Abstract
Background
Electroencephalography (EEG) is a promising tool for identifying the physiological biomarkers of fibromyalgia (FM). Evidence suggests differences in power band and density between individuals with FM and healthy controls. EEG changes appear to be associated with pain intensity; however, their relationship with the quality of pain has not been examined. We aimed to investigate whether abnormal EEG in the frontal and central points of the 10–20 EEG system in individuals with FM is associated with pain’s sensory-discriminative and affective-motivational dimensions. The association between EEG and the two dimensions of emotional disorders (depression and anxiety) was also investigated.
Methods
In this cross-sectional pilot study, pain experience (pain rating index [PRI]) and two dimensions of emotional disorders (depression and anxiety) were assessed using the McGill Pain Questionnaire (PRI-sensory and PRI-affective) and Hospital Anxiety and Depression Scale (HADS), respectively. In quantitative EEG analysis, the relative spectral power of each frequency band (delta, theta, alpha, and beta) was identified in the frontal and central points during rest.
Results
A negative correlation was found between the relative spectral power for the delta bands in the frontal (r= -0.656; p = 0.028) and central points (r= -0.624; p = 0.040) and the PRI-affective scores. A positive correlation was found between the alpha bands in the frontal (r = 0.642; p = 0.033) and central points (r = 0.642; p = 0.033) and the PRI-affective scores. A negative correlation between the delta bands in the central points and the anxiety subscale of the HADS (r = -0.648; p = 0.031) was detected.
Conclusion
The affective-motivational dimension of pain and mood disorders may be related to abnormal patterns of electrical activity in patients with FM.
Trial registration
Retrospectively registered on ClinicalTrials.gov (NCT05962658).
Similar content being viewed by others
Introduction
Fibromyalgia (FM) is a hard-to-manage syndrome that is characterized by generalized and chronic musculoskeletal pain mainly in the tendons and joints. The location and intensity of pain can change over time and during the disease. Other symptoms include fatigue, sleep disturbances, mood disorders, and cognitive dysfunction, such as memory and/or attention changes, descried as “fibro fog” [1,2,3,4,5,6]. With a prevalence of approximately 2–4% in the general population [7], FM considerably affects patients’ quality of life due to functional impairment related to activities of daily living and social participation [8]. The socioeconomic burden of FM is very high; it is estimated that people with FM generate three times more costs (i.e., medical consultations and indirect costs related to loss of productivity) than individuals with chronic pain of other origins [9].
Diagnosing patients with FM in a primary care setting is a complex task. In 1990, the American College of Rheumatology established a set of classification criteria for FM diagnosis. In 2010 and 2016, a positive diagnosis relied on the presence of multiple pain sites, including other sleep, fatigue and “fibro fog” symptoms for at least 3 months [10]. Additionally, the ICD-11 criteria for fibromyalgia emphasize the emotional distress associated with the condition, recognizing it as a core component of the syndrome [11]. However, because its diagnosis relies primarily on the presence of a standardized set of symptoms that are vague and generalized, FM is frequently misdiagnosed and more than 75% of those patients are estimated to remain undiagnosed [12]. Therefore, it is crucial to identify reliable biomarkers that could help in diagnosis and clinical decision-making for choosing the best treatment.
Over the last few decades, quantitative electroencephalography (qEEG) has been used as a tool for detecting changes in brain activities associated with several disorders [13, 14], including FM [15]. Previous studies suggest that power band and density differences exist between individuals with FM and healthy controls [16,17,18,19,20]. In addition, some studies have pointed out that distinct EEG patterns are related to clinical symptoms of FM, such as depression [16, 20], fatigue, and pain [18, 19]. Indeed, patients with chronic pain present abnormal patterns of brain activity, mainly in those areas related to pain processing, such as the anterior cingulate cortex and prefrontal cingulate cortex [1, 19]. Pain duration may be linked to the predominance of specific frequency bands, such as reduced delta spectral power in the insula. Additionally, a predominance of beta spectral power in the front medial area was previously identified in patients with anxiety and depression scores [1]. In general, significant differences in cortical activity in patients with FM during resting state, with decreased absolute power of delta (0.5 to ≤ 4 Hz), theta (> 4 to ≤ 8 Hz), and alpha (> 8 to ≤ 13 Hz) and increased beta activity in the frontal and central brain areas have been observed [15, 21]. Studies have investigated the relationship between EEG patterns and pain sensation [22] or pain intensity [23] in FM. Although pain intensity emerged as the predominant outcome domain in these studies, exploring the potential correlation between changes in cortical activity in FM patients and the specific qualities of pain they experience could yield valuable biomarkers. These biomarkers might enable more effective personalized management of FM [24,25,26].
The experience of pain can be described along two main dimensions: the sensory-discriminative dimension, comprising spatial, temporal, and intensity properties, and the affective-motivational dimension related to the motivational aspect of pain, as well as the behavioral and autonomic reactions evoked [21, 22]. Previous studies point toward a relative specialization of cerebral areas for processing such dimensions of pain [27, 28]. Interestingly, patients with chronic pain present a higher activation of specific brain areas such as the ventromedial prefrontal cortex, dorsolateral prefrontal cortex, and anterior cingulate cortex, all of which are affective-motivational areas. The predominant engagement of frontal and central brain regions in pain processing, along with the abnormal patterns of EEG activity in patients with chronic pain, particularly those with FM, emphasizes the importance of conducting thorough investigations into the experiences of pain quality.
Methods
Study design and setting
This pilot study was conducted in a cross-sectional and exploratory design. The study was carried out in the Laboratory of Applied Neurosciences of the Universidade Federal de Pernambuco, Recife-Brazil from 2021 to 2022. The sample was not probabilistic, and all participants were recruited from reference services in Pernambuco and digital media announcements. The STROBE checklist for cross-sectional studies was adhered to in the development of this study.
Objectives
We aimed to investigate whether the abnormal EEG activities in frontal points of the 10–20 EEG system as F3, F4, Fz, F7, and F8 and central points as C3, C4, and Cz of patients with FM are differently associated with the sensory-discriminative and affective-motivational dimensions of pain. In addition, we investigated the association between EEG activities and two dimensions of emotional disorders (depression and anxiety).
Participants
Participants, both with a diagnosis of FM (FM group) and without (control group), enrolled in this study. Female participants with FM diagnosis (aged between 18 and 60 years old) were recruited and included if they met the following criteria: FM diagnosis according to the 2010 American College of Rheumatology criteria [29] at least 3 months before participation in the study; widespread pain index (WPI) of at least 7 and a symptom severity scale (SS) that equals 5, or a WPI between 4 and 6 and an SS of at least 9; generalized pain, defined as pain in at least four regions of the body assessed via the Pain Rating Index.
Self-reported and pain-free healthy participants (control group), who are sex and age-matched with participants with FM, were also included. Participants with autoimmune or inflammatory diseases that cause pain, such as rheumatoid arthritis, systemic lupus erythematosus, or inflammatory bowel disease were excluded. Additionally, participants with a history of neurological or psychiatric disorders, cognitive impairment, a history of alcohol or drug addiction, and any contraindication for EEG as excessive seborrhea, scalp infection, or pediculosis, were also excluded from the study.
Clinical outcomes
The primary outcome was pain. We used the McGill Pain Questionnaire (MPQ) to classify pain in two dimensions: sensory-discriminatory and affective-motivational [25, 30]. The MPQ is a multidimensional, easy-to-use assessment of pain that consists of 15 representative words from the sensory (11) and affective (4) categories. Each category was rated on a 4-point rating intensity scale (0 = none, 1 = mild, 2 = moderate, or 3 = severe) [31]. Two scores of the pain experience (Pain Rating Index; PRI) were obtained by MPQ: PRI sensory (PRI-S; the sum of groups 1–11; total score range: 0–33) and PRI affective (PRI-A; the sum of groups 12–15; total score range: 0–12). Depression and anxiety were assessed as secondary outcomes using the Hospital Anxiety and Depression Scale (HADS) [32]. The scale consists of a 14-item self-report instrument that is divided into two subscales for anxiety and depression, each containing seven items. The scoring is associated with a Likert-type scale ranging from 0 to 3, and each subscale is evaluated on a range of 0–21 points, with a total score ranging from 0 to 42. A higher score indicates a more severe level of anxiety or depression disorder [33]. The Fibromyalgia Impact Questionnaire (FIQ) was used to assess the overall impact of fibromyalgia on daily lives of participants, measuring physical functioning, work status, depression, anxiety, sleep, pain, stiffness, fatigue, and well-being. It consists of 10 items, with a total score ranging from 0 to 100, where higher scores indicate a greater impact of fibromyalgia on the life of individual [34].
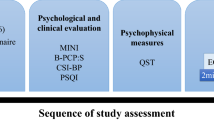
Experimental procedures
The experimental procedures of the study were approved by the Ethics Committee of the Universidade Federal de Pernambuco (4.638.767). This work was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all study participants. The study was retrospectively registered (Registration Date: 18th July 2023) on ClinicalTrials.gov (NCT05962658).Each participant took part in one session that lasted approximately 2 h. All participants with FM were instructed not to change their medication use or eating habits before the session [20, 21]. Initially, clinical and sociodemographic evaluations were conducted. Next, participants were placed in an isolated room without communicating with the external environment. They sat in a comfortable chair and were asked to stay relaxed. EEG signal recording was performed with digital EEG equipment (Neuron-Spectrun/Neurosoft, Russia) using Ag/AgCl electrodes positioned on the scalp with conductive gel following the international 10–20 EEG system [27], with a maximum impedance of 10 kΩ. Additionally, a ground electrode was positioned on the lateral third of the right clavicle, whereas two reference electrodes were positioned over the right and left mastoid processes. Participants kept their eyes closed for 120 s during the recording.
EEG data acquisition and processing
We recorded the relative spectral power of each frequency band (delta, theta, alpha, and beta) at F3, F4, Fz, F7, F8, C3, C4, and Cz. The sampling rate for recording the 500 Hz signal was captured by the Neuron-Spectrum signal amplifier and recorded by the Neuron-Spectrum-4/P omega software (Neurosoft - SN 0117TS-2009, Russia). Additionally, high-pass (0.5 Hz), low-pass (35 Hz), and notch (60 Hz; suitable for 220 V mains) filters were applied during data acquisition and processing. The collected data were preprocessed using the EEGLab toolbox in MATLAB® software (version R2014a; Natick, MA, United States). In addition, an Independent Component Analysis (ICA) was performed using the ICA algorithm to separate the components related to biological artifacts such as eye movements and muscle activity. The rejection of these components was achieved through the Multiple Artifact Rejection Algorithm (MARA), considering a 50% cutoff point [35]. For the frequency analysis of the relative spectral power, the fast Fourier transform method was used for each epoch of 30 s. The dominant frequency, i.e. the frequency with the greatest power in the signal, in each participant was identified for each electrode. Spectral power density assessment was also performed, for each frequency band: delta − (0.5 and ≤ 4 Hz); theta - 𝜃 (> 4 to ≤ 8 Hz); alpha1 – 𝛼1 (> 8 to ≤ 11 Hz); alpha2 (> 11 Hz); beta1 – 𝛽1 (> 13 to ≤ 19 Hz); beta2 – 𝛽2 (19 to ≤ 22 Hz) and beta3 – 𝛽3 (22 to < 30 Hz) [35]. For the relative spectral power distribution calculations, the absolute spectral power of each frequency band was divided by the total power of all the bands that were present in the range of 0.5 to 35 Hz [21].
Statistical analysis
A descriptive analysis was performed to characterize the participants with FM in which continuous variables are presented as means and standard deviations. The Kolmogorov-Smirnov test was performed to assess the normality of all data. Initially, a preliminary analysis was performed by the Mann-Whitney test to check whether the selected sample of participants with FM had distinct EEG patterns (i.e., mean relative spectral power of the frequency band described below) compared with healthy participants. The Mann-Whitney test was also used to determine the differences in mean relative spectral power of the frequency bands: delta - 𝛿 (0.5 and ≤ 4 Hz); theta - 𝜃 (> 4 to ≤ 8 Hz); alpha1 – 𝛼1 (> 8 to ≤ 11 Hz); alpha2 (> 11 Hz); beta1 – 𝛽1 (> 13 to ≤ 19 Hz); beta2 – 𝛽2 (19 to ≤ 22 Hz) and beta3 – 𝛽3 (22 to < 30 Hz) in the pre-specified electrodes (F3, F4, Fz, F7, F8, C3, C4 and Cz). Mann-Whitney-U-test effect size was calculated for the primary outcome using the standardized test statistic Z and the number of pairs “n” through the following equation: r =|Z| / √n An effect size “r” greater than 0.5 is considered a large effect. Spearman’s correlation coefficient was used to assess the degree of correlation of qEEG data with clinical data on pain (PRI-S and PRI-A), depression, and anxiety (HADS). Statistical analysis was performed using SPSS (Statistic Package for Social Science) version 20.0 for Windows (SPSS Inc., Chicago, USA), and the significance level was set at p < 0.05.
Results
Forty-two participants with FM were screened for this study. Eleven met the inclusion criteria and participated in the study (mean age 49.18 years; SD = 7.49 years) (Fig. 1). In addition, for the control group, 10 self-reported healthy and pain-free participants were recruited (mean age 48.5 years; SD = 7.96 years). Clinical characteristics and medication in use of participants with FM are presented in Table 1. Pain levels of participants in the past 24 h were severe, with a mean score of 8.18 (SD = 1.47) on a 0–10 scale. The MPQ showed high scores for both sensory-discriminative (mean = 20.54, SD = 6.59) and affective-motivational pain dimensions (mean = 8.00, SD = 2.28), indicating multifaceted pain. The FIQ score (mean = 71.35, SD = 17.74) indicated a severe impact on daily functioning and quality of life. The HADS score suggested moderate anxiety and mild depression were prevalent. Most participants were on serotonin reuptake inhibitors, with others using anti-inflammatories, benzodiazepines, and opiates.
Preliminary analysis
Mann-Whitney test showed that participants with FM present lower values of relative spectral power in an eyes-closed resting state for the delta band in the F3, F4, Fz, F7, and F8 points than healthy participants (U = 19382; p < 0.001). A similar pattern of decreased mean amplitude values in participants with FM was found for the delta (U = 19519; p < 0.001) and theta (U = 20548.5; p < 0.01) bands in the central points when compared with healthy participants. A decrease in beta2 expression in the central points (U = 19532.4; p < 0.01) and an increase in beta3 expression in the frontal points (U = 21.687.3, p < 0.001) was detected in participants with FM. No additional differences between the two groups were observed in any of the other frequency bands or areas that were analyzed (Table 2). Spectral power graphs of frequency bands for both groups are shown in Fig. 2 (delta, theta, apha1, and apha2 bands) and Fig. 3 (beta1, beta2, and beta3 bands for both groups). Power spectra topographic maps are shown in Figs. 4 and 5.
Correlation of relative spectral power and pain and emotional disorder dimensions
For pain analysis, the Spearman test showed a negative and significant correlation between the relative spectral power in the eyes-closed resting state for the delta band in the frontal points (r = -0.656; p = 0.028) and central points (r = -0.624; p = 0.040) and the PRI-A score. In addition, a positive correlation was found between the relative spectral power for the alpha band in the frontal (r = 0.642; p = 0.033) and central points (r = 0.642; p = 0.033) and the PRI-A scores. For the FIQ scores, the Spearman test revealed a positive correlation with the frontal beta (r = 0.67; p = 0.02) and theta band (r = 0.62; p = 0.04). For the emotional disorder dimensions, the Spearman test showed a negative correlation between the relative spectral power for the delta band in the central points and the anxiety subscale score of HADS (r = -0.648; p = 0.031). No additional correlations were found among the pain dimensions, emotional disorder dimensions, and all other frequency bands and regions (Table 3).
Discussion
The main objective of this study was to investigate whether abnormal qEEG activities in the frontal and central points of the 10–20 EEG system are differently associated with the sensory-discriminatory and affective-motivational dimensions of pain and with emotional symptoms, depression, and anxiety in participants with FM. In the analysis of pain-free controls, we confirmed alterations in qEEG patterns during the eyes-closed resting state in the central and frontal points in participants with FM compared with those of pain-free controls. We found decreased relative spectral power of theta and beta 2 in the central points, increased beta 3 activity in the frontal points, and decreased delta activity in the frontal and central points. Our findings partially follow previous studies showing that individuals with FM had reduced power in low-frequency EEG oscillations (delta and theta in the central points) together with increased power in high-frequency EEG oscillations (beta) over the frontal points during the eyes-closed resting state [1, 21]. Therefore, the abnormal qEEG pattern of reduced delta and enhanced beta activity in the present and previous studies could be interpreted as a neurophysiological marker for individuals with FM during resting. However, there is no consensus in the literature regarding the prevalence of such changes, as other studies have also described different patterns of activity. Additionally, it should be considered that findings may not be consistent with earlier studies due to methodological and study design differences.
A generalized lower frequency power of beta and no significant change in delta activity was described in individuals with FM at rest [36]. Similarly, our study showed decreased relative spectral power of beta 2 in the central points, but in contrast, changes in delta activity were also found in the frontal points. These differences could be attributed to the variation in FM patients’ clinical characteristics. Disease duration, predominance of musculoskeletal symptoms, and emotional disorders were quite different between the study samples. FM symptoms vary considerably over time and from one patient to another [37]. Considering the dynamic nature of clinical manifestations and the high individual variability, the distinct neurophysiological pattern seems to fit the state of symptoms, and therefore a single reliable qEEG signature for patients with FM may be unrealistic.
Our main results give insights that lower delta power and higher alpha power in both the central and frontal points in resting eyes-closed qEEG were associated with higher affective-motivational pain scores in women with FM. A previous study showed event-related desynchronization of the delta band, among other bands, in the central area of the brain in individuals with FM. Such a pattern of activity seems to be related to higher levels of pain, possibly due to an impaired ability to modulate pain perception [23]. The occurrence of lower relative spectral power of delta also highlights the prevalence of higher frequency bands (i.e., alpha), which may point to exacerbated activation of the pain network as a result of a central compensation mechanism, even in resting conditions, in patients with FM [1, 18, 20, 38].
Although emotional disorders are commonly prevalent in individuals with FM, very few studies have investigated the possible correlation between dysfunctional qEEG patterns and the development of depression/anxiety in this population [16, 20, 39]. However, those studies recruited individuals with FM and depression as comorbidities, excluding bipolar depression or pure anxiety disorders. Since we found a correlation between lower delta power in the central points and greater anxiety levels, it becomes difficult to hypothesize why such changes emerged. Although unusual, this is not the first time that lower delta power in the central brain area has been linked to clinical symptoms of anxiety. Lin et al. [40] showed that individuals with anxious major depressive disorder present a generalized pattern of hypercortical arousal compared with a group of healthy controls. In addition to a lower total (and relative) delta in the central points, such patients also presented lower delta in the midline, frontal, parietal, and occipital areas [40]. Previous studies using EEG as a biomarker to identify mood disorders have described hyperactivity (including higher beta, lower delta, and lower theta) in individuals with anxious major depressive disorder [39, 41]. Therefore, we do not rule out that our unusual finding (i.e., lower delta in the central points) may be related to the clinical characteristics of our sample, comprising patients with FM but also with mixed depressive disorder that may not have been identified in clinical screening.
Beyond changes in the central points, our study showed a positive correlation between alpha power in the frontal points and affective-motivational pain scores: the higher the power, the higher the affective-motivational pain score. Lim et al. [17] showed an association between the predominance of higher frequency bands in frontal areas, such as the left dorsolateral prefrontal cortex (DLPFC), and higher levels of affective pain [17]. The involvement of the DLPFC in affective pain processing was not surprising. Among other functions, the DLPFC is considered a neural substrate for executive function, memory, and integration of cognitive, motivational, and emotional information [42,43,44]. Pain is a multidimensional experience that involves sensorial, discriminative, affective, and motivational components and can be associated (or not) with a real tissue injury [45]. In this scenario, it is necessary to better understand whether and how the abnormal qEEG patterns of frontal areas, such as the DLPFC, in patients with FM influence the (hyper)activation of affective-motivational components of pain in this population.
In this study, we did not observe a correlation between qEEG activity patterns in both frontal and central points and the sensory-discriminative dimension of pain. Although a few previous studies have pointed this out, as shown by changes in alpha band activity (i.e., power density and peak frequency) in patients with different types of chronic pain [46], others did not find any correlation [47, 48]. So far, the presence (or absence) of correlations between pain characteristics evaluated by the sensory-discriminative dimension of pain scores and dysfunctional qEEG patterns remains an open question. A recent study performed by Uygur-Kucukseymen et al. [23] addressed this question and observed lower event-related desynchronization on qEEG in the frontal brain areas of individuals with FM, which seems to be related to higher levels of pain intensity and lower inhibitory modulation ability [23]. Despite these promising results, it’s important to note that these findings were derived from different methodological approaches compared to our study. For instance, the Uygur-Kucukseymen study [23] used conditioned pain modulation and other methods, while in our study, qEEG data were collected only during a resting state with eyes closed. qEEG data activity patterns in the resting condition may indicate changes in default mode network (DMN) functioning. Thus, the DMN seems to present a different pattern of cortical recruitment and activation during the pain chronification process. In the early stages, central brain areas, such as the primary and secondary somatosensory cortices are involved. On the other hand, in the late stages, there is greater activation of the frontal areas, such as the ventromedial prefrontal cortex, DLPFC, insular cortex, and anterior cingulate cortex [49].
This study has some limitations that should be considered before interpreting the data. First, qEEG data acquisition was performed without any drug intake restrictions. However, previous studies adopted a similar approach without lowering the confidence of the results [20, 21, 39]. Second, our sample size was smaller in comparison to other studies in the field. Therefore, we regard our findings as preliminary and our study as a pilot experiment. The COVID-19 pandemic emergency was an obstacle to the recruitment of participants for our study. Finally, no corrections for multiple comparisons were performed due to the small sample size and the focus on biological and clinical significance. However, it should be acknowledged that not applying correction for multiple comparisons increases the likelihood of type I errors (false positives). Despite this, as a pilot study, our findings are promising and establish a new perspective in understanding the existing relationship between biological markers obtained through qEEG and some clinical aspects of FM – mainly those related to emotional disorders. Increasing our sample in the future can guide further research in consolidating the possible association between changes in qEEG activity patterns and affective-motivational components. Our findings also highlight the need for future research to more specifically address variables such as medication use, duration of diagnosis, and age, as well as their potential interactions with the outcomes observed. Additionally, future studies could explore EEG power spectra source analysis to determine whether the observed spectral band differences correspond to anatomical regions linked with the pain network.
Conclusions
Patients with FM showed abnormal brain electrical activity patterns in the central and frontal points. The decrease in delta spectral power and the increase in alpha spectral power in the frontal and central points were associated with higher scores in the affective-motivational dimension of pain, and in particular, the decrease in delta in the central points was associated with higher scores of pain and anxiety.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- DLPFC:
-
Dorsolateral Prefrontal Cortex
- DMN:
-
Default Mode Network
- EEG:
-
Electroencephalography
- FM:
-
Fibromyalgia
- HADS:
-
Hospital Anxiety and Depression Scale
- ICA:
-
Independent Component Analysis
- MARA:
-
Multiple Artifact Rejection Algorithm
- MPQ:
-
McGill Pain Questionnaire
- PRI-A:
-
Pain Rating Index - Affective
- PRI-S:
-
Pain Rating Index - Sensory
- PRI:
-
Pain Rating Index
- qEEG:
-
Quantitative Electroencephalography
- SD:
-
Standard Deviation
- SS:
-
Symptom Severity Scale
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- WPI:
-
Widespread Pain Index
References
Gonzalez-Roldan AM, Cifre I, Sitges C, Montoya P. Altered dynamic of EEG oscillations in fibromyalgia patients at rest. Pain Med. 2016;17(6):1058–68. https://doi.org/10.1093/pm/pnw023
Bell T, Trost Z, Buelow MT, Clay O, Younger J, Moore D, Crowe M. Meta-analysis of cognitive performance in fibromyalgia. J Clin Exp Neuropsychol. 2018;40(7):698–714. https://doi.org/10.1080/13803395.2017.1422699. Epub 2018 Feb 1. PMID: 29388512; PMCID: PMC6151134.
Wu YL, Huang CJ, Fang SC, Ko LH, Tsai PS. Cognitive impairment in fibromyalgia: a meta-analysis of case-control studies. Psychosom Med. 2018;80(5):432–438. https://doi.org/10.1097/PSY.0000000000000575. PMID: 29528888.
Ferrera D, Gómez-Esquer F, Peláez I, Barjola P, Fernandes-Magalhaes R, Carpio A, De Lahoz ME, Martín-Buro MC, Mercado F. Working memory dysfunction in fibromyalgia is associated with genotypes of the catechol- O-methyltransferase gene: an event-related potential study. Eur Arch Psychiatry Clin Neurosci. 2023;273(1):25–40. Epub 2022 Sep 13. PMID: 36100778; PMCID: PMC9958168.
Fernandes-Magalhaes R, Ferrera D, Peláez I, Martín-Buro MC, Carpio A, De Lahoz ME, Barjola P, Mercado F. Neural correlates of the attentional bias towards pain-related faces in fibromyalgia patients: an ERP study using a dot-probe task. Neuropsychologia. 2022;166:108141. doi: 10.1016/j.neuropsychologia.2021.108141. Epub 2022 Jan 4. PMID: 34995568.
Peláez I, Ferrera D, Barjola P, Fernandes R, Mercado F. Subliminal emotional pictures are capable of modulating early cerebral responses to pain in fibromyalgia. PLoS ONE. 2019;14(6):e0217909. https://doi.org/10.1371/journal.pone.0217909. PMID: 31166997; PMCID: PMC6550399.
Fitzcharles MA, Perrot S, Hauser W. Comorbid fibromyalgia: a qualitative review of prevalence and importance. Eur J Pain. 2018;22(9):1565–76. https://doi.org/10.1002/ejp.1252
Costa ID, Gamundi A, Miranda JG, Franca LG, De Santana CN, Montoya P. Altered functional performance in patients with fibromyalgia. Front Hum Neurosci. 2017;11:14. https://doi.org/10.3389/fnhum.2017.00014
Souza JBd, Perissinotti DMN. The prevalence of fibromyalgia in Brazil—a population-based study with secondary data of the study on chronic pain prevalence in Brazil. Br J Pain. 2018;1(4):345–8.
Arnold LM, Bennett RM, Crofford LJ, Dean LE, Clauw DJ, Goldenberg DL, Fitzcharles MA, Paiva ES, Staud R, Sarzi-Puttini P, Buskila D, Macfarlane GJ. AAPT diagnostic criteria for fibromyalgia. J Pain. 2019;20(6):611–28. https://doi.org/10.1016/j.jpain.2018.10.008
International Classification of Diseases, Eleventh Revision (ICD-11), World Health Organization (WHO) 2019/2021 https://icd.who.int/browse11. Licensed under Creative Commons Attribution-NoDerivatives 3.0 IGO licence (CC BY-ND 3.0 IGO).
Clauw DJ, Arnold LM, McCarberg BH. The science of fibromyalgia. Mayo Clin Proc. 2011;86(10):907–11. https://doi.org/10.4065/mcp.2011.0206
Shirahige L, Berenguer-Rocha M, Mendonca S, Rocha S, Rodrigues MC, Monte-Silva K. Quantitative electroencephalography characteristics for Parkinson’s disease: a systematic review. J Parkinsons Dis. 2020;10(2):455–70. https://doi.org/10.3233/JPD-191840
Brito R, Baltar A, Berenguer-Rocha M, Shirahige L, Rocha S, Fonseca A, et al. Intrahemispheric EEG: a new perspective for quantitative EEG assessment in poststroke individuals. Neural Plast. 2021;2021:5664647. https://doi.org/10.1155/2021/5664647
De Melo GA, Madruga M, Torro N. Electroencephalographic evaluation in fibromyalgia: a systematic review. Clin EEG Neurosci. 2021. https://doi.org/10.1177/1550059421997128
Vanneste S, Ost J, Van Havenbergh T, De Ridder D. Resting state electrical brain activity and connectivity in fibromyalgia. PLoS ONE. 2017;12(6):e0178516. https://doi.org/10.1371/journal.pone.0178516
Lim M, Kim JS, Kim DJ, Chung CK. Increased low- and high-frequency oscillatory activity in the prefrontal cortex of fibromyalgia patients. Front Hum Neurosci. 2016;10:111. https://doi.org/10.3389/fnhum.2016.00111
Choe MK, Lim M, Kim JS, Lee DS, Chung CK. Disrupted resting state network of fibromyalgia in theta frequency. Sci Rep. 2018;8:2064. https://doi.org/10.1038/s41598-017-18999-z
Fallon N, Chiu Y, Nurmikko T, Stancak A. Altered theta oscillations in resting EEG of fibromyalgia syndrome patients. Eur J Pain. 2018;22(1):49–57. https://doi.org/10.1002/ejp.1076
Navarro López J, Moral Bergós Rd, Marijuán PC. Significant new quantitative EEG patterns in fibromyalgia. Eur J Psychiatry. 2015;29(4):277–92.
Hargrove JB, Bennett RM, Simons DG, Smith SJ, Nagpal S, Deering DE. Quantitative electroencephalographic abnormalities in fibromyalgia patients. Clin EEG Neurosci. 2010;41(3):132–9. https://doi.org/10.1177/155005941004100305
Villafaina S, Collado-Mateo D, Fuentes-Garcia JP, Cano-Plasencia R, Gusi N. Impact of fibromyalgia on alpha-2 EEG power spectrum in the resting condition: a descriptive correlational study. Biomed Res Int. 2019;2019:7851047. https://doi.org/10.1155/2019/7851047
Uygur-Kucukseymen E, Castelo-Branco L, Pacheco-Barrios K, Luna-Cuadros MA, Cardenas-Rojas A, Gianlorenco AC, et al. Decreased neural inhibitory state in fibromyalgia pain: a cross-sectional study. Neurophysiol Clin. 2020;50(4):279–88. https://doi.org/10.1016/j.neucli.2020.06.002
Talbot K, Madden VJ, Jones SL, Moseley GL. The sensory and affective components of pain: are they differentially modifiable dimensions or inseparable aspects of a unitary experience? A systematic review. Br J Anaesth. 2019;123(3):e263–72. https://doi.org/10.1016/j.bja.2019.03.033
Varoli FK, Pedrazzi V. Adapted version of the McGill pain questionnaire to Brazilian Portuguese. Braz Dent J. 2006;17(4):328–35. https://doi.org/10.1590/s0103-64402006000400012
Peláez I, Ferrera D, Barjola P, Fernandes R, Mercado F. Subliminal emotional pictures are capable of modulating early cerebral responses to pain in fibromyalgia. PLoS ONE. 2019;14(6). https://doi.org/10.1371/journal.pone.0217909. PMID: 31166997; PMCID: PMC6550399.
Slater J, Joober R, Koborsy BL, Mitchell S, Sahlas E, Palmer C. Can electroencephalography (EEG) identify ADHD subtypes? A systematic review. Neurosci Biobehav Rev. 2022;139:104752. https://doi.org/10.1016/j.neubiorev.2022.104752
Olbrich S, Arns M. EEG biomarkers in major depressive disorder: discriminative power and prediction of treatment response. Int Rev Psychiatry. 2013;25(6):604–18. https://doi.org/10.3109/09540261.2013.816269
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RL, et al. 2016 revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46:319–29. https://doi.org/10.1016/j.semarthrit.2016.08.012
Pimenta CAM, Teixeira MJ. Questionário De Dor McGill: proposta de adaptação para a língua portuguesa. Rev Esc Enferm USP. 1996;30:473–83.
Menezes Costa Lda C, Maher CG, McAuley JH, Hancock MJ, de Melo Oliveira W, Azevedo DC, et al. The brazilian-portuguese versions of the McGill pain questionnaire were reproducible, valid, and responsive in patients with musculoskeletal pain. J Clin Epidemiol. 2011;64:903–12. https://doi.org/10.1016/j.jclinepi.2010.12.009
Castro MM, Quarantini L, Batista-Neves S, Kraychete DC, Daltro C, Miranda-Scippa A. Validity of the hospital anxiety and depression scale in patients with chronic pain. Rev Bras Anestesiol. 2006;56:470–7. https://doi.org/10.1590/s0034-70942006000500005
Casson AJ, Abdulaal M, Dulabh M, Kohli S, Krachunov S, Trimble E. Electroencephalogram. In: Seamless healthcare monitoring. Springer; 2018. pp. 45–81.
Marques Amélia, Pasqual AM, Barsante Santos A, Assumpção LA, Matsutani LV, Lage, Pereira CAB. Validação Da versão Brasileira do Fibromyalgia Impact Questionnaire (FIQ). Revista brasileira de reumatologia. 2006;46(1):24–31.
Winkler I, Brandl S, Horn F, Waldburger E, Allefeld C, Tangermann M. Robust artifactual independent component classification for BCI practitioners. J Neural Eng. 2014;11:035013. https://doi.org/10.1088/1741-2560/11/3/035013
Martin-Brufau R, Gomez MN, Sanchez-Sanchez-Rojas L, Nombela C. Fibromyalgia detection based on EEG connectivity patterns. J Clin Med. 2021;10. https://doi.org/10.3390/jcm10153277
Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Hauser W, Fluss E, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76:318–28. https://doi.org/10.1136/annrheumdis-2016-209724
Gonzalez-Villar AJ, Trinanes Y, Gomez-Perretta C, Carrillo-de-la-Pena MT. Patients with fibromyalgia show increased beta connectivity across distant networks and microstates alterations in resting-state electroencephalogram. NeuroImage. 2020;223:117266. https://doi.org/10.1016/j.neuroimage.2020.117266
Villafaina S, Sitges C, Collado-Mateo D, Fuentes-Garcia JP, Gusi N. Influence of depressive feelings in the brain processing of women with fibromyalgia: an EEG study. Medicine. 2019;98.
Lin IM, Chen TC, Lin HY, Wang SY, Sung JL, Yen CW. Electroencephalogram patterns in patients comorbid with major depressive disorder and anxiety symptoms: proposing a hypothesis based on hypercortical arousal and not frontal or parietal alpha asymmetry. J Affect Disord. 2021;282:945–52. https://doi.org/10.1016/j.jad.2021.01.001
Wilson HD, Robinson JP, Turk DC. Toward the identification of symptom patterns in people with fibromyalgia. Arthritis Rheum. 2009;61:527–34. https://doi.org/10.1002/art.24163
Lorenz J, Minoshima S, Casey KL. Keeping pain out of mind: the role of the dorsolateral prefrontal cortex in pain modulation. Brain. 2003;126:1079–91. https://doi.org/10.1093/brain/awg102
Tiemann L, Schulz E, Gross J, Ploner M. Gamma oscillations as a neuronal correlate of the attentional effects of pain. Pain. 2010;150:302–8. https://doi.org/10.1016/j.pain.2010.05.014
Wiech K, Ploner M, Tracey I. Neurocognitive aspects of pain perception. Trends Cogn Sci. 2008;12:306–13. https://doi.org/10.1016/j.tics.2008.05.005
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161:1976–82. https://doi.org/10.1097/j.pain.0000000000001939
Harper DE, Ichesco E, Schrepf A, Hampson JP, Clauw DJ, Schmidt-Wilcke T, et al. Resting functional connectivity of the periaqueductal gray is associated with normal inhibition and pathological facilitation in conditioned pain modulation. J Pain. 2018;19:e635631–5615. https://doi.org/10.1016/j.jpain.2018.01.001
Levy MJF, Boulle F, Steinbusch HW, van den Hove DLA, Kenis G, Lanfumey L. Neurotrophic factors and neuroplasticity pathways in the pathophysiology and treatment of depression. Psychopharmacology. 2018;235:2195–220. https://doi.org/10.1007/s00213-018-4950-4
Victor TW, Jensen MP, Gammaitoni AR, Gould EM, White RE, Galer BS. The dimensions of pain quality: factor analysis of the pain quality assessment scale. Clin J Pain. 2008;24:550–5. https://doi.org/10.1097/AJP.0b013e31816b1058
Hashmi JA, Baliki MN, Huang L, Baria AT, Torbey S, Hermann KM, et al. Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain. 2013;136:2751–68. https://doi.org/10.1093/brain/awt211
Acknowledgements
Not applicable.
Funding
This study was financed by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior–Brazil (CAPES)–Finance Code 001. K.M.S was supported by CNPq, Grant No. 311224/2019-9.
Author information
Authors and Affiliations
Contributions
Conceptualization: K.M.S., L.D., and M.C.; Methodology, K.M.S., L.D., M. C., and L.S.; Formal analysis, A.F., and D.P.; Investigation, L.D., R.B., L.S., and M.A.; resources, K.M.S.; Data curation: L.D., M.A.; Writing—original draft preparation, L.D.; Writing—review and editing, K.M.S., D.P., M.C, L.M.; Project administration, K.M.S.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol was reviewed and approved by the Ethics Committee of the Universidade Federal de Pernambuco - Brazil, approval number 4.638.767 (April 2021). All procedure were in accordance with the ethical standards of the Declaration of Helsinki. Written informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Diniz, L., Carneiro, M., Fonseca, A. et al. Can electroencephalography (EEG) identify the different dimensions of pain in fibromyalgia? A pilot study. BMC Musculoskelet Disord 25, 705 (2024). https://doi.org/10.1186/s12891-024-07824-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07824-0