Abstract
Background
This meta-analysis compares the efficacy of unilateral biportal endoscopic transforaminal lumbar interbody fusion (UBE-TLIF) to conventional interbody fusion in lumbar degenerative diseases (LDD).
Methods
An extensive literature search was conducted in PubMed, Web of Science, and the Cochrane Library. Research related to UBE-TLIF published up to November 2022 was reviewed. The relevant articles were selected based on inclusion and exclusion criteria, as well as an evaluation of the quality of the data extraction literature. Meta-analysis was performed using Review Manager 5.3 software.
Results
This meta-analysis included six high-quality case–control trials (CCTs) involving 621 subjects. The clinical outcomes assessment showed no statistical differences in complication rates, fusion rates, leg pain VAS scores, or ODI scores. After UBE-TLIF, low back pain VAS scores were significantly improved with less intraoperative blood loss and a shorter hospital stay. A longer time was required for UBE-TLIF, however.
Conclusion
Despite the lack of sufficient high quality randomized controlled trials (RCTs) in this study, the results of this meta-analysis suggest that UBE-TLIF is more effective than open surgery in terms of length of stay, blood loss reduction during surgery, and improved low back pain after surgery. Nevertheless, the evidence will be supplemented in the future by more and better quality multicenter randomized controlled trials.
Similar content being viewed by others
Introduction
Lumbar degenerative disease (LDD) is common, often necessitating surgical intervention when conservative treatment fails [1,2,3]. Lumbar fusion surgery effectively addresses LDD by stabilizing spinal segments, restoring intervertebral disc height, relieving nerve root compression, and ensuring spinal stability [4, 5]. However, conventional open surgery presents challenges, including significant trauma, potential muscle atrophy, chronic low back pain, and adjacent segment instability. As a result, spinal surgeons have shifted their focus to minimizing surgical trauma and promoting a speedy recovery, leading to an increase in the adoption of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) [6,7,8]. Nevertheless, this technique is constrained by limited operating space and a steep learning curve [9,10,11]. In recent years, unilateral biportal endoscopy (UBE) has emerged as a new minimally invasive spine technique. A variety of lumbar diseases have been successfully treated with UBE technology in related studies. UBE is effectively employed in addressing various lumbar spine conditions, including intervertebral disc herniation, spinal canal or intervertebral foramen stenosis decompression, and intradural cyst treatment, yielding favorable outcomes [12,13,14].
Heo et al. [15] reported successful cases of UBE for lumbar interbody fusion in 2017. However, uncertainties remain about the efficacy of UBE-TLIF compared to open surgery (MIS-TLIF/PLIF/TLIF). This study utilizes meta-analysis to assess the early clinical outcomes of various surgical approaches for treating lumbar degenerative diseases. The aim is to offer a more systematic and comprehensive evidence-based foundation for the clinical implementation of UBE-TLIF technology.
Materials and methods
Retrieval strategy
This study compared UBE-TLIF and open surgery for lumbar degenerative disease using both randomized controlled trials (RCTs) and case–control trials (CCTs). PubMed, Web of Science, and Cochrane Library databases were searched from January 2013 to November 2022, and only English articles were included. The search terms used were “biportal”, “endoscopic”, “fusion”, “interbody fusion”, and “lumbar”. To screen high-quality relevant articles, the retrieval strategy combines subject terms with free words. As each article describes “lumbar degenerative disease” differently, this is not a limitation for extending the scope of the search.
Inclusion and exclusion criteria
Inclusion criteria: 1) Studies comparing unilateral biportal endoscopic lumbar interbody fusion and open lumbar fusion; 2) Study types included RCTs or CCTs with a minimum follow-up period of 6 months; 3) Patients of both genders diagnosed with single-segment lumbar degenerative disease based on physical examinations and imaging data (age ≥ 18 years); 4) Included studies should provide comprehensive data and include at least three of the evaluation indicators.
Exclusion criteria 1) studies without a control group; 2) studies with less than six months of follow-up; 3) studies lacking relevant data; 4) repetitive reports; 5) case reports, cadaver studies, expert opinions, technical reports, and reviews.
Data selection
Two authors extracted data using standard extraction tables, and a third author summarized and reviewed. The data encompassed demographic characteristics, surgical information, and primary and secondary outcomes. Primary outcomes included Oswestry disability index (ODI) and visual analogue scale (VAS). Secondary outcomes included length of hospital stay, operative time, intraoperative blood loss, fusion rate, and complications. MIS-TLIF, TLIF, and PLIF were categorized under open surgery groups.
Quality evaluation
Two authors conducted the screening based on the previously described inclusion and exclusion criteria. Methodological quality and bias risk for randomized controlled trials were assessed using the Cochrane Risk of Bias criteria [16]. Cohort studies were evaluated using the Newcastle–Ottawa Scale (NOS) [17]. Studies were scored based on population selection, comparability between groups, and outcomes, with higher scores indicating better study quality. Overall, studies were ultimately categorized as high quality (5–9 points) or low quality (0–4 points).
Statistical analysis
ReviewManager5.3 statistical software (provided by the Cochrane collaboration network) was used for Meta analysis. Dichotomous variables were presented as odds ratios (OR), while continuous variables were expressed as weighted mean differences (WMDs) with 95% confidence intervals. Heterogeneity among study results was assessed using the I2 test, with a significance level set at α = 0.1. If P ≥ 0.1 or I2 ≤ 50%, homogeneity between studies existed and a fixed-effects model was used. Conversely, if P < 0.1 or I2 > 50%, the extracted data were highly heterogeneous, and sensitivity analysis was performed in order to identify the source of heterogeneity, followed by subgroup analysis. When the source of heterogeneity remains elusive, a random effects model will be employed.
Result
Search results and quality analysis
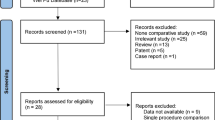
Figure 1 illustrates the PRISMA evaluation procedure. Initially, 468 articles were identified through search terms, titles, and abstracts. After excluding 437 case reports, duplicate studies, or reviews, 31 articles remained that met the inclusion criteria. In the end, only six articles [18,19,20,21,22,23] were included in the meta-analysis. All studies achieved a NOS score > 5, indicating high-quality literature (Table 1).
Demographic characteristics
The selected studies were all published between 2019 and 2022, and the pertinent demographic characteristics are detailed in Table 2. A total of 581 patients were enrolled, including 272 UBE-TLIF patients, 151 MIS-TLIF patients, and 158 PLIF/TLIF patients. In the included trials, five UBE-TLIF comparisons with MIS-TLIF and four UBE-TLIF comparisons with PLIF/TLIF were performed. The mean age of patients receiving UBE-TLIF and open surgery was 63.72 years and 62.42 years, respectively.
Primary outcome
Pain outcomes
Pain outcomes, assessed using VAS scores, were reported in four CCTs [19, 21,22,23], including UBE-TLIF (n = 143) and open surgery (n = 204). There was no statistical heterogeneity in the preoperative back VAS scores between the UBE-TLIF and open surgery groups (P = 0.11, I2 = 54%). According to the meta-analysis, there was no statistically significant difference in preoperative back VAS scores between the two groups (WMD = 0.12, 95% CI: -0.43 to 0.68, P = 0.66; Fig. 2A). However, the early postoperative back VAS score for the UBE-TLIF group was significantly lower than for the open surgery group (I2 = 51%, WMD = -1.20, 95% CI: -1.51 to -0.90, P < 0.00001; Fig. 2B). A meta-analysis of back pain data at the final follow-up showed no statistically significant difference between the two groups (I2 = 0%, WMD = -0.14, 95% CI: -0.33 to 0.05, P = 0.14; Fig. 2C). Regarding VAS score for leg pain, the results indicated no statistically significant difference between the two groups at each time point (preoperative: I2 = 32%, WMD = 0.02, 95% CI: -0.26 to 0.31, P = 0.87; Fig. 3A) (early postoperative period: I2 = 71%, WMD = -0.13, 95% CI: -0.61 to 0.34, P = 0.58; Fig. 3B) (final follow-up: I2 = 46%, WMD = 0.05, 95% CI: -0.13 to 0.24, P = 0.56; Fig. 3C).
Functional outcomes
There have been four clinical trials involving ODI [19, 21,22,23], including UBE-TLIF groups (n = 143) and open surgery groups (n = 204). Meta-analysis showed no statistically significant difference in ODI scores between the two groups (preoperative: I2 = 80%, WMD = 1.30, 95% CI: -2.65 to 5.25, P = 0.52; Fig. 4A) (early postoperative period: I2 = 0%, WMD = -1.77, 95% CI: -4.66 to 1.12, P = 0.23; Fig. 4B) (final follow-up: I2 = 69%, WMD = -0.03, 95% CI: -2.12 to 2.07, P = 0.98; Fig. 4C).
Secondary outcomes
Operation time & hospitalization time
A total of five CCTs [19,20,21,22,23] reported the operative times for various approaches, including the UBE-TLIF group (n = 200) and the open operation group (n = 236). Subgroup analysis indicated significant differences in the MIS-TLIF subgroup (I2 = 0%, WMD = 30.40, 95% CI: 25.19 to 35.62, P < 0.00001) or PLIF/TLIF subgroup (I2 = 97%, WMD = 60.48, 95% CI: 5.81 to 115.14, P = 0.03). Furthermore, the combined analysis revealed a significant difference between the UBE-TLIF and open operation groups (I2 = 94%, WMD = 41.18, 95% CI: 19.20 to 63.15, P = 0.0002; Fig. 5A). Three CCTs [20,21,22] evaluated the length of hospital stay for both surgical approaches, including 59 patients in the UBE-TLIF group and 88 patients in the open operation group. There was no statistically significant difference between the two groups in terms of length of stay (I2 = 92%, WMD = -1.85, 95%CI: -5.01 to 1.30, P = 0.25; Fig. 5B).
Intraoperative blood loss & fusion rates
Across three retrospective studies [19, 20, 22], intraoperative blood loss was reported in two surgical approaches, including UBE-TLIF (n = 97) and open surgery (n = 111). The meta-analysis revealed significant differences between the UBE-TLIF and open operations groups (I2 = 73%, WMD = -122.60, 95% CI: -187.08 to -58.12, P = 0.0002; Fig. 6A). Approximately 85.7% of UBE-TLIF patients (240/280) and 87.2% of open surgery patients (279/320) reported fusion at the final follow-up in six CCTs [18,19,20,21,22,23]. There was no difference in fusion rates between MIS-TLIF subgroup (I2 = 0%, OR = 1.06, 95% CI: 0.53 to 2.13, P = 0.87) or PLIF/TLIF subgroup (I2 = 0%, OR = 0.65, 95% CI: 0.33 to 1.28, P = 0.21). Overall, the combined analysis showed no significant differences between the UBE-TLIF and open operation groups (I2 = 0%, OR = 0.82, 95% CI: 0.51 to 1.34, P = 0.44; Fig. 6B). Based on the available evidence, UBE-TLIF appears to achieve similar fusion rates to open surgery.
Complication
All studies reported postoperative complications [18,19,20,21,22,23]. There were 19 cases (7.0%) of complications in the UBE-TLIF group, and 20 cases (6.5%) in the open operation group. Subgroup analysis shows no difference in complication rates between the MIS-TLIF subgroup (I2 = 0%, OR = 0.73, 95% CI: 0.31 to 1.71, P = 0.47) or PLIF/TLIF subgroup (I2 = 0%, OR = 1.05, 95% CI: 0.40 to 2.75, P = 0.91). Undoubtedly, the combined results indicate no significant difference between the UBE-TLIF group and the open operating group (I2 = 0%, OR = 0.86, 95% CI: 0.46 to 1.62, P = 0.64; Fig. 7). Furthermore, the postoperative complications can be classified into three categories: neurological complications (postoperative epidural hematoma, dural tear, incomplete decompression, transient palsy, nerve root injury), hardware-related complications (cage subsidence), and surgical site complications (postoperative infection, DVT). Meta-analysis results showed no statistically significant complications in any subgroup (Fig. 8).
Publication bias
This study identified high heterogeneity in postoperative leg VAS scores, operation time, preoperative and postoperative ODI scores, length of hospital stay, and intraoperative blood loss. The duration of stay was determined through a leave-one-out sensitivity analysis. Only after omitting Kang et al. [20] was a shortened postoperative hospital stay in the UBE-TLIF group observed. Sensitivity analysis indicated minimal heterogeneity in other indicators, affirming result reliability. The author suggests that heterogeneity could stem from cultural disparities, variations in surgeon skill levels, differences in postoperative care protocols, and the presence of complications. In assessing publication bias, an asymmetric funnel plot suggests potential bias in reporting postoperative complications.
Discussion
Necessity analysis
Advances in medical devices and surgical concepts have made minimally invasive surgery the mainstay of treatment for LDD. The fundamental objective of minimally invasive surgery is to alleviate symptoms [24]. In contrast to conventional open surgery, UBE-TLIF instruments are positioned within two distinct channels, affording greater maneuverability to achieve more comprehensive decompression. Endoscopes were employed to facilitate visual assessment of procedures encompassing endplate manipulation, cartilage endplate removal, and bony endplate exposure. Advocates of the UBE-TLIF technique emphasize multiple merits, including minimized incision size, less strain on paraspinal muscles, and a shortened learning curve [23, 25,26,27]. Consequently, given the lack of systematic reviews, this meta-analysis was undertaken to establish a more reliable foundation for clinical decision-making.
Clinical efficacy evaluation
According to Fairbank et al. [28], the ODI and VAS scores effectively gauge the impact of low back pain on daily functional capacity. In the clinical data of this study, there was no significant difference in fusion rate, leg VAS score, or ODI improvement between UBE-TLIF and open surgery. In conclusion, UBE-TLIF has not demonstrated a higher fusion rate or greater functional improvement compared with open surgery. Compared with the open surgery group, the early low back VAS score of the UBE-TLIF group decreased by 1.20 units. Although open surgery remains the prevailing treatment approach for LDD, the combined early postoperative low back VAS scores in this study favor UBE-TLIF. There is no doubt that early improvement in low back pain can be attributed to the minimally invasive nature of UBE-TLIF surgery and its preservation of spinal column anatomy. Furthermore, the percutaneous tension-free access incision utilized in UBE-TLIF surgery mitigates soft tissue compression and stripping, thereby reducing the occurrence of chronic back pain [29]. There has been evidence that postoperative low back pain is associated with muscle denervation and atrophy, emphasizing the importance of reducing muscle damage during surgery [23, 30].
Liu et al. [22] and Kang et al. [20] reported increased early postoperative serum creatine phosphokinase (CPK) and C-reactive protein (CRP) levels in both UBE-TLIF and PLIF groups, with a smaller rise in the UBE-TLIF group. According to the above study, UBE-TLIF surgery reduces systemic inflammation, medication-induced muscle damage, postoperative pain, and improves quality of life. Meta-analysis also showed that UBE-TLIF had less intraoperative blood loss but a longer operation time (P < 0.05), which is consistent with the results of previous studies [19,20,21,22,23]. The author speculates that surgeon experience is the main factor behind this difference in operative time. Spine surgeons who are unfamiliar with endoscopic manipulation may find UBE-TLIF challenging because of the need to manipulate biportal channels and optimize the visibility of the surgical field. Additionally, the learning curve of a new technique can affect the operative time. In a 2020 study, Kim et al. [31] reported that approximately 34 cases were needed to attain proficiency in the UBE-TLIF technique. Wang et al. [32] demonstrate that the operation time of UBE-TLIF was gradually shortened with the increase in the number of surgical cases, ultimately stabilizing after the completion of 17 instances.
The initial learning curve during surgery can impact the occurrence of postoperative complications, especially neurological issues such as dural tears, nerve root injuries, and epidural hematomas. Neurological complications were 1.38 units higher in the UBE-TLIF group than in the open surgery group, with dural tears leading the way, although there was no statistically significant difference between the two groups. Dural tears may manifest early during the learning process or be linked to adhesion of the ligamentum flavum. Smaller dural tears can typically be repaired with gelatin sponge, while larger tears usually necessitate conversion to MIS-TLIF. There were no cases of large dural tears requiring open surgery in the included studies.
Limitation analysis
The UBE-TLIF technique can theoretically avoid extensive muscle stripping, relieve low back pain, encourage patients to move early, and reduce the risk of complications caused by long-term bed rest. It is especially suitable for patients with poor basic conditions. Furthermore, UBE-TLIF is associated with shorter hospital stays, supporting rehabilitation and reducing hospitalization costs. However, this meta-analysis has several limitations: 1) Due to the recent introduction of UBE-TLIF, there is limited available literature; 2) Despite the overall high quality of the included studies, the lack of RCTs may have influenced the findings; 3) Variations in follow-up duration among the included studies may influence outcomes; 4) The lack of distinction between different surgical procedures may introduce bias when describing them as open procedures.
Conclusions
The meta-analysis results indicate that UBE-TLIF outperforms open surgery in reducing hospital stay, decreasing intraoperative blood loss, and improving early postoperative function. However, no significant difference was found in long-term function between the two groups. Nevertheless, additional high-quality multicenter randomized controlled trials are required to bolster these results.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- LDD:
-
Lumbar degenerative diseases
- UBE-TLIF:
-
Unilateral biportal endoscopic transforaminal lumbar interbody fusion
- CCTs:
-
Case–control trials
- RCTs:
-
Randomized controlled trials
- UBE:
-
Unilateral biportal endoscopy
- MIS-TLIF:
-
Minimally invasive transforaminal lumbar interbody fusion
- VAS:
-
Visual analog scale
- ODI:
-
Oswestry Disability Index
- NOS:
-
Newcastle–Ottawa scale
- CPK:
-
Creatine phosphokinase
- CRP:
-
C-reactive protein
References
Diebo B, Shah N, Boachie-Adjei O, Zhu F, Rothenfluh D, Paulino C, Schwab F, Lafage V. Adult spinal deformity. Lancet (London, England). 2019;394(10193):160–72.
Vos T, Flaxman A, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon J, Abdalla S, Aboyans V, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England). 2012;380(9859):2163–96.
Zhang Y, Lu D, Ji W, He F, Chen A, Yang H, Zhu X. Which is the most effective treatment for lumbar spinal stenosis: decompression, fusion, or interspinous process device? A Bayesian network meta-analysis. J Orthop Translat. 2021;26:45–53.
Kim J, Choi D. Biportal endoscopic transforaminal lumbar interbody fusion with arthroscopy. Clin Orthop Surg. 2018;10(2):248–52.
Silverman L, Heaton W, Farhang N, Saxon L, Dulatova G, Rodriguez-Granrose D, Flanagan F, Foley K. Perspectives on the treatment of lumbar disc degeneration: the value proposition for a cell-based therapy, immunomodulatory properties of discogenic cells and the associated clinical evaluation strategy. Front Surg. 2020;7:554382.
Sik Goh T, Hwan Park S, Suk Kim D, Ryu S, Min Son S, Sub Lee J. Comparison of endoscopic spine surgery and minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease: A meta-analysis. J Clin Neurosci. 2021;88:5–9.
Wu J, Guan T, Tian F, Liu X. Comparision of biportal endoscopic and microscopic decompression in treatment of lumbar spinal stenosis: a comparative study protocol. Medicine. 2020;99(30):e21309.
Kim N, Jung S. Percutaneous unilateral biportal endoscopic spine surgery using a 30-degree arthroscope in patients with severe lumbar spinal stenosis: a technical note. Clin Spine Surg. 2019;32(8):324–9.
Nandyala SV, Fineberg SJ, Pelton M, Singh K. Minimally invasive transforaminal lumbar interbody fusion: one surgeon’s learning curve. Spine J. 2014;14(8):1460–5.
Park Y, Seok SO, Lee SB, Ha JW. Minimally invasive lumbar spinal fusion is more effective than open fusion: a meta-analysis. Yonsei Med J. 2018;59(4):524–38.
Gadjradj PS, Harhangi BS, Amelink J, van Susante J, Kamper S, van Tulder M, Peul WC, Vleggeert-Lankamp C, Rubinstein SM. Percutaneous transforaminal endoscopic discectomy versus open microdiscectomy for lumbar disc herniation: a systematic review and meta-analysis. Spine (Phila Pa 1976). 2021;46(8):538–49.
Choi KC, Shim HK, Hwang JS, Shin SH, Lee DC, Jung HH, Park HA, Park CK. Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg. 2018;116:e750–8.
Heo DH, Kim JS, Park CW, Quillo-Olvera J, Park CK. Contralateral sublaminar endoscopic approach for removal of lumbar juxtafacet cysts using percutaneous biportal endoscopic surgery: technical report and preliminary results. World Neurosurg. 2019;122:474–9.
Pranata R, Lim M, Vania R, July J. Biportal endoscopic spinal surgery versus microscopic decompression for lumbar spinal stenosis: a systematic review and meta-analysis. World Neurosurg. 2020;138:e450–8.
Heo D, Son S, Eum J, Park C. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus. 2017;43(2):E8.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:00142.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Gatam AR, Gatam L, Mahadhipta H, Ajiantoro A, Luthfi O, Aprilya D. Unilateral biportal endoscopic lumbar interbody fusion: a technical note and an outcome comparison with the conventional minimally invasive fusion. Orthop Res Rev. 2021;13:229–39.
Heo DH, Park CK. Clinical results of percutaneous biportal endoscopic lumbar interbody fusion with application of enhanced recovery after surgery. Neurosurg Focus. 2019;46(4):E18.
Kang MS, You KH, Choi JY, Heo DH, Chung HJ, Park HJ. Minimally invasive transforaminal lumbar interbody fusion using the biportal endoscopic techniques versus microscopic tubular technique. Spine J. 2021;21(12):2066–77.
Kim JE, Yoo HS, Choi DJ, Park EJ, Jee SM. Comparison of minimal invasive versus biportal endoscopic transforaminal lumbar interbody fusion for single-level lumbar disease. Clin Spine Surg. 2021;34(2):E64-e71.
Liu G, Liu W, Jin D, Yan P, Yang Z, Liu R. Clinical outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF). The spine journal : official journal of the North American Spine Society. 2023;23(2):271–80.
Park MK, Park SA, Son SK, Park WW, Choi SH. Clinical and radiological outcomes of unilateral biportal endoscopic lumbar interbody fusion (ULIF) compared with conventional posterior lumbar interbody fusion (PLIF): 1-year follow-up. Neurosurg Rev. 2019;42(3):753–61.
Siebert E, Prüss H, Klingebiel R, Failli V, Einhäupl K, Schwab J. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol. 2009;5(7):392–403.
Choi DJ, Choi CM, Jung JT, Lee SJ, Kim YS. Learning curve associated with complications in biportal endoscopic spinal surgery: challenges and strategies. Asian Spine J. 2016;10(4):624–9.
Park SM, Kim HJ, Kim GU, Choi MH, Chang BS, Lee CK, Yeom JS. Learning curve for lumbar decompressive laminectomy in biportal endoscopic spinal surgery using the cumulative summation test for learning curve. World Neurosurg. 2019;122:e1007–13.
Kang MS, Hwang JH, Choi DJ, Chung HJ, Lee JH, Kim HN, Park HJ. Clinical outcome of biportal endoscopic revisional lumbar discectomy for recurrent lumbar disc herniation. J Orthop Surg Res. 2020;15(1):557.
Fairbank J, Pynsent P. The Oswestry disability index. Spine. 2000;25(22):2940–52. discussion 2952.
Kim W, Kim S, Kang S, Park H, Han S, Lee S. Pooled analysis of unsuccessful percutaneous biportal endoscopic surgery outcomes from a multi-institutional retrospective cohort of 797 cases. Acta Neurochir. 2020;162(2):279–87.
Sihvonen T, Herno A, Paljärvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;18(5):575–81.
Kim JE, Yoo HS, Choi DJ, Hwang JH, Park EJ, Chung S. Learning curve and clinical outcome of biportal endoscopic-assisted lumbar interbody fusion. Biomed Res Int. 2020;2020:8815432.
Wang N, Bei C, Wan J, Wang H. Learning curve analysis of unilateral biportal endoscopic lumbar interbody fusion. Chin J Reparative Reconstruct Surg. 2022;36(10):1229–33.
Acknowledgements
The authors thank all the participants, as well as Mr. Hu for the revisions.
Funding
This work is funded by the Zhejiang Medical and Health Program (main research) project. Zhejiang Medical and Health Plan (No. 2020KY957; No. 2022KY1251).
Author information
Authors and Affiliations
Contributions
QY conceived the study, and both QY, PR, XH, XP and HL participated in the study and conducted a statistical analysis and drafted the manuscript. All five authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, Q., Lu, H.g., Pan, X.k. et al. Unilateral biportal endoscopic transforaminal lumbar interbody fusion versus conventional interbody fusion for the treatment of degenerative lumbar spine disease: a systematic review and meta-analysis. BMC Musculoskelet Disord 24, 838 (2023). https://doi.org/10.1186/s12891-023-06949-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06949-y