Abstract
Objective
Frozen Shoulder (FS) is a musculoskeletal pathology that leads to disability, functional decline, and a worsening in quality of life. Physiotherapists are the primary professionals involved in the treatment of FS, and it is essential to determine if their practice aligns with evidence-based suggestions.
Aim
The aim is to assess the knowledge, skills, and operational strategies of Italian physiotherapists regarding FS and compare them with the existing literature.
Methods
A web-based, anonymous, and voluntary cross-sectional survey was developed and administered to Italian physiotherapists to evaluate their clinical practices.
Results
A total of 501 physiotherapists (38.5% female), completed the survey. More than half were under 35 years old (67.8%), declared working in private practice settings or being self-employed (57.1%), and were primarily engaged with musculoskeletal patients (81.8%). For subjects with FS at their first access, 21.4% identified X-rays as the most useful imaging technique to recognize pathologies beyond rehabilitation competence. In terms of general management, the majority reported working with an orthopaedic or physiatrist (47.5%) or in a multidisciplinary team (33.5%). Regarding manual therapy techniques, 63.3% of physiotherapists preferred intense degree mobilization, posterior direction, and moderate pain at the end of the range of motion for low irritable/high stiffness FS; however, there is a lack of consensus for managing very irritable/low stiffness FS. The majority of physiotherapists (57.7%) concurred that stretching improves the balance between metalloproteinase and its inhibitors. Additionally, 48.3% of physiotherapists selected mobile phone videos and messages to improve patients’ compliance with exercises at home and for motivational/educational purposes.
Discussion and Conclusion
The clinical practices of Italian physiotherapists in FS subjects sometimes deviate from evidence-based recommendations. While some discrepancies may be attributed to the existing uncertainties in the literature regarding knowledge and management strategies for FS patients, the authors recommend a stronger adherence to evidence-based practice.
Implications of Physiotherapy Practice
Italian PTs’ clinical practices in FS rehabilitation show partial alignment with evidence-based recommendations, particularly in the areas of diagnostic imaging suggestions and clinical assessment.
Italian PTs’ clinical practices exhibit partial adherence to evidence-based suggestions regarding the identification of predisposing factors, staging education, and mobilization modalities in FS cases.
Italian PTs with Orthopaedic Manipulative Physical Therapists (OMPT) certification, those possessing clinical experience ranging from 6 to 10 years, and individuals working in private practice demonstrate greater appropriateness in terms of knowledge, competence, and adherence to evidence-based clinical practices for FS rehabilitation.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Frozen Shoulder (FS), also known as adhesive capsulitis [1, 2], is characterized by persistent, stabbing pain experienced both day and night, along with a gradual limitation of glenohumeral range of movement (ROM)—both active and passive—despite normal radiographic findings. Specific landmarks for diagnosis include a ROM restriction of at least 25% in at least two movement planes, with more than 50% limitation in external rotation at the arm by the side compared to the non-involved side. Additionally, the symptoms must be stable for at least one month or worsening [3, 4], persisting for a duration ranging from few months up to two years [5]. FS commonly affects individuals aged between 45 and 60 years, particularly those with sedentary jobs and low physical activity levels [3], and is often associated with comorbidities, such as diabetes, thyroid [6,7,8,9,10,11], autoimmune [7, 9], and Dupuytren’s disease [7, 8, 12].
Despite extensive study of the pathophysiology [13], the underlying mechanisms of FS remain unclear, leading to uncertainty about the optimal treatment. Evidence firstly suggested conservative treatment [13,14,15]; in particular, pharmacological treatments and physiotherapy, including education [16,17,18], active and passive glenohumeral mobilization [19, 20], stretching [2, 21], and therapeutic exercise [3] were favoured; while, electrotherapy was discouraged [22]. Given that FS significantly impacts quality of life, causing high disability and functional decline [21, 23], understanding the clinical practices of PTs becomes crucial, as they are the primary professionals involved in treating such pathologies. It is essential to assess whether their practice aligns with evidence-based recommendations.
Similar surveys conducted in the United Kingdom and the United Arab Emirates have investigated the diagnosis and management of FS among PTs [24, 25]. Thus, given the lack of such data in Italy, this study aimed to verify the knowledge, skills, and operative strategies of Italian PTs regarding FS treatment.
Evidence suggests that PTs with advanced competencies should be more likely to follow evidence-based practice in their clinical practice [26, 27]. Thus, Italian PTs with a postgraduate manual therapy specialization in Orthopaedic Manipulative Physiotherapy (OMPT) training were investigated to evaluate the effects of implementing evidence-based practice though such particular specialization course. Moreover, the present survey also assessed the impact of other professional characteristics that could condition the clinical practice as (1) years of working experience, (2) working context, (3) university education (recognized as the highest academic qualification), and (4) the number of patients with FS treated, on average, per month.
Methods
Study design
A web-based observational cross-sectional survey was conducted following the CHERRIES checklist [28] and the STROBE [29] reporting guidelines. The study protocol has been submitted and approved by the Technical Scientific Committee of the University of Molise (Italy). All study-related procedures were carried out following the principles of the Declaration of Helsinki [30].
Participants and settings
The sample consisted of PTs practicing in Italy at the time of survey completion. The methodological approach employed in this survey, focused on attaining a maximum number of responses within a predetermined timeframe, is a conventional method for PTs enrolment [26, 27, 31, 32].
Survey participation was extended to professionals through various channels, including social media platforms (Facebook and Twitter), instant messaging applications (Telegram and WhatsApp), or email. The survey link directed PTs to a landing page emphasizing the voluntary and anonymous nature of their involvement. The consent declaration followed an explanation of the study’s purpose, stating, “The participant who willingly chooses to take part in the study must expressly grant consent by clicking the “YES” button, confirming acceptance”. Access to the survey was granted only upon clicking the button mentioned above, signifying consent acceptance (Appendix 1 – Invitation Letter). The respondent sample was categorized into two subgroups: colleagues with postgraduate OMPT specialization and colleagues without such specialization, facilitating meaningful comparisons. The OMPT title aligns with the Italian post-graduate program adhering to the International Federation of OMPT (IFOMPT) standards [33].
Questionnaire development
An online survey was developed based on a questionnaire developed by Brindisino et al. [26]. This instrument was designed to evaluate the proficiency of Italian PTs across key domains: (a) clinical examination strategies, (b) the role of diagnostic imaging in the diagnostic process, (c) physiotherapy, and (d) pharmacological management for subjects with shoulder pain. Notably, the preceding survey targeted both surgeons and PTs; in contrast, the current questionnaire specifically focused on FS pathology and exclusively enlisted the participation of PTs. As a result, specific adjustments were implemented, notably the exclusion of questions related to pharmacological management. This modification reflects the legal limitations that prevent PTs in Italy from prescribing or administering drugs.
Furthermore, two experienced PTs, each with 12 and 15 years of expertise in rehabilitating shoulder pathologies, particularly stiff shoulders, contributed to the restructuring of certain questions. The authors specifically aimed to delve deeper into clinical examination procedures, incorporating six additional questions. Additionally, questions pertaining to the role of education, management strategies, and prognostic factors were introduced. A specific question was included to assess knowledge about the definition of FS. Other questions were tailored to comprehend how PTs evaluate and consider the patient’s perspective and engage in bio-psycho-social practices.
All these questions constituted the pre-final version of the survey. To enhance clarity and comprehensibility, the pre-final version underwent an evaluation by a team of colleagues with diverse experiences in shoulder disease rehabilitation. The team made modifications to only two questions and reached a consensus on the survey, resulting in the final version as follows. The first section (Appendix 2- Section A) consisted of 10 closed multiple-choice questions investigating demographic information for better framing the characteristics of respondents. PT’s year of work experience, working contest, University education (recognized as the highest academic qualification), having a post-graduate IFOMPT specialization degree, and the number of patients with FS treated, on average, per month, were also used to classify the respondents in sub-categories to perform inferences between groups.
The second section (Appendix 2 - Section B) included 22 specific closed multiple-choice questions concerning clinical examination knowledge and strategies, the role of imaging, physiotherapy management, definition, prognostic factors values and knowledge, and bio-psycho-social taking care approaches toward FS. Google Form was the online platform chosen for survey administration and data collection.
Data collection
The survey was conducted using electronic devices and social media platforms and remained accessible for three months (from 01 April 2023 to 01 July 2023). The server was programmed to prevent multiple submissions from the same IP address after a successful submission. Respondents had the option to edit their answers by navigating through the survey questions until the final submission. Data collection was carried out anonymously, without recording IP addresses to safeguard respondent data. Subsequently, the data was forwarded to an external statistician, not involved in the study, for blind data analysis.
Data analysis
Data extraction, processing, and addressing missing responses were performed using Excel. Questions with a missing response rate ≥ 20.0% were considered incomplete and excluded from the analysis [34]. Descriptive statistics, including mean ± standard deviation for interval variables and absolute frequencies with percentages for categorical variables, were used to represent the sample characteristics.
Statistical analysis to identify differences between subgroups of the sample and questionnaire responses utilized the chi-square test or Fisher’s exact test (for cell dimensions lower than 5). In cases where the Chi-Square (χ2) test revealed a statistically significant difference (p < 0.05), adjusted residuals with Bonferroni-corrected p-values were calculated [35] to determine the most contributing cells to the statistical significance of the study [36, 37]. The statistical analysis was conducted using SPSS version 20 Windows software (SPSS Inc., Chicago, Illinois, USA, 2004), with the α level set at p-value < 0.05.
Role of funding source
The founders had no involvement in the design, conduct, or reporting of this study. Additionally, this research did not receive any specific grant from any funding agency in the public, commercial, or non-profit sectors.
Results
Descriptive information, overall sample
A total of 501 PTs completed the survey, and all questionnaires were filled out completely. The analysis revealed that a significant proportion of respondents were male (61.5%) under the age of 35 (67.8%), and 40.8% reported having less than five years of clinical experience. Notably, only 24.8% had clinical experience ranging from 6 to 10 years. Additionally, a majority of PTs indicated their affiliation with private practice or self-employment (57.1%), with a predominant focus on musculoskeletal patients (81.8%).
In terms of the number of FS patients treated, 74.5% of PTs reported managing two or fewer patients, on average, per month. Concerning educational background, 89.2% of PTs held a bachelor’s degree, and only 29.9% possessed a post-graduate IFOMPT specialization degree. The detailed descriptive characteristics of the sample are presented in Table 1.
Clinical knowledge and expertise of respondents (Q12 - Q33)
Questions from Q12 to Q33 investigated the Italian PTs’ clinical knowledge and expertise (both for assessment and treatment) regarding managing subjects with FS.
When dealing with FS subjects at their first access (first assessment), in order to recognize pathologies beyond rehabilitation competence, 21.4% of PTs (Q12) identified X-ray as the most effective imaging technique. In contrast, 42.3% (Q13) believed that clinical examination alone, without additional imaging, was sufficient for the early identification of potential FS. A total of 39.1% of PTs (Q14) considered active and passive ROM assessment, clinical tests, and history-taking as the most valuable procedures for the early identification of FS.
The entire capsule or coracohumeral ligament was considered “the central pivot” of FS by 54.9% and 19.8% of respondents, respectively (Q15). In comparison, the most indicative clinical test for the diagnosis of FS was identified by 67.7% of PTs with a bilateral comparison of external rotation ROM with arm by side (Q16).
Sixty-four point five per cent of respondents defined FS following Kelley’s guideline [4] (Q17), and 48.7% recognized dysmetabolic diseases, age between 40 and 65, sedentary lifestyle, history of FS, being overweight, associated comorbidities as predisposing factors for FS (Q18). When considering priorities for patients, 32.3% and 19.6% of PTs emphasized the importance of reassurance about FS and night pain management, respectively (Q19). Additionally, 68.5% advocated tailoring the treatment based on the subject’s clinical presentation (Q20). Italian PTs expressed a consensus (89.6%) that education about the nature of the pathology, pharmacological interventions, and rehabilitative management should be integrated across the rehabilitation path, addressing both the psychological and pain management aspects (Q21).
In terms of pathology progression, PTs predominantly focused on educating individuals with FS by presenting it as a condition with either three detailed phases (39.5%) or two phases (28.7%) (Q22). They reported collaborating with physicians (47.5%) or functioning within multidisciplinary teams (33.5%), particularly when the expertise of other professionals is deemed necessary (Q23). Concerning the assessment (Q24), PTs universally considered both the pure anatomical aspect and the psychological aspects (fear, worry, anxiety, anger, distrust…) associated with the shoulder problem (85.6%). Furthermore, 88.4% of PTs expressed empathy and attentiveness to the psychological aspect of their clinical practice (Q25). The assessment of the psychological aspect mainly involved extemporaneous, individualized, and non-standardized questions (35.5%) (Q27).
The majority of PTs asserted that specific a-priori coded factors could indicate a worse prognosis (52.1%) (Q26). Additionally, 64.5% identified age < 60 years, external rotation at 0° adducted arm, diabetes and thyroid disease, bilaterality of clinical presentation, and worse symptoms at onset as factors suggesting a worse prognosis (Q28).
Regarding mobilization strategies (Q29 and Q30), 63.3% of PTs expressed a preference for intense mobilization with a posterior direction, moderately painful at the end of the ROM for individuals with low irritability/high stiffness in FS. Conversely, for subjects with high irritability/low stiffness FS, 42.1% of PTs chose mobilization below the pain threshold in any direction, not very intense, at the end of the ROM. Additionally, 57.7% of PTs agreed that stretching improves the balance between metalloproteinase and tissue inhibitors of metalloproteinase (Q31). In terms of enhancing patients’ compliance with exercises at home and for motivational/educational purposes, 48.3% of PTs chose mobile phone videos and messages (Q32). Lastly, concerning conservative treatment (Q33), 53.5% of PTs stated that cortisone therapy (oral or infiltrative) is the preferred solution for better managing the painful phase. The detailed answers to questions Q12-Q33 are reported in Table 2.
Subgroup analyses
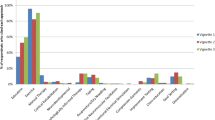
This survey also evaluated the impact of (a) years of working experience, (b) working context, (c) university education (recognized as the highest academic qualification), (d) having a post-graduate IFOMPT specialization degree, and (e) the number of patients with FS treated, on average, per month. The responses to all clinical knowledge and expertise questions (Q12-Q33) were compared with the existing recommendations in the literature. To ensure consistency in the considered variables, categories were consolidated into new labels, as outlined in the “revised descriptive choices” presented in Table 3.
Years of work experience (Q5)
According to Bonferroni’s post-hoc analysis, PTs with 6 to 10 years of experience provided answers in accordance with evidence-based recommendations for Q16, Q28, Q29, Q31, and Q33. Contrariwise, PTs with more than ten years or with less than five years of experience significantly deviated from recommended practices in their answers to Q14, Q29, Q31, and Q21, Q33, respectively.
In terms of the correlation between years of working experience and Q22, where there was no recommended answer, a statistically significant analysis showed differences between groups for respondents with less than five years of experience and those with more than ten years of experience when FS was explained as a pathology with a 4-phase evolution.
Working contest (Q6)
According to Bonferroni’s post-hoc analysis, PT engaged in private practice or self-employed activities adhered significantly to the recommendations when answering Q32 and Q33.
Moreover, they are also less inclined to prioritize reducing daily pain in individuals with FS. Substantial differences between groups emerged in Q19 and Q22, questions for which recommended answers were not outlined in the literature.
University education (Q8)
According to Bonferroni’s post-hoc analysis and considering significant differences between groups and Q25, respondents with a post-bachelor degree tended to be more competent about the anatomical condition than all the other aspects. Furthermore, a significant difference was found between recommended answers to Q15 and Q26 and such group.
Post-graduate IFOMPT specialization degree (Q9)
Statistical significance was obtained between respondents with IFOMPT certification and reassurance about the pathology as the priority for subjects with FS (Q19) and explaining the FS evolution as two phases (i.e., pain predominant or stiff predominant) (Q22). Moreover, such respondents were less inclined to solely assess anatomical features linked to FS (Q24) and significantly answered as recommended by evidence to questions Q12, from Q15 to Q18, Q20, Q21, and from Q27 to Q33.
Number of patients with FS treated, on average, per month (Q11)
Respondents treating more than three subjects with FS per month were more likely to answer that ROM recovery was the priority for FS patients (Q19). Conversely, a significant positive association was found between the recommended answer to Q28 and PTs who treated ≤ 2 patients with FS.
Bonferroni’s post-hoc analysis values were detailed in Tables 4, 5 and 6.
Discussion
The survey revealed that most respondents correctly defined FS [4]. However, there was diversity in explaining the evolution of FS, whether in three, two, or no phases, reflecting heterogeneity in the literature [38]. Current evidence suggests that the traditional chronological division of FS staging lacks interprofessional reliability and clinical relevance; in contrast, categorizing subjects based on high, moderate, and low irritability [3] has been recognized as better guidance for management, allowing for different treatment strategies. Unfortunately, respondents expressed a lack of confidence in these skills, particularly in managing very irritable/low stiff FS, showing a significant lack of consensus. These findings, consistent with previous surveys [24, 25], suggest a need for reflection among clinicians on the absence of evidence-based management guidelines. The newest introduction of the modern theoretical model categorizing FS based on irritability may justify the observed heterogeneity in responses.
To date, prognostic factors assessment has been judged more useful than diagnostic approach [39], and Italian PTs showed to acknowledge such clinical and anamnestic features, categorizing a-priori subjects that could have a worse prognosis.
In addressing the management of the painful phase of FS, most respondents considered it useful to incorporate pharmacological treatments or electrophysical agents. While pharmacological treatments are strongly supported for pain relief [15], electrophysical agents are not recommended, despite being widely used in the Italian clinical practice [22].
Stretching was reported as a valid strategy for improving the subject’s clinical situation as it improves the ratio of metalloproteinase to inhibitory tissues and tissue turnover [40,41,42], as most respondents stated. Conversely, some respondents indicated that stretching could increase the centimetric length of fibrotic structures, highlighting structure-centric and erroneous beliefs regarding the properties of manual therapy techniques [43, 44]. This is a matter of concern, as it might encourage clinicians to apply intense stretching, especially in the early stage when such practice is discouraged and could potentially exacerbate the inflammatory response by increasing the myofibroblast stimulation [5].
Lastly, as far as treatment is concerned, most Italian PTs used videos and mobile text messaging, demonstrating competence in enhancing therapeutic adherence and emphasizing the significance of long-term outcomes in FS subjects. Unfortunately, 22.8% of respondents do not use any particular strategy, possibly indicating a criticism of monitoring home exercise and engaging collaboration.
The identification of FS primarily relies on clinical evaluation, and radiographic imaging is recommended to exclude other pathologies, serving as a complementary diagnostic tool [5, 14, 45]. Our findings indicated that, during the initial assessment, Italian PTs considered X-ray, MRI, or a combination of both as the most useful diagnostic modalities. While this aligns with a previous survey from UK, United Arab Emirates and Korea [24, 25, 46], it’s worth noting that MRI should not be the initial choice for diagnosing FS, as it does not offer additional information beyond clinical examination and could incur unnecessary healthcare costs [47]. These imaging preferences may be influenced by the fact that Italian PTs are not authorized to prescribe diagnostic imaging scans due to legal constraints, and the academic curriculum may lack comprehensive training on imaging assessments.
The majority of Italian PTs identified the entire capsule as “the central pivot” of FS, and recognized bilateral comparison of ROM in external rotation with the arm by the side as the most indicative diagnostic clinical test, aligning with existing evidence [17].
However, the existing evidence suggests that “diagnostic maneuvers” should be supplemented by history taking, palpation, and X-ray examination [3, 4, 13] This is primarily because, in early FS, ROM limitation could be minimal and challenging to diagnose [24, 48] Consequently, FS is often diagnosed at a later stage when stiffness is well established [5, 45]. On this note, evidence indicates that ultrasound with Doppler may serve as a modality to differentiate early stage FS from rotator cuff tendinopathy. The enhanced vascularity and hypoechoic changes around the rotator cuff interval are significant specific indicators of early FS [49]. In the context of Italian physiotherapy practice, ultrasound imaging is allowed not for medical diagnosis purposes, but for a more comprehensive structural evaluation, improving clinical reasoning [50]. Once again, the divergence of PTs’ responses from evidence-based recommendations may be attributed to the fact that the interpretation of clinical examination and testing requires profound expertise and pathology-specific knowledge, which most respondents may not have obtained from their bachelor’s degree programme [51].
Less than half of the respondents accurately identified suggested clinical and anamnestic predisposing factors. One potential explanation is that most PTs completed a three-year BSc training, which may not offer adequate depth in comprehending the pathophysiology and epidemiology of specific clinical conditions. Moreover, there was a greater emphasis on diagnostic evaluation compared to prognostic evaluation [52, 53], emphasizing the importance of encouraging clinicians to identify prognostic factors from a biopsychosocial perspective. This approach has the potential to benefit individuals with FS through a timely, comprehensive, and collaborative strategy involving professionals beyond the scope of physical therapy [39].
Respondents underlined the importance of reassuring patients and addressing nightly pain as the top priorities for individuals with FS, aligning with previous research findings [17, 21, 54]. Moreover, advice and education about the pathology, coupled with simple strategies to modify occupational and recreational activities, were regarded as the primary antalgic strategies. This approach aimed to enhance adherence, reduce anxiety and depression, correct false pain beliefs, and alleviate feelings of uncertainty [5, 17, 21, 55]. Highlighting the significance of the psychological domain in FS subjects [39, 56], the survey results indicated that Italian PTs considered both anatomical factors (directly linked to the shoulder problem) and psychological aspects (such as fear, worry, anxiety, anger, distrust) to demonstrate competence in understanding the anatomical condition and being empathic and attentive to the psychological setup.
PTs preferred to work in a multidisciplinary team when competences of other professionals are required, consistently with what emerged from a previous survey [24] and more recent evidence suggestions [39, 57]. Italian PTs understood the value of multidisciplinary care in improving outcomes and the importance of a targeted/tailored approach that considers the bio-psychological aspects of managing FS. Unfortunately, most respondents were not accustomed to properly assessing psychological variables with dedicated patient-reported outcome measures; instead, extemporaneous non-standardized questions were preferred. This practice could be a limitation in evaluation, potentially leading to a lack of comprehensive assessment of the psychological domain and missing essential features for modifying care appropriately.
Associations
This cross-sectional study also analysed the association between current evidence-based shared recommendations and different subgroups (Table 3).
PTs with less than six years and those with more than ten years of experience provided answers that did not align with the actual recommendations. A possible explanation for these results could be that the first mentioned had restricted knowledge, having only undertaken a three-year academic path and less expertise, and others could be less inclined and motivated to update their expertise.
Furthermore, PTs who worked in private practice or were self-employed significantly adhered to recommendations regarding increasing subject compliance and conservative management of the painful phase: probably, they may be more oriented toward following evidence to achieve results and customer loyalty [58, 59]; as well as for those with post-bachelor degrees, which tend to be significantly more competent in anatomical conditions and more adherent to recommendations about clinical tests and prognosis.
Similarly, PTs with higher university qualifications tended to align more with the literature, a trend consistent with previous investigations in Italy. PTs with post-graduate IFOMPT specialization degree showing significant agreement with evidence-based recommendations for most knowledge and management strategies. One possible explanation for this, is that such specialized courses are well-founded on evidence-based practice and adhere to international standards. [60]. This aligns with findings from other Italian surveys as well [26, 61]. Moreover, working in a direct access setting, managing multiple FS cases, or having 6 to 10 years of experience could imply greater knowledge, competence, and adherence to evidence-based clinical practice.
However, further prospective studies are needed to better evaluate these assumptions.
Study limitations
The main limitation of this study was the categorization of the patients managed by PTs, as the first category was set at “≤ 2”, which implicitly could include the possibility of managing no patients at all.
Moreover, this survey investigated the PTs’ clinical practice through a non-a-priori validated questionnaire, which could weaken the robustness of the results. However, this survey represents the first attempt to understand the preferences, beliefs, and clinical practice of PTs regarding FS, and it could serve as a baseline for future investigations.
Additionally, our survey mostly recruited young and less experienced PTs, and the total sample was less than 1% of the total Italian PTs (n = 69,848). These characteristics could further weaken our results. However, the present sample remains one of the largest samples recruited in musculoskeletal field surveys in Italy.
Lastly, the survey’s administration through electronic devices and social media might have excluded PTs who are not familiar with these means. However, in today’s context, these communication channels are widely used among healthcare professionals. It’s worth noting that the participation of PTs with post-graduate IFOMPT specialization degrees was limited, representing a minority within the entire national scenario.
Conclusion
This cross-sectional study highlights the preferences in clinical practices among Italian PTs for FS rehabilitation in comparison to evidence-based recommendations. Noteworthy, diagnostic imaging, clinical assessment, identification of predisposing factors, staging education, and mobilization modalities were areas where the PTs practice mostly diverged from the evidence’s suggestions. PTs with post-graduate IFOMPT specialization degrees, those with 6 to 10 years of clinical experience, and those working in private practice demonstrated greater appropriateness in terms of knowledge, competence, and adherence to evidence-based clinical practice.
Data availability
No datasets were generated or analysed during the current study.
References
Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Care Res (Hoboken). 2004;51:642–51.
Bunker TD. Frozen shoulder: unravelling the enigma. Ann R Coll Surg Engl. 1997;79:210–3.
Mertens MG, Meert L, Struyf F, Schwank A, Meeus M. Exercise Therapy is effective for improvement in range of motion, function, and Pain in patients with frozen shoulder: a systematic review and Meta-analysis. Arch Phys Med Rehabil. 2022;103:998–e101214.
Kelley MJ, et al. Shoulder Pain and mobility deficits: Adhesive Capsulitis. J Orthop Sports Phys Therapy. 2013;43:A1–31.
Millar NL et al. Frozen shoulder. Nat Rev Dis Primers 8, (2022).
Redler LH, Dennis ER. Treatment of Adhesive Capsulitis of the shoulder. J Am Acad Orthop Surg. 2019;27:e544–54.
Le HV, Lee SJ, Nazarian A, Rodriguez EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elb. 2017;9:75–84.
Kingston K, Curry EJ, Galvin JW, Li X. Shoulder adhesive capsulitis: epidemiology and predictors of surgery. J Shoulder Elb Surg. 2018;27:1437–43.
Akbar M, et al. Fibroblast activation and inflammation in frozen shoulder. PLoS ONE. 2019;14:e0215301.
Lewis J. Frozen shoulder contracture syndrome – aetiology, diagnosis and management. Man Ther. 2015;20:2–9.
Wang K, et al. Risk factors in idiopathic adhesive capsulitis: a case control study. J Shoulder Elb Surg. 2013;22:e24–9.
Page MJ, et al. Electrotherapy modalities for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Reviews. 2014. https://doi.org/10.1002/14651858.CD011324.
Kraal T, et al. The puzzling pathophysiology of frozen shoulders – a scoping review. J Exp Orthop. 2020;7:91.
Mertens MG, et al. An overview of effective and potential new conservative interventions in patients with frozen shoulder. Rheumatol Int. 2022;42:925–36.
Challoumas D, Biddle M, McLean M, Millar NL. Comparison of treatments for frozen shoulder: a systematic review and Meta-analysis. JAMA Netw Open 3, (2020).
Gleyze P, et al. Pain management in the rehabilitation of stiff shoulder: prospective multicenter comparative study of 193 cases. Orthop Traumatology: Surg Res. 2011;97:S195–203.
Jones S, Hanchard N, Hamilton S, Rangan A. A qualitative study of patients’ perceptions and priorities when living with primary frozen shoulder. BMJ Open. 2013;3:e003452.
Leventhal H, Phillips LA, Burns E. The common-sense model of self-regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. 2016;39:935–46.
Zavala-González J, Pavez-Baeza F, Gutiérrez-Espinoza H, Olguín-Huerta C. The effectiveness of joint mobilization techniques for range of motion in adult patients with primary adhesive capsulitis of the shoulder: a systematic review and meta-analysis. Medwave. 2018;18:e7265–7265.
Noten S, et al. Efficacy of different types of mobilization techniques in patients with primary Adhesive Capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016;97:815–25.
King WV, Hebron C. Frozen shoulder: living with uncertainty and being in no-man’s land. Physiother Theory Pract. 2022;1–15. https://doi.org/10.1080/09593985.2022.2032512.
Brindisino F, et al. Effectiveness of electrophysical agents in subjects with frozen shoulder: a systematic review and meta-analysis. Disabil Rehabil. 2023;1–22. https://doi.org/10.1080/09638288.2023.2251880.
Alsubheen SA et al. Effectiveness of Nonsurgical Interventions for Managing Adhesive Capsulitis in Patients With Diabetes: A Systematic Review. Archives of Physical Medicine and Rehabilitation vol. 100 350–365 Preprint at https://doi.org/10.1016/j.apmr.2018.08.181 (2019).
Hanchard NCA, et al. A questionnaire survey of UK physiotherapists on the diagnosis and management of contracted (frozen) shoulder. Physiotherapy. 2011;97:115–25.
Alhammadi MJ, Hegazy FA. Physiotherapists’ practice patterns for the diagnosis and management of patients with chronic contracted frozen shoulder in the United Arab Emirates. PLoS ONE. 2023;18:e0283255.
Brindisino F, et al. Subacromial impingement syndrome: a survey of Italian physiotherapists and orthopaedics on diagnostic strategies and management modalities. Arch Physiother. 2020;10:16.
Brindisino F, et al. Post-surgery rehabilitation following rotator cuff repair. A survey of current (2020) Italian clinical practice. Disabil Rehabil. 2022;44:4689–99.
Eysenbach. Checklist for Reporting Results of Internet E-Surveys (CHERRIES) Item Category Checklist Item Explanation Design. (2004).
von Elm E, et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Kong H, West S. WMA declaration of HELSINKI – ethical principles for scientific requirements and research protocols. Ferney-Voltaire, France: World Medical Association; 2013. pp. 29–32.
Bisconti M, Brindisino F, Maselli F. Gender medicine and physiotherapy: a need for education. Findings from an Italian National Survey. Healthcare. 2020;8:516.
Scalise V, Brindisino F, Pellicciari L, Minnucci S, Bonetti F. Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods. Int J Environ Res Public Health 18, 1995 (2021).
IFOMPT. OMPT definition. 2004. https://www.ifompt.org/About+IFOMPT/OMPT+Definition.html.
Lau C, et al. Facilitating Community-based Exercise for people with Stroke: cross-sectional e-Survey of physical therapist practice and perceived needs. Phys Ther. 2016;96:469–78.
Shelby J, Haberman. The analysis of residuals in Cross-classified Tables. Int Biometric Soc. 1973;29:205–20.
Beasley TM, Schumacker RE. Multiple regression Approach to analyzing contingency tables: Post Hoc and Planned Comparison procedures. J Experimental Educ. 1995;64:79–93.
García-pérez MA. Núñez-antón, V. Cellwise residual analysis in two-way contingency tables. Educ Psychol Meas. 2003;63:825–39.
Abrassart S, et al. Frozen shoulder’ is ill-defined. How can it be described better? EFORT Open Rev. 2020;5:273–9.
Brindisino F, et al. Does the psychological profile of a patient with frozen shoulder predict future outcome? A systematic review. Physiotherapy Res Int. 2023. https://doi.org/10.1002/pri.2056.
Lubis AMT, Lubis VK. Matrix metalloproteinase, tissue inhibitor of metalloproteinase and transforming growth factor-beta 1 in frozen shoulder, and their changes as response to intensive stretching and supervised neglect exercise. J Orthop Sci. 2013;18:519–27.
Donatelli R, Ruivo RM, Thurner M, Ibrahim MI. New concepts in restoring shoulder elevation in a stiff and painful shoulder patient. Phys Ther Sport. 2014;15:3–14.
Çelik D, Kaya Mutlu E. Does adding mobilization to stretching improve outcomes for people with frozen shoulder? A randomized controlled clinical trial. Clin Rehabil. 2016;30:786–94.
Lederman E. A process approach in osteopathy: beyond the structural model. Int J Osteopath Med. 2017;23:22–35.
Chaudhry H, et al. Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy. J Osteopath Med. 2008;108:379–90.
Wise SR, Seales P, Houser AP, Weber CB. Frozen shoulder: diagnosis and management. Curr Sports Med Rep. 2023;22:307–12.
Cho C-H, et al. Definition, diagnosis, treatment, and prognosis of frozen shoulder: a Consensus Survey of Shoulder specialists. Clin Orthop Surg. 2020;12:60.
Dimitriou D, et al. Is routine magnetic resonance imaging necessary in patients with clinically diagnosed frozen shoulder? Utility of magnetic resonance imaging in frozen shoulder. JSES Int. 2022;6:855–8.
Sharma SP, Bærheim A, Kvåle A. Passive range of motion in patients with adhesive shoulder capsulitis, an intertester reliability study over eight weeks. BMC Musculoskelet Disord. 2015;16:37.
Lee JC, Sykes C, Saifuddin A, Connell D. Adhesive capsulitis: sonographic changes in the rotator cuff interval with arthroscopic correlation. Skeletal Radiol. 2005;34:522–7.
Whittaker JL, et al. Rehabilitative Ultrasound Imaging: understanding the technology and its applications. J Orthop Sports Phys Therapy. 2007;37:434–49.
Giovannico G, et al. A description of physical therapists knowledge in basic competence examination of Musculo-skeletal conditions an Italian National Cross-sectional Survey. Muscle Ligaments Tendons J. 2020;10:686.
Wallden M, Chek P. The ghost in the machine – is musculoskeletal medicine lacking soul? J Bodyw Mov Ther. 2018;22:438–48.
van Smeden M, Reitsma JB, Riley RD, Collins GS, Moons KG. Clinical prediction models: diagnosis versus prognosis. J Clin Epidemiol. 2021;132:142–5.
Lyne SA, Goldblatt FM, Shanahan EM. Living with a frozen shoulder – a phenomenological inquiry. BMC Musculoskelet Disord. 2022;23:318.
Shoulder F. What can a physical therapist do for my painful and stiff shoulder? J Orthop Sports Phys Therapy. 2013;43:351–351.
Page MJ, et al. Patients’ experience of shoulder disorders: a systematic review of qualitative studies for the OMERACT Shoulder Core Domain Set. Rheumatology. 2019;58:1410–21.
Brindisino F, et al. Depression and anxiety are Associated with worse subjective and functional baseline scores in patients with frozen shoulder contracture syndrome: a systematic review. Arthrosc Sports Med Rehabil. 2022;4:e1219–34.
Casserley-Feeney SN, et al. Patient satisfaction with private physiotherapy for musculoskeletal Pain. BMC Musculoskelet Disord. 2008;9:50.
Hush JM, Cameron K, Mackey M. Patient satisfaction with Musculoskeletal Physical Therapy Care: a systematic review. Phys Ther. 2011;91:25–36.
Roberts S, et al. Routine X-rays for suspected frozen shoulder offer little over diagnosis based on history and clinical examination alone. Musculoskelet Care. 2019;17:288–92.
Brindisino F, Matteuzzi I, Bury J, McCreesh K, Littlewood C. Rotator cuff disorders: a survey of current (2018) Italian physiotherapy practice. Physiother Pract Res. 2020;41:11–22.
Acknowledgements
The authors want to thank all Italian physiotherapists that completed the survey.
Funding
This research received no specific grant from any funding agency in the public, commercial or non-profit sectors.
Author information
Authors and Affiliations
Contributions
Authors’ contributions: Concept / idea: FB, RA, DVResearch design: FB, RA, MCWriting: FB, RA, MC, GGir, AA, MSData collection: LP, GGio, FBData analysis: LP, GGio, MS, FBProject management: FB, MC, RA, DVConsultation (including review of manuscript before submitting): FB, GGir, MC, RA, AA, GGio, LP, MS, DVConsultation (including review of manuscript during peer review process): FB, GGir, MC, RA, AA, GGio, LP, MS, DVFinal approval of the Manuscript: FB, GGir, MC, RA, AA, GGio, LP, MS, DV.
Corresponding author
Ethics declarations
Ethical approval
was obtained from the Ethics Committee of University of Molise (Italy) with the registration number 11/2023. All the study-related procedures were performed according to the principles of the Declaration of Helsinki. Informed consent to participate was provided by all subjects included.
Permission to reproduce material from other sources
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflict of interests (i.e. actual or perceived conflict of interest).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brindisino, F., Girardi, G., Crestani, M. et al. Rehabilitation in subjects with frozen shoulder: a survey of current (2023) clinical practice of Italian physiotherapists. BMC Musculoskelet Disord 25, 573 (2024). https://doi.org/10.1186/s12891-024-07682-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07682-w