Abstract
Background
Periprosthetic joint infection (PJI) is a severe complication of joint arthroplasty that causes significant pain and economic loss. This study aimed to determine whether the current evidence supports single-stage revision for PJI based on reinfection and reoperation rates.
Methods
We searched the PubMed, EBSCO, Medline, and Cochrane Library databases from inception to 30 May 2023 to identify studies that compared single-stage revision and two-stage revision for PJI. Data on reinfection and reoperation rates were pooled.
Results
This meta-analysis included a total of 40 studies with 8711 patients. Overall, there was no significant difference between single- and two-stage revision regarding the postoperative reinfection rate and reoperation rate. Subgroup analysis by surgery period and different surgical sites revealed no difference between the two groups in the reinfection and reoperation rates.
Conclusions
Based on the available evidence, our study did not identify a significant difference in reinfection and reoperation rates between single- and two-stage revision for PJI. Given the limitations in inclusion/exclusion criteria and the observed heterogeneity, we acknowledge the complexity of drawing strong conclusions. Therefore, we suggest that the choice between single- and two-stage revision should be carefully considered on an individual basis, taking into account patient-specific factors and further research developments.
Similar content being viewed by others
Background
As a terminal means for treating osteoarthritis, joint arthroplasty can effectively reduce pain and improve quality of life. However, periprosthetic joint infection (PJI) is a severe complication of joint arthroplasty that causes significant pain and economic loss. It is expected that 10,000 patients with PJI will require revision each year by 2030 [1]. In recent years, improvements in surgical techniques and surgical conditions have led to a decline in the incidence of PJI from 1%–23% to 1%–2% [2]. With improvements in economic conditions and people's quality of life requirements, the total number of arthroplasty procedures have increased rapidly, and the number of PJIs has increased accordingly. Two-stage revision is considered the gold standard for treating PJI [3, 4]. However, the ideal time interval between surgical treatments, optimal antimicrobial agent, and duration of treatment remains controversial and the reported postoperative infection recurrence rate varies widely. In addition, some patients are in poor physical condition and may not be able to tolerate a second surgery. In recent years, the single-stage revision technique has received widespread attention and its application is increasing worldwide. Compared with two-stage revision, single-stage revision is more conducive to the functional recovery of the affected limb, reduces the occurrence of complications, reduces the overall treatment cost, reduces the surgical trauma, and improves patient satisfaction [5,6,7]. Moreover, several studies have reported comparable success with single-stage revision versus two-stage revision [6, 8, 9]. However, the evidence regarding single- and two-stage revision for PJI is inconsistent. This meta-analysis aimed to determine whether the reinfection and reoperation rates differ between the two treatment modalities and to ultimately reduce uncertainty in clinical decision-making for PJI treatment.
Methods
According to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement, this meta-analysis was performed in agreement [10]. The protocol for this meta-analysis was registered on PROSPERO (Registration No: CRD 42022369943).
Inclusion criteria
Study type: randomized controlled trial, cohort study, or retrospective study (Level I to III evidence). Study population: patients undergoing PJI. Intervention and control: single-stage in the treatment group, two-stage in the control group. Outcome index: clear reinfection or reoperation reported. Reinfection can be defined as the recurrence of clinical, serologic, or radiographic signs of infection during the follow-up period after the initial infection has been controlled. Reoperation can be defined as the patients need for further revision surgery.
Exclusion criteria
Letters, case reports, reviews, animal trials, or republished studies; Studies lacking a control group; Patients with septic arthritis or tuberculous arthritis.
Search strategy
Two of the authors (YZ and HL) performed the search in PubMed, EBSCO, Medline, and the Cochrane Central Register of Controlled Trials from the inception dates to May 30, 2023, using the keywords “(Two-stage or 2-stage or two stage or second-stage or double-stage) and (Single-stage or one-stage or 1-stage) and (arthroplasty or replacement) and (unhealed or infection or reoperate* or revise)”. No language restrictions were applied during the search.
Study selection
Two researchers (YZ and ZFW) screened the retrieved literature strictly and individually against inclusion and exclusion criteria. If two researchers do not agree during the literature screening process, it will be left to the senior researcher (HL).
Data collection process
Data on relevant outcome measures were extracted from the literature that met the inclusion criteria, including first author, year of publication, number of patients included, population characteristics (age, gender, comorbidities, etc), study design, PJI definition criteria, used, joint, surgical strategy, definition of failure (reoperation for infection, DAIR (debridement, antibiotic and implant retention), suppressive antibiotics), reason for reoperation other than infection and timming, follow-up by two researchers (SHF and HL) individually.
Outcomes
The primary outcome was the incidence of reinfection. A secondary outcome was the incidence of reoperation.
Assessment of risk of bias and quality of evidence
Two researchers (HL and SHF) independently assessed the quality of all included trials based on Cochrane risk-of-bias criteria [11]. The Newcastle–Ottawa scale (NOS) was used to evaluate the literature quality of the retrospective studies [12].
Data synthesis
The Meta-analysis was performed using Stata (version 17; StataCorp, 2021) software. The heterogeneity was assessed by using the Q test and I2 value calculation. Suppose the heterogeneity was not present (P>0.1 and I2<50%), the data was combined with a fixed effect model. The random effects model was used if heterogeneity was present (P<0.1 or I2 >50%). The odds ratio (OR) and their associated 95% confidence interval (CI) were used to assess outcomes, and a P value less than 0.05 suggested that the difference was statistically significant.
Subgroup analyses
We performed subgroup analyses for different surgical areas and periods of surgery.
Sensitivity analyses
We performed a sensitivity analysis on a case-by-case exclusion basis using random effect models.
Results
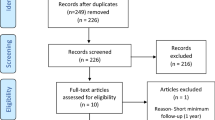
A total of 1663 documents were retrieved, 1012 duplicate documents were eliminated, the remaining 651 documents were read for abstracts and titles, 594 irrelevant documents were excluded, and 1 document failed to obtain the full text. The remaining 56 articles were read in full text. Fifteen studies were excluded, of which one review study, five case reports, three outcomes were no recurrence of infection, and six participants were without PJI. A total of 41 studies were included in the systematic review [5,6,7,8,9, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], of which one study was excluded from the meta-analysis as the reinfection or reoperation outcomes could not be extracted [26]. A total of 40 articles were included in the meta-analysis (Fig. 1). The characteristics of the included studies are detailed in Table 1.
A total of 41 retrospective studies were included in our systematic review. We used the NOS to assess the methodological quality and risk of bias. The quality scores were 6 to 9, indicating an overall low risk of bias (Table 1).
Reinfection
A total of 37 studies reported the recurrence of infection [6, 8, 9, 13,14,15,16,17,18,19,20, 22,23,24,25, 27,28,29,30,31,32,33,34,35,36, 38,39,40,41,42,43,44,45,46,47,48,49]. Van den Kieboom et al. [44] included both superficial and deep infections. We did not exclude superficial infections as these may result in deep infections. Among the cohort evaluated by Larsson et al., [30] we excluded one patient in the single-stage group who experienced treatment failure because the appropriate criteria were not met. There was mild heterogeneity between studies (I2=24.3%, P=0.106), and a fixed-effect model was used. There was no difference in the reinfection rate after single- versus two-stage revision for PJI (OR: 0.88; 95% CI: 0.73–1.07; P=0.209; Fig. S1A). As different surgical sites and surgery periods may have been a source of heterogeneity, subgroup analyses were performed. There was no difference in the reinfection rate between the single- and two-stage groups among the subgroups with PJI of the hip (OR: 1.35; 95% CI: 0.66–2.76; P=0.410; I2=53.5%; Fig. S1B), knee (OR: 0.76; 95% CI: 0.58–1.00; P=0.052; I2=0%; Fig. S1B), or shoulder (OR: 0.55; 95% CI: 0.16–1.88; P=0.338; I2=0%; Fig. S1B). Subgroup analysis based on the surgery period showed no significant difference in the reinfection rate between the single- and two-stage groups that underwent surgery after 2005 (OR: 0.79; 95% CI: 0.58–1.08; P=0.142; I2=0%; Fig. 2C), during both surgery periods (OR: 0.78; 95% CI: 0.58–1.07; P=0.125; I2=0%; Fig. S1C), or before 2005 (OR: 2.69; 95% CI: 0.58–12.37; P=0.204; I2=60.6 %; Fig. S1C).
Reoperation
A total of 18 studies reported the number of reoperations [5, 7,8,9, 16, 21,22,23, 33, 35, 36, 38,39,40,41,42,43,44]. There was no significant difference in the reoperation rate between the single- and two-stage groups (OR: 1.04; 95% CI: 0.79–1.37; P=0.792; I2=52.2 %; Fig. S2A). Considering the heterogeneity of the results, subgroup analyses were performed for different surgical sites and surgery periods. Subgroup analyses showed no difference in the reoperation rate after single-stage revision versus two-stage revision for PJI of the hip (OR: 1.49; 95% CI: 0.77–2.89; P=0.239; I2=76.6%; Fig. S2B), knee (OR: 0.93; 95% CI: 0.74–1.16; P=0.509; I2=2.6%; Fig. S2B), or shoulder (OR: 1.10; 95% CI: 0.31–3.75; P=0.880; Fig. S2B). Subgroup analysis based on the surgery period showed no difference in the reoperation rate between the single- and two-stage groups that underwent surgery after 2005 (OR: 0.77; 95% CI: 0.55–1.08; P=0.129; I2=0%; Fig. S2C) or during both surgery periods (OR: 1.23 95% CI: 0.82–1.83; P=0.316; I2=69.2%; Fig. S2C). Only one study that reported reoperation data was performed before 2005, and statistical calculations could not be performed because the number of events in both groups was 0.
Sensitivity analysis
A sensitivity analysis of the included studies was performed on a case-by-case exclusion basis. The remaining studies were combined using the OR values if any study was excluded. No individual study had a significant impact on the results (Fig. S3A and B).
Risk of bias
As shown in Fig. 2, the funnel plots showed some asymmetry, but the Harbord test showed no evidence of publication bias regarding reinfection (P=0.537) and reoperation (P=0.322).
Discussion
Several systematic reviews and meta-analyses have explored reinfection rates after single- or two-stage revision, but the two treatment protocols were not compared and the studies were limited to a single surgical site analysis [49,50,51,52,53,54,55,56]. Nagra et al. [57] published a meta-analysis of the two treatment options in 2016, but included only five retrospective studies comparing 796 patients with PJI of the knee. Since the publication of the meta-analysis by Nagra et al., [57] there has been a significant increase in studies reporting reinfection rates after single-stage revision for PJI of the knee. Therefore, we searched the literature for relevant studies and included studies evaluating the treatment of knee, hip, and shoulder PJI to determine whether the reinfection and reoperation rates differed between the single- and two-stage revision groups.
Our study found no difference in the reinfection and reoperation rates between the single-and two-stage groups. The decision whether to perform a single or two-stage revision is made at the discretion of the surgeon after considering all the details of the patient and the surgical site; therefore, there was some allocation bias that led to this result. In addition, for patients with hip and shoulder PJI, only part of the prosthesis may be revised [21, 40], leading to incomplete debridement and an increased reinfection rate after single-stage revision. The reoperation rate did not differ between the single-stage and two-stage groups for different surgical sites. As the data collected for the current analysis spanned a long period from 1969 to 2019, which may constitute a potential confounding source for our analysis, we performed subgroup analyses of surgery periods. These subgroup analyses showed no significant differences in the rates of reinfection and reoperation between the two groups. Svensson et al. [41] defined reinfection as the need for reoperation due to reinfection. However, some patients may have had secondary infections that resolved with medication and did not require a second revision surgery. This may have led to increased reporting bias.
Although two-stage revision has traditionally been considered the gold standard for treating PJI [58], it significantly reduces patient activity time to a total of approximately twice as long as single-stage revision. Removal of a well-immobilized prosthesis may also lead to degeneration of bone stock and perioperative fractures [21]. Single-stage revision offers advantages such as a similar failure rate as a two-stage replacement, reduced hospitalization and costs, and improved cost-effectiveness [58, 59]. Our findings suggest that there was no difference between single- and two-stage revision in the rates of reinfection and reoperation. Studies have found that the risk factors for failure of single-stage revision may be related to prior joint infection with Enterococcus or Streptococcus species [60], so it may be interesting to compare the outcomes of single-stage revision to treat PJI caused by these two bacterial species. Moreover, different studies have used different surgical procedures and methods for the criteria for single- versus two-stage revision, and there is no regulation of the use of antibiotics. The present study focused on whether single-stage revision can achieve the same treatment effect as two-stage revision while reducing the surgery time, pain, and cost. Therefore, more comparisons of antibiotics and optimization of surgical procedures need to be performed to provide a basis for formulating relevant guidelines.
Strengths
This is the first comprehensive comparison of the efficacy of single- and two-stage revision for PJI. This meta-analysis pooled 40 published studies involving 8711 patients with PJI, which may improve the statistical power of the data analysis and thus provide more reliable estimates. Sources of heterogeneity were analyzed, and subgroup analyses were performed for different surgical sites and periods of surgery. Our results showed that the success rate of single-stage revision was comparable to that of two-stage revision, challenging the assumption that two-stage revision is the gold standard for PJI. Clinicians are encouraged to consider single-stage revision for eligible patients with PJI. Compared with studies within a single country, our study pooled relative data from multiple countries worldwide, enhancing the universal applicability of the findings. Based on the Harbord tests and funnel plots, there was no significant publication bias in the included studies. Therefore, the results based on the available evidence are compelling.
Limitations
This study has several limitations. First, the most significant limitation of our article is that the included studies were all non-randomized controlled studies. The allocation of patients was not based on randomization but rather on the surgeons' experience, resulting in a preference for two-stage revision in patients with contraindications to single-stage revision or those with severe joint infection [9, 28], leading to allocation bias. Therefore, the confidence of the results needs to be further confirmed by randomized controlled trials. Second, the definition of reinfection after revision differed between studies. Castellani et al. [15] defined the outcome as a failure without stating the rates of reinfection or revision. Thus, we could only judge whether patients had reinfection based on the description of the definition in the complete text, and discussed each patient to decide whether to include them in the group with reinfection, which may have deviated from the authors’ original definition [15]. Third, Kheir, [27] Mahieu et al., [35] and Van den Kieboom et al. [44] studied patients with specific bacterial infections or those with negative bacterial cultures, which increased the bias of the results. Fourth, the present review included studies with follow-up periods ranging from 6 months to 22 years. Some studies had a very long follow-up, and the reason for reoperation was independent of the surgical modalities; in other studies, the follow-up time needed to be longer, resulting in missing outcome measures. Fifth, when we performed statistical calculations, we did not adjust the original data in accordance with confounding factors but simply combined the original data statistically, which increased the bias of the article. Sixth, in the studies we included, both partial and complete implant removal were incorporated, to some extent, increasing the heterogeneity of the article.
Conclusions
To our knowledge, this is the first meta-analysis to summarize the current evidence about the differences between single- and two-stage revision in treating PJI. We found that there was no difference between single- and two-stage revision in the reinfection and reoperation rates. Recognizing constraints in our inclusion/exclusion criteria and the observed diversity, we acknowledge the challenge of making definitive conclusions. Hence, we recommend a thoughtful, case-by-case consideration of the choice between single- and two-stage revision, considering patient-specific factors and staying attuned to ongoing research advancements.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PJI:
-
Periprosthetic joint infection
- OR:
-
odds ratio
- CI:
-
confidence interval
References
Kildow BJ, Della-Valle CJ, Springer BD. Single vs 2-stage revision for the treatment of periprosthetic joint infection. J Arthroplasty. 2020;35(3s):S24–s30.
Finley R, Glass-Kaastra SK, Hutchinson J, Patrick DM, Weiss K, Conly J. Declines in outpatient antimicrobial use in Canada (1995–2010). PLoS One. 2013;8(10):e76398.
Anagnostakos K, Kelm J, Schmitt E, Jung J. Fungal periprosthetic hip and knee joint infections clinical experience with a 2-stage treatment protocol. J Arthroplasty. 2012;27(2):293–8.
Lazic I, Scheele C, Pohlig F, von Eisenhart-Rothe R, Suren C. Treatment options in PJI - is two-stage still gold standard? J Orthop. 2021;23:180–4.
Baker P, Petheram TG, Kurtz S, Konttinen YT, Gregg P, Deehan D. Patient reported outcome measures after revision of the infected TKR: comparison of single versus two-stage revision. Knee Surg Sports Traumatol Arthrosc. 2013;21(12):2713–20.
Ribes C, Masquefa T, Dutronc H, De Seynes C, Dupon M, Fabre T, et al. One-stage versus two-stage prosthesis replacement for prosthetic knee infections. Med Mal Infect. 2019;49(7):519–26.
Lenguerrand E, Whitehouse MR, Kunutsor SK, Beswick AD, Baker RP, Rolfson O, et al. Mortality and re-revision following single-stage and two-stage revision surgery for the management of infected primary knee arthroplasty in England and Wales : evidence from the National Joint Registry. Bone Joint Res. 2022;11(10):690–9.
Matar HE, Bloch BV, Snape SE, James PJ. Outcomes of single- and two-stage revision total knee arthroplasty for chronic periprosthetic joint infection : long-term outcomes of changing clinical practice in a specialist centre. Bone Joint J. 2021;103-b(8):1373–9.
Klemt C, Tirumala V, Oganesyan R, Xiong L, van den Kieboom J, Kwon YM. Single-stage revision of the infected total knee arthroplasty is associated with improved functional outcomes: a propensity score-matched cohort study. J Arthroplasty. 2021;36(1):298–304.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142.
Wells G, Shea B, O'Connell J. The Newcastle-Ottawa Scale (NOS) for Assessing The Quality of Nonrandomised Studies in Meta-analyses. Ottawa Health Research Institute Web site. 2014;7.
Bauer T, Piriou P, Lhotellier L, Leclerc P, Mamoudy P, Lortat-Jacob A. Results of reimplantation for infected total knee arthroplasty: 107 cases. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(7):692–700.
Betsch BY, Eggli S, Siebenrock KA, Täuber MG, Kathrin M. Treatment of joint prosthesis infection in accordance with current recommendations improves outcome. Clin Infect Dis. 2008;46(8):1221–6.
Castellani L, Daneman N, Mubareka S, Jenkinson R. Factors associated with choice and success of one- versus two-stage revision arthroplasty for infected hip and knee prostheses. Hss J. 2017;13(3):224–31.
Chalmers BP, Kapadia M, Chiu Y-F, Henry MW, Miller AO, Carli AV. Treatment and outcome of periprosthetic joint infection in unicompartmental knee arthroplasty. J Arthroplasty. 2020;35(7):1917–23.
Choi HR, Kwon YM, Freiberg AA, Malchau H. Comparison of one-stage revision with antibiotic cement versus two-stage revision results for infected total hip arthroplasty. J Arthroplasty. 2013;28(8 Suppl):66–70.
Crego-Vita D, Sánchez-Pérez C, Espigares-Correa A, Aedo-Martín D. Total knee arthroplasty infection, what is the best strategy for better functional outcomes? Acta Ortop Mex. 2019;33(5):297–302.
Cristea Ş, Cristea C, Banibache L, Panait G, Popescu MV, Antonescu DM, et al. Artroplastia totală de şold ăi de genunchi supurată – tratament. Rom J Infect Dis. 2007;10(3):86–92.
Cury RD, Cinagawa EH, Camargo OP, Honda EK, Klautau GB, Salles MJ. Treatment of infection after total knee arthroplasty. Acta Ortopédica Brasileira. 2015;23(5):239–43.
Engesater LB, Dale H, Schrama JC, Hallan G, Lie SA. Surgical procedures in the treatment of 784 infected THAs reported to the Norwegian Arthroplasty Register. Acta Orthop. 2011;82(5):530–7.
Gao H, Lv H. One-stage revision operations for infection after hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22(1):5–8.
Haddad F, Sukeik M, Alazzawi S. Is single-stage revision according to a strict protocol effective in treatment of chronic knee arthroplasty infections? Clin Orthop Relat Res. 2015;473(1):8–14.
Hope PG, Kristinsson KG, Norman P, Elson RA. Deep infection of cemented total hip arthroplasties caused by coagulase-negative staphylococci. J Bone Joint Surg Br. 1989;71(5):851–5.
Jacquot A, Sirveaux F, Roche O, Favard L, Clavert P, Molé D. Surgical management of the infected reversed shoulder arthroplasty: a French multicenter study of reoperation in 32 patients. J Shoulder Elbow Surg. 2015;24(11):1713–22.
Kandel CE, Jenkinson R, Daneman N, Backstein D, Hansen BE, Muller MP, et al. Predictors of treatment failure for hip and knee prosthetic joint infections in the setting of 1- and 2-stage exchange arthroplasty: a multicenter retrospective cohort. Open Forum Infect Dis. 2019;6(11):ofz452.
Kheir MM, Tan TL, Higuera C, George J, Della Valle CJ, Shen M, et al. Periprosthetic joint infections caused by enterococci have poor outcomes. J Arthroplasty. 2017;32(3):933–47.
Klouche S, Leonard P, Zeller V, Lhotellier L, Graff W, Leclerc P, et al. Infected total hip arthroplasty revision: one- or two-stage procedure? Orthop Traumatol Surg Res. 2012;98(2):144–50.
Laffer RR, Graber P, Ochsner PE, Zimmerli W. Outcome of prosthetic knee-associated infection: evaluation of 40 consecutive episodes at a single centre. Clin Microbiol Infect. 2006;12(5):433–9.
Larsson P, Erschbamer M, Spross C, Grob K, Jost B, Erhardt J. Evaluation of ninety-six periprosthetic hip joint infections seen within five consecutive years. Acta Orthop Belg. 2018;84(3):298–306.
Lecuire F, Collodel M, Basso M, Rubini J, Gontier D, Carrère J. [Revision of infected total hip prostheses by ablation reimplantation of an uncemented prosthesis. 57 case reports]. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(4):337–48.
Lemmens L, Geelen H, Depypere M, De Munter P, Verhaegen F, Zimmerli W, et al. Management of periprosthetic infection after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30(11):2514–22.
Leta TH, Lygre SHL, Schrama JC, Hallan G, Gjertsen J-E, Dale H, et al. Outcome of revision surgery for infection after total knee arthroplasty: results of 3 surgical strategies. JBJS Rev. 2019;7(6):e4.
Li H, Ni M, Li X, Zhang Q, Li X, Chen J. Two-stage revisions for culture-negative infected total knee arthroplasties: a five-year outcome in comparison with one-stage and two-stage revisions for culture-positive cases. J Orthop Sci. 2017;22(2):306–12.
Mahieu R, Dubee V, Seegers V, Lemarie C, Ansart S, Bernard L, et al. The prognosis of streptococcal prosthetic bone and joint infections depends on surgical management-A multicenter retrospective study. Int J Infect Dis. 2019;85:175–81.
Massin P, Delory T, Lhotellier L, Pasquier G, Roche O, Cazenave A, et al. Infection recurrence factors in one- and two-stage total knee prosthesis exchanges. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3131–9.
Ritter MA, Farris A. Outcome of infected total joint replacement. Orthopedics. 2010;33(3).
Siddiqi A, Nace J, George NE, Buxbaum EJ, Ong AC, Orozco FR, et al. Primary total knee arthroplasty implants as functional prosthetic spacers for definitive management of periprosthetic joint infection: a multicenter study. J Arthroplasty. 2019;34(12):3040–7.
Sotiriou D, Stigbrand H, Ullmark G. Is two-stage revision surgery for infected hip arthroplasty worth the suffering, resources and results compared to one-stage? Hip Int. 2022;32(2):205–12.
Stone GP, Clark RE, O’Brien KC, Vaccaro L, Simon P, Lorenzetti AJ, et al. Surgical management of periprosthetic shoulder infections. J Shoulder Elbow Surg. 2017;26(7):1222–9.
Svensson K, Rolfson O, Kärrholm J, Mohaddes M. Similar risk of re-revision in patients after one- or two-stage surgical revision of infected total hip arthroplasty: an analysis of revisions in the swedish hip arthroplasty register 1979–2015. J Clin Med. 2019;8(4):485.
Tirumala V, Klemt C, van den Kieboom J, Xiong L, Kwon YM. Comparison of patient reported outcome measures after single versus two-stage revision for chronic infection of total hip arthroplasty: a retrospective propensity score matched cohort study. Arch Orthop Trauma Surg. 2021;141(10):1789–96.
Tuecking L-R, Silligmann J, Savov P, Omar M, Windhagen H, Ettinger M. Detailed revision risk analysis after single- vs. two-stage revision total knee arthroplasty in periprosthetic joint infection: a retrospective tertiary center analysis. Antibiotics (Basel, Switzerland). 2021;10(10):1177.
van den Kieboom J, Tirumala V, Box H, Oganesyan R, Klemt C, Kwon YM. One-stage revision is as effective as two-stage revision for chronic culture-negative periprosthetic joint infection after total hip and knee arthroplasty. Bone Joint J. 2021;103-b(3):515–21.
Van Dijk B, Nurmohamed F, Hooning van Duijvenbode JFF, Veltman ES, Rentenaar RJ, Weinans H, et al. A mean 4-year evaluation of infection control rates of hip and knee prosthetic joint infection-related revision arthroplasty: an observational study. Acta Orthop. 2022;93:652–7.
Wolf M, Clar H, Friesenbichler J, Schwantzer G, Bernhardt G, Gruber G, et al. Prosthetic joint infection following total hip replacement: results of one-stage versus two-stage exchange. Int Orthop. 2014;38(7):1363–8.
Wouthuyzen-Bakker M, Sebillotte M, Lomas J, Kendrick B, Palomares EB, Murillo O, et al. Timing of implant-removal in late acute periprosthetic joint infection: a multicenter observational study. J Infect. 2019;79(3):199–205.
Xu Z, Huang C, Lin Y, Chen Y, Fang X, Huang Z, et al. Clinical outcomes of culture-negative and culture-positive periprosthetic joint infection: similar success rate. Different Incidence of Complications. Orthop Surg. 2022;14(7):1420–7.
Goud AL, Harlianto NI, Ezzafzafi S, Veltman ES, Bekkers JEJ, van der Wal BCH. Reinfection rates after one- and two-stage revision surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2021.
Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD. Re-infection outcomes following one- and two-stage surgical revision of infected hip prosthesis: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0139166.
Kunutsor SK, Whitehouse MR, Blom AW, Board T, Kay P, Wroblewski BM, et al. One- and two-stage surgical revision of peri-prosthetic joint infection of the hip: a pooled individual participant data analysis of 44 cohort studies. Eur J Epidemiol. 2018;33(10):933–46.
Kunutsor SK, Whitehouse MR, Lenguerrand E, Blom AW, Beswick AD. Re-infection outcomes following one- and two-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS One. 2016;11(3):e0151537.
Kunutsor SK, Whitehouse MR, Webb J, Toms A, Stockley I, Taylor A, et al. Re-infection outcomes following one- and two-stage surgical revision of infected hip prosthesis in unselected patients: protocol for a systematic review and an individual participant data meta-analysis. Syst Rev. 2015;4:58.
Kunutsor SK, Wylde V, Beswick AD, Whitehouse MR, Blom AW. One- and two-stage surgical revision of infected shoulder prostheses following arthroplasty surgery: a systematic review and meta-analysis. Sci Rep. 2019;9(1):232.
Lange J, Troelsen A, Thomsen RW, Søballe K. Chronic infections in hip arthroplasties: comparing risk of reinfection following one-stage and two-stage revision: a systematic review and meta-analysis. Clin Epidemiol. 2012;4:57–73.
Marcheggiani Muccioli GM, Huri G, Grassi A, Roberti di Sarsina T, Carbone G, Guerra E, et al. Surgical treat GM, Huri G, Grassi A, Roberti di Sarsina T, Carbone G, Guerra E, et al. Surgical treatment of infected shoulder arthroplasty. a systematic review. Int Orthop. 2017;41(4):823–30.
Nagra NS, Hamilton TW, Ganatra S, Murray DW, Pandit H. One-stage versus two-stage exchange arthroplasty for infected total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3106–14.
Siddiqi A, George NE, White PB, Szczech BW, Thompson JV, Etcheson JI, et al. Articulating spacers as a modified one-stage revision total knee arthroplasty: a preliminary analysis. Surg Technol Int. 2018;32:239–48.
Okafor CE, Nghiem S, Byrnes J. Is 2-stage septic revision worth the money? a cost-utility analysis of a 1-stage versus 2-stage septic revision of total knee arthroplasty. Journal of. 2022.
Citak M, Friedenstab J, Abdelaziz H, Suero EM, Zahar A, Salber J, et al. Risk factors for failure after 1-stage exchange total knee arthroplasty in the management of periprosthetic joint infection. J Bone Joint Surg Am. 2019;101(12):1061–9.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
HL and YZ conceptualized the study; HL, YZ, ZW and SF performed the selection, data extraction, and risk of bias assessment; HL performed the statistical analysis and drafted the manuscript; XY and YZ provided critical appraisal of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 2: Figure S1.
Reinfection rate in included studies (A) Subgroup analysis of the reinfection according to different surgical sites (B) and surgery periods (C)
Additional file 2: Figure S2.
Reoperation rate in included studies (A) Subgroup analysis of the reoperation according to different surgical sites (B) and surgery periods (C)
Additional file 2: Figure S3.
The result of sensitivity analysis of reinfection (A) and reoperation (B)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, Y., Fan, S., Wang, Z. et al. Systematic review and meta-analysis of single-stage vs two-stage revision for periprosthetic joint infection: a call for a prospective randomized trial. BMC Musculoskelet Disord 25, 153 (2024). https://doi.org/10.1186/s12891-024-07229-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07229-z