Abstract
Background
Postoperative pancreatic fistula (POPF) is a major complication of pancreatic surgery. Drain fluid amylase concentration (DAC) is considered a predictive indicator of POPF. However, other indicators related to postoperative drain fluid amylase status exist, and the most reliable indicator for predicting POPF remains unclear. The object of this study is to identify the single most accurate indicator related to drain fluid amylase status of POPF after distal pancreatectomy (DP).
Methods
This single-institution retrospective study included 122 patients who underwent DP. The study was conducted between 2010 and 2022 at Gifu University Hospital. We statistically analyzed DAC, drain fluid amylase amount (DAA) calculated by multiplying DAC and daily drainage volume, and drain and serum amylase concentration ratio (DSACR) to assess the correlation with POPF.
Results
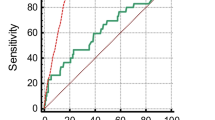
Based on the definition and grading of the International Study Group of Pancreatic Fistula, 24.6 (%) of the 122 patients had Grades B and C POPF. The result of the receiver operating characteristic (ROC) curve for predicting POPF after DP, DSACR had the highest area under curve(AUC) value among DAC, DAA, and DSACR both POD1 and POD3. The cutoff value of DSACR on POD1 was 17 (AUC 0.69, sensitivity 80.0%, specificity 58.2%, and accuracy 63.6%). The cutoff value of DSACR on POD3 was 22 (AUC 0.77, sensitivity 77.7%, specificity 73.3%, and accuracy 73.6%). Overall, DSACR on POD3 had the highest AUC value. Furthermore, a multivariate logistic regression analysis revealed that pancreatic texture (soft; odds ratio [OR] 9.22; 95% confidence interval [CI] 2.22–44.19; p < 0.01) and DSACR on POD3 (> 22; OR 8.76; 95% CI 2.78–31.59; p < 0.001) were independently associated with POPF after DP.
Conclusions
DSACR is the most reliable indicator of drain fluid amylase status for predicting POPF after DP.
Similar content being viewed by others
Background
Postoperative pancreatic fistula (POPF) is a major complication of pancreatic surgery. POPF causes secondary complications, such as abdominal abscess, delayed gastric emptying, and postoperative bleeding, and may result in a prolonged hospital stay and surgery-related death [1,2,3]. Although surgical procedures have been standardized and surgical devices have been developed in pancreatic surgery, the incidence of POPF has been reported to range from 3–50%, even at high-volume centers [4,5,6,7]. When limited to distal pancreatectomy (DP) cases, POPF still occurs at a rate of 24–39% [8,9,10,11,12,13].
Many studies have demonstrated the risk factors of POPF, such as pancreatic texture, body mass index (BMI), intraoperative blood loss, and postoperative drain fluid amylase concentration (DAC) [14,15,16,17,18,19,20,21,22,23,24,25,26]. Additionally, we have reported that DAC on postoperative day (POD) 3 after pancreatectomy can be a reliable indicator for predicting the development of POPF [27, 28]. However, there are other indicators related to the drain fluid amylase status such as daily drainage volume, drain fluid amylase amount (DAA), and drain fluid and serum amylase concentration ratio (DSACR). Few studies have compared these indicators [26, 29, 30]; therefore, the most reliable indicator for predicting POPF remains unclear. The object of this study is to identify the single most accurate indicator related to drain fluid amylase status of POPF after DP.
Methods
Patient
This retrospective study included 140 patients who underwent DP for pancreatic disease at department of gastroenterological surgery in Gifu University Hospital between January 2010 and October 2022. All procedures were conducted by expert surgeons who had qualified through the board certification system of the Japanese Society of Hepato-Biliary-Pancreatic Surgery (JSHBPS). We excluded 18 patients (simultaneous resection of other organs); therefore, 122 patients were included in this study (Fig. 1). The study was conducted in accordance with the World Medical Association Declaration of Helsinki, and the Ethics Committee of Gifu University approved the study (approval number: 2022–157) [28].
Perioperative management
In cases of DP for PDAC, regional lymph node dissection with splenectomy following the classification of pancreatic carcinoma by the Japan Pancreas Society [31] and pancreatic resection of the portal vein were performed. In the case of DP for non-PDAC, systematic lymph node dissection was omitted, and pancreatic resection was performed with a sufficient margin from the tumor using hand-sewn closure or a linear stapler.
In the hand-sewn closure group, the pancreas was resected after identifying the main pancreatic duct, which was ligated with a 3–0 silk suture. The stump of the remnant pancreas was closed with vertical mattress sutures using 5–0 polypropylene. In the linear stapler group, the pancreas was transected with a purple or black cartridge using the Endo GIA™ Tri-Staple or Signia™ stapling system (Medtronic plc., Dublin, Ireland). The closed jaw was clamped carefully and slowly for 5 min at a fixed speed. Firing was performed at a rate of 1 cm/min by firmly fixing the stapler. After firing, the jaws of the stapler were closed for 1 min. One 19-Fr. Blake silicon drain (Johnson & Johnson, Inc. New Brunswick, NJ, USA) was placed near the stump of the remnant pancreas. The drain was removed on POD4–5, when the drainage fluid was clear, postoperative course was stable, the patient had no abdominal pain, fever, or other symptoms, and no fluid collection in pancreatic stump on ultrasonography (US) or computed tomography (CT). The DAC and drainage volumes were measured from POD1 until the drain was removed. All patients received prophylactic antibiotics (cefmetazole) either intraoperatively or two days postoperatively.
Definition of DAA and DSACR
DAA on POD1 was calculated by multiplying the DAC on POD1 and the 24-h drainage volume from the morning of POD1. DAA on POD3 was calculated in the same manner.
DSACR on POD1 was calculated by dividing the DAC on POD1 by serum amylase concentration (SAC) on POD1. DSACR on POD3 was calculated in the same manner.
Definition of POPF
In this study, we included only clinically relevant POPF. Therefore, only Grades B and C pancreatic fistulas were defined as POPF (Grade B, symptomatic fistula requiring therapeutic intervention, such as antibiotics, drain placement for over 3 weeks, and percutaneous drainage; Grade C, symptomatic fistula associated with a severe general condition of patients, sepsis, and multi-organ failure requiring aggressive treatment in the intensive care unit with surgical intervention) based on the International Study Group of Pancreatic Fistula (ISGPF) definitions [32]. The day of POPF diagnosis was defined as intra-abdominal fluid collection with positive cultures identified by US or CT.
Statistical analysis
Continuous and categorical variables are presented as median (range) values and frequencies (percentages), respectively. Fisher’s exact test was used for comparisons of variables between the POPF and non-POPF groups and for categorical variables. The Mann–Whitney U test was used in independent cases for comparisons of variables between groups, and the Wilcoxon signed-rank test was used in paired cases for continuous variables. The predictive ability of POPF after DP was assessed by calculating the area under the receiver operating characteristic (ROC) curve. Youden's index was used to determine the optimal cutoff value to calculate specificities and sensitivities in the ROC curve analysis. Variables identified as potentially significant by univariate analysis were selected for multivariate analysis using a logistic regression model to identify the independent predictors of POPF after DP. The limit of statistical significance for all analyses was defined as a two-sided p-value < 0.05. All statistical analyses were performed using JMP software (SAS Institute Inc., Cary, NC, USA).
Results
Comparison of patient characteristics and surgical outcomes between patients with and without POPF
Table 1 summarizes the characteristics of patients with and without POPF. POPF occurred in 30 (24.6%) patients. Among patients with POPF, Grade C POPF occurred in two patients (6.7%), and the remaining 28 patients (93.3%) had Grade B POPF. Age, sex, BMI, preoperative serum albumin level, history of diabetes mellitus, pancreatic disease, and tumor location did not significantly differ between the two groups.
Table 2 shows the surgical outcomes of the two groups. No significant differences existed between the two groups in operative time, intraoperative blood loss, surgical procedures (open or laparoscopic surgery/spleen preservation or not), pancreatic stump closure method, and pancreatic thickness. A significant difference existed in the soft pancreatic texture rate (85.7% in the POPF group vs. 46.8% in the non-POPF group, p < 0.001). DAC, DAA, and DSACR on both POD1 and 3 were significantly higher in the POPF group than in the non-POPF group. However, postoperative SAC and daily drainage volume were not significantly different between the two groups.
Relationship between changes in DAC, DAA, and DSACR with and without POPF
Both DAC and DAA significantly decreased from POD1 to 3, regardless of the presence or absence of POPF (all p < 0.001) (Fig. 2a and b). The DSACR also showed a significant decrease from POD1 to 3 in the non-POPF group (p = 0.02). Notably, no significant change was observed in DSACR in the POPF group (p = 0.20) (Fig. 2c).
Relationship between changes in DAC, DAA, and DSACR with and without POPF. The Wilcoxon signed-rank test was conducted for comparisons between the groups. DAC, drain fluid amylase concentration; DAA, drain fluid amylase amount; DSACR, drain fluid and serum amylase concentration ratio; POPF, postoperative pancreatic fistula. *p < 0.05; ***p < 0.001
Cutoff values of DAC, DAA, and DSACR on POD1 and 3 for predicting POPF
Figure 3 and Table 3 show the ROC curves for generating the cutoff values of DAC, DAA, and DSACR on POD 1 and 3. The cutoff value of DAC on POD1 was 7238 (U/L), with an area under the curve (AUC) of 0.65, sensitivity of 56.7%, specificity of 80.2%, and accuracy of 74.4% (Fig. 3a). The cutoff value of DAA on POD1 was 103 (U/day), with an AUC of 0.64, sensitivity of 80.0%, specificity of 46.2%, and accuracy of 54.5% (Fig. 3b). The cutoff value of DSACR on POD1 was 17, with an AUC of 0.69, sensitivity of 80.0%, specificity of 58.2%, and accuracy of 63.6% (Fig. 3c). The cutoff value of DAC on POD3 was 737 (U/L), with an AUC of 0.73, sensitivity of 73.3%, specificity of 65.9%, and accuracy of 67.8% (Fig. 3d). The cutoff value of DAA on POD3 was 31 (U/day), with an AUC of 0.72, sensitivity of 70.0%, specificity of 73.6%, and accuracy of 72.7% (Fig. 3e). The cutoff value of the DSACR on POD3 was 22, with an AUC of 0.77, sensitivity of 77.7%, specificity of 73.3%, and accuracy of 73.6% (Fig. 3f). Generally, the results indicated that the most reliable indicator for predicting POPF after DP was the DSACR on POD3, which had the highest AUC value. Additionally, the AUC of all indicators tended to be higher on POD3 than on POD1.
Uni- and multivariate analysis of prediction for POPF after DP
In the univariate logistic regression analysis, POPF after DP was significantly associated with pancreatic texture, and DSACR on POD1 and POD3 (all p < 0.001).
Multivariate logistic regression analysis revealed that pancreatic texture (soft: odds ratio [OR] 9.22; 95% confidence interval [CI] 2.22–44.19; p < 0.01) and DSACR on POD3 (> 22; OR 8.76; 95% CI 2.78–31.59; p < 0.0001) were independently associated with POPF after DP (Table 4).
Discussion
Notwithstanding the attempts to reduce POPF frequency with the development of surgical techniques and devices, a high incidence of POPF is reported in pancreatic surgery [4,5,6,7,8,9,10,11,12,13].
Many studies have reported various predictive factors for POPF, including patient-related factors (e.g., sex and BMI), pancreas-related factors (e.g., pancreatic texture and thickness), and perioperative-related factors (e.g., stump closure method, intraoperative blood loss, and DAC) [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. Particularly, many studies involved the association between postoperative drain amylase status and POPF [16,17,18,19,20,21,22,23,24,25]. We have reported that DAC on POD3 can significantly predict the development of POPF [27, 28]. However, while DAC is the most widely used drain amylase-related indicator, other indicators, such as DAA and DSACR, exist. The values of the DAA and DSACR consider the daily drainage volume and SAC, respectively, in the DAC. These indicators may be more reliable than DAC. We identified the DSACR on POD3 as the most reliable indicator for predicting POPF after DP.
The incidence of POPF varied significantly in different studies because of the definition of POPF used at each institution. Thus, in 2005, the ISGPF developed a definition and grading of POPF that has been universally accepted and unified [32]. Three basic parameters were considered in defining POPF for ISGPF: 1) amylase content in the drain fluid, 2) daily output volume of the drain fluid, and 3) duration. Finally, amylase content in drain fluid was defined as “greater than three times the serum amylase activity” and the duration was defined as “after postoperative day 3,” that is, “DSACR after POD3 > 3.” However, the daily output volume of the drain fluid was defined as “any measurable volume” and was excluded from the definition of POPF.
Once POPF develops, enzymatic fluid leaks into the abdominal cavity from the pancreatic stump, resulting in an increased amylase content in the drain fluid. Therefore, prior to this study, we hypothesized that DAA is a more reliable predictor than DAC because drainage quantity is being considered. However, the study results revealed that DAA was the least reliable of the three indicators related to drain amylase status as a predictor of POPF after DP. Previous studies have focused on postoperative drainage volume and the total amount of amylase in the drainage fluid [22, 26, 29, 30]; however, the results are not always consistent. Molinari et al. [22] reported no significant difference in drainage volume between patients with and without POPF, similar to our results. Conversely, Fukami et al. [26] reported that the median drainage volumes on POD1 and 3 were significantly lower in the POPF group than in the non-POPF group. This result could be due to the reduced drainage efficiency by the highly turbid drain fluid and the dense adhesion around the pancreatic stump in the POPF group. We suspected that the use of a non-suctioned (gravity) drain in their study, unlike in our study, may have been a reason for the difference in results. However, their conclusion that DAA was inferior to DAC as a predictor of POPF was consistent with our findings. Sakamoto et al. [29] reported an analysis of POPF prediction limited to DP cases, similar to this study. They reported that the DAC value on both POD1 and 3 did not have a significant correlation with POPF, whereas DAA had a significant correlation. Okano et al. [30] investigated the predictive ability of DAA in 54 patients who underwent pancreatectomy, and they reported that neither DAC nor DAA were significant predictors of POPF, whereas the persistence ratio of DAA between POD1 and 3 was significant. Although further investigation is required, it would be difficult to make DAA a universal indicator, as it may be affected by the properties of the drain fluid, type of drain, and condition of the pancreatic stump.
While DAC is undoubtedly an excellent predictor of POPF, it is difficult to set appropriate cutoff values. This is because pancreatic exocrine function varies from case to case, and thus the threshold for predicting POPF is likely to be different in each case. Another reason is that DAC fluctuates significantly over time after surgery. This study showed a significant decrease from POD1 to 3 with and without POPF. Consequently, the cutoff value for predicting POPF in previous studies varied from 1300 to 5000 for POD1 and 737 to 3000 for POD3 [16,17,18,19,20,21,22,23,24,25,26,27,28]. Therefore, it is presumed that the accuracy of DAC would be further improved if it reflects the pancreatic exocrine function of individual cases and is less prone to change with time after surgery. In this study, we observed that only the DSACR showed no significant changes from POD1 to 3 in the POPF group. Furthermore, the cutoff values of DSACR for predicting POPF were only slightly different between POD1 and 3 (optimal cutoff values of DSACR: 17 and 22, respectively), unlike other indicators (DAC: 7238 and 737 U/l, DAA: 103 and 31 U/day, respectively). To the best of our knowledge, few studies have evaluated the usefulness of DSACR for predicting POPF during the postoperative period. Based on the results of this study, we propose that the most reliable predictive indicator for POPF after DP is DSACR on POD3. DSACR may contribute to both improving diagnostic accuracy and resolving difficulties in setting optimal cutoff values.
This study had some limitations. First, it was single-center retrospective study with a small sample size. This sample size may have caused selection bias and multiplicity issues in statistical analysis. This limitation should be considered when evaluating the results of this study. A prospective multicenter study with a larger number of patients is required for more accurate results. Second, technical variations existed in the DP surgical procedure, such as open or laparoscopic, spleen-preserving or non-preserving, pancreas transection methods, and with and without lymph node dissection. This study showed no significant correlation between these surgery-related factors and POPF. It is expedient to unify surgical procedures to calculate more appropriate cutoff values for DSACR.
Conclusions
We discovered DSACR to be the most reliable indicator for predicting POPF by comparing several indicators related to the drain fluid amylase status.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on request.
Abbreviations
- POPF:
-
Postoperative pancreatic fistula
- DP:
-
Distal pancreatectomy
- BMI:
-
Body mass index
- DAC:
-
Drainage fluid amylase concentration
- POD:
-
Postoperative day
- DAA:
-
Drain fluid amylase amount
- DSACR:
-
Drainage fluid and serum amylase concentration ratio
- JSHBPS:
-
Japanese Society of Hepato-Biliary-Pancreatic Surgery
- SAC:
-
Serum amylase concentration
- ISGPF:
-
International Study Group of Pancreatic Fistula
- US:
-
Ultrasonography
- CT:
-
Computed tomography
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Fujino Y. Perioperative management of distal pancreatectomy. World J Gastroenterol. 2015;21:3166–9.
Sell NM, Pucci MJ, Gabale S, Leiby BE, Rosato EL, Winter JM, et al. The influence of transection site on the development of pancreatic fistula in patients undergoing distal pancreatectomy: a review of 294 consecutive cases. Surgery. 2015;157:1080–7.
Glowka TR, von Websky M, Pantelis D, Manekeller S, Standop J, Kalff JC, et al. Risk factors for delayed gastric emptying following distal pancreatectomy. Langenbecks Arch Surg. 2016;401:161–7.
Andrianello S, Marchegiani G, Malleo G, Masini G, Balduzzi A, Paiella S, et al. Pancreaticojejunostomy with externalized stent vs pancreaticogastrostomy with externalized stent for patients with high-risk pancreatic anastomosis: a single-center, phase 3, randomized clinical trial. JAMA Surg. 2020;155:313–21.
Zhang H, Zhu F, Shen M, Tian R, Shi CJ, Wang X, et al. Systematic review and meta-analysis comparing three techniques for pancreatic remnant closure following distal pancreatectomy. Br J Surg. 2015;102:4–15.
Kawai M, Tani M, Terasawa H, Ina S, Hirono S, Nishioka R, et al. Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for 104 consecutive patients. Ann Surg. 2006;244:1–7.
Xiong JJ, Tan CL, Szatmary P, Huang W, Ke NW, Hu WM, et al. Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Br J Surg. 2014;101:1196–208.
Hirano S, Kondo S, Hara T, Ambo Y, Tanaka E, Shichinohe T, et al. Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long-term results. Ann Surg. 2007;246:46–51.
McPhee JT, Hill JS, Whalen GF, Zayaruzny M, Litwin DE, Sullivan ME, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246:246–53.
Sledzianowski JF, Duffas JP, Muscari F, Suc B, Fourtanier F. Risk factors for mortality and intra-abdominal morbidity after distal pancreatectomy. Surgery. 2005;137:180–5.
Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, et al. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg. 2008;143:956–65.
Shimada K, Sakamoto Y, Sano T, Kosuge T. Prognostic factors after distal pancreatectomy with extended lymphadenectomy for invasive pancreatic adenocarcinoma of the body and tail. Surgery. 2006;139:288–95.
Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg. 1999;229:693–8 discussion 698-700.
Gaujoux S, Cortes A, Couvelard A, Noullet S, Clavel L, Rebours V, et al. Fatty pancreas and increased body mass index are risk factors of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2010;148:15–23.
Mathur A, Pitt HA, Marine M, Saxena R, Schmidt CM, Howard TJ, et al. Fatty pancreas: a factor in postoperative pancreatic fistula. Ann Surg. 2007;246:1058–64.
Newhook TE, Vega EA, Vreeland TJ, Prakash L, Dewhurst WL, Bruno ML, et al. Early postoperative drain fluid amylase in risk-stratified patients promotes tailored post-pancreatectomy drain management and potential for accelerated discharge. Surgery. 2020;167:442–7.
Maggino L, Malleo G, Bassi C, Allegrini V, Beane JD, Beckman RM, et al. Identification of an optimal cut-off for drain fluid amylase on postoperative day 1 for predicting clinically relevant fistula after distal pancreatectomy: a multi-institutional analysis and external validation. Ann Surg. 2019;269:337–43.
Giglio MC, Spalding DR, Giakoustidis A, Zarzavadjian Le Bian A, Jiao LR, Habib NA, et al. Meta-analysis of drain amylase content on postoperative day 1 as a predictor of pancreatic fistula following pancreatic resection. Br J Surg. 2016;103:328–36.
Noji T, Nakamura T, Ambo Y, Suzuki O, Nakamura F, Kishida A, et al. Clinically relevant pancreas-related infectious complication after pancreaticoenteral anastomosis could be predicted by the parameters obtained on postoperative day 3. Pancreas. 2012;41:916–21.
Kanda M, Fujii T, Takami H, Suenaga M, Inokawa Y, Yamada S, et al. Novel diagnostics for aggravating pancreatic fistulas at the acute phase after pancreatectomy. World J Gastroenterol. 2014;20:8535–44.
Mintziras I, Maurer E, Kanngiesser V, Bartsch DK. C-reactive protein and drain amylase accurately predict clinically relevant pancreatic fistula after partial pancreaticoduodenectomy. Int J Surg. 2020;76:53–8.
Molinari E, Bassi C, Salvia R, Butturini G, Crippa S, Talamini G, et al. Amylase value in drains after pancreatic resection as predictive factor of postoperative pancreatic fistula: results of a prospective study in 137 patients. Ann Surg. 2007;246:281–7.
Shinchi H, Wada K, Traverso LW. The usefulness of drain data to identify a clinically relevant pancreatic anastomotic leak after pancreaticoduodenectomy? J Gastrointest Surg. 2006;10:490–8.
Ansorge C, Nordin JZ, Lundell L, Strömmer L, Rangelova E, Blomberg J, et al. Diagnostic value of abdominal drainage in individual risk assessment of pancreatic fistula following pancreaticoduodenectomy. Br J Surg. 2014;101:100–8.
Yang J, Huang Q, Wang C. Postoperative drain amylase predicts pancreatic fistula in pancreatic surgery: a systematic review and meta-analysis. Int J Surg. 2015;22:38–45.
Fukami Y, Saito T, Osawa T, Hanazawa T, Kurahashi T, Kurahashi S, et al. Which is the best predictor of clinically relevant pancreatic fistula after pancreatectomy: drain fluid concentration or total amount of amylase? Ann Gastroenterol Surg. 2021;5:844–52.
Fukada M, Murase K, Higashi T, Yokoi R, Tanaka Y, Okumura N, et al. Early predictive factors for postoperative pancreatic fistula after distal pancreatectomy for pancreatic cancer. Cancer Diagn Progn. 2022;2:452–61.
Fukada M, Murase K, Higashi T, Fujibayashi S, Kuno M, Yasufuku I, et al. The pancreas-to-muscle signal intensity ratio on T1-weighted MRI as a predictive biomarker for postoperative pancreatic fistula after distal pancreatectomy: a single-center retrospective study. World J Surg Oncol. 2022;20:250.
Sakamoto K, Ogawa K, Tamura K, Iwata M, Matsui T, Nishi Y, et al. Postoperative elevation of C-reactive protein levels and high drain fluid amylase output are strong predictors of pancreatic fistulas after distal pancreatectomy. J Hepatobil Pancreat Sci. 2021;28:874–82.
Okano K, Kakinoki K, Suto H, Oshima M, Kashiwagi H, Yamamoto N, et al. Persisting ratio of total amylase output in drain fluid can predict postoperative clinical pancreatic fistula. J Hepatobil Pancreat Sci. 2011;18:815–20.
Japan Pancreas Society. Classification of pancreatic carcinoma. 4th ed. Tokyo: Kanehara & Co., Ltd.; 2017.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Hilal MA, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2016;161:584–91.
Acknowledgements
The authors thank the medical staff of the Department of Gastroenterological Surgery at Gifu University Hospital for their participation in this study. We could not have completed this study without diligence and support. We would also like to thank Editage (www.editage.jp) for English language editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Masahiro Fukada conceived the study concept, planned the design as the principal investigator, interpreted the results, and wrote the manuscript draft. Nobuhisa Matsuhashi revised the manuscript draft by adding intellectual content and providing critical advice. Masahiro Fukada, Katsutoshi Murase, Toshiya Higashi, Itaru Yasufuku, Yuta Sato, Jesse Yu Tajima, Sigeru Kiyama, Yoshihiro Tanaka, Naoki Okumura, Takao Takahashi, and Nobihisa Matsuhashi obtained the data, provided critical comments to improve the manuscript, and gave final approval for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was conducted in accordance with the World Medical Association Declaration of Helsinki and approved by the Ethics Committee of Gifu University (approval number '2022–157'). As this was a retrospective study and did not include any potentially identifiable patient data, informed consent was waived by the Ethics Committee of Gifu University. This retrospective study was approved by the Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
TakaoTakahashi received honoraria for lectures from Takeda Pharmaceutical Co. Ltd. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fukada, M., Murase, K., Higashi, T. et al. Drain fluid and serum amylase concentration ratio is the most reliable indicator for predicting postoperative pancreatic fistula after distal pancreatectomy. BMC Surg 23, 87 (2023). https://doi.org/10.1186/s12893-023-01980-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-01980-1