Abstract
Background
Although genes have been previously detected in pancreatic cancer (PC), aberrant genes that play roles in resectable pancreatic cancer should be further assessed.
Methods
Messenger RNA samples and clinicopathological data corrected with PC were downloaded from The Cancer Genome Atlas (TCGA). Resectable PC patients were randomly divided into a primary set and a validation set. Univariable Cox regression analysis, lasso-penalized Cox regression analysis, and multivariable Cox analysis were implemented to distinguish survival-related genes (SRGs). A risk score based on the SRGs was calculated by univariable Cox regression analysis. A genomic-clinical nomogram was established by integrating the risk score and clinicopathological data to predict overall survival (OS) in resectable PC.
Results
Five survival-related genes (AADAC, DEF8, HIST1H1C, MET, and CHFR) were significantly correlated with OS in resectable PC. The resectable PC patients, based on risk score, were sorted into a high-risk group that showed considerably unfavorable OS (p < 0.001) than the low-risk group, in both the primary set and the validation set. The concordance index (C-index) was calculated to evaluate the predictive performance of the nomogram were respectively in the primary set [0.696 (0.608–0.784)] and the validation set [0.682 (0.606–0.758)]. Additionally, gene set enrichment Analysis discovered several meaningful enriched pathways.
Conclusion
Our study identified five prognostic gene biomarkers for OS prediction and which facilitate postoperative molecular target therapy for the resectable PC, especially the nomic-clinical nomogram which may be used as an effective model for the postoperative OS evaluation and also an optimal therapeutic tool for the resectable PC.
Similar content being viewed by others
Introduction
Pancreatic cancer is a malignant neoplasm with a high incidence and mortality worldwide [1, 2]. The near inability to diagnose early stage pancreatic cancer results in missed chances of surgery, which is the main method of cure for PC patients [3]. Additionally, therapeutic schedules for advanced stage pancreatic cancer have made little progress in past decades due to its characteristic insensitivity to radiotherapy and chemotherapy [4]. Furthermore, some of its characteristic proteins are also expressed in chronic pancreatitis, decreasing the biomarker specificity for the diagnosis of PC [5]. Thus, neither the diagnosis nor the therapeutic schedule of pancreatic cancer is satisfactory at present. Therefore, there is an urgent need to identify a novel advanced biomarker for diagnosing and developing therapies for PC patients to decrease mortality. Patients with PC sometimes have very different OS and have different reactions to certain drugs, so key genes that affect OS must be identified.
The TCGA is a National Cancer Institute initiative that provides information on approximately thirty different tumor types with genomic platforms and free access to all investigators [6]. For instance, the mRNA sequencing data and clinicopathological data associated with PC can be obtained from the TCGA.
Accumulating studies have indicated that aberrant genes play important roles in the initiation, progression, and prognosis of tumors and have been explored as cancer biomarkers in past decades [7,8,9,10,11,12]. Although these aberrant gene have been utilized to establish predictive models for PC prognosis prediction, no consensus on their effectiveness has yet been reached. For instance, Song [13] and Shi [14] established predictive models that only used aberrant gene expression. Song W and colleagues [15] established predictive models for PC prognosis prediction using only clinicopathological data. No model to date has been established based on both aberrant gene data and clinicopathological data. Therefore, in this study, we aimed to identify significant aberrant genes and clinicopathological data that could be used to establish a genomic-clinical nomogram, which in turn to predict the prognosis of PC and develop an optimal therapeutic schedule for resectable PC patients.
Methods
Data collection and processing
We downloaded messenger RNA samples and clinicopathological data associated with PC from The Cancer Genome Atlas (https://cancergenome.nih.gov/). We also omitted patients who had zero days of survival, no surgical treatment information, incomplete clinical information, and no gene expression information. Finally, one hundred and twenty-one patients with clinicopathological data associated with messenger RNA information were included, and confirmed by postoperative pathology verified to be pancreatic ductal adenocarcinoma, and were complete resected, Furthermore, patients after surgery were given gemcitabine and 5-fluorouracil chemotherapy. To perform further analysis, the one hundred and twenty-one patients were randomly sorted into a primary set and a validation set.
Identification of aberrantly expressed mRNA
Transcripts per million normalization and log2 transformation were used for the expression profiles. A total of 14,396 annotated genes were employed for differentially expressed analyses by the “Limma” version 3.6.2 R package [16]. Aberrantly expressed genes were selected for subsequent prognostic analysis if (a) they showed consistent expression patterns in the primary set and (b) they were listed in the validation set.
Distinguishing the aberrantly expressed mRNA correlated with prognosis
Univariable Cox regression analysis, lasso-penalized Cox regression analysis [17], and multivariable Cox analysis were applied to determine the survival-related genes (SRGs). P < 0.01 in the univariable Cox regression analysis was regarded as statistically significant. The SRGs were explored as risk score = (Coefficient mRNA1 × expression of mRNA1) + (Coefficient mRNA2 × expression of mRNA2) + (Coefficient mRNAn × expression mRNAn). The R packages “survival” and “survminer” were applied to evaluate the optimal cutoff of risk score. The performance of the risk score was evaluated by area under the curve (AUC) and survival analysis. The R package “survivalROC” was applied to evaluate the prognostic value of the SRGs [18]. A two-sided log-rank p < 0.05 was regarded as significant for survival analysis.
Identification of clinicopathological data in the primary set and validation set
The clinical information associated with the one hundred and twenty-one PC patients were incorporated into the subsequent analysis. Whole clinical information including age, surgery method, whether radiation, gender, grade stage, and TNM stage were screened to build prognostic model. Multivariable Cox regression analyses were implemented for both the primary set and the validation set. P < 0.05 was regarded as statistically significant.
Development and discriminatory validity of the predictive nomogram
A predictive nomogram was established based on the risk scores and clinicopathological data using a backward stepwise Cox proportional hazard model [19] in both the primary set and validation set. The C-index was used to assess the discriminability of the nomogram [20, 21]. A calibration curve was used to evaluate the performance of the nomogram. The protein levels of the five aberrantly expressed SRGs were validated by The Human Protein Atlas database (http://www.proteinatlas.org).
Gene set enrichment analyses
To uncover the underlying Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways of the gene signature, gene set enrichment analyses [22] were employed for screening enriched terms in the primary set or validation set. P < 0.05 and a false discovery rate q < 0.25 were considered statistically significant.
Statistical analysis
Statistical analyses were performed using SPSS V21.0 (SPSS Inc.) and R software v3.6.2 (R Foundation for Statistical Computing, Vienna, Austria). Fisher’s exact test was used to explore qualitative variables as appropriate. The ROC curve was plotted using the R package “qROC.” [23] A heatmap was generated using the R package “gplots.” [24] If not specified above, p < 0.05 was considered statistically significant.
Ethics statement
The TCGA is freely available to all investigators. Thus, supplementary approval by an ethics committee was not necessary in this study.
Results
Building and validation of survival-related gene set
One hundred twenty-one patients and 1055 genes were involved in the primary set to build the prognostic model. Univariable Cox regression, Lasso-penalized Cox analysis, and multivariable Cox analysis distinguished five genes for building a prognostic model. The five genes associated with the model were AADAC, DEF8, HIST1H1C, MET, and CHFR. The risk score was calculated as 0.022 × Expression of AADAC-0.320 × Expression of DEF8+ 0.007 × Expression of HIST1H1C + 0.041 × Expression of MET-0.989 × Expression of CHFR. The heatmap of mRNA expression and the risk score analysis for resectable pancreatic cancer were plotted for the primary set (Fig. 1a) and the validation set (Fig. 1b).
Performance evaluation of risk score in the primary and validation set
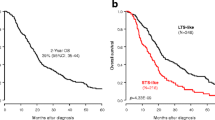
An optimal cutoff of 1.817 for the risk score was utilized to divide patients into a high-risk and a low-risk group in the primary set and the validation set. The overall survival of resectable pancreatic cancer based on risk score of the high-risk group was significantly more unfavorable than that of the low-risk group (p < 0.001; Fig. 2a). Additionally, the prognostic model was validated in the validation set. The overall survival of the resectable pancreatic cancer based on risk score of the high-risk group was significantly poorer than that of the low-risk group (p < 0.001; Fig. 2b). The AUC value calculated to evaluate the performance of the risk score for 1-and 3-year OS were 0.811 and 0.838 in the primary set (Fig. 2a) and 0.719 and 0.699 in the validation set (Fig. 2b).
Evaluation of prognostic factors for resectable pancreatic cancer patients
One hundred and seventy-one patients were divided into a primary set and validation set with whole clinicopathological characteristics, including age, surgery method, radiation, gender, grade stage, and TNM stage, to build a second prognostic model (Table 1).
Development and validation of the predictive nomogram
The nomogram was built from radiotherapy-based characteristics and risk score for the primary set (Fig. 3a). The C-index [0.696 (0.608–0.784)], utilized to evaluate the predictive performance of the nomogram, indicated good performance for the primary set. The calibration curves for the nomogram showed that the nomogram model may be an ideal prediction model for the primary set (Fig. 3b). Meanwhile, the nomogram was validated for the validation set, and the corresponding calibration curves were generated (Fig. 4). The C-index [0.682 (0.606–0.758)] exhibited a greater predictive performance than the nomogram for the validation set. External validation using an online database showed that the proteins encoded by the DEF8 and CHFR genes were found to be significantly underexpressed, and those of the AADAC, HIST1H1C, and MET genes were found to be significantly overexpressed (Fig. 5). The patient immunochemistry data are listed in Supplementary Table S1.
Gene set enrichment analyses
GSEA was implemented and identified 87 significantly enriched KEGG pathways. Among the enriched pathways involved were the calcium signaling pathway, JAK_STAT (The Janus kinase/signal transducer and activator of tranions) signaling pathway, and pentose phosphate signaling pathway. The others involved glycolysis gluconeogenesis-related physiological activity pathways commonly dysregulated in diseases (Fig. 6).
Discussion
Pancreatic cancer has a dismal prognosis and is the seventh leading cause of cancer-related deaths worldwide [25, 26]. The diagnostic experiments available at present are nonspecific in the early stage, and most patients do not exhibit obvious symptoms in the advanced stage, leading to high mortality rates for the disease [27]. Thus, an analysis of aberrant genes as gene signatures in pancreatic cancer to reveal tumorigenesis and prognosis is meaningful. In particular, understanding aberrant genes that regulate molecular mechanisms in resectable PC may provide clinicians with new methods that can be utilized for the diagnosis and therapy of this disease. Recently, the dysfunction of mRNA was shown to occur in diverse cancers and is significantly involved in their prognoses [28,29,30,31]. For instance, some studies have revealed that mRNA gene signatures associated with certain characteristics such as the cell cycle or immune signature can be used in assessing the prediction of mortality risk in cancer [32, 33]. Unsurprisingly, many potential and worthy mRNAs would be indispensable to be identified to assess the prediction of mortality risk for resectable PC patients. Nevertheless, no explicit studies have discovered the aberrant gene expressions associated with prognosis in resectable PC patients. Thus, screening molecular biomarkers for resectable PC patients is urgently needed. In this study, we identified novel and useful SRGs that served as molecular biomarkers for resectable PC patients based on TCGA data.
Univariable Cox regression analysis, lasso-penalized Cox regression analysis, and multivariable Cox analysis suggested that five SRGs [AADAC (P = 0.008), DEF8 (P = 0.026), HIST1H1C(P = 0.031, MET(P = 0.001), and CHFR(P = 0.041)] were significantly associated with the prognosis of resectable PC,. The arylacetamide deacetylase gene (AADAC) lies on chromosome 3q25.1, and its expressed protein consists of 399 amino acids [34, 35]. The protein coded by AADAC protein is extensively implicated in the hydrolysis of various drugs [36], whose function may be related to chemotherapy resistance in pancreatic cancer. Previous experiments unveiled that the AADAC protein is expressed in the pancreas, adrenal glands, small intestine, and liver [37]. Differentially expressed in FDCP 8 homolog (DEF8) is a molecular component that modulates lysosome positioning and secretion [38]. Histone cluster 1 H1 family member c (HIST1H1C) is associated with modulating superior order chromatin structures and may be implemented to preserve DNA methylation patterns [39]. The overexpression of HIST1H1C is associated with unfavorable prognosis in adrenocortical carcinoma [40] and nonfunctional pituitary adenomas [41]. Methyltransferase (MET) is a proto-oncogene encoding the receptor tyrosine kinase c-MET for hepatocyte growth factor (HGF) [42], which triggers cell migration, proliferation, and angiogenesis. Aberrant MET expression is commonly expressed in various malignancies [43,44,45,46,47]. The protein coded by CHFR (Checkpoint with fork head and ring finger domains) serves as a checkpoint that might play diverse roles at different phases of the cell cycle [48, 49]. Specifically, there is evidence that downregulation of CHFR performs this checkpoint function in pancreatic cell lines [50]. The downregulation of CHFR is also correlated with poor prognosis in lung cancer [51], colon cancer [52], and gastric cancers [53]. Some previous experiments showed that targeting CHFR in cancer therapy is effective. For instance, the downregulation of CHFR in Oral squamous cell carcinoma cells was found to be effective in increasing the response to docetaxel [54]. Similarly, the downregulation of CHFR in gastric cancer patients makes them more sensitive to docetaxel exposure [55]. Consequently, CHFR might be a molecular target of therapy in the future. Noteworthy, Henriksen and colleagues disclosed that CHFR gene methylation was involved in lymph node metastasis in patients with PC [56].
We revealed many significantly enriched pathways for the five gene signatures in GSEA, one of which is the JAK-STAT signaling pathway. The JAK-STAT signaling pathway is principally involved in cytokines and growth factors. JAK initiation irritates cell proliferation, differentiation, migration and apoptosis in mammals [57], and previous experiments suggest that this pathway is correlated with pancreatic cancer [58]. As described above, the five gene signatures are associated with dysregulated signaling pathways that may serve as potential molecular targets for therapy for resectable PC.
This study found that the risk score based on prognosis-related genes had a relatively excellent and consistent performance in predicting OS in resectable PC. The AUC based on the risk score for 1-year survival was more than 0.70, indicating a relatively high diagnostic performance in the primary dataset and validation set. For 3-year survival, the AUC based on the risk score was 0.699, indicating a relatively low diagnostic performance in the validation set. However, when the gene signatures alone were used to build a predictive model, it was unable to adequately predict the prognosis of resectable pancreatic cancer. For this reason, we integrated clinicopathological data and gene information to build a predictive nomogram. The C-index [0.696 (0.608–0.784)], utilized to evaluate the predictive performance of the nomogram, indicated good performance for the primary set. Additionally, the C-index [0.682 (0.606–0.758)] exhibited a relatively greater predictive performance by the nomogram for the validation set. Our predictive model suggests that resectable pancreatic cancer patients may benefit from postoperative radiotherapy. External validation using an online database showed that the proteins coded by DEF8 and CHFR were found to be significantly underexpressed and those coded by AADAC, HIST1H1C, and MET were found to be significantly overexpressed (Fig. 5). Thus, our predictive nomogram may contribute to the assessment and development of therapeutic decisions for resectable PC patients.
Few limitations of our studies are as follows: First, we used a single set to build a predictive nomogram. Therefore, a more independent and external set is necessary to verify the predictive ability of the nomogram. Second, functional experiments are necessary to determine the intangible mechanisms of the predictive genes.
Conclusions
Our study identified five prognostic gene biomarkers for OS prediction and might facilitate postoperative molecular targeting therapy for resectable PC. In particular, the genomic-clinical nomogram may be an effective model for evaluating postoperative OS and developing an optimal therapeutic schedule for patients with resectable PC.
Abbreviations
- PC:
-
Pancreatic cancer
- TCGA:
-
The cancer genome atlas
- SRGs:
-
Survival-related genes
- OS:
-
Overall survival
- KEGG:
-
Kyoto encyclopedia of genes and genomes
- C-index:
-
Concordance index
- AUC:
-
Area under the curve
- MET:
-
Methyltransferase
- CHFR:
-
Checkpoint with fork head and ring finger domains
- AADAC:
-
Arylacetamide deacetylase gene
- DEF8:
-
Differentially expressed in FDCP 8 homolog\HIST1H1C Histone cluster 1 H1 family member c
- GSEA:
-
Gene set enrichment analyses
- JAK_STAT:
-
The janus kinase/signal transducer and activator of tranions
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Huang Y-H, Hu J, Chen F, Lecomte N, Basnet H, David CJ, Witkin MD, Allen PJ, Leach SD, Hollmann TJ. ID1 mediates escape from TGFβ tumor suppression in pancreatic Cancer. Cancer Discov. 2020;10(1):142–57.
Neesse A, Bauer CA, Öhlund D, Lauth M, Buchholz M, Michl P, Tuveson DA, Gress TM. Stromal biology and therapy in pancreatic cancer: ready for clinical translation? Gut. 2019;68(1):159–71.
Kokkinos J, Ignacio RMC, Sharbeen G, Boyer C, Gonzales-Aloy E, Goldstein D, McCarroll JA, Phillips PA, Johns AL, Gill AJ. Targeting the Undruggable in pancreatic Cancer using Nano-based gene silencing drugs. Biomaterials. 2020;119742. https://doi.org/10.1016/j.biomaterials.2019.119742.
Eguchi H, Ishikawa O, Ohigashi H, Takahashi H, Yano M, Nishiyama K, Tomita Y, Uehara R, Takehara A, Nakamura Y. Serum REG4 level is a predictive biomarker for the response to preoperative chemoradiotherapy in patients with pancreatic cancer. Pancreas. 2009;38(7):791–8.
Chandran UR, Medvedeva OP, Barmada MM, Blood PD, Chakka A, Luthra S, Ferreira A, Wong KF, Lee AV, Zhang Z, et al. TCGA Expedition: A Data Acquisition and Management System for TCGA Data. PLoS One. 2016;11:e0165395. https://doi.org/10.1371/journal.pone.0165395.
Kong F, Li L, Wang G, Deng X, Li Z, Kong X. VDR signaling inhibits cancer-associated-fibroblasts’ release of exosomal miR-10a-5p and limits their supportive effects on pancreatic cancer cells. Gut. 2019;68(5):950–1.
Gibori H, Eliyahu S, Krivitsky A, Ben-Shushan D, Epshtein Y, Tiram G, Blau R, Ofek P, Lee JS, Ruppin E. Amphiphilic nanocarrier-induced modulation of PLK1 and miR-34a leads to improved therapeutic response in pancreatic cancer. Nat Commun. 2018;9(1):1–18.
Chiou S-H, Risca VI, Wang GX, Yang D, Grüner BM, Kathiria AS, Ma RK, Vaka D, Chu P, Kozak M. BLIMP1 induces transient metastatic heterogeneity in pancreatic cancer. Cancer Discov. 2017;7(10):1184–99.
Wartenberg M, Cibin S, Zlobec I, Vassella E, Eppenberger-Castori S, Terracciano L, Eichmann MD, Worni M, Gloor B, Perren A. Integrated genomic and immunophenotypic classification of pancreatic cancer reveals three distinct subtypes with prognostic/predictive significance. Clin Cancer Res. 2018;24(18):4444–54.
Zhang D, Li L, Jiang H, Knolhoff BL, Lockhart AC, Wang-Gillam A, DeNardo DG, Ruzinova MB, Lim K-H. Constitutive IRAK4 activation underlies poor prognosis and chemoresistance in pancreatic ductal adenocarcinoma. Clin Cancer Res. 2017;23(7):1748–59.
Guo K, Cui J, Quan M, Xie D, Jia Z, Wei D, Wang L, Gao Y, Ma Q, Xie K. The novel KLF4/MSI2 signaling pathway regulates growth and metastasis of pancreatic cancer. Clin Cancer Res. 2017;23(3):687–96.
Song J, Xu Q, Zhang H, Yin X, Zhu C, Zhao K, Zhu J. Five key lncRNAs considered as prognostic targets for predicting pancreatic ductal adenocarcinoma. J Cell Biochem. 2018;119(6):4559–69.
Shi X-H, Li X, Zhang H, He R-Z, Zhao Y, Zhou M, Pan S-T, Zhao C-L, Feng Y-C, Wang M. A five-microRNA signature for survival prognosis in pancreatic adenocarcinoma based on TCGA data. Sci Rep. 2018;8(1):1–10.
Song W, Miao DL, Chen L. Nomogram for predicting survival in patients with pancreatic cancer. Onco Targets Ther. 2018;11:539–45.
Diboun I, Wernisch L, Orengo CA, Koltzenburg M. Microarray analysis after RNA amplification can detect pronounced differences in gene expression using limma. BMC Genomics. 2006;7:252.
Tibshirani R. The lasso method for variable selection in the cox model. Stat Med. 1997;16(4):385–95.
Heagerty PJ, Lumley T, Pepe MS. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 2000;56(2):337–44.
Wu J, Zhou L, Huang L, Gu J, Li S, Liu B, Feng J, Zhou Y. Nomogram integrating gene expression signatures with clinicopathological features to predict survival in operable NSCLC: a pooled analysis of 2164 patients. J Exp Clin Cancer Res. 2017;36(1):4.
Huitzil-Melendez F-D, Capanu M, O'Reilly EM, Duffy A, Gansukh B, Saltz LL, Abou-Alfa GK. Advanced hepatocellular carcinoma: which staging systems best predict prognosis? J Clin Oncol. 2010;28(17):2889.
Diboun I, Wernisch L, Orengo CA, Koltzenburg M. Microarray analysis after RNA amplification can detect pronounced differences in gene expression using limma. BMC Genomics. 2006;7(1):252.
Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub TR, Lander ES. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci. 2005;102(43):15545–50.
Moore HE IV, Andlauer O, Simon N, Mignot E. Exploring medical diagnostic performance using interactive, multi-parameter sourced receiver operating characteristic scatter plots. Comput Biol Med. 2014;47:120–9.
Jedroszka D, Orzechowska M, Hamouz R, Gorniak K, Bednarek AK. Markers of epithelial-to-mesenchymal transition reflect tumor biology according to patient age and Gleason score in prostate cancer. PLoS One. 2017;12:e0188842. https://doi.org/10.1371/journal.pone.0188842.
Huang H, Brekken RA. The next wave of stroma-targeting therapy in pancreatic cancer. Cancer Res. 2019;79(2):328–30.
Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019;10(1):10.
Hidalgo M, Cascinu S, Kleeff J, Labianca R, Löhr J-M, Neoptolemos J, Real FX, Van Laethem J-L, Heinemann V. Addressing the challenges of pancreatic cancer: future directions for improving outcomes. Pancreatology. 2015;15(1):8–18.
Liu GM, Xie WX, Zhang CY, Xu JW. Identification of a four-gene metabolic signature predicting overall survival for hepatocellular carcinoma. J Cell Physiol. 2020;235(2):1624–36.
Jiang K, Liu H, Xie D, Xiao Q. Differentially expressed genes ASPN, COL1A1, FN1, VCAN and MUC5AC are potential prognostic biomarkers for gastric cancer. Oncol Lett. 2019;17(3):3191–202.
Chen YL, Ge GJ, Qi C, Wang H, Wang HL, Li LY, Li GH, Xia LQ. A five-gene signature may predict sunitinib sensitivity and serve as prognostic biomarkers for renal cell carcinoma. J Cell Physiol. 2018;233(10):6649–60.
Kong J, Wang T, Shen S, Zhang Z, Yang X, Wang W. A genomic-clinical nomogram predicting recurrence-free survival for patients diagnosed with hepatocellular carcinoma. PeerJ. 2019;7:e7942.
Zhao L, Jiang L, He L, Wei Q, Bi J, Wang Y, Yu L, He M, Zhao L, Wei M. Identification of a novel cell cycle-related gene signature predicting survival in patients with gastric cancer. J Cell Physiol. 2019;234(5):6350–60.
Song Q, Shang J, Yang Z, Zhang L, Zhang C, Chen J, Wu X. Identification of an immune signature predicting prognosis risk of patients in lung adenocarcinoma. J Transl Med. 2019;17(1):70.
Yamazaki K, Kusano K, Tadano K, Tanaka I. Radiation hybrid mapping of human arylacetamide deacetylase (AADAC) locus to chromosome 3. Genomics. 1997;44(2):248–50.
Muta K, Fukami T, Nakajima M, Yokoi T. N-glycosylation during translation is essential for human arylacetamide deacetylase enzyme activity. Biochem Pharmacol. 2014;87(2):352–9.
Liu X, Wu J, Zhang D, Bing Z, Tian J, Ni M, Zhang X, Meng Z, Liu S. Identification of potential key genes associated with the pathogenesis and prognosis of gastric cancer based on integrated bioinformatics analysis. Front Genet. 2018;9:265.
Yuan L, Zheng W, Yang Z, Deng X, Song Z, Deng H. Association of the AADAC gene and Tourette syndrome in a Han Chinese cohort. Neurosci Lett. 2018;666:24–7.
Fujiwara T, Ye S, Castro-Gomes T, Winchell CG, Andrews NW, Voth DE, Varughese KI, Mackintosh SG, Feng Y, Pavlos N, et al. PLEKHM1/DEF8/RAB7 complex regulates lysosome positioning and bone homeostasis. JCI Insight. 2016;1(17):e86330.
Fan Y, Nikitina T, Zhao J, Fleury TJ, Bhattacharyya R, Bouhassira EE, Stein A, Woodcock CL, Skoultchi AI. Histone H1 depletion in mammals alters global chromatin structure but causes specific changes in gene regulation. Cell. 2005;123(7):1199–212.
Alshabi AM, Vastrad B, Shaikh IA, Vastrad C. Identification of important invasion and proliferation related genes in adrenocortical carcinoma. Med Oncol. 2019;36(9):73.
Applebaum MA, Jha AR, Kao C, Hernandez KM, DeWane G, Salwen HR, Chlenski A, Dobratic M, Mariani CJ, Godley LA, et al. Integrative genomics reveals hypoxia inducible genes that are associated with a poor prognosis in neuroblastoma patients. Oncotarget. 2016;7(47):76816–26.
Garcia-Vilas JA, Medina MA. Updates on the hepatocyte growth factor/c-met axis in hepatocellular carcinoma and its therapeutic implications. World J Gastroenterol. 2018;24(33):3695–708.
Zhu L, Xue F, Xu X, Xu J, Hu S, Liu S, Cui Y, Gao C. MicroRNA-198 inhibition of HGF/c-MET signaling pathway overcomes resistance to radiotherapy and induces apoptosis in human non-small-cell lung cancer. J Cell Biochem. 2018;119(9):7873–86.
Zhao M, Wang Y, Liu Y, Zhang W, Liu Y, Yang X, Cao Y, Wang S. C7 peptide inhibits hepatocellular carcinoma metastasis by targeting the HGF/c-met signaling pathway. Cancer Biol Ther. 2019;20(12):1430–42.
Nandagopal L, Sonpavde GP, Agarwal N. Investigational MET inhibitors to treat Renal cell carcinoma. Expert Opin Investig Drugs. 2019;28(10):851–60.
Miglio U, Berrino E, Panero M, Ferrero G, Coscujuela Tarrero L, Miano V, Dell'Aglio C, Sarotto I, Annaratone L, Marchiò C, et al. The expression of LINE1-MET chimeric transcript identifies a subgroup of aggressive breast cancers. Int J Cancer. 2018;143(11):2838–48.
Cheng F, Guo D. MET in glioma: signaling pathways and targeted therapies. J Exp Clin Cancer Res. 2019;38(1):270.
Scolnick DM, Halazonetis TD. Chfr defines a mitotic stress checkpoint that delays entry into metaphase. Nature. 2000;406(6794):430–5.
Yu X, Minter-Dykhouse K, Malureanu L, Zhao WM, Zhang D, Merkle CJ, Ward IM, Saya H, Fang G, van Deursen J, et al. Chfr is required for tumor suppression and Aurora a regulation. Nat Genet. 2005;37(4):401–6.
Toyota M, Sasaki Y, Satoh A, Ogi K, Kikuchi T, Suzuki H, Mita H, Tanaka N, Itoh F, Issa J-PJ. Epigenetic inactivation of CHFR in human tumors. Proc Natl Acad Sci. 2003;100(13):7818–23.
Koga T, Takeshita M, Yano T, Maehara Y, Sueishi K. CHFR hypermethylation and EGFR mutation are mutually exclusive and exhibit contrastive clinical backgrounds and outcomes in non-small cell lung cancer. Int J Cancer. 2011;128(5):1009–17.
Kawasaki T, Ohnishi M, Nosho K, Suemoto Y, Kirkner GJ, Meyerhardt JA, Fuchs CS, Ogino S. CpG island methylator phenotype-low (CIMP-low) colorectal cancer shows not only few methylated CIMP-high-specific CpG islands, but also low-level methylation at individual loci. Mod Pathol. 2008;21(3):245–55.
Milne AN, Sitarz R, Carvalho R, Polak MM, Ligtenberg M, Pauwels P, Offerhaus GJA, Weterman MA. Molecular analysis of primary gastric cancer, corresponding xenografts, and 2 novel gastric carcinoma cell lines reveals novel alterations in gastric carcinogenesis. Hum Pathol. 2007;38(6):903–13.
Ogi K, Toyota M, Mita H, Satoh A, Kashima L, Sasaki Y, Suzuki H, Akino K, Nishikawa N, Noguchi M. Small interfering RNA-induced CHFR silencing sensitizes oral squamous cell cancer cells to microtubule inhibitors. Cancer Biol Ther. 2005;4(7):773–80.
Koga Y, Kitajima Y, Miyoshi A, Sato K, Sato S, Miyazaki K. The significance of aberrant CHFR methylation for clinical response to microtubule inhibitors in gastric cancer. J Gastroenterol. 2006;41(2):133–9.
Henriksen SD, Madsen PH, Larsen AC, Johansen MB, Drewes AM, Pedersen IS, Krarup H, Thorlacius-Ussing O. Cell-free DNA promoter hypermethylation in plasma as a diagnostic marker for pancreatic adenocarcinoma. Clin Epigenetics. 2016;8:117.
Rawlings JS, Rosler KM, Harrison DA. The JAK/STAT signaling pathway. J Cell Sci. 2004;117(8):1281–3.
Mace TA, Shakya R, Elnaggar O, Wilson K, Komar HM, Yang J, Pitarresi JR, Young GS, Ostrowski MC, Ludwig T. Single agent BMS-911543 Jak2 inhibitor has distinct inhibitory effects on STAT5 signaling in genetically engineered mice with pancreatic cancer. Oncotarget. 2015;6(42):44509.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
CW, ZWW participated in the drafting, writing, revising of the manuscript. BLT participated in the conception and design of the study. Both of them contributed to analysis and interpretation of the data and they approved the final version of the manuscript to be submitted, and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Supplementary Table S1. Clinical Traits of Immunohistochemistry in the Human Protein Atlas Database.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, C., Wu, Z. & Tian, B. Five gene signatures were identified in the prediction of overall survival in resectable pancreatic cancer. BMC Surg 20, 207 (2020). https://doi.org/10.1186/s12893-020-00856-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-020-00856-y