Abstract
Background
To analyze whether neoadjuvant chemoradiotherapy (nCRT) could improve the survival for patients with adenocarcinoma of the esophagogastric junction compared with neoadjuvant chemotherapy (nCT). Both neoadjuvant chemotherapy alone and chemoradiotherapy before surgery have been shown to improve overall long-term survival for patients with adenocarcinoma in the esophagus or esophagogastric junction compared to surgery alone. It remains controversial whether nCRT is superior to nCT.
Methods
170 Patients with locally advanced (cT3-4NxM0) Siewert II and III adenocarcinoma of the esophagogastric junction (AEG) were treated with neoadjuvant chemotherapy consisting of capecitabine plus oxaliplatin with or without concurrent radiotherapy in the Fourth Hospital of Hebei Medical University. Intensity-modulated radiation therapy (IMRT) was used and delivered in 5 daily fractions of 1.8 Gy per week for 5 weeks (total dose of PTV: 45 Gy). 120 Patients were included in the propensity score matching (PSM) analysis to compare the effects of nCRT with nCT on survival.
Results
With a median follow-up of 41.2 months for patients alive after propensity score matching analysis, the 1- and 3-year OS were 84.8%, 55.0% in nCRT group and 78.3%, 38.3% in nCT group (P = 0.040; HR = 1.65, 95% CI 1.02–2.69). The 1- and 3-year PFS were 84.9%, 49.2% in nCRT group and 68.3%, 29.0% in nCT group (P = 0.010; HR = 1.80, 95% CI 1.14–2.85). The pathological complete response (pCR) was 17.0% in nCRT group and 1.9% in nCT group (P = 0.030). No significant difference was observed in postoperative complications between the two groups.
Conclusion
The nCRT confers a better survival with improved R0 resection rate and pCR rate compared with nCT for the patients with locally advanced AEG.
Similar content being viewed by others
Background
Surgical resection remains the main cornerstone of the treatment for resectable advanced adenocarcinoma of the esophagogastric junction (AEG). Neoadjuvant chemotherapy alone (nCT) and chemoradiotherapy (nCRT) have been shown to improve overall long-term survival for patients with adenocarcinoma in the esophagus or esophagogastric junction compared to surgery alone [1,2,3,4,5,6]. The MAGIC trial showed a significant benefit of perioperative chemotherapy (epirubicin, cisplatin, and infused fluorouracil) plus surgery over surgery alone in R0 resection rates and survival for resectable gastroesophageal cancer [7]. In the CROSS study [3], the long-term follow-up results showed that the neoadjuvant chemoradiotherapy combined with surgery had the overall survival benefits both for squamous cell carcinoma and adenocarcinoma subtypes in patients with resectable esophageal or esophagogastric junctional cancer. So the neoadjuvant treatment has become the standard treatment modality. Neoadjuvant CRT could confer a better local tumor control with improved R0 resection rates, higher complete histological response (pCR) rate, fewer lymph node metastases compared with nCT, but no survival difference was observed between preoperative CRT and CT [8,9,10]. It remains controversial whether nCRT is superior to nCT. Both nCRT and nCT were undertaken in the clinical practice in our institution. The incidence of Siewert type I tumors is less frequent in Eastern countries than in Western countries. The majority of patients with AEG in Asia have Siewert II and III cancers, which distribution is quite different from western countries. The similar clinicopathologic characteristics were found in AEG II and AEG III, and there was no significant difference in prognosis between AEG II and AEG III [11]. Our previous retrospective study showed that the addition of radiotherapy to preoperative chemotherapy could improve survival with safety, but was not an independent prognostic factor for overall survival (OS) and progression-free survival (PFS) [12]. Only the patients accomplishing preoperative therapy and surgery were enrolled and the intent-to-treat (ITT) method was not used in the study, so bias may exist in evaluating the survival. In this study, all patients who received nCRT/nCT were enrolled and followed up for a longer period in time, and were analyzed by propensity score matching (PSM) analysis to explore whether radiotherapy added to nCT could improve the survival of the patients with locally advanced Siewert II and III AEG.
Methods
Eligibility criteria
We reviewed the data of patients with locally advanced (cT3-4NxM0) Siewert II and III AEG and treated by nCRT or nCT in our hospital between March 2012 and December 2015. It was decided by the preference of surgical oncologists and importantly by the preference of the patients if patients received nCT or nCRT. The patients were divided into nCRT group and nCT group. The Review Board of the Fourth Hospital of Hebei Medical University approved this retrospective study (Ethic approval code: 2017MEC004).
Treatment
Patients were treated with capecitabine plus oxaliplatin for chemotherapy. The chemotherapy comprised intravenous administration of oxaliplatin (130 mg/m2) on day 1, followed by orally administration of 1000 mg/m2 of capecitabine twice daily for 14 days. The same chemotherapy regimen was given before and after surgery. In the nCRT group, radiotherapy and chemotherapy were performed concurrently. A total radiation dose of 45 Gy by intensity-modulated radiation therapy (IMRT) was administered in 25 fractions of 1.8 Gy, with one time a day and five days per week. The liver, kidneys, spinal cord and heart were organs at risk which were needed to be protected. Surgery was given preferably 6 to 8 weeks after the end of neoadjuvant treatment. Surgical treatment include proximal subtotal gastrectomy/total gastrectomy and extended lymph node dissection (D2 resection). Proximal subtotal gastrectomy and jejunal interposition, proximal subtotal gastrectomy anastomoses with esophagogastric residues, or total gastrectomy anastomoses with Roux-en-Y was conducted through laparotomy.
Pathologic evaluation
The pathological analysis included complete resection rate and pathological complete response (pCR), which defined as absence of tumor in the final specimen, lymphovascular invasion, nerval invasion, node positive number, node positive rate.
Follow-up and statistical analysis
The patients were followed up regularly. The follow-up included a complete medical history, a physical examination, chest and abdominal CT or magnetic resonance imaging, or positron emission tomography if possible and endoscopy if clinically indicated. OS was defined the time from the beginning of treatment to the time of death or follow-up deadline. PFS was defined the time from the beginning of treatment to the time of the first tumor progression time or death. The patients were not randomly assigned in our cohort. To minimize the baseline differences between the nCRT group and nCT group, the PSM analysis was conducted with age, sex, Siewert type, Eastern Cooperative Oncology Group score (ECOG), clinical T stage (cT), clinical N stage (cN) and Her-2 status included in the covariates. To evaluate the significance of differences between the two groups, Chi-square test and t-test were used. The OS and PFS were analyzed using Kaplan–Meier method. The log-rank test was used to analyse the differences in survival. P value lower than 0.05 was considered statistically significant. SPSS version 19.0 software was used for all statistical analysis.
Results
Patients’ characteristics
There were 170 patients with either nCT or nCRT. Eighty-one patients were in nCRT group and eighty-nine patients in nCT groups. The patients’ baseline characteristics were listed in Table 1. After propensity score matching with the covariates which included age, sex, smoking status, Siewert type, ECOG score, cT, cN, and Her-2 status, there were sixty patients in each group, as in Table 1. There were forty-eight and forty-nine patients receiving adjuvant chemotherapy (a median of 4 cycles) respectively in nCRT group and nCT group (P = 0.192). The study enrollment was demonstrated in Fig. 1.
Survival
The median follow-up time was 26.0 (4.5–74.2) months for all patients before PSM. The 1- and 3-year OS were 85.1% and 56.7% in nCRT group versus 79.8% and 36.5% in nCT group (p = 0.029, HR = 0.637, 95%CI 0.42–0.96). The 1- and 3-year PFS rates were 83.9% and 52.7% in nCRT group versus 73.0% and 32.1% in nCT group (P = 0.011; HR = 0.61, 95%CI 0.41–0.90). The median follow-up time was 41.2 (22.5–73.7) months for patients alive after PSM. Sixty-nine patients were deceased (29 in nCRT group and 40 in nCT group). The median survival, 1- and 3-year OS were 46.0 months, 84.8% and 55.0% in nCRT group versus 24.0 months, 78.3% and 38.3% in nCT group (p = 0.040, HR = 1.65, 95%CI 1.02–2.69) (Fig. 2a). The median PFS, 1- and 3-year PFS rates were 31.5 months, 84.9% and 49.2% in nCRT group versus 19.0 months, 68.3% and 29.0% in nCT group (p = 0.010; HR = 1.80, 95%CI 1.14–2.85) (Fig. 2b).
Fifty-three patients and fifty-two patients received operation in nCRT group and nCT group respectively. The reasons for receiving no operation were demonstrated in Fig. 1. For the patients with surgery, the median survival, 1- and 3-year OS were 59.3 months, 88.6% and 62.5% in nCRT group versus 28.0 months, 78.8% and 35.3% in nCT group (p = 0.016, HR = 1.94, 95% CI 1.12–3.37). The median PFS, 1- and 3-year PFS rates were 45.9 months, 88.6% and 56.0% in nCRT group versus 19.0 months, 67.3% and 29.9% in nCT group (p = 0.004; HR = 2.09, 95%CI 1.25–3.50).
Pathologic evaluation after surgery
The median interval time from the end of neoadjuvant therapy to surgery were 45 days (range 40–57) and 47 days (range 43–58) in the nCRT group and nCT group respectively. The median number of examined lymph nodes were 29 (range 9–54) in nCRT group and 32 in nCT group (range 10–72), respectively. R0 resection and pCR were improved in nCRT group compared with nCT group (p = 0.026 and p = 0.030). Lymphovascular invasion, nerval invasion and node positive rate were decreased in nCRT group versus nCT group (p = 0.058, p = 0.011, p < 0.001 respectively) (Table 2).
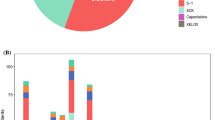
Toxicities and postoperative complications
During the neoadjuvant therapy, all patients were assessed weekly about acute toxicities. The toxicities included gastrointestinal toxicities, hematologic toxicities (leukopenia, neutropenia, anemia and thrombocytopenia), pneumonitis and esophagitis. There was no significant difference in gastrointestinal toxicities between nCRT group and nCT group (p = 0.250). There were 7 patients with ≥ grade 3 hematologic toxicities in nCRT group and 0 in nCT group (p < 0.05). And 3 of them did not receive surgery because of the hematological toxicity (thrombocytopenia) and poor general condition thereafter for a long time after chemoradiotherapy. No grade 3 esophagitis and pneumonitis occurred in nCRT group.
Postoperative complications occurred in 20.8% (11/53) of the nCRT patients and 19.2% (10/52) of the nCT patients (p = 0.713). There were 10 patients with pneumonia after surgery in nCRT (one with chylothorax) and 9 patients in nCT group (three with pleural effusion) (Table 3). One patient was with pleural effusion alone in nCRT group and one with venous thromboembolic disease alone in nCT group. In the nCRT group, one patient died of postoperative respiratory failure. There were two patients with intestinal obstruction in nCRT group and one patient in nCT group, who were deceased 17, 18 and 24 months respectively after surgery.
Patterns of failure
For patients who were given operation after matching, locoregional recurrence occurred in 3.8% (2/53) patients of nCRT group and 26.9% (14/52) of nCT group (p = 0.001). Distant metastases were observed in 20.8% (11/53) patients of nCRT group and 23.1% (12/52) patients of nCT group (p = 0.774). Locoregional recurrence concurrent with distant metastasis was 3.8% (2/53) in nCRT group and 7.7% (4/52) in nCT group (Table 4). No locoregional recurrence occurred in pCR patients. Only, one pCR patient failed with liver metastasis in nCRT group.
For the 7 patients who received no operation in nCRT group, locoregional recurrence occurred in 2 patients and distant metastases in 4 patients (2 liver metastasis, 1 peritoneal metastasis and 1 peritoneal with liver metastasis). And among the 8 patients in the nCT group, 3 patients developed locoregional recurrence and 2 patients were diagnosed with liver and abdominal metastasis.
Discussion
The purpose of this study was used ITT method to evaluate whether nCRT could improve the prognosis of the patients with locally advanced AEG compared with nCT. Because the patients were not randomly assigned in our cohort, PSM analysis was used to minimize the statistical bias. In our study, the OS and PFS were both improved in nCRT group compared with nCT group with statistical difference (55.0% and 49.2% versus 38.3% and 29.0% in 3-year OS and PFS) after PSM. The chemoradiotherapy improved 16.7% compared to chemotherapy alone in 3-year OS. The R0 resection rate were higher in nCRT compared with nCT group (98.1% versus 82.7%, P = 0.026) and pCR (17.0% versus 1.9%, P = 0.030). Node positive rate was decreased in the nCRT group compared with nCT group (4.4% versus 23.4%, P < 0.05).
Whether sruvival can benefit from radiotherapy combined with preoperative chemotherapy was still controversial. Sthal et al. [8] compared the preoperative CRT with CT in patients of locally advanced AEG. The results showed that preoperative radiotherapy improved 3-year survival rate by nearly 20% and improved R0 resection rate and pCR. In the randomized studies with pCR as the primary endpoint [9, 10], pCR was improved by nCRT and no significant difference in OS was observed, which favored the patients receiving CRT with no significant difference in surgical toxicity. In a recent systematic review and meta-analysis [13] comparing neoadjuvant CRT with CT for adenocarcinoma of GEJ, no difference was found in terms of median OS, despite a higher pCR rate and a reduced risk of locoregional recurrences for the combined approach. In addition, the propensity-adjusted analysis comparing neoadjuvant chemoradiotherapy and chemotherapy from the National Cancer Data Base (NCDB) of America showed no difference in survival in resectable esophageal and gastroesophageal junction adenocarcinoma, though R0 resection and pCR in the neoadjuvant radiotherapy were improved and lymph node positive rate decreased in neoadjuvant chemoradiotherapy compared with neoadjuvant chemotherapy [14]. There were more patients with smaller tumors and lower proportion of patients with stage III stage in the study with big data base. And we should note that more patients received adjuvant chemotherapy in nCT group than in nCRT group (24.5% versus 7.1%) in the study. In our study, 90.1% and 94.2% patients received adjuvant chemotherapy respectively in nCRT group and nCT group, so the effect of adjuvant chemotherapy on survival was not analyzed. In the aforementioned randomized studies for comparing nCT and nCRT, it is underpowered to analyze the survival difference either because of primary endpoint design [9, 10] or due to the difficulty of accrual [8]. Aforementioned studies included the patients with early stage of AEG and esophageal adenocarcinoma [9, 10, 15], even the patients with squamous cell carcinoma of esophagus [16]. Only Stahl et al. trial studied the patients with AEG in locally advanced stage (T3-4NXM0) [8]. And in our study only the locally advanced (cT3-4NxM0) AEG were included. It may explain the different results in different researches.
In our study, 3 patients were not given operation in nCT group because of disease progression at liver metastasis and peritoneal metastasis. Disease progression in a short period of time may be related to imperfect staging before treatment. Therefore, standard comprehensive staging is essential. Laparoscopy has become an important tool in the diagnosis, staging and treatment of patients with AEG. It was reported that diagnostic staging laparoscopy before treatment could avoid unnecessary laparotomy and let the patients to be able to receive appropriate alternative treatment [17]. Even for the patients with negative pretreatment laparoscopy, post-preoperative treatment laparoscopy may also prevent non-therapeutic laparotomies [18].
From the patterns of failure in our study, nCRT decreased the locoregional failure significantly in nCRT group were 3.8% versus 26.9% in nCT group (p = 0.001) without significant effect on distant metastases compared with nCT (20.8% versus 23.1%) (p = 0.774), which was similar to the result from Stahl M, et al. study [8]. Micrometastases outside the local tumor may affect the long-term result, which means adjuvant chemotherapy or other systemic therapy is important to reduce the risk of distant metastases.
CRT might increase treatment-related death [19, 20]. Common side effects during chemotherapy and chemoradiotherapy were gastrointestinal and hematologic toxicities. In our study, there were 7 patients (11.7%) and 0 with hematologic ≥ grade 3 toxicity during the neoadjuvant treatment in nCRT group and nCT group respectively. In nCRT group, three patients did not undergo surgery due to the hematological toxicities and the poor general condition after chemoradiotherapy. The concurrent chemoradiotherapy may increase the severity of side effects to a certain extent, and make patients loss the opportunity to receive subsequent surgical treatment. But there was no ≥ grade 3 radiation esophagitis or pneumonitis in nCRT group. No significant difference was observed in postoperative complications between the two groups, which was similar in two retrospective studies [21, 22]. Only one patient died of postoperative respiratory failure in nCRT group in 30 days after surgery. The nCRT with capecitabine plus oxaliplatin was well-tolerated. A mata-analysis [23] had confirmed that neoadjuvant CRT plus surgery did not increase the risk of adverse events morbidity.
However, this study had some limitations. As a retrospective study, bias may exist in evaluating the survival even with the propensity score matching analysis. Despite the advantages of nCRT over nCT, some patients may postpone or lose the opportunity to receive surgery or subsequent treatment due to the hematological toxicities. The follow-up time was not long enough to evaluate the 5-year survival precisely. Future randomized studies with big sample sizes are required to prove that adding radiotherapy to preoperative chemotherapy improves prognosis.
Conclusion
In conclusion, neoadjuvant chemoradiotherapy might improve the overall survival and progression-free survival, increase R0 resection and pCR rate, decrease the locoregional failure over neoadjuvant chemotherapy with no significant increase of postoperative complications for the patients with locally advanced adenocarcinoma of esophagogastric junction.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- nCRT:
-
Neoadjuvant chemoradiotherapy
- nCT:
-
Neoadjuvant chemotherapy
- AEG:
-
Adenocarcinoma of the esophagogastric junction
- IMRT:
-
Intensity-modulated radiation therapy
- PSM:
-
Propensity score matching
- pCR:
-
Pathological complete response
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- ITT:
-
Intent-to-treat
- ECOG:
-
Eastern Cooperative Oncology Group
References
Schuhmacher C, Gretschel S, Lordick F, et al. Neoadjuvant chemotherapy compared with surgery alone for locally advanced cancer of the stomach and cardia: European Organisation for Research and Treatment of Cancer randomized trial 40954. J Clin Oncol. 2010;28(35):5210–8. https://doi.org/10.1200/JCO.2009.26.6114.
Ychou M, Boige V, Pignon JP, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29(13):1715–21. https://doi.org/10.1200/JCO.2010.33.0597.
Shapiro J, van Lanschot JJB, Hulshof MCCM, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–8. https://doi.org/10.1016/S1470-2045(15)00040-6.
Walsh TN, Noonan N, Hollywood D, et al. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med. 1996;335(7):462–7. https://doi.org/10.1056/NEJM199608153350702.
Kim S, Paget-Bailly S, Messager M, et al. Perioperative docetaxel, cisplatin, and 5-fluorouracil compared to standard chemotherapy for resectable gastroesophageal adenocarcinoma. Eur J Surg Oncol. 2017;43(1):218–25. https://doi.org/10.1016/j.ejso.2016.06.395.
Ronellenfitsch U, Schwarzbach M, Hofheinz R, et al. Preoperative chemo (radio)therapy versus primary surgery for gastroesophageal adenocarcinoma: systematic review with meta-analysis combining individual patient and aggregate data. Eur J Cancer. 2013;49(15):3149–58. https://doi.org/10.1016/j.ejca.2013.05.029.
Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl Med. 2006;355(1):11–20. https://doi.org/10.1056/NEJMoa055531.
Stahl M, Walz MK, Stuschke M, et al. Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol. 2009;27(6):851–6. https://doi.org/10.1200/JCO.2008.17.0506.
Burmeister BH, Thomas JM, Burmeister EA, et al. Is concurrent radiation therapy required in patients receiving preoperative chemotherapy for adenocarcinoma of the oesophagus? A randomised phase II trial. Eur Cancer. 2011;47(3):354–60. https://doi.org/10.1016/j.ejca.2010.09.009.
Klevebro F, Alexandersson DG, Wang N, et al. A randomised clinical trial of neoadjuvant chemotherapy versus neoadjuvant chemoradiotherapy for cancer of the oesophagus or gastro-oesophageal junction. Ann Oncol. 2016;27(4):660–7. https://doi.org/10.1093/annonc/mdw010.
Suh YS, Han DS, Kong SH, et al. Should adenocarcinoma of the esophagogastric junction be classified as esophageal cancer? A comparative analysis according to the seventh AJCC TNM classification. Ann Surg. 2012;255(5):908–15. https://doi.org/10.1097/SLA.0b013e31824beb95.
Ge XK, Zhao Q, Song YZ, et al. Comparison of preoperative concurrent chemoradiotherapy with chemotherapy alone in patients with locally advanced Siewert IIand III adenocarcinoma of the esophagogastric junction. Eur J Surg Oncol. 2018; 44 (4) :502–508. [PMID: 29395438. DOI:https://doi.org/10.1016/j.ejso.2017.11.026]
Meng X, Wang L, Zhao Y, et al. neoadjuvant chemoradiation treatment for resectable esophago-gastric cancer: a systematic review and meta-analysis. J Cancer. 2019;10(1):192–204. https://doi.org/10.7150/jca.25915.
Al-sukhni E, Gabriel E, Attwood K, et al. No survival difference with neaodjuvant chemoradiotherapy compared with chemotherapy in resectable esophageal and gastroesophageal junction adenocarcinoma: Results from the National Cancer Data Base. J Am Coll Surg. 2016;223(6):784–92. https://doi.org/10.1016/j.jamcollsurg.2016.09.002.
Davies AR, Gossage JA, Zylstra J, et al. Tumor stage after neoadjuvant chemotherapy determines survival after surgery for adenocarcinoma of the esophagus and esophagogastric junction. J Clin Oncol, 2014; 32 (27):2983–2990. [PMID: 25071104. DOI:https://doi.org/10.1200/JCO.2014.55.9070]
Zhao Q, Li Y, Wang J, et al. Concurrent Neoadjuvant chemoradiotherapy for Siewert II and III adenocarcinoma at gastroesophageal junction. Am J Med Sci. 2015;349(6):472–6. https://doi.org/10.1097/MAJ.0000000000000476.
Irino T, Sano T, Hiki N, et al. Diagnostic staging laparoscopy in gastric cancer: a prospective cohort at a cancer institute in Japan. Surg Endosc. 2018;32(1):268–75. https://doi.org/10.1007/s00464-017-5673-z.
Thiels CA, Ikoma N, Fournier K, et al. Repeat staging laparoscopy for gastric cancer after preoperative therapy. J Surg Oncol. 2018;118(1):61–7. https://doi.org/10.1002/jso.25094.
Reynolds JV, Ravi N, Hollywood D, et al. Neoadjuvant chemoradiation may increase the risk of respiratory complications and sepsis after transthoracic esophagectomy. J Thorac Cardiovasc Surg. 2006;132(3):549–55. https://doi.org/10.1016/j.jtcvs.2006.05.015.
Klevebro F, Johnsen G, Johnson E, et al. Morbidity and mortality after surgery for cancer of the oesophagus and gastro-oesophageal junction: A randomized clinical trial of neoadjuvant chemotherapy versus neoadjuvant chemoradiation. Eur J Surg Oncol, 2015; 41 (7):920–926. [PMID:25908010. DOI:https://doi.org/10.1016/j.ejso.2015.03.226]
Goense L, van der Sluis PC, van Rossum PSN, et al. Perioperative chemotherapy versus neoadjuvant chemoradiotherapy for esophageal or GEJ adenocarcinoma: a propensity score-matched analysis comparing toxicity, pathologic outcome, and survival. J Surg Oncol. 2017;115(7):812–20. https://doi.org/10.1002/jso.24596.
Anderegg MCJ, van der Sluis PC, Ruurda JP, , et al. preoperative chemoradiotherapy versus perioperative chemotherapy for patients with resectable esophagealor gastroesophageal junction adenocarcinoma. Ann Surg Oncol. 2017;24(8):2282–90. https://doi.org/10.1245/s10434-017-5827-1.
Petrelli F, Ghidini M, Barni S, et al. Neoadjuvant chemoradiotherapy or chemotherapy for gastroesophageal junction adenocarcinoma: a systematic review and meta-analysis. Gastric Cancer. 2019;22(2):245–54. https://doi.org/10.1007/s10120-018-0901-3.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors helped to perform the research; XYQ designed this study; XKG, YZS, YT, SSW and ML analyzed the data; JL and QZ drafted the paper and Co-first authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The retrospective collection and analysis of data were approved by Review Board of the Fourth Hospital of Hebei Medical University (2017MEC004). Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Zhao, Q., Ge, X. et al. Neoadjuvant chemoradiotherapy improves survival in locally advanced adenocarcinoma of esophagogastric junction compared with neoadjuvant chemotherapy: a propensity score matching analysis. BMC Surg 21, 137 (2021). https://doi.org/10.1186/s12893-021-01136-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-021-01136-z