Abstract
Background
Rehabilitation is essential to optimize outcomes after surgical procedures in musculoskeletal disorders. However, adherence to rehabilitation continues to be an important barrier, since compliance with the programs is not always as desired, which may have a negative impact on clinical results.
Methods
Randomized controlled trial aimed at to determining the effectiveness of using a virtual assistant (i.e., chatbot) to promote adherence to home rehabilitation. Overall, seventy patients under 75, undergoing total knee replacement, who have a personal smartphone and are familiar with its use, will be assigned into the control (standard care) or the experimental (standard care plus virtual assistant) group. Adherence (primary outcome) will be assessed three months after surgery. The WOMAC questionnaire, knee pain and system usability scale will be also outcomes of interest at three months and one year. Overall, an analysis of variance will look for possible time, group and time*group interactions.
Discussion
The expected result is to determine whether the use of a chatbot that interacts with the patient can increase adherence to post-surgical home physiotherapy, and result in better clinical results (functional and pain) than standard care.
Trial registration
clinicaltrials.gov id. NCT05363137
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Musculoskeletal disorders (MD) are the leading cause of pain and disability [1]. Physiotherapy plays a fundamental role in the recovery, but low adherence, reported to be from 65% to as low as 20% [2,3,4], continue to be one of the main barriers [5], especially regarding in-home and non-face-to-face interventions [2, 6].
Understanding adherence as the degree to which a person’s behavior corresponds to the agreed recommendations of a health care provider (WHO, 2003), adherent patients may have better clinical outcome [7,8,9], whereas poor compliance has a negative influence, with likely consequences on socio-sanitary costs [10].
The current limitation of resources has caused healthcare systems to progressively implement non-face-to-face rehabilitation programs, based on education and information brochures [11, 12]. A situation enhanced by the recent health pandemic that has driven a paradigm shift, especially in cases of risk such as older adults, people with comorbidities, as well as people with mobility difficulties, living in isolated areas or with any other similar situation that makes health care difficult [13].
Current trends point to the use of information and communication technologies (ICT) and digital media as a solution to administer home treatments [14,15,16,17]. However, since non-compliance rates are one of the main barriers, the digital applications of physiotherapy should be aimed not only at improving clinical results, but also at fostering adherence. This will be achieved through interactive and accessible environments that promote self-efficacy and behavioral changes, setting measurable and achievable goals and reporting on progress.
ICT, rehabilitation and adherence
The use of ICT in rehabilitation has evolved over time, since the 1980s when it was proposed to emphasize follow-up with phone calls [18], towards other solutions such as pre-recorded videos for use and interaction with the patient [19], interactive videoconferences [15], and technologies based on sensors and remote monitoring [20]. In addition, interventions based on virtual equipment and environments, specifically designed for rehabilitation or not, have been common, among which the interest in devices such as the Wii® have stood out [21,22,23].
In recent years, smartphones have revolutionized communication, with new opportunities also in the medical field. Especially considering factors like half of smartphone users use their devices for health information [24], or that a fifth part use applications related to this area [25]. Due to this, the range of health-oriented mobile applications (Apps) available for health professionals, patients, students and the general population is increasing [26].
Although adherence is a topic that is attracting more and more interest, the applications do not usually specifically aim to promote this aspect. In the field of healthcare there are a large number of mobile applications or electronic devices used for this purpose (e.g., the electronic pillbox) [27], but are mostly oriented to taking medications, helping the patient with reminders. Other applications do have additional features that promote adherence to medication without forgetting adherence to treatment. However, very little research has been done to assess their effectiveness for the purposes for which they were designed or the level of acceptance among users [28].
Scientific proposal and objective
Smart mobile devices are possibly the technology that currently offers the greatest potential. Apps are the main trend today [28]. As an alternative, this project proposes the use of a virtual assistant, acting as a conversational healthcare provider by means of a chatbot. Chatbots can have different degrees of complexity; the most advanced ones, are designed with artificial intelligence, through natural language processing (NLP). The assistants are responsible for simulating a human conversation, which can be very useful for guiding the patient in the physiotherapy program. Chatbots, mainly used for commercial purposes, have been increasingly appraised in healthcare [29, 30]. However, their use to manage musculoskeletal disorders is still understudied.
Given the above factors, this research aims to determine the effectiveness of a virtual assistant chatbot, that communicates via an instant messaging service application, to promote compliance and adherence to home physiotherapy programs in people undergoing total knee replacement. The hypothesis is that the use of a chatbot that interacts with a patient undergoing total knee replacement through an instant messaging service will increase adherence to home physiotherapy, what improve clinical outcome (function and pain).
Study population
More than one hundred MD have been classified (WHO, 2019). The scientific proposal will be transferable to the high number conditions that require physiotherapy treatment, with a consequent socio-economic impact. However, in order to carry out a clinical validation with a homogeneous sample, we target patients with severe knee osteoarthritis undergoing total knee replacement. This is justified, on the one hand, by the age of the population, which is proposed to be older adults. This will avoid unnecessary travel and will encourage compliance with recommendations such as social distancing. In addition, it satisfies the clinical need to perform physiotherapy after a highly invasive surgical procedure, which should preferably be done at home to optimize resources and reduce social and health risks.
Methods
Design
This design of this 2-armed randomized clinical trial has been approved by the Research Ethics Committees of Hospital Clínic i Universitari (no. 2020/350) and Hospital Politècnic i Universitari from Valencia (no. 2021-001-1), ensuring compliance with the ethical and legal provisions of the research. The experiments will be performed in accordance with the principles of the Declaration of Helsinki. The study has been prospectively registered (clinicaltrials.gov id. NCT05363137). Informed consent will be obtained from participants. The Universitat de València is responsible for the integrity and conduct of the study, which started on September 2022. The intervention period, in which participants will took part sequentially, will end approximately one year later, while the follow-up extends up to one year after enrolling the last participant.
Participants
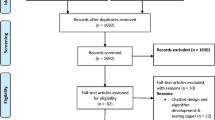
Individuals on the waiting list for total knee replacement surgery will be invited if the following inclusion criteria are met: age less than 75, undergoing primary total knee replacement surgery, have a personal smartphone, with an instant messaging application installed, and familiar with the use of such application (more than 3 accesses per week), with no evident cognitive state that prevents to understand care provider instructions, read and write and able to consent to participate. Potential participants with vestibular or central nervous system affection (e.g., stroke), who cannot read or write, or do not understand Spanish, will be excluded. Figure 1 shows the participants flowchart.
Procedures
Two orthopedic surgeons (one per hospital) will screen potential participants; then, the principal investigator will verify compliance with the inclusion criteria. informed consent will be obtained from the participants. A simple randomization method will be conducted, according to which a random number generator sequence is generated in origin with a software program (Matlab®). The principal investigator will allocate participants according to this sequence. One member of the team, blinded to group allocation, will have the only task to collect data and assess participants. Both groups will receive standard postoperative care, and the interventors will be blinded to group allocation. However, one member of the team, who will not be involved in standard care sessions, will show participants in the experimental group how to use the chatbot tool designed for this trial.
Interventions
Both groups will receive standard postoperative care. Overall, standard in-patient rehabilitation begins the after surgery and lasts until medical discharge (usually less than 3 days). The patients are encouraged to train and taught how should keep training at home. Approximately one week after surgery, patients are appointed to start a standard outpatient rehabilitation program, in which mainly strengthening, functional and balance exercises are performed. After this, there is one more education session, in which the physiotherapist explains and instructs the exercises that they should continue doing at home, and facilitates a printed brochure with the information. The participants in the experimental group will receive the same education (i.e. last day before inpatient and outpatient discharge), but instead of being provided with a brochure, they will be informed that the intervention program will be supervised via an automated chatbot, through which they will receive motivational messages, reminders, and instruction on how to train. They will also be requested to answer some question (necessary to collect information such as compliance), as if it were a conversation. The tool allows participants to send messages with open questions or directly asking for help; if some message was not within the predefined possibilities, the physiotherapist receives a notification, and could contact via this messaging service or by telephone call as soon as possible.
Data collection and measures
The basic characteristics of participants, including sex, age, weight and height (to calculate body mass index), previous falls and description (6 moths), operated knee, occupation and residence (rural/city) will be collected. The summary of measures and time points for assessment are shown in Table 1.
Adherence-related measures
The primary outcome will be the compliance with the intervention (i.e. the number of implemented sessions n and the rate between n and the programmed sessions). Adherence will be achieved for participants who comply over 80% of sessions goal, which is consistent with the definition of adherence from a pharmacological perspective [31, 32]. In the experimental group, compliance will be registered with the instant messaging tool. In the control group, a calendar will be provided to participants, who will be instructed to register every training day and time. Participants who document the number of days they train, with over 80% of documented sessions will be classified as achieved adherence.
The Spanish version of the International Physical Activity Questionnaire (IPAQ-E) will assess the types of intensity of physical activity and sitting time as part of the participants’ daily lives, i.e., the total physical activity in metabolic equivalent of task (MET)-minutes/week and time spent sitting. ActiGraph wGT3X-BT monitors will be provided to participants to capture and record physical activity parameters, since this is a reliable and valid measurement of PA in older adults after TKR [33].
In addition, we will assess the system usability, feasibility and safety. Safety will be assessed by reporting the number of adverse events recorded from baseline to 12 m, these being was defined as any unfavorable or unintended diagnosis, sign, symptom, or disease associated with the study. Feasibility will be evaluated with recruitment and retention rates. The system usability scale will be used for measuring the usability of the tool, since this is a reliable tool to evaluate a wide variety of products and services, including hardware, software, mobile devices, websites and applications; [34] it consists of a 10-item questionnaire with five response options from strongly agree to strongly disagree. The sores are added together and then multiplied by 2.5 to convert the original scores to 0-100. Based on research, a score above a 68 would be considered above average and anything below 68 is below average, however the results will be normalized as a percentile ranking. In addition, we will collect information on the number of interactions with the tool per patient, total accesses, the percentage of the originally specified treatment that has been completed, as well as the total protocols completed.
Clinical outcome
The following measures will be used to assess function and pain in order to determine the effects on clinical outcome. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), a self-administered questionnaire consisting of 24 items divided into pain, stiffness and physical function will register self-reported status [35]. The Timed up and go test, a timed test of general mobility in which the participant is instructed to get up from an arm-chair, walk three meters, turn around a cone, and come back to sit again [36]. The Five times sit to stand test will be used to assess functional performance, as a valid instrument that test lower limb strength and balance [37]. Knee range of motion will be the clinician-reported measure used to assess knee function with a digital goniometer (Baseline ®) [38]. Knee pain will be assessed with a visual analogue scale, which ranges from, no pain, to 10, the worst possible pain, felt in the knee during the last week. Timepoints for assessment are shown in Table 1.
Data analysis
A descriptive analysis of the characteristics of the participants will be conducted using means, standard deviations, frequencies, interquartile ranges and contingency tables. To test the hypothesis that the participants in the experimental group will have a higher compliance and, consequently, better clinical outcome in terms of functionality and pain than participants in control group, an inferential analysis will compare baseline status with t-tests that will be parametric or not depending on the Wilcoxon and Shapiro-Wilk results. Subsequently, baseline progression will be compared with an analysis of variance (ANOVA) based on a general mixed model of repeated measures, looking for time (pre-post), group (experimental-control) and time per group interactions. In case of baseline differences, an analysis of covariance (ANCOVA) will be performed in which the data will be adjusted to the baseline scores, which will be entered as covariates. Post-hoc analysis will be performed in case of significant differences (Dunett and Tukey). Significance levels will be set at 95%. Quantitative adherence data will be compared in the same way (number of sessions, etc.). Additionally, a qualitative analysis will be used to estimate whether basal changes exceed the minimum detectable change or the minimum of clinical important difference. The questionnaires will be analyzed qualitatively.
To deal with missing data, in the event that a participant cannot, or decides not to attend the follow-up evaluation, we will try to get them to solve self-reported questionnaires at home. The possibility of displacement of the evaluator is also considered. In addition, the baseline characteristics of those patients who have been evaluated and those who have not will be compared, looking for possible sources of bias. A record of the reasons for dropping out will be made and, if necessary, the best analysis mechanism will be evaluated, with methods to impute data and re-analyze them with intention to treat, evaluating the possible impact on the conclusions. The incidence of clinical adverse events will be recorded and categorized as definite, probable, or possibly related to the interventions. In addition, the number and type of errors in the tool, failures and the number of times that there has been a need for reprogramming will be analyzed. The difficulties in use reported by the participants will be synthesized according to established scales.
If it is considered that the tool can increase the compliance ratio with the domiciliary physiotherapy program by 20%, a priori sample size calculation with the G*Power tool, using a F-test, repeated measures between groups, with f = 0.3, α = 0.05 and β = 0.2, considering an overall retention rate of 85%, and rounding up, suggests that an estimated of 70 participants equally distributed into the two groups will be needed to achieve a power over 80%. A post-hoc analysis will determine the actual trial power.
Discussion
Adherence to treatment and compliance with rehabilitation continue to be one of the main barriers in the recovery of patients with musculoskeletal disorders [5]. Even more, taking into account the current limitation of resources, which makes it less and less feasible for public health services to offer face-to-face rehabilitation [11]. And yet, a considerable number of studies suggest that domiciliary rehabilitation programs can be as effective as outpatient, supervised or even group rehabilitation programs [39]. But success largely depends on compliance with exercise programs [7,8,9].
In recent years, special attention has been paid to how to solve the problem of adherence, with multiple and very diverse proposals in different areas of health and conditions, not only in MD, but also neurological patients or even in patients with behavioral disorders [30]. We believe that both the evaluation of new strategies and the use of ICT are factors that will be key to overcoming this barrier.
The use of a virtual assistant is not usual in healthcare, but it is true that it is not something new either. A number of research has appraised this technology in different forms for different conditions. However, its use via an instant messaging service to treat musculoskeletal conditions has not been comprehensively apprised. It is quite likely that in the coming years there will be an increase and generalization in the use of virtual assistants and conversational Chabots in healthcare. So it becomes necessary to generate scientific evidence on aspects such as usefulness, usability, validity and effectiveness in different areas.
Strengths and limitations
The proposal is innovative; is positioned at the forefront of remote physiotherapy treatment, being aware that technological advances will be integrated progressively. In addition, it takes into account both the current resource limitation and possible health situations similar to the COVID-19 pandemic, which would require remote treatment. Therefore, through an initiative that provides a solution to current and future needs, this research responds to the requirements of an aging society. In addition, the proposal is evaluated in end users, in order to improve the capabilities of older adults with chronic MD in their daily lives. It is, therefore, a current and groundbreaking project, perfectly aligned with social and health priorities.
The interventions have been designed in a realistic way, taking into consideration the information provided by long-experienced physiotherapists, orthopedic surgeons and researchers, but also patient feedback in previous studies [40]. The experimental intervention has been designed as similar as possible to standard outpatient care, and adapted to home environment. Inclusion criteria are broad, not restricted to a large number of patients with comorbidities, which will increase the applicability. The exclusion criteria did not seek to promote the results, and therefore, there is no exclusion due to social disadvantages, depression, anxiety or poor motivation, which are frequently set in clinical research.
This research comes with limitations, for instance, the interventions cannot be concealed, and that some of the measures are usual in research but not clinical practice. We plan to share, critically appraise and disseminate the results by offering critical discussion of the findings, description of potential clinical impact, clinical application, and contextualization within contemporary literature [40]. A protocol publication helps to reduce implementation bias; however, in case of substantial changes in study design and protocol, these will be reported with reasons.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. Any information can be requested / consulted to the principal investigator or corresponding author.
Abbreviations
- MD:
-
Musculoskeletal disorders
- ICT:
-
Information and communication technologies
- NLP:
-
Natural language processing
- IPAQ-E:
-
International Physical Activity Questionnaire
- WOMAC:
-
The Western Ontario and McMaster Universities Osteoarthritis Index
References
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 Diseases and Injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. The Lancet. 2018;392:1789–858.
McLean SM, Burton M, Bradley L, Littlewood C. Interventions for enhancing adherence with physiotherapy: a systematic review. Man Therap. 2010;15:514–21.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9.
Dean SG, Smith JA, Payne S, Weinman J. Managing time: an interpretative phenomenological analysis of patients’ and physiotherapists’ perceptions of adherence to therapeutic exercise for low back pain. Disabil Rehabil. 2005;27:625–36.
Lin J, Sklar GE, Oh VM, Sen, Li SC. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4:269–86.
Okezue OC, Nwafor GC, Ezeukwu OA, John JN, Uchenwoke CI. Adherence to Home Exercise Programmes and its Associated factors among patients receiving physiotherapy. Clinical Health Promotion - Research and best practice for patients. staff and community. 2019;9:7–14.
Mazières B, Thevenon A, Coudeyre E, Chevalier X, Revel M, Rannou F. Adherence to, and results of, physical therapy programs in patients with hip or knee osteoarthritis. Development of french clinical practice guidelines. Joint Bone Spine. 2008;75:589–96.
Baumgartner PC, Haynes RB, Hersberger KE, Arnet I. A systematic review of medication adherence thresholds dependent of clinical outcomes. Frontiers in Pharmacology. 2018;9 NOV:1290.
Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–42.
Jack K, McLean SM, Moffett JK, Gardiner E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Therap. 2010;15:220–8.
Anesi GL, Kerlin MP. The impact of resource limitations on care delivery and outcomes: routine variation, the coronavirus disease 2019 pandemic, and persistent shortage. Curr Opin Crit Care. 2021;27:513.
Butler CR, Wong SPY, Wightman AG, O’Hare AM. US Clinicians’ Experiences and Perspectives on Resource Limitation and Patient Care during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2027315–5.
Lee AC. COVID-19 and the advancement of digital physical therapist practice and telehealth. Phys Ther. 2020;100:1054–7.
Peretti A, Amenta F, Tayebati S, … GN-J rehabilitation, 2017 undefined. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. rehab.jmir.org.
Brennan DM, Georgeadis AC, Baron CR, Barker LM. The effect of videoconference-based telerehabilitation on story retelling performance by brain-injured subjects and its implications for remote speech-language therapy. Telemedicine and e-Health. 2004;10:147–54.
McCue M, Fairman A, Pramuka M. Enhancing quality of life through Telerehabilitation. Phys Med Rehabil Clin North Am. 2010;21:195–205.
Owens JG, Rauzi MR, Kittelson A, Graber J, Bade MJ, Johnson J, et al. How New Technology is improving physical therapy. Curr Rev Musculoskelet Med. 2020;13:200–11.
Korner-Bitensky N, Wood-Dauphinee S. Barthel index information elicited over the telephone: is it reliable? Am J Phys Med Rehabil. 1995;74:9–18.
Wertz R, Dronkers NF, Bernstein-Ellis E, Sterling LK, Shubitowski Y, Elman R, et al. Potential of telephonic and television technology for appraising and diagnosing neurogenic communication disorders in remote settings. Aphasiology. 1992;6:195–202.
Piqueras M, Marco E, Coll M, Escalada F, Ballester A, Cinca C, et al. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: a randomized controlled trial. J Rehabil Med. 2013;45:392–6.
Staiano AE, Flynn R. Therapeutic uses of active videogames: a systematic review. Games for Health Journal. 2014;3:351–65.
Webster D, Celik O. Systematic review of Kinect applications in elderly care and stroke rehabilitation. J Neuroeng Rehabil. 2014;11:108.
Bateni H. Changes in balance in older adults based on use of physical therapy vs the Wii Fit gaming system: a preliminary study. Physiotherapy (United Kingdom). 2012;98:211–6.
Kamel Boulos MN, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP. Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform. 2014;5:229.
Santo K, Chow CK, Thiagalingam A, Rogers K, Chalmers J, Redfern J. MEDication reminder APPs to improve medication adherence in Coronary Heart Disease (MedApp-CHD) study: a randomised controlled trial protocol. BMJ Open. 2017;7.
Murnane EL, Hu↵aker D, Kossinets G. Mobile Health Apps: Adoption, Adherence, and Abandonment. dl.acm.org. 2015;:261–4.
Schwartz JK. Pillbox use, satisfaction, and effectiveness among persons with chronic health conditions. Assist Technol. 2017;29:181–7.
Pérez-Jover V, Sala-González M, Guilabert M, Mira JJ. Mobile apps for increasing treatment adherence: systematic review. J Med Internet Res. 2019;21:e12505.
Gentner T, Neitzel T, Schulze J, Buettner R. A Systematic Literature Review of Medical Chatbot Research from a Behavior Change Perspective. Proceedings – 2020 IEEE 44th Annual Computers, Software, and Applications Conference, COMPSAC 2020. 2020;:735–40.
Bhirud N, Tatale S, Tataale S, Randive S, Nahar S. A Literature Review on Chatbots in Healthcare Domain Computational feasibility of Paninian Grammar for indian Languages’ analyses View project machine learning View project A Literature Review on Chatbots Healthcare Domain. INTERNATIONAL JOURNAL OF SCIENTIFIC & TECHNOLOGY RESEARCH. 2019;8:7.
Morrison A, Stauffer ME, Kaufman AS. Defining medication adherence in individual patients. Patient Prefer Adherence. 2015;9:893.
Christiansen MB, Thoma LM, Master H, Voinier D, Schmitt LA, Ziegler ML, et al. The feasibility and preliminary outcomes of a physical therapist-administered physical activity intervention after total knee replacement. Arthritis Care Res (Hoboken). 2020;72:661.
Almeida GJ, Irrgang JJ, Fitzgerald GK, Jakicic JM, Piva SR. Reliability of physical activity measures during free-living activities in people after total knee arthroplasty. Phys Ther. 2016;96:898–907.
Brooke J. SUS: a “Quick and Dirty” usability scale. CRC Press; 1996.
Roos EM, Toksvig-Larsen S. Knee injury and osteoarthritis outcome score (KOOS) – validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17.
J Am Geriatr Soc. 1991;39:142–8.
Medina-Mirapeix F, Vivo-Fernández I, López-Cañizares J, García-Vidal JA, Benítez-Martínez JC, del Baño-Aledo ME. Five times sit-to-stand test in subjects with total knee replacement: reliability and relationship with functional mobility tests. Gait Posture. 2018;59:258–60.
Domínguez-Navarro F, Silvestre-Muñoz A, Igual-Camacho C, Díaz-Díaz B, Torrella JV, Rodrigo J, et al. A randomized controlled trial assessing the effects of preoperative strengthening plus balance training on balance and functional outcome up to 1 year following total knee replacement. Arthroscopy: Knee Surgery, Sports Traumatology; 2020. pp. 1–11.
Gutiérrez-Espinoza H, Araya-Quintanilla F, Cereceda-Muriel C, Álvarez-Bueno C, Martínez-Vizcaíno V, Cavero-Redondo I. Effect of supervised physiotherapy versus home exercise program in patients with subacromial impingement syndrome: a systematic review and meta-analysis. Phys Ther Sport. 2020;41:34–42.
Blasco J-M, Igual-Camacho C, Roig-Casasús S. In-home versus hospital preoperative balance and proprioceptive training in patients undergoing TKR; rationale, design, and method of a randomized controlled trial. BMC Musculoskelet Disord. 2017;18:518.
Acknowledgements
Not applicable.
Funding
Project PID2020-115825RA-I00, funded by MCIN/ AEI/https://doi.org/10.13039/501100011033, convocatoria Proyectos I + D + i 2020 - Modalidades “Retos Investigación” y “Generación de Conocimiento”. The funder played no role on the study design.
Author information
Authors and Affiliations
Contributions
All the authors agree with the last version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent
The design has been approved by the Research Ethics Committees of Hospital Clínic i Universitari (no. 2020/350) and Hospital Politècnic i Universitari from Valencia (no. 2021-001-1), ensuring compliance with the ethical and legal provisions of the research. The experiments will be performed in accordance with the principles of the Declaration of Helsinki. Informed consent will be obtained from participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Blasco, JM., Díaz-Díaz, B., Igual-Camacho, C. et al. Effectiveness of using a chatbot to promote adherence to home physiotherapy after total knee replacement, rationale and design of a randomized clinical trial. BMC Musculoskelet Disord 24, 491 (2023). https://doi.org/10.1186/s12891-023-06607-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06607-3