Abstract
Background
We mainly evaluated whether preserving the inferior mesenteric artery (IMA) sheath to dissecting IMA root lymph nodes (also called No.253 lymph nodes) would benefit patients in terms of comparable lymph-node yield removed during operation and postoperative complications in laparoscopic radical resection of rectal cancer.
Methods
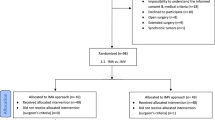
This is a prospective study included 141 rectal cancer patients who received laparoscopic radical resection during September 2018 to December 2020. All patients were randomly assigned to the preserved group (n = 71) and the peeled group (n = 70). The baseline characteristics, pathological features, intraoperative and postoperative data outcomes and complications were analyzed by independent samples t test, chi-square test or Fisher’s exact test between the 2 groups.
Results
The baseline characteristic and pathological features had no statistical difference between the 2 groups. The preserved group had a shorter operative time (P = 0.002), a shorter lymph node dissection time (P < 0.001), less intraoperative bleeding (P = 0.004), an earlier time to first flatus (P = 0.013), an earlier time to fluid intake (P = 0.033) and a shorter length of hospitalization (P = 0.012) than the peeled group. The differences between the 2 groups were not statistically significant (P > 0.05) in regard to the total number of lymph nodes cleared, positive lymph nodes, bleeding, anastomotic leakage, pneumonia, wound infection, abscess, ileus, urinary retention, urinary tract infection and chyle leakage.
Conclusion
Preserving of the IMA sheath in laparoscopic radical surgery for rectal cancer will reduce the total operation time and the length of hospitalization. This surgical method could lead to lower complication rate and faster recovery.
Trial registration
The study was approved by the Ethics Committee of The First Affiliated Hospital of Wannan Medical College and registered by the China Clinical Trials Registry (ChiCTR2200060830, Date of Registration:2022-06-12 -retrospective registration) http://www.chictr.org.cn/index.aspx.
Similar content being viewed by others
Introduction
There were 4.064 million new cases of cancer and 2.413 million new deaths occurred in 2016 and showing a continuing upward trend in China [1]. The colorectal cancer is the second most common cause of cancer death, with the incidence in adults age 50 years or younger increasing by 1.5% per year from 2014 to 2018 in the USA, and the 5-year survival rate in the UK is only 50% [2,3,4]. Therefore, it is important for doctors to improve treatment outcomes in colorectal cancer patients.
Even so, there are numerous ways to treat rectal cancer, including surgery, radiation, chemotherapy, molecular targeted therapies, immunotherapies, and Chinese herbal medications. Some molecular targeted drugs, such as cetuximab, panitumumab and bevacizumab, have been shown to play important roles in the treatment of rectal cancer [5,6,7]. Some immunotherapy drugs that can help improve the immune system of rectal cancer patients, react and kill tumor cells, such as nivolumab and pembrolizumab, have been developed and have achieved good clinical efficacy, and some drugs have even been included in the treatment guidelines for colorectal cancer [8,9,10]. Like artemisinin, which can effectively treat malaria, Chinese herbal medicine has achieved therapeutic effects on colorectal cancer in previous practices. Some special ingredients contained in Chinese herbal medicine can kill tumor cells, and the treatment of colorectal cancer with traditional Chinese medicine has been included in the treatment guidelines of CSCO [11,12,13]. Laparoscopic radical resection of rectal cancer is a key component of these techniques. As it results in less surgical damage and accomplishes better lymph node dissection than traditional laparotomy, laparoscopic radical surgery for rectal cancer is becoming more and more popular among surgeons [14, 15].
Different scholars have different opinions regarding laparoscopic radical surgery for rectal cancer, and many studies have been performed on the dissection of No.253 lymph nodes, but few clinical studies have been conducted on the preservation of the IMA sheath during the dissection of No.253 lymph nodes. In the past, we thought that peeling the IMA sheath would increase the detection rate of No.253 lymph nodes in patients with rectal cancer [16]. But now scholars have the opposite opinion. Professor Gong ‘s [17] research findings that peeling the IMA sheath can increase surgical and anesthesia time, and may also cause bleeding damage to the IMA, thereby increasing the surgical risk for patients. Compared to preserving the vascular sheath, peeling the vascular sheath does not increase the number of lymph node dissection and improve the quality of surgery.
We designed this prospective randomized controlled study to investigate whether preserving the IMA sheath is more advantageous in lymph node dissection treatment and postoperative complications compared to peeling the IMA sheath to clean the lymph nodes at the root of the IMA.
Materials and methods
Study population
This is a prospective randomized controlled trial included 141 rectal cancer patients who received laparoscopic radical resection during September 2018 to December 2020, in the Department of Gastrointestinal Surgery, The First Affiliated Hospital of Wannan Medical College. All patients were prospectively and randomly assigned to the preserved group (n = 71) and the peeled group (n = 70) by envelope method. Both groups of patients underwent Dixon surgery for laparoscopic radical resection of rectal cancer, while the patient’s left colic artery (LCA) was preserved during the surgery. Patients with preserved IMA sheaths were placed in the preserved group, and patients with peeled IMA sheaths were placed in the peeled group. All patients and their families communicated with providers and signed informed consent forms before surgery. This study had been performed in accordance with the principles stated in the Declaration of Helsinki. The study was approved by the Ethics Committee of The First Affiliated Hospital of Wannan Medical College and registered by the China Clinical Trials Registry (ChiCTR2200060830).
Inclusion and exclusion criteria
The inclusion criteria were as follows: preoperative pathology showing adenocarcinoma, preoperative diagnosis of stage T1-T3(according to the American Joint Committee on Cancer (AJCC) 7th edition TNM tumor staging criteria) rectal cancer by CT or MRI with a range of 5-15 cm from the anal verge, single rectal tumor lesion with no distant metastases, preoperative American Society of Anesthesiologists (ASA) rating of I-III, no emergency surgery, and no preoperative radiotherapy or other antineoplastic treatment.
Exclusion criteria were as follows: conversion to open surgery during laparoscopic surgery; intraoperative finding of mesenteric metastases or local invasion; intraoperative IMA root ligation for bleeding; and patients with comorbid systemic diseases that are inoperable, such as severe coagulation dysfunction, severe liver disease, severe renal disease, severe cardiac disease, severe pulmonary disease or other systemic malignancies. All patients received oral antibiotics 3 days prior to surgery to prevent infection and a cleansing enema 1 day prior to surgery. Those with one or more of the above conditions were excluded. A flow diagram for the study participant screening and grouping is shown in Fig. 1.
Randomization
The researchers, not the operators, put one of the two surgical schemes into an opaque envelope which has the same appearance and size and 100 envelopes are allocated for each scheme. After these envelopes are completely messed up, write a code on the outside of the envelope, seal it and give it to the operator. When a research object enters the study, if it meets the inclusion criteria and exclusion criteria, number the patient, open the corresponding numbered envelope, and perform the surgery according to the grouping scheme in the envelope. The treatment plan received by each subject was determined by the generated random sequence.
Surgical methodology
All the operations were performed by the same team of surgeons following the established grouping requirements. The patient was placed in a supine head-high, leg-low position under general anesthesia via tracheal intubation. Disinfecting the skin, and laying sterile sheets routinely, the abdominal cavity was routinely explored, peeling the right paramedian rectal sulcus with an ultrasound knife. The left mesorectal was separated along the abdominal aorta, the inferior mesenteric plexus was exposed, the IMA was exposed, and lymph node dissection from the beginning of the IMA to the beginning of the LCA without peeling the IMA sheath was performed in the preserved group. In the preserved group, the IMA sheath was not peeled, and the lymph nodes and adipose tissue in the No.253 lymph nodes area were dissected outside the IMA sheath. In the peeled group, the IMA sheath was peeled, and the lymph nodes were dissected at No.253 lymph nodes, the LCA, sigmoid artery (SA) and superior rectal artery (SRA) were exposed. To peel the IMA sheath, we gently peeled the IMA sheath from the root of the IMA with the ultrasound knife and then carefully and gently pushed the nonworking side of the ultrasound knife through the gap between the sheath and the vessel to the bifurcation of the IMA and the LCA, peeling away the intact IMA sheath. Before peeling the IMA sheath, we would carefully free the lymph and adipose tissue at the root of the IMA, expose and protect the root nerve plexus that runs along both sides of the IMA root. Generally, we operated from the point 0.5 cm away from the connection between the IMA and the abdominal aorta to avoid thermal damage to the nerves and blood vessels. The surrounding adipose tissue and lymph nodes were gently dissected, completing the dissection of the No.253 lymph nodes (Fig. 2). The No.253 lymph nodes were cleared, the inferior mesenteric vein (IMV) was ligated at the intersection with the LCA, and the SA and SRA were ligated and dissected. The area for No.253 lymph nodes dissection was delineated by the IMV on the left, the abdominal aorta on the right, the duodenum on the cephalic side and the area of the angle between the IMA and the LCA on the caudal side (Fig. 3). We dissected the sigmoid and descending colonic mesentery and loosened the lateral mesentery to the splenic area if tension was excessive. We exposed the posterior rectal space downward and the inferior epigastric plexus and separated the sides of the anterior sacral space to the pararectal sulcus, the lateral space, the anterior rectal space, and the lower edge to 2 cm below the tumor, taking care to protect the plexus and the bare rectal bowel wall. The distance to the lower margin of rectal resection was determined, the rectum was cut by a linear cutter stapler (Echelon Flex, Johnson & Johnson) at least 2 cm away from the lower edge of the tumor. Then we used a 3–5 cm vertical incision below the umbilicus, beyond this length we defined it as an intraoperative transverse abdomen, and the severed intestinal canal was pulled out from the abdominal cavity. Then, we trimmed the colon mesentery to better remove the tumor and perform intestinal anastomosis and cut the intestinal canal at a distance of 10 cm from the upper edge of the tumor. An iodine gauze strip was used to disinfect the intestinal cavity. A circular stapler anvil (Echelon Flex, Johnson & Johnson) was placed in the proximal intestinal canal, tied and fixed in the intestinal canal before putting it into the abdominal cavity. The assistant disinfected the external skin of the anus with iodine gauze again, relaxed and expanded the anus with fingers, and then placed a circular stapler (Echelon Flex, Johnson & Johnson) from the anus to anastomose with the anvil in the abdominal cavity. Injected about 50-100ml of diluted iodine solution from the anus into the intestinal canal to check if there were any gaps at the anastomosis. Then, reinforced and sutured the anterior wall of the rectum with absorbable suture at the anastomosis site.
Statistical analysis
All categorical data were measured in numbers or percentages. Microsoft Excel was used for clinical data collection. Statistical Package for Social Science (version 23.0; IBM Corp) software was used for statistical analysis of the data. Values were expressed as ‾x ± s, and independent samples t test was used for comparison of both groups. Categorical data were compared using the chi-square test (χ2) or Fisher’s exact test. The difference was statistically significant at P < 0.05.
Results
A total of 141 patients underwent laparoscopic radical rectal cancer treatment in our hospital between September 1, 2018, and December 31, 2020. They were randomly divided into the preservation group and the peeled group, and the general clinical data of the 2 groups were compared in Table 1. No significant differences were observed in the baseline characteristics of the groups (P > 0.05).
Intraoperative data outcomes
Preserved group had a shorter No.253 lymph nodes dissection time (15.7 ± 4. 2 min vs. 26.0 ± 3. 6 min, P < 0.001), a shorter operative time (162.1 ± 20. 6 min vs. 174.4 ± 26. 0 min, P = 0.002), and less intraoperative bleeding (39.9 ± 7. 0 ml vs. 44.6 ± 11. 3 ml, P = 0.004) (Table 2) than the peeled group.
Operative time was defined as the time from incision to skin closure. No.253 lymph nodes dissection time was defined as the time between the start of lymph node dissection at No.253 lymph nodes and the end of regional dissection. Operative bleeding was obtained from the perioperative care record sheet.
Pathological outcomes
There was no statistically significant difference between the 2 groups in terms of the number of lymph nodes dissected, the number of No.253 lymph nodes dissected, the number of positive No.253 lymph nodes and number of patients with No.253 lymph nodes involvement (P > 0.05, Table 3).
Postoperative recovery and complications
The preserved group had an earlier time to first flatus (P = 0.013), earlier time to fluid intake (P = 0.033) and shorter hospitalization (P = 0.012). The differences between the 2 groups were not statistically significant (P > 0.05. Table 4) for anastomotic leakage, pneumonia, wound infection, abscess, deep vein thrombosis, ileus, urinary preserved, urinary tract infection and chyle leakage.
Postoperative bleeding was defined as bleeding requiring hemostatic medication or surgical intervention to stop it. Abscess was defined as a postoperative abscess that appeared around the anastomosis or elsewhere in the abdominal cavity. Chyle leakage was defined as a milky white drainage fluid with all positive qualitative tests for chyle and Sudan III staining tests.
Discussion
We cleaned the lymph nodes at the root of the IMA during laparoscopic rectal cancer radical surgery by preserving the IMA sheath and peeling the IMA sheath. The purpose of designing this trial is to compare the outcomes of lymph node dissection and complications of postoperative between the two surgical methods to explore the advantages and disadvantages of the two surgical methods. The study results indicate that peeling the IMA sheath does not significantly increase the number of lymph node dissection in patients, and does not demonstrate a significant advantage in postoperative complications. However, it can increase the time for surgery and anesthesia in patients.
TNM staging (which involves the number of positive lymph nodes) plays an important role in the treatment strategy and prognosis of colorectal cancer, including in peel or laparoscopic surgery or even surgery assisted by the da Vinci robot. Before the appearance of distant metastases, lymph node metastasis is a critical prognostic factor for patients with colorectal cancer and is related to the subsequent treatment plan and course of treatment [18]. Chinese and Japanese scholars have emphasized the importance of lymph node dissection and the importance of dissecting lymph nodes that may have metastases intraoperatively, which has also received increasing attention from Western scholars [19]. In total mesorectal excision, the effectiveness of lymph node dissection is particularly important; therefore, as many lymph nodes as possible need to be dissected to prevent postoperative recurrence.
The lymph nodes at the root of the IMA are classified as third station lymph nodes of the sigmoid colon or rectum. Most scholars think that the area for No.253 lymph nodes dissection is delineated by the IMV on the left, the abdominal aorta on the right, the duodenum on the cephalic side and the area of the angle between the IMA and the LCA on the caudal side [20, 21]. No.253 lymph nodes are located between the beginning of the IMA and the beginning of the LCA. When the mesentery is opened at the level of sacral promontory, the IMA root lymph nodes can be clearly visualized in a high-definition laparoscopic view. Around the IMA root, there is a complex network of lymphatic vessels that run together, draining cephalad to the lumbar lymphatic pools on both sides along the abdominal aorta to the periaortic lymph nodes, and they receive lymphatic drainage from the sigmoid colon and rectum. From the pathway of rectal lymphatic drainage, low rectal cancer patients are at risk of No.253 lymph nodes metastasis; therefore, routine No.253 lymph nodes dissection is recommended for rectal cancer [22, 23].
The surgical approach of this trial was performed in accordance with the standard laparoscopic radical rectal cancer surgery (Dixon procedure) with preservation of the LCA, while the lymph nodes in No.253 lymph nodes were cleared according to the established requirements for the preserved or peeled groups, and the LCA was preserved because previous research has shown that preserving the LCA in radical rectal cancer surgery can increase the blood supply to the proximal IMA of the colon, provide better conditions for the growth and healing of the anastomosis, reduce the incidence of anastomotic leak and anastomotic stenosis postoperatively and is convenient during laparoscopy [24,25,26] .
The influence of heteromorphosis of IMA vascular branches on the surgical approach to peeling the sheath should be noted when dissecting No.253 lymph nodes. For IMA vascular typing, Yada [27] and Shen [28] classified IMA into four types (type I to type IV, Fig. 4) based on the relationship between the LCA, SA and the root of the SRA as follows: in type I ,the LCA branches first, followed by the SA and SRA ; in type II: IMA first divides into one branch, which is the common branch of LCA and SA, SRA is a single branch, and then the common branch is divided into rising LCA and falling SA; in type III, the LCA, SA and SRA branch from the IMA simultaneously at a node; in type IV ,the LCA is absent ,and the IMA divides directly into the SA and SRA. Ke [29] performed a study measuring vascular branches of IMA statistics on 471 patients through vessel reconstruction and found that most patients had type III (n = 209, 44.7%), followed by type I patients (n = 193, 41.2%) and type II patients (n = 42, 9.0%), while type IV patients were the least numerous (n = 24, 5.1%). By understanding the IMA type, clinical surgeons can facilitate the intraoperative search, determination and precise preservation of the LCA and advance the design of the ligature and location of the SA and SRA vessels. Particularly, in patients with LCA deficiency. It is possible to avoid spending more operative time searching for nonexistent LCA in the naked IMA trunk, thus shortening the operative time, reducing the risk of unnecessary injuries and improving the efficiency and safety of the operation.
IMA subtypes: (A) Type I: the LCA branches first, followed by the SA and SRA ; (B) Type II: IMA first divides into one branch, which is the common branch of LCA and SA, SRA is a single branch, and then the common branch is divided into rising LCA and falling SA; (C) Type III: the LCA, SA and SRA branch from the IMA simultaneously at a node; (D) Type IV: the LCA is absent ,and the IMA divides directly into the SA and SRA
The IMA sheath is the tissue that lies between the outer surface of the IMA and the collagen layer that connects the outermost nerve fibers. It contains collagen fibers, nerves, microvasculature, lymphatic vessels and adipose tissue. Studies have shown that microscopically, the IMA sheath contains only lymphatic vessels without the presence of lymph nodes, and no tumor cells are observed within the IMA sheath in lymph node metastasis-positive cases [30, 31]. However, some oriental scholars believe that better lymph node dissection and ensuring the integrity of the resected mesentery are important means to avoid tumor cell omission during surgery. Therefore, in laparoscopic rectal cancer surgery, in order to avoid the tumor cells moving away along the lymphatic vessels in the sheath, and the root of IMA is the key metastasis path for middle and upper rectal cancer, So the dissection of IMA vascular sheath can treat tumor metastasis in this area or prevent the metastasis of rectal cancer to the cephalic side by cutting off the metastasis pathway here [22, 32, 33]. Following the principle of radical tumor resection and choroidal debridement, it is important to debride the extrathecal lymph nodes and intrathecal lymph nodes of the residual sheath as completely as possible.
On the basis of dissection of the IMA sheath. There are currently two types of lymph node dissection for No.253 lymph nodes, and one is to preserve the IMA sheath surgical approach. Li [34] and Gong [17] concluded that depending on the anatomy of the sheath, since there are only lymphatic structures and no lymph nodes in the sheath, stripping the sheath cannot change the lymph node staging of postoperative pathological tissue, nor can it affect the subsequent treatment. Meanwhile, the reported literature mostly comprises retrospective studies on the surgical approach of peeling the arterial sheath for lymph node dissection. Because of the lack of multicenter and large sample size prospective studies, the significance of peeling the sheath for lymph node dissection is unclear and not clearly recommended by relevant guidelines. Additionally, peeling the IMA sheath to dissect No.253 lymph nodes is clearly more difficult in patients who are elderly, obese, have arteriosclerosis or a history of abdominal surgery, and is likely to cause damage to arteries and nerves. The other approach is to operate without preserving the IMA sheath, such as Yan [22] and He [35], who think that the No.253 lymph nodes and the lymphatic vessels within the arterial sheath should be removed together from the consideration of the principle of radical resection in oncological surgery. At the same time, lymph nodes dissection at No. 253 lymph nodes was performed within the sheath, which could serve as a prophylactic dissection for patients without metastases in the sheath and could achieve radical treatment for those with metastases.
In this study, the preserved group had a shorter total operative time than the peeled group. The preservation of the IMA sheath for dissection reduces the operative time, makes the procedure simpler, and reduces the risk of intraoperative anesthetic accidents in patients with a long smoking history, especially those with comorbidities of diabetes, heart disease, kidney or liver problems, which helps to reduce operative risk, improve perioperative safety and improve patient prognosis [36]. The preserved group had less intraoperative bleeding than the peeled group. We can see that the specific difference of bleeding volume is not very large, which may be related to surgical proficiency or the use of ultrasonic scalpel reduces the intraoperative bleeding volume, but there is still a statistical significance between the two groups. We know that less bleeding can better achieve a clear intraoperative visual field, which helps to improve the safety of surgery and reduce the risk of intraoperative side injuries.
The preserved group had significantly shorter times to first flatus and fluid intake than the peeled group. Due to the presence of numerous capillaries and lymphatic vessels within the vascular sheath [37, 38], we think that preservation of the IMA sheath could well preserve the local blood and lymphatic return to the intestine and promote early recovery of intestinal function. Postoperative pathology showed no statistically significant difference in the total number of lymph nodes dissected, the number of No.253 lymph nodes cleared and the positive nodes between the 2 groups, indicating that peeling the IMA sheath to dissect No.253 lymph nodes did not increase the number of all lymph nodes cleared or the positive rate of lymph nodes. Moreover, it is possible that the length of hospitalization was also shorter in the preserved group because patients in the preserved group had shorter times to postoperative flatus and fluid intake.
There were no cases of postoperative mortality or deep vein thrombosis after the operation. Although there were cases of postoperative bleeding in the preserved and peeled group, they were all controlled by appropriate treatment. There were four anastomotic leakage patients in the peeled group (4/70, 5.7%) and only two in the preserved group (2/71, 2.8%). This might be due to the peeling of the sheath affecting the blood flow to the anastomosis, while the influence of the physical condition of the individual patients could not be excluded. Two of the patients with anastomotic leakage were older (both older than 70 years) or had underlying diseases such as hypertension and diabetes. Both groups had three patients with postoperative pneumonia, and all six patients had a long history of smoking. Data from the 2 groups showed no significant difference in the incidences of wound infection and abscess. The number of patients with postoperative ileus is lower than that in the past because surgeons pay more and more attention to the application of enhanced recovery after surgery (ERAS) concept in clinical work. Only two and three patients in both groups developed postoperative ileus; however, the symptoms were quickly alleviated with appropriate and timely treatment. Urinary retention infrequently occurred in both groups, and the data were not significantly different between the 2 groups (5/71, 7.0% vs. 6/70, 8.6% P = 0.735). There was no significant difference in terms of urinary tract infection between the 2 groups. With the use of an ultrasound knife in laparoscopic surgery, the number of patients with chyle leakage in laparoscopic rectal cancer surgery decreased significantly, but there were still cases of celiac disease in the reserved and peeled groups (1/71, 1.4% vs. 2/70, 2.9% P = 0.551). However, in this study, there was no statistically significant difference between the two datasets.
Although this study shows some significant results, there are still some limitations. First, this study is an independent single-center prospective randomized controlled trial, and further validation of the results is needed in a multicenter prospective study with a large sample size. Second, due to limitations in inclusion or exclusion criteria, further data were not available for some patients who had undergone preoperative radiotherapy or emergency cares, and a separate clinical trial could be designed in the future to verify the efficacy of surgery in this population. Finally, in order to reduce the impact of different surgical methods on No.253 of lymph node dissection, the surgical method adopted in this trial was to preserve the LCA for low anterior resection of rectal cancer. Whether the data brought by other surgical methods are similar to this trial needs further prospective trial to verify.
Conclusion
Preserving of the IMA sheath in laparoscopic radical surgery for rectal cancer will reduce the total operation time and the length of hospitalization. This surgical method could lead to lower complication rate and faster recovery.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Change history
18 August 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12893-023-02142-z
Abbreviations
- IMA:
-
Inferior mesenteric artery
- AJCC:
-
American Joint Committee on Cancer
- ASA:
-
American Society of Anesthesiologists
- LCA:
-
Left colic artery
- SA:
-
Sigmoid artery
- SRA:
-
Superior rectal artery
- IMV:
-
Inferior mesenteric vein
- ERAS:
-
Enhanced recovery after surgery
References
Zheng RS, Zhang SW, Zeng HM, Wang SM, Sun KX, Chen R, He J et al. Cancer incidence and mortality in China, 2016, J Natl Cancer Cent, https://doi.org/10.1016/j.jncc.2022.02.002.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022 Jan;72(1):7–33.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories,1980– 2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88.
George AT, Aggarwal S, Dharmavaram S, Menon A, Dube M, Vogler M, et al. Regional variations in UK colorectal cancer screening and mortality. Lancet. 2018 Jul;28(10144):277–8.
Leiphrakpam PD, Rajappa SJ, Krishnan M, Batra R, Murthy SS, Are C. Colorectal cancer: review of signaling pathways and associated therapeutic strategies. J Surg Oncol. 2023;127(8):1277–95.
Ohishi T, Kaneko MK, Yoshida Y, Takashima A, Kato Y, Kawada M. Current targeted therapy for metastatic colorectal Cancer. Int J Mol Sci. 2023;24(2):1702. Published 2023 Jan 15.
Bando H, Ohtsu A, Yoshino T. Therapeutic landscape and future direction of metastatic colorectal cancer. Nat Rev Gastroenterol Hepatol. 2023;20(5):306–22. https://doi.org/10.1038/s41575-022-00736-1.
Yang Z, Wu G, Zhang X, Gao J, Meng C, Liu Y, et al. Current progress and future perspectives of neoadjuvant anti-PD-1/PD-L1 therapy for colorectal cancer. Front Immunol. 2022;13:1001444.
Élez E, Mulet-Margalef N, Sanso M, Ruiz-Pace F, Mancuso FM, Comas R, et al. A Comprehensive Biomarker analysis of microsatellite Unstable/Mismatch repair deficient colorectal Cancer cohort treated with immunotherapy. Int J Mol Sci. 2022;24(1):118.
Diaz LA Jr, Shiu KK, Kim TW, Jensen BV, Jensen LH, Punt C, et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol. 2022;23(5):659–70.
Lam W, Bussom S, Guan F, Jiang Z, Zhang W, Gullen EA, et al. The four-herb chinese medicine PHY906 reduces chemotherapy-induced gastrointestinal toxicity. Sci Transl Med. 2010 Aug;18(45):45ra59.
Juan ME, Wenzel U, Daniel H, Planas JM. Resveratrol induces apoptosis through ROS-dependent mitochondria pathway in HT-29 human colorectal carcinoma cells. J Agric Food Chem. 2008;56(12):4813–8.
Wang Q, Li Z, Guo J, Li W, You F. Effect of chinese herbal medicine formula on progression-free survival among patients with metastatic colorectal cancer: study protocol for a multi-center, double-blinded, randomized, placebo-controlled trial. PLoS ONE. 2022;17(12):e0275058.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016 Mar-Apr;66(2):115–32.
Zhao SD, Zhu LY, Cui YC, Ye YJ, Shen ZL. [Research progress of sexual dysfunction following rectal cancer surgery]. Zhonghua Wei Chang Wai Ke Za Zhi. 2021 Oct;25(10):925–30. Chinese.
Francone E, Bonfante P, Bruno MS, Intersimone D, Falco E, Berti S. Laparoscopic inferior mesenteric artery peeling: an alternative to high or low vascular ligation for sigmoid Colon cancer resection. World J Surg. 2016;40(11):2790–5.
Gong HJ, Han G, Wang DD. Application of intrathecal vascular anatomy in D2 radical gastrectomy for gastric cancer. Chin J Clin Physicians (electronic version). 2013;7(04):1501–4.
Ge W, Li Q, Liu WJ. Carbon nanoparticle suspension could help get a more accurate nodal staging for patient with rectal cancer. Sci Rep. 2021;11(1):9933.
Sluckin TC, Hazen SJA, Kusters M. From “East vs West” towards international multidisciplinary collaboration: an appraisal of lateral lymph nodes in rectal cancer. Ann Gastroenterol Surg. 2021;5(6):731–7.
Li K, Li Z, Yan B, Tan J, Chen D, Chen W, et al. Preoperative Carbon Nanoparticle Injection improves Inferior Mesenteric Artery Lymph Node Retrieval in patients with rectal Cancer. Surgery. 2021;13(21):0039–6060.
Li K, Zeng J, Pang P, Cheng H, He X, Cao F, et al. Significance of nerve plane for Inferior Mesenteric Plexus Preservation in laparoscopic rectal Cancer surgery. Front Oncol. 2022 Apr;22:12:853662.
Yan S, Ma XF, Zhao K, Chen XQ, Guo C, Liu CH. Controversy and consensus on routine No.253 lymph node dissection for low rectal cancer. CHN J of Practical Surg 2020 40(03): 315–22.
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, et al. Japanese Society for Cancer of the Colon and rectum. Japanese Society for Cancer of the Colon and rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020 Jan;25(1):1–42.
Li Z, Xiong H, Qiao T, Jiao S, Zhu Y, Wang G, et al. Long-term oncologic outcomes of natural orifice specimen extraction surgery versus conventional laparoscopic-assisted resection in the treatment of rectal cancer: a propensity-score matching study. BMC Surg. 2022 Jul;25(1):286.
Zheng H, Li F, Xie X, Zhao S, Huang B, Tong W. Preservation versus nonpreservation of the left colic artery in anterior resection for rectal cancer: a propensity score-matched analysis. BMC Surg. 2022 May;10(1):164.
Hiranuma C, Ishiyama Y, Hirano Y, Hattori M, Douden K. D3 lymph node dissection with versus without left colic artery preservation in single-incision laparoscopic surgery for sigmoid and rectosigmoid cancer: a propensity score-matched analysis. Asian J Endosc Surg. 2022 Nov 28.
Yada H, Sawai K, Taniguchi H, Hoshima M, Katoh M, Takahashi T. Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg. 1997 Jan;21(1):109–15.
Shen HY, Liu Z, Mei SW. Clinical anatomy study of the IMA and its branches based on CTA and vascular three-dimensional reconstruction technology. Chin J Colorec Dis (Electronic Edition). 2021;10(03):284–90.
Ke J, Cai J, Wen X, Wu X, He Z, Zou Y, et al. Anatomic variations of inferior mesenteric artery and left colic artery evaluated by 3-dimensional CT angiography: insights into rectal cancer surgery - A retrospective observational study. Int J Surg. 2017 May;41:106–11.
Sakamoto W, Yamada L, Suzuki O, Kikuchi T, Okayama H, Endo H, et al. Microanatomy of inferior mesenteric artery sheath in colorectal cancer surgery. J Anus Rectum Colon. 2019 Oct;30(4):167–74.
Zheng Z, Wang X, Huang Y, Lu X, Zhao X, Chi P. An intrasheath separation technique for nerve-sparing high ligation of the Inferior Mesenteric Artery in Colorectal Cancer surgery. Front Oncol. 2021;11:694059.
Zhang C, Li GX, Ding ZH, Wu T, Zhong SZ. Nan Fang Yi Ke Da Xue Xue Bao. 2006;26(1):49–52.
Zhou H, Ruan C, Sun Y, Zhang J, Wang Z, Hu Z. Nerve-guided laparoscopic total mesorectal excision for distal rectal cancer. Ann Surg Oncol. 2015;22(2):550–1.
Li ZH. Study on the risk and value of using ultrasonic SA for intrathecal lymph node dissection of gastric cancer. Guangzhou University of Chinese Medicine; 2015.
He YL. Relationship between lymph node dissection and vascular sheath in gastric cancer. Surg theory Pract,2005(05):470–2.
Chaturvedi R, Burton BN, Gabriel RA. Complication rates and the benefits of Neuraxial Anesthesia in the patient with High Comorbidity Burden Undergoing Primary Total Joint Arthroplasty. J Arthroplasty. 2020 Nov;35(11):3089–92.
Peng JJ, He YL, Zhan WH, Cai SR, Wu H, Zhang CH. [Effect of advanced gastric cancer on vagniae vasPorum of gastric vessels]. Zhonghua Wei Chang Wai Ke Za Zhi. 2007 Jan;10(1):49–52. Chinese.
Luo Y, Yu MH, Huang YZ, Jing R, Qin J, Qin SL, et al. Lymphadenectomy around Inferior Mesenteric Artery in Low-Tie vs High-Tie Laparoscopic Anterior Resection: short- and long-term outcome of a cohort of 614 rectal cancers. Cancer Manag Res. 2021 May;14:13:3963–71.
Acknowledgements
We thank the patients who participated in this study and their families, investigators, pathology staff and other staff involved in this study.
Funding
This work was supported by the Natural Science Research Project of Higher Education in Anhui Province (KJ2021A0857); National Natural Science Foundation of China (81902515); Excellent Youth Talent Support Program (Key) of Anhui Province(gxyqzd2020029); Young and Middle-aged Scientific Research Project of Wannan Medical College(WK2020F13,WK2020F33);Funding (81902515) was mainly used for data collection and analysis, funding (KJ2021A0857, gxyqzd2020029, WK2020F13,WK2020F33) was mainly used for interpretation of data, writing the manuscript and English editing.
Author information
Authors and Affiliations
Contributions
QL, YW and JW W designed the study, analyzed and interpreted the patient data, prepared all figures and tables and wrote the main manuscript text, LQ, TT C and SW collected, interpreted the patient data. YB X and XX H performed the surgical procedures. L X performed the operations, interpreted the data and drafted the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of The First Affiliated Hospital of Wannan Medical College and registered by the China Clinical Trials Registry (ChiCTR2200060830). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: table 2 and 4 has been updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Q., Wang, Y., Wang, Jw. et al. Preserving or peeling the inferior mesenteric arterial sheath during laparoscopic rectal cancer surgery: a prospective study of surgical outcomes. BMC Surg 23, 176 (2023). https://doi.org/10.1186/s12893-023-02083-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-02083-7