Abstract
Purpose
The rate of postoperative morbidity, including infectious complications, is still high after major hepatobiliary pancreatic (HBP) surgery. Although surgery-related disseminated intravascular coagulation (DIC) occurs in some cases, its significance has not been elucidated in HBP surgery. This study aimed to evaluate the influence of surgery-related DIC on the complication severity after HBP surgery.
Methods
We analyzed the records of 100 patients with hepatectomy in two or more segments, hepatectomy with biliary tract reconstruction, and pancreaticoduodenectomy. The baseline characteristics and complications were compared between patients with and without surgery-related DIC on postoperative day 1 (POD1) after HBP surgery between 2010 and 2018. Complication severity was assessed using the Comprehensive Complication Index (CCI).
Results
The DIC group (surgery-related DIC on POD1) had predictive factors, such as larger bleeding volume and higher liver enzyme levels. The DIC group exhibited significantly elevated rates of surgical site infection, sepsis, prolonged intensive care unit stay, more frequent blood transfusions, and higher CCI. Furthermore, compared with and without adjustment of DIC, odds ratio (OR) of AST level and operation time for the risk of high CCI decreased (OR of AST level: 1.25 to 1.19 and OR of operation time: 1.30 to 1.23) and the significant differences had vanished.
Conclusions
Surgery-related DIC on POD1 could be a partial mediator between AST level, operation time and higher CCI. The prevention or proper management of surgery-related DIC on POD1 can be an important target to reduce the severity of postoperative complications.
Similar content being viewed by others
Introduction
Major hepatobiliary pancreatic (HBP) surgery is known to be associated with a high risk of postoperative complications. Although the mortality rate is low, the morbidity rates still range from 40–75% [1,2,3,4,5]. Hence, surgeons should anticipate high rates of morbidity and control the associated risks to prevent complications.
Disseminated intravascular coagulation (DIC) occurs in various clinical conditions, including sepsis, trauma, cancer, and immunological disorders [6]. Guidelines for the diagnosis and treatment of DIC were recently published in Britain [6], Japan [7], and Italy [8]. Although surgery-related DIC occasionally occurs after invasive surgery, including hepatobiliary and pancreatic surgery [9], the significance of surgery-related DIC has not yet been determined.
The objective of this study was to evaluate the influence of surgery-related DIC on the severity of complications after major HBP surgery.
Methods
Patients
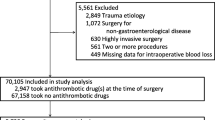
We performed 149 major HBP surgeries in our unit between January 2010 and October 2018, excluding cases that involved liver transplantation and liver donation. We analyzed 100 major HBP surgeries that we could identify as involving surgery-related DIC. Data concerning patient characteristics at the time of surgery (age, gender, primary disease, surgical procedure, body mass index, diabetes, preoperative biliary drainage, cholangitis in medical history), surgical factors (operation time, bleeding volume), levels of total bilirubin (T-bil), aspartate transaminase (AST), alkaline phosphatase (ALP), alkaline transferase (ALT), albumin, Albumin-Bilirubin (ALBI) score [10], international normalized ratio of prothrombin time (PT-INR), white blood cell (WBC), hemoglobin, and platelet, prior to surgery, and short-outcomes were collected from electronic records. This study has been reported in line with the STROCSS criteria [11].
Preoperative biliary drainage
Preoperative biliary decompression was performed to reduce serum bilirubin concentrations for all patients with jaundice and to control segmental cholangitis. A biliary stent, percutaneous transhepatic biliary drainage, or endoscopic nasobiliary drainage was used for drainage. Prophylactic antibiotics were administered for three days postoperatively according to sensitivity results of a preoperative biliary culture test.
HBP surgery
Major HBP surgery was defined to contain pancreaticoduodenectomy (PD), hemihepatectomy or greater, and hepatopancreaticoduodenectomy [12].
The DIC score
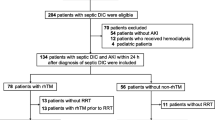
The DIC score established by the Japanese Association for Acute Medicine (JAAM DIC diagnostic criteria) was also assessed on postoperative day 1 (POD1). The scoring system used to diagnose DIC was developed by JAAM in 2006 [13]. The revised scoring system for DIC that is used in Japan is shown in Table 1. Surgery-related DIC on POD1 was diagnosed when (1) the DIC score was 4 points or more on POD1 and (2) the DIC score was 3 points or less before surgery. All patients were followed up for 30 days after enrollment into the study, and the incidence rate of the preoperative complications at 30 days was assessed. All complications were evaluated using the Clavien-Dindo classification [14]. The disease was classified as grade II or higher if complications were present. The Comprehensive Complication Index (CCI) was finally calculated as the sum of all complications that were weighted for their severity by patients and physicians, with the final formula yielding a score that ranged from 0 (no complication) to 100 (death) [15]. Severe morbidity was defined as CCI ≥ 40, as described in a previous report [16].
The CCI can easily be calculated online, with free access at www.assessurgery.com. Follow-up results were obtained from medical records and the primary physician interviews.
Statistical analysis
JMP statistical software (JMP® 14; SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. Data were summarized using median values and interquartile ranges (IQR) for continuous variables, and number and percentage values for categorical variables. The Mann–Whitney U test was used in analyzing all continuous variables and Pearson’s Chi-squared test was used to determine the significance of differences between categorical values. Fisher’s exact test was used when a table included a cell with an expected frequency of < 5. The incidence curves of patients with a high CCI (≥ 40) were compared using the logistic analyses as a univariate analysis. The well-known factors such as operation time, bleeding time and patient age as a risk for the occurrence of postoperative complications were selected in a multivariate analysis. Bleeding volume and operative time were strongly correlated, therefor bleeding volume was excluded. Regarding a liver enzyme such as AST level, AST values were included in the analysis continuous variables due to the strongly correlation with AST values and postoperative complications in univariate analysis. DIC on POD1 was analyzed as a mediator to connect exposures such as surgical invasiveness and preoperative patients’ condition with high CCI, using the causal mediation analysis [17]. To evaluate the influence of surgery-related DIC as a mediate factor of high CCI, multivariate analyses of risk of high CCI with and without adjustment of DIC were performed. A p-value of less than 0.05 was considered statistically significant in all analyses.
Results
Correlation between surgery-related DIC and clinical characteristics
We analyzed the records of 77 men and 23 women with an overall median age at operation of 69.5 years [64–77]. The distribution of patients’ characteristics is shown in Table 2. The underlying diagnosis was hepatocellular carcinoma (HCC) in 42 cases (42%), pancreatic cancer in 8 cases (8%), duodenal cancer in 14 cases (14%), and cholangiocarcinoma in 22 cases (22%). We first divided the patients into two groups according to the presence of surgery-related DIC on POD1 (Table 3). Patients with surgery-related DIC on POD1 (DIC group) had a significantly increased bleeding volume, and higher AST and ALT levels before surgery. However, there were no significant differences in preoperative conditions, including prior cholangitis and biliary drainage.
Clinical outcomes based on surgery-related DIC
Table 4 shows the short-term outcomes based on the conditions of surgery-related DIC on POD1. Patients in the DIC group had significantly higher rates of surgical site infection (SSI), bloodstream infection, stays in an intensive care unit (ICU), red blood cells (RBC) infusion, fresh frozen plasma (FFP) infusion and 30-day morbidity compared with patients in the non-DIC group. Next, we analyzed the influence of surgery-related DIC on POD1 on postoperative complications using the CCI [15]. Patients with higher DIC score tended to increase the CCI, especially among patients more over 4 points of DIC score. (Fig. 1A) Patients with surgery-related DIC on POD1 had a significantly higher CCI than patients who did not develop surgery-related DIC on POD1 (38.5 vs 14.5, p < 0.01). (Fig. 1B).
Risk factors for surgery-related DIC on day 1
We analyzed risk factors for DIC on day 1. Univariable analysis showed that higher AST +10U/L level (OR; 1.24, 95% confidence interval; 1.06–1.45, p < 0.01), operation time+1 h (OR; 1.20, 95% confidence interval; 1.02–1.42, p = 0.02), and bleeding volume+100 ml (OR; 1.05, 95% confidence interval; 1.01–1.09, p = 0.01) had a relation with the risk of surgery-related DIC on day 1. Multivariate analysis revealed that the independent risk factors of surgery-related DIC were higher AST +10 U/L level (OR; 1.23, 95% confidence interval; 1.05–1.45, p < 0.01), and operation time+1h (OR; 1.22, 95% confidence interval; 1.02–1.46, p = 0.02), (Table 4).
Risk factors for high CCI without and with adjustment of surgery-related DIC on day 1
We analyzed risk factors for severe morbidity via univariate and multivariate analysis. Univariate analysis revealed that surgery-related DIC on POD1 had strong relation for severe morbidities (OR; 9.86, 95% confidence interval; 3.23–30.07, p < 0.01). Univariate analysis even after adjustment with age revealed that surgery-related DIC on POD1 had strong relation for severe morbidities (OR; 9.81, 95% confidence interval; 3.20–30.09, p < 0.01). Multivariate analysis without adjustment of surgery-related DIC on day 1 revealed that higher AST +10 U/L level (OR; 1.25, 95% confidence interval; 1.06–1.47, p < 0.01), and operation time+1 h (OR; 1.30, 95% confidence interval; 1.07–1.59, p < 0.01) had a strong relation with the risk of high CCI (Table 6). Multivariate analysis with adjustment of surgery-related DIC on day 1 also revealed that higher AST +10 U/L level (OR; 1.19, 95% confidence interval; 0.99–1.43, p = 0.06), operation time+1 h (OR; 1.23, 95% confidence interval; 0.99.-1.53, p = 0.06), DIC on POD1 (OR; 6.12, 95% confidence interval; 1.82–20.47, p < 0.01) had a relation with the risk of high CCI (Table 6).
Discussion
This study enrolled 100 major HBP surgeries to evaluate the impact of surgery-related DIC on the severity of complications using the causal mediation analysis. These results indicated that DIC could be detected as a partial mediator between higher AST level, prolonged operation time and higher CCI. Surgery-related DIC on POD1 was also significantly associated with surgical site infection, bloodstream infection, longer stays in an ICU, high CCI, and morbidity within 30 days. Our report will help to spread the awareness of surgery-related DIC and stimulate discussion of therapeutic interventions for surgery-related DIC such as the anticoagulant therapy.
The risk factors for surgery-related DIC were higher preoperative liver enzyme levels (OR; 1.23, 95% confidence interval; 1.05–1.45, p < 0.01), and longer operation time (OR; 1.22, 95% confidence interval; 1.02–1.46, p = 0.02). (Table. 4) This result showed that surgery-related DIC was strongly related to preoperative liver function and invasive surgery. Several indexes combined with preoperative liver enzymes such as the AST-to-platelet ratio index and AST-to-neutrophil ratio index have been shown to be useful as predictors of postoperative outcomes after hepatectomy [18,19,20]. Invasive surgery, such as intraoperative and postoperative bleeding and longer operation time was also well-established risk factors for high morbidity and poor survival among patients with colorectal liver metastases and hepatocellular carcinoma [21,22,23,24,25]. ALBI score was well-known as a predictive factor of posthepatectomy liver failure and poor outcomes [26, 27]. In our study, ALBI score had no relation with surgery-related DIC and high CCI. These reports supported that our finding that surgery-related DIC was strongly related to preoperative liver damage and invasive surgery.
Our findings also showed that surgery-related DIC on POD1 reflects the degree of invasion in patients that undergo major HBP surgery. We hypothesized that invasive procedures could cause clotting abnormality and that postoperative complications could be increased by delaying blood supply to organs after major HBP surgery. DIC is recognized as a severe condition involving the widespread activation of coagulation, which leads to blood clots and can decrease blood supply to organs [28]. The cardiovascular surgery-associated DIC was discussed in previous report [29]. However, surgery-related DIC is not still prevalent in the field of gastrointestinal surgery [30], and it is challenging to treat surgery-related DIC in Japan because of the risk of postoperative bleeding. However, only a few studies have reported that recombinant soluble thrombomodulin improved surgery-related DIC [30, 31]. Hashimoto et al. reviewed that anticoagulant therapy may be effective and safe in DIC after gastrointestinal surgery [32, 33]. The DIC score ≥ 5 postoperatively was reported as an independent risk factor for post-hepatectomy liver failure [34]. Surgery-related DIC may result in systemic inflammation and infection after invasive gastroenterological surgery. In addition, blood coagulation and fibrinolysis result in systemic thrombin and plasmin activation in vessels in DIC patients [35]. Therefore, we focused on the relationship between surgery-related DIC on POD1 and postoperative complications. It needs to be further discussed that a high DIC score on POD1 should have included decrease in PT and platelet number levels due to hepatectomy and does not reflect DIC status after operation completely. However, Table 4 showed that the DIC group had a high rate of using perioperative FFP and RBC infusions to improve coagulopathy, suggesting that surgeons carefully monitored coagulopathy postoperatively in the clinical setting. To evaluate the influence of surgery-related DIC, which is as a mediate factor, on high CCI clearly, DIC on POD1 wea analyzed as a mediator to connect exposures such as surgical invasiveness and preoperative patients’ condition with high CCI, using the causal mediation analysis [17].Table .6 shows that DIC had a strong relation with high CCI. (OR:9.86) Higher AST level and operation time had a relation with surgery-related DIC and high CCI in Tables 5 and 6. Compared with and without adjustment of surgery-related DIC, OR of AST level and operation time decreased (OR of AST level: 1.25 to 1.19 and OR of operation time: 1.30 to 1.23) and the significant differences had disappeared. These results indicated that DIC could be a partial mediator between AST level, operation time and high CCI.
In 2013, the CCI was developed and has been reported as an accurate index that reflects the severity of all postoperative complications [15]. The CCI summarizes the postoperative experience with respect to the development of complications using the Clavien-Dindo classification system [36]. Nakanishi et al. reported that massive intraoperative blood loss and combined PD were independent risk factors for CCI ≧ 40 among patients that underwent major hepatectomy for biliary cancer [16]. In this study, surgery-related DIC on POD1 led to an increase in several severe complications and an elevated CCI. Generally, DIC should be treated promptly to resolve the pathological conditions associated with DIC [37, 38]. Optimized surgical decisions are needed to minimize the risk of massive blood loss and a longer operation time [16]. Additionally, a reduction in surgical invasiveness and treatment of surgery-related DIC could prevent development of high CCI conditions in patients after major HBP surgery.
Although this study presents the risk factors for severe complications among major HBP surgery, it is limited by its small sample size, short period of observation, and single-center design. In addition, many unknown issues involving surgery-related DIC on POD1, including the relationships between DIC and complications, remain undetermined. Larger cohorts, including multi-institutional joint research, are necessary to investigate the relationship between surgery-related DIC on POD1 and the severity of complications after major HBP surgery and add sub-analyses separated in hepatectomy and pancreatectomy. The results in this study can provide a good opportunity to focus on surgery-related DIC for many surgeons.
Conclusions
Surgery-related DIC on POD1 could be a partial mediator between AST level, operation time and higher CCI. The prevention or proper management of surgery-related DIC on POD1 can be an important target to reduce the severity of postoperative complications.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to institutional policies but are available from the corresponding author on reasonable request.
Change history
24 June 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12893-023-02073-9
Abbreviations
- HBP:
-
Major hepatobiliary pancreatic
- DIC:
-
Disseminated intravascular coagulation
- T-bil:
-
Total bilirubin
- AST:
-
Aspartate transaminase
- ALBI score:
-
Albumin-Bilirubin score
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alkaline transferase
- PT-INR:
-
International normalized ratio of prothrombin time
- WBC:
-
White blood cell
- PD:
-
Pancreaticoduodenectomy
- JAAM:
-
The Japanese Association for Acute Medicine
- CCI:
-
Comprehensive Complication Index
- HCC:
-
Hepatocellular carcinoma
- RBC:
-
Red blood cells
- FFP:
-
Fresh frozen plasma
References
Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 2013;258(1):129–40.
Sano T, Shimada K, Sakamoto Y, Yamamoto J, Yamasaki S, Kosuge T. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg. 2006;244(2):240–7.
Malgras B, Duron S, Gaujoux S, Dokmak S, Aussilhou B, Rebours V, Palazzo M, Belghiti J, Sauvanet A. Early biliary complications following pancreaticoduodenectomy: prevalence and risk factors. HPB (Oxford). 2016;18(4):367–74.
Loehrer AP, House MG, Nakeeb A, Kilbane EM, Pitt HA. Cholangiocarcinoma: are North American surgical outcomes optimal? J Am Coll Surg. 2013;216(2):192–200.
Aoki S, Miyata H, Konno H, Gotoh M, Motoi F, Kumamaru H, Wakabayashi G, Kakeji Y, Mori M, Seto Y, et al. Risk factors of serious postoperative complications after pancreaticoduodenectomy and risk calculators for predicting postoperative complications: a nationwide study of 17,564 patients in Japan. J Hepatobiliary Pancreat Sci. 2017;24:243–51.
Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145(1):24–33.
Wada H, Asakura H, Okamoto K, Iba T, Uchiyama T, Kawasugi K, Koga S, Mayumi T, Koike K, Gando S, et al. Expert consensus for the treatment of disseminated intravascular coagulation in Japan. Thromb Res. 2010;125(1):6–11.
Di Nisio M, Baudo F, Cosmi B, D’Angelo A, De Gasperi A, Malato A, Schiavoni M, Squizzato A. Italian Society for T, Haemostasis: Diagnosis and treatment of disseminated intravascular coagulation: guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thromb Res. 2012;129(5):e177-184.
Tsuzuki T, Toyama K, Nakayasu K, Iida S, Ueda M, Toizumi A. Disseminated intravascular coagulation after hepatic resection. Surgery. 1990;107(2):172–6.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O’Beirne J, Fox R, Skowronska A, Palmer D, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–8.
Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP, Group S. The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int J Surg. 2017;46:198–202.
Hayashi H, Morikawa T, Yoshida H, Motoi F, Okada T, Nakagawa K, Mizuma M, Naitoh T, Katayose Y, Unno M. Safety of postoperative thromboprophylaxis after major hepatobiliary-pancreatic surgery in Japanese patients. Surg Today. 2014;44(9):1660–8.
Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, Mayumi T, Murata A, Ikeda T, Ishikura H, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006;34(3):625–31.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258(1):1–7.
Nakanishi Y, Tsuchikawa T, Okamura K, Nakamura T, Tamoto E, Noji T, Asano T, Amano T, Shichinohe T, Hirano S. Risk factors for a high comprehensive complication index score after major hepatectomy for biliary cancer: a study of 229 patients at a single institution. HPB (Oxford). 2016;18(9):735–41.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82.
Matsumoto M, Wakiyama S, Shiba H, Haruki K, Futagawa Y, Ishida Y, Misawa T, Yanaga K. Usefulness of aspartate aminotransferase to platelet ratio index as a prognostic factor following hepatic resection for hepatocellular carcinoma. Mol Clin Oncol. 2018;9(4):369–76.
Cheng J, Zhao P, Liu J, Liu X, Wu X. Preoperative aspartate aminotransferase-to-platelet ratio index (APRI) is a predictor on postoperative outcomes of hepatocellular carcinoma. Medicine (Baltimore). 2016;95(48):e5486.
Ji F, Fu S, Guo Z, Pang H, Chen D, Wang X, Ju W, Wang D, He X, Hua Y, et al. Prognostic significance of preoperative aspartate aminotransferase to neutrophil ratio index in patients with hepatocellular carcinoma after hepatic resection. Oncotarget. 2016;7(44):72276–89.
Dionigi G, Boni L, Rovera F, Rausei S, Cuffari S, Cantone G, Bacuzzi A, Dionigi R. Effect of perioperative blood transfusion on clinical outcomes in hepatic surgery for cancer. World J Gastroenterol: WJG. 2009;15(32):3976–83.
Shiba H, Ishida Y, Wakiyama S, Iida T, Matsumoto M, Sakamoto T, Ito R, Gocho T, Furukawa K, Fujiwara Y, et al. Negative impact of blood transfusion on recurrence and prognosis of hepatocellular carcinoma after hepatic resection. J Gastrointest Surg. 2009;13(9):1636–42.
Makino Y, Yamanoi A, Kimoto T, El-Assal ON, Kohno H, Nagasue N. The influence of perioperative blood transfusion on intrahepatic recurrence after curative resection of hepatocellular carcinoma. Am J Gastroenterol. 2000;95(5):1294–300.
de Boer MT, Molenaar IQ, Porte RJ. Impact of blood loss on outcome after liver resection. Dig Surg. 2007;24(4):259–64.
Okamura Y, Takeda S, Fujii T, Sugimoto H, Nomoto S, Nakao A. Prognostic significance of postoperative complications after hepatectomy for hepatocellular carcinoma. J Surg Oncol. 2011;104(7):814–21.
Honmyo N, Kobayashi T, Hamaoka M, Kohashi T, Abe T, Oishi K, Tazawa H, Imaoka Y, Akita T, Tanaka J, et al. Comparison of new prognostic systems for patients with resectable hepatocellular carcinoma: albumin-bilirubin grade and albumin-indocyanine green evaluation grade. Hepatol Res. 2019;49(10):1218–26.
Honmyo N, Kobayashi T, Kuroda S, Oshita A, Onoe T, Kohashi T, Fukuda S, Ohmori I, Abe T, Imaoka Y, et al. A novel model for predicting posthepatectomy liver failure based on liver function and degree of liver resection in patients with hepatocellular carcinoma. HPB (Oxford). 2021;23(1):134–43.
Levi M, Ten Cate H. Disseminated intravascular coagulation. N Engl J Med. 1999;341(8):586–92.
Yasuda N, Goto K, Kuribayashi Y, Ohchi Y, Kitano T. Incidence, outcome, and risk factors of cardiovascular surgery-associated disseminated intravascular coagulation: a single-center retrospective study. J Clin Med. 2022;11(13):3633.
Hashimoto D, Chikamoto A, Miyanari N, Ohara C, Kuramoto M, Horino K, Ohshima H, Baba H. Recombinant soluble thrombomodulin for postoperative disseminated intravascular coagulation. J Surg Res. 2015;197(2):405–11.
Konishi H, Okamoto K, Shoda K, Arita T, Kosuga T, Morimura R, Komatsu S, Murayama Y, Shiozaki A, Kuriu Y, et al. Early thrombomodulin-alpha administration outcome for acute disseminated intravascular coagulopathy in gastrointestinal surgery. World J Gastroenterol: WJG. 2017;23(5):891–8.
Hashimoto D, Okawa T, Maruyama R, Matsumura F, Shibata Y, Kohrogi H. Anticoagulant therapy for disseminated intravascular coagulation after gastrointestinal surgery. Anticancer Res. 2019;39(1):25–31.
Yamaguchi T, Kitajima Y, Miyauchi Y, Izawa K, Tanaka M, Hirata M, Sadatsuki Y, Ogawa Y. Assessment of bleeding in patients with disseminated intravascular coagulation after receiving surgery and recombinant human soluble thrombomodulin: a cohort study using a database. PLoS ONE. 2018;13(10):e0205146.
Kuroda S, Kobayashi T, Tashiro H, Onoe T, Oshita A, Abe T, Kohashi T, Oishi K, Ohmori I, Imaoka Y, et al. A multicenter randomized controlled trial comparing administration of antithrombin III after liver resection (HiSCO-05 trial). Surgery. 2021;170:1140–50.
Wada H. Disseminated intravascular coagulation. Clin Chim Acta. 2004;344(1–2):13–21.
de la Plaza LR, Ramia Angel JM, Bellon JM, Arteaga Peralta V, Garcia Amador C, Lopez Marcano AJ, Medina Velasco AA, Gonzalez Sierra B, Manuel Vazquez A. Clinical validation of the comprehensive complication index as a measure of postoperative morbidity at a surgical department: a prospective study. Ann Surg. 2018;268(5):838–44.
Suetani K, Okuse C, Nakahara K, Michikawa Y, Noguchi Y, Suzuki M, Morita R, Sato N, Kato M, Itoh F. Thrombomodulin in the management of acute cholangitis-induced disseminated intravascular coagulation. World J Gastroenterol: WJG. 2015;21(2):533–40.
Ito T, Nagahara A, Osada T, Kato J, Ueyama H, Saito H, Taniki N, Kanazawa R, Shimizu R, Sai J, et al. Efficacy of recombinant human soluble thrombomodulin in patients with sepsis and disseminated intravascular coagulation in the gastroenterology field. Biomedical reports. 2015;3(4):457–60.
Acknowledgements
We thank Editage (www.editage.jp) for the English language review.
Funding
This work was supported in part by JSPS KAKENHI Grant Numbers JP20K09104, 22K16534, 22K16535, 23H02981 and AMED under Grant Number 22fk0210108. The funders had no role in the study design, data collection, and analysis. They did not participate in the preparation of the manuscript or the decision to publish.
Author information
Authors and Affiliations
Contributions
Yuki Imaoka and Masahiro Ohira performed the investigation, analyzed the data, and wrote the manuscript. Kouki Imaoka, Tomoaki Bekki, Ryosuke Nakano, Shintaro Kuroda, Hiroyuki Tahara, Kentaro Ide, Tsuyoshi Kobayashi and Yuka Tanaka performed the investigation and analyzed the data. Hideki Ohdan designed the study. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of Hiroshima University Hospital (E-1321, E-1580). The study conforms to the provisions of the Declaration of Helsinki. The need for written informed consent was waived owing to the retrospective nature of the study by the ethics committee of Hiroshima University Hospital. The opt-out method to obtain patient consent was utilized.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: figure 1 has been updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Imaoka, Y., Ohira, M., Imaoka, K. et al. Surgery-related disseminated intravascular coagulation predicts postoperative complications. BMC Surg 23, 86 (2023). https://doi.org/10.1186/s12893-023-01986-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-01986-9