinoma, version 2.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20:925–51.
Vuong HG, Le MK, Hassell L, Kondo T, Kakudo K. The differences in distant metastatic patterns and their corresponding survival between thyroid cancer subtypes. Head Neck. 2022;44:926–32.
Baloch ZW, Asa SL, Barletta JA, Ghossein RA, Juhlin CC, Jung CK, et al. Overview of the 2022 WHO classification of thyroid neoplasms. Endocr Pathol. 2022;33:27–63.
Xiang J, Wang Z, Sun W, Zhang H. A relook at the 8th edition of the AJCC TNM staging system of anaplastic thyroid carcinoma: a SEER-based study. Clin Endocrinol (Oxf). 2021;94:700–10.
Kebebew E, Greenspan FS, Clark OH, Woeber KA, McMillan A. Anaplastic thyroid carcinoma. Treatment outcome and prognostic factors. Cancer. 2005;103:1330–5.
Besic N, Gazic B. Sites of metastases of anaplastic thyroid carcinoma: autopsy findings in 45 cases from a single institution. Thyroid. 2013;23:709–13.
Hugen N, Sloot YJE, Netea-Maier RT, van de Water C, Smit JWA, Nagtegaal ID, et al. Divergent metastatic patterns between subtypes of thyroid carcinoma results from the nationwide Dutch pathology registry. J Clin Endocrinol Metab. 2020;105:e299–306.
Matsuzu K, Sugino K, Masudo K, Mori K, Ono R, Yamazaki H, et al. Clinical outcomes and risk stratification for papillary thyroid carcinoma presenting with distant metastasis before the era of tyrosine kinase inhibitors. Endocr J. 2020;67:869–76.
Sampson E, Brierley JD, Le LW, Rotstein L, Tsang RW. Clinical management and outcome of papillary and follicular (differentiated) thyroid cancer presenting with distant metastasis at diagnosis. Cancer. 2007;110:1451–6.
Shao Y, Li G, Wei T, Gong R, Li Z, Zhu J, et al. Distant metastasis in medullary thyroid carcinoma: clinical outcomes and implications of T stage. Clin Endocrinol (Oxf). 2022;97:676–84.
Smallridge RC, Copland JA. Anaplastic thyroid carcinoma: pathogenesis and emerging therapies. Clin Oncol. 2010;22:486–97.
Kim TY, Kim KW, Jung TS, Kim JM, Kim SW, Chung KW, et al. Prognostic factors for Korean patients with anaplastic thyroid carcinoma. Head Neck. 2007;29:765–72.
Wang M, Wei T, Gong R, Zhu J, Li Z. Risk stratification in patients with anaplastic thyroid carcinoma: role of age. Endocrine. 2022;77:305–18.
Nixon IJ, Wang LY, Migliacci JC, Eskander A, Campbell MJ, Aniss A, et al. An international multi-institutional validation of age 55 years as a cutoff for risk stratification in the AJCC/UICC staging system for well-differentiated thyroid cancer. Thyroid. 2016;26:373–80.
Gui W, Zhu W, Lu W, Shang C, Zheng F, Lin X, et al. Development and validation of a prognostic nomogram to predict overall survival and cancer-specific survival for patients with anaplastic thyroid carcinoma. PeerJ. 2020;8:e9173.
Sugitani I, Miyauchi A, Sugino K, Okamoto T, Yoshida A, Suzuki S. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC research consortium of Japan cohort study of 677 patients. World J Surg. 2012;36:1247–54.
Chen J, Tward JD, Shrieve DC, Hitchcock YJ. Surgery and radiotherapy improves survival in patients with anaplastic thyroid carcinoma: analysis of the surveillance, epidemiology, and end results 1983–2002. Am J Clin Oncol. 2008;31:460–4.
Zhou W, Yue Y, Zhang X. Radiotherapy plus chemotherapy leads to prolonged survival in patients with anaplastic thyroid cancer compared with radiotherapy alone regardless of surgical resection and distant metastasis: a retrospective population study. Front Endocrinol (Lausanne). 2021;12:748023.
Song T, Chen L, Zhang H, Lu Y, Yu K, Zhan W, et al. Multimodal treatment based on thyroidectomy improves survival in patients with metastatic anaplastic thyroid carcinoma: a SEER analysis from 1998 to 2015. Gland Surg. 2020;9:1205–13.
Nel CJ, van Heerden JA, Goellner JR, Gharib H, McConahey WM, Taylor WF et al. Anaplastic carcinoma of the thyroid: a clinicopathologic study of 82 cases. Mayo Clin Proc. 1985;60:51–8.
McIver B, Hay ID, Giuffrida DF, Dvorak CE, Grant CS, Thompson GB, et al. Anaplastic thyroid carcinoma: a 50-year experience at a single institution. Surgery. 2001;130:1028–34.
Shimaoka K, Schoenfeld DA, DeWys WD, Creech RH, DeConti R. A randomized trial of doxorubicin versus doxorubicin plus cisplatin in patients with advanced thyroid carcinoma. Cancer. 1985;56:2155–60.
Ain KB, Egorin MJ, DeSimone PA. Treatment of anaplastic thyroid carcinoma with paclitaxel: phase 2 trial using ninety-six-hour infusion. Collaborative Anaplastic Thyroid Cancer Health Intervention Trials (CATCHIT) Group Thyroid. 2000;10:587–94.
Higashiyama T, Ito Y, Hirokawa M, Fukushima M, Uruno T, Miya A, et al. Induction chemotherapy with weekly paclitaxel administration for anaplastic thyroid carcinoma. Thyroid. 2010;20:7–14.
Subbiah V, Kreitman RJ, Wainberg ZA, Cho JY, Schellens JHM, Soria JC, et al. Dabrafenib plus trametinib in patients with BRAF V600E-mutant anaplastic thyroid cancer: updated analysis from the phase II ROAR basket study. Annals Oncology: Official J Eur Soc Med Oncol. 2022;33:406–15.
Nachalon Y, Stern-Shavit S, Bachar G, Shvero J, Limon D, Popovtzer A. Aggressive palliation and survival in anaplastic thyroid carcinoma. JAMA otolaryngology– head neck Surg. 2015;141:1128–32.
Kwon J, Kim BH, Jung HW, Besic N, Sugitani I, Wu HG. The prognostic impacts of postoperative radiotherapy in the patients with resected anaplastic thyroid carcinoma: a systematic review and meta-analysis. European journal of cancer (Oxford, England: 1990). 2016;59:34–45.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization, H.G. and H.L.; methodology, H.G.; software, H.L.; investigation, H.L.; writing—original draft preparation, H.G.; writing—review and editing, H.L.; supervision, H.L. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patients’ data from the SEER database is public and anonymous, ethical approval and informed consent are not applicable in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guo, H., Lin, H. The value of multimodal treatment in anaplastic thyroid cancer patients with distant metastasis. BMC Surg 24, 79 (2024). https://doi.org/10.1186/s12893-024-02375-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-024-02375-6