Abstract
Objectives
This study proposes a new surgical alternative for the most common deformity in the ears, the so-called "protruding/prominent ears", which is a condition that affects 5% of the Caucasian population (Goulart et al. in Rev Bras Cir Plast 26:602–607, 2011). This technique comes with the benefits of reduced surgical time, shallow learning curve, and a low revision rate.
Methods
We studied a total of 213 patients with an indication for otoplasty from January 2020 to January 2021. Women made up 65% of the study population, while men made up 35%, with an average age of 21 years, the youngest being 7 years of age. The technique presented here corrects all the deformities that cause protruding ears and can be performed together with other ear surgeries, such as surgical treatment of macrotia and lobuloplasty. All surgeries were performed in an outpatient setting under local anesthesia and sedation.
Results
All surgeries followed a performance-optimized protocol, with an average total surgical time of 45 min for a bilateral approach. Revision surgery was needed in 2% of cases, with the most frequent complaint being asymmetry in the upper third of the ears. The complication rate was approximately 7.5%, with 1 case of hematoma, 1 case of mild infection, 2 cases of altered ear sensitivity, 3 cases of keloid scar formation, 6 cases of asymmetry in the upper third of the ears, and 3 cases of irregularities or spikes in the antihelix cartilage. Patient satisfaction was measured using the McDowell/Wright Objectives and Outcome Index (McDowell in Plast Reconstr Surg 41:17–27).
Conclusion
The proposed performance technique is a viable alternative to optimize the surgical time of otoplasty in an outpatient setting. This technique can be performed together with other corrective ear surgeries, has a shallow learning curve, and has a low revision rate.
Level IV: Evidence obtained from multiple time series with or without the intervention, such as case studies.
Similar content being viewed by others
Introduction
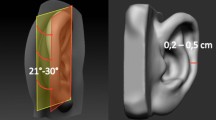
Prominent ears result from changes in the cartilage and are often bilateral. This is usually due to genetic and hereditary factors but can also be caused by the fetal position [1]. Prominent ears should not cause bullying but increased public exposure on social media leads to judgment and psychological and traumatic damage [2, 3]. Prominent ears are one of the main causes of bullying due to their physical appearance [3,4,5]. From Dieffenbach in 1845 to Fritsch in 1992, various corrective ear surgery techniques have been developed [6,7,8,9]. Each technique has advantages and disadvantages, such as the techniques using Mustardé sutures to redesign the antihelix, developed in 1962 [10, 11], and the techniques using Furnas sutures for conchal-scaphal fixation, as described in 1959 [8]. This study presents a new option for the otoplasty technique, with an improved surgical time, low revision and high satisfaction rates. Furthermore, the technique allows designing the antihelix through parallel cartilage islands without the need for fixation points with nonabsorbable threads, which, in some cases, lead to suture extrusions [12]. It also requires no major detachments in the mastoid and fixation with Furnas sutures, which can generate chronic pain or local sensitivity changes [8].
Patients and methods
A total of 213 patients were operated on from January 2020 to January 2021, 136 women and 77 men, all with bilateral intervention, and a mean age of 21 years. Patients were evaluated based on complaints of prominent ears and had an indication for surgery to correct antihelix erasure, conchal hypertrophy or lobe projection, with one or more of these corrections being performed.
The patients were operated on an outpatient basis, without admission to the hospital, and stayed in the hospital for approximately two hours.
All surgeries were performed under local anesthesia using 20 ml saline solution, 5 ml 2% xylocaine, 3 ml 0.5% Marcaine, 0.5 ml adrenaline, and sedation with 0.05 mg/kg midazolam, 2–3 mcg/kg fentanyl, and 10–20 mcg/kg/min propofol. In anxious patients, 1 mcg/kg clonidine was administered, and in children, 0.5–1 mg/kg ketamine was administered if necessary.
Cotton molds soaked in saline solution were applied as dressings in the region of the scapha and auricular concha, as well as cotton pads under the ears, and a 10 cm wide orthopedic tubular mesh was used to stabilize the dressing without going through the neck, which was kept for 5 days (Fig. 1).
Surgical technique
1st Step—marking the ears
The patient is marked while sitting and supine. We performed a bidigital maneuver on the antihelix to check its new projection. A retroauricular skin flap is marked, observing the line projection of the antihelix and the inferior border of the auricular sulcus. Conchal hypertrophy is marked during the perioperative period (Fig. 2).
2nd Step—infiltration with local anesthetic
After sedation, we performed local anesthesia only in the retroauricular flap marked, with associated skin detachment.
3rd Step—surgical procedure
The performance-optimized otoplasty technique consists of three stages of cartilage treatment depending on the needs of each patient and in accordance with the medical indication. We performed 2–3 mm thick, half-moon shaped, parallel chondrotomies on cartilage islands in the antihelix cartilage, following the surgical posterior edge of the ears, with a total depth to the dermis. The objective of this maneuver is to mold the antihelix area into an inverted U-shape, with the first island being the lateral wall, the second, the top; and the third, the medial wall, thus forming a new design by repositioning the upper third of the ears close to the head (Fig. 3).
4th Step—conchal cartilage treatment
After anesthetic reinforcement in the greater auricular nerve and anterior infiltration of the concha for skin detachment, we performed an incision in the conchal cartilage flap to remove its juxta-perichondrial excess (Fig. 4).
5th Ste—treatment of the helix
When a patient shows an anterior projection of the earlobe, we break the cartilage spring at the antihelix–helix junction, and when indicated, remove the posterior skin excess on the fishtail or combine it with lobuloplasty (Fig. 5).
6th Step—skin closure
After properly reviewing hemostasis, we performed a reinforcement stitch in the upper third of the posterior region of the ears, 1.5 cm from the open upper margin, between the area above the chondrotomies and the mastoid, with a 4.0 monocryl suture. This procedure had the purpose of reducing the recurrence of spikes in the upper third, which is the main cause of asymmetry, and stabilization of cartilage islands on the antihelix. The closure is performed with monocryl 4.0 suture in continuous intradermal suture (Fig. 6).
7th Step—cotton mold and bandage helmet
The standard dressing was kept for 5 days, and then the patient was instructed to wear a ballet-style compression bandage only at night to sleep for a minimum period of 30 days. The following are some of the outcomes of this technique (Figs. 7, 8, 9, 10, 11, 12).
Consent
Informed consent was obtained from all individual participants and parents/legal guardians in case of minor participants included in the study.
Patient consent
Patients signed informed consent regarding publishing their data and photographs. The participant has consented to the submission of the case reports to the journal.
Outcomes
The performance-optimized otoplasty technique proved to be efficient in reducing the surgical time to less than 45 min (total bilateral treatment time) compared to the average time of conventional techniques, which is approximately 95 min [12, 13]. It also allowed us to perform all surgeries under local anesthesia and sedation in an outpatient setting, with a hospital stay of approximately 2 h and 15 min. Furthermore, we did not use non-absorbable sutures in the cartilage, which in some cases can cause extrusions, infections, or chronic pain [9].
The new design of the antihelix cartilage resulted in a harmonious shape, without the appearance of operated ears in 98.6% of cases.
Table 1 shows the adherence criteria adopted in the study during the 1-year period.
To analyze the satisfaction of the 213 patients studied, we used the criteria based on objectives and satisfaction with results described by McDowell/Wright [15], as shown in Table 2.
Conclusion
The patients in this study demonstrated satisfaction with the results obtained by the otoplasty technique presented, with quick recovery and return to their daily activities, making this a viable alternative for performing surgeries in an outpatient setting, with low operating costs.
Availability of data and materials
Data sets are available by friendly request to the corresponding author.
References
Thorne CHMD, Wilkes GMD. Ear deformities, otoplasty, and ear reconstruction. Plast Reconstr Surg. 2012;129(4):701e–16e. https://doi.org/10.1097/PRS.0b013e3182450d9f.
García-Purriños F, Raposo A, Guilllén A, Calero J, Giribet A, Barrios A. Otoplasty using the combined Mustardé-Furnas technique: satisfaction and objective results. Aesthet Surg J. 2019;39(10):NP411–5. https://doi.org/10.1093/asj/sjz167.
Boroditsky ML, Van Slyke AC, Arneja JS. Outcomes and complications of the Mustardé otoplasty: a “good-fast-cheap” technique for the prominent ear deformity. Plast Reconstr Surg Glob Open. 2020;8(9): e3103. https://doi.org/10.1097/gox.0000000000003103.
Lee Y, Kim YS, Lee WJ, Rha DK, Kim J. Proposal of a classification system for the assessment and treatment of prominent ear deformity. Aesthet Plast Surg. 2018;42(3):759–65. https://doi.org/10.1007/s00266-017-1061-2.
Steven S, Kent HB. Decoding the DNA of the Toyota production system. Harv Bus Rev. 1999;77:97–107.
Furnas DW. Correction of prominent ears by conchamastoid sutures. Plast Reconstr Surg. 1968;42(3):189–93. https://doi.org/10.1097/00006534-196809000-00001.
Peter A, Becky L, Guy J. Otoplasty: critical review of clinical results. The Laryngoscope.
Smittenberg MN, Marsman M, Veeger NJGM, Moues CM. Comparison of cartilage-scoring and cartilage-sparing otoplasty: a retrospective analysis of complications and aesthetic outcome of 1060 ears. Plast Reconstr Surg. 2018;141(4):500e–506. https://doi.org/10.1097/PRS.0000000000004241.
Benoit IMM, Hendrickx MH, Assaf Z, Andrew G. The ‘WiFi’ otoplasty: combined concentric posterior microchondrectomies and sutures for correction of prominent ears. J Plast Reconstr Aesthet Surg. 2018;71(6):900–5. https://doi.org/10.1016/j.bjps.2018.01.030.
Jones ES, Gibson JAG, Dobbs TD, Whitaker IS. The psychological, social and educational impact of prominent ears: a systematic review. J Plast Reconstr Aesthet Surg. 2020;73(12):2111–20.
Gasques JA, Pereira de Godoy JM, Cruz EM. Psychosocial effects of otoplasty in children with prominent ears. Aesthet Plast Surg. 2008;32(6):910–4. https://doi.org/10.1007/s00266-008-9179-x.
Nazarian R, Eshraghi AA. Otoplasty for the protruded ear. Semin Plast Surg. 2011;25(4):288–94. https://doi.org/10.1055/s-0031-1288921.
Wright WK. Otoplasty goals and principles. Arch Otolaryngol. 1970;92(6):568–72. https://doi.org/10.1001/archotol.1970.04310060040008.
Goulart FO, Arruda DSV, Karner BM, Gomes PL, Carreirão S. Correction of prominent ears by the cartilaginous incision technique, definition of the antihelix with Mustardé sutures and fixation of the cartilage at the mastoid. Rev Bras Cir Plast. 2011;26(4):602–7.
McDowell AJ. Goals in otoplasty for protruding ears. Plast Reconstr Surg. 1968;41(1):17–27. https://doi.org/10.1097/00006534-196801000-00004.
Acknowledgements
We would like to appreciate all the patients and their caretakers for participating in this study. We also thank the Orelhinha Institute and our research assistants for their unwavering dedication to the success of the study.
Funding
This work was self-funded by the authors.
Author information
Authors and Affiliations
Contributions
M.S.A. wrote the main manuscript, did the research and development work on the technique presented, and chose the photos. L.S.M. revised the manuscript and prepared the tables. All authors reviewed, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Orelhinha Institute approved this study. Informed consent was obtained from all individual participants and parents/legal guardians in case of minor participants included in the study. Patients signed informed consent regarding publishing their data and photographs. The participant has consented to the submission of the case reports to the journal.
Consent of publication
All participants consented for publication of the results of the study.
Competing interests
All authors declared they had no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Assis, M.S., Miranda, L.S. Performance-optimized otoplasty. BMC Surg 22, 182 (2022). https://doi.org/10.1186/s12893-022-01587-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-022-01587-y