Abstract
Purpose
To investigate the effects of various demographic, structural, radiographic, and clinical factors on the prognosis of patients with medial compartmental knee osteoarthritis with varus deformity undergoing medial opening wedge high tibial osteotomy (HTO) in combination with bone marrow concentrate (BMC) injection.
Methods
In this prospective study, 20 patients underwent medial opening wedge HTO in combination with BMC injection with 12 months of follow-up. The structural and radiographic outcomes were evaluated by femorotibial angle and posterior tibial slope angle. The clinical outcomes were evaluated by visual analogue scale (VAS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), and The Knee injury and Osteoarthritis Outcome Score (KOOS). Multivariate nonlinear mixed-effects models with asymptotic regressions were used to model the trajectory of symptom improvement.
Results
Medial opening wedge HTO in combination with BMC corrected the malalignment of the knee and led to significant symptom relief. The improvement of clinical symptoms reached a plateau 6 months after the surgery. Greater symptom severity at baseline and lower Kellgren-Lawrance (KL) grades were correlated with better post-operative clinical outcomes. Body-Mass-Index (BMI), femorotibial angle, age, and sex may also play a role in influencing the extent of symptom relief.
Conclusion
Symptom severity at baseline is important for prognosis prediction. In clinical practice, we suggest that the evaluation of clinical features and functional status of the patients be more emphasised.
Similar content being viewed by others
Introduction
Knee osteoarthritis is one of the leading causes of knee pain and dysfunction [1, 2]. Because of the ageing population and the prevalence of obesity, the increase in global incidence rate of knee osteoarthritis has led to severe physical, psychological, and economic burden on patients’ families and the whole society [3,4,5,6]. According to the current European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) guideline, the Osteoarthritis Research Society International (OARSI) guideline, and American College of Rheumatology/Arthritis Foundation (ACR/AF) guideline in 2019, non-pharmacological treatments, including exercise, education, and weight loss (if overweight), should be initially prescribed [7,8,9]. Pharmacological agents such as non-steroidal anti-inflammatory drugs, intra-articular corticosteroids, and hyaluronic acids are subsequently added [7,8,9]. For patients with symptoms that can not be alleviated by conservative treatments, surgical intervention is further considered [10]. Among the various surgical interventions, total knee arthroplasty, unicompartmental knee arthroplasty, high tibial osteotomy (HTO), and distal femoral osteotomy are the most common types. For patients who want to preserve the knee joints and whose symptoms are caused by lower limb malalignment, HTO is a major trend [11,12,13].
Among the various HTO techniques, medial opening wedge HTO, lateral opening wedge HTO, medial closing wedge HTO, and lateral closing wedge HTO are the most common subtypes [13]. For medial compartment knee osteoarthritis with varus deformity, medial opening wedge HTO alleviates the symptoms by correcting the malalignment and redistributing the body weight loading [14, 15]. However, HTO alone does not aim to repair the structural damage of the knee. Therefore, orthobiologics, including platelet-rich plasma, bone marrow concentrate (BMC), and adipose-derived mesenchymal stem cells, have been applied for soft tissue regeneration and for their potential role in immunomodulation [16,17,18].
For medial opening wedge HTO, several studies have investigated the association of baseline demographic and radiographic features with clinical outcomes [19,20,21,22,23]. Although a few clinical studies and systematic reviews have investigated the efficacy of the combination of HTO and orthobiologics [24,25,26], few have reported and evaluated various structural, radiographic, and clinical factors that influenced the prognosis [27]. In our study, patients with medial compartment knee osteoarthritis were recruited. Medial opening wedge HTO was performed and BMC were postoperatively injected. Various demographic, structural, radiographic, and clinical factors that could potentially affect the outcomes were investigated to provide a more profound understanding of the efficacy of the combination therapy of medial opening wedge HTO and BMC.
Materials and methods
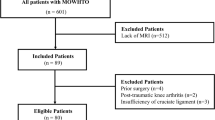
Patient enrollment
This prospective, open-label study was performed in line with the principles of the Declaration of Helsinki. The protocol was approved by the institutional review board (IRB) of Shin Kong Wu Ho-Su Memorial Hospital (Taipei, Taiwan) (IRB number: 20181006R). Prior to the recruitment of the study, the informed consent was obtained from all participants. We prospectively collected the data of 20 patients who underwent HTO in combination with BMC injection between June 2019 and May 2021. The inclusion criteria were as follows: (1) medial knee pain that could not be alleviated by non-pharmacological or pharmacological treatments; (2) radiographs showing moderate to severe medial compartment knee osteoarthritis with Kellgren-Lawrance (KL) grade II–IV; (3) patients with tibiofemoral angle less than valgus 5° or with varus deformity measured by standing anteroposterior radiographs; and (4) age between 20 and 70 years old. The exclusion criteria were as follows: (1) history of knee surgery; (2) history of stem cell transplantation in the knee; (3) other pathological diseases including rheumatoid arthritis, active knee infections, haemophilia, chronic anterior or posterior cruciate ligament instability; (4) participants with severe obesity (body mass index [BMI] ≥ 35); (5) active neuromuscular injury; (6) participants with poor health conditions that cannot tolerate surgical interventions; (7) participants with severe mental illness, developmental disability, inability to read consent forms, or unable to cooperate with the researchers; and (8) participants under pregnancy or breastfeeding. A total of 20 participants were recruited and included in the analysis. None of the participants were lost to follow-up.
Surgical procedures
In the pre-operative phase, the desired correction angle and wedge size were measured and calculated from standing radiographs. Under endotracheal tube intubation general anaesthesia, the participant was placed in the supine position on a radiolucent operating table with a tourniquet applied. A medial longitudinal skin incision was made just distal to the joint line. After the pes anserinus was detached from the tibia, the superficial medial collateral ligament was exposed. The patellar tendon was protected by anterior retraction. Medial opening wedge osteotomy was carried out with a custom-made cutting jig. After temporary fixation of the cutting jig with multiple Kirschner-pins, the sawing was performed. The open wedge was subsequently filled with bone allograft, and a proximal medial tibia locking plate (APlus™) was used to fix the osteotomy.
Preparation of the BMC
Prior to bone marrow collection, 1000–1500 IU/mL heparin was used to flush and rinse all the instruments. 1.5 ml acid-citrate-dextrose solution was then added to a 10 ml syringe as an anticoagulant. Subsequently, 8.5 ml bone marrow was slowly aspirated. A total of 30–40 ml bone marrow was extracted by iliac crest aspiration. The bone marrow aspirate was centrifuged using A-BMC (Aeon™) to autologous BMC. After the HTO operation, 4–6 ml bone marrow aspiration concentrate was injected into the knee joint.
Outcome measurement
Radiographic outcomes of anatomical femorotibial angle and posterior tibial slope angle were measured at baseline and 12 months post-intervention. The measurements of anatomical femorotibial angle and posterior tibial slope angle were demonstrated in Supplementary Fig. 1. The clinical outcomes of pain (visual analogue scale [VAS]) and global function (Western Ontario and McMaster Universities Arthritis Index [WOMAC] and The Knee injury and Osteoarthritis Outcome Score [KOOS]) were obtained at baseline, 1 month, 3 months, 6 months, and 12 months postintervention.
Statistical analysis
Shapiro–Wilk test was used to check the normality of the data. To evaluate the differences of the structural and radiological outcomes before and after HTO, paired Wilcoxon signed-rank tests and paired T tests were used for non-normally and normally distributed data, respectively. To evaluate the differences of the clinical outcomes at baseline and different follow-up time points, Friedman tests and repeated measures ANOVA (analyses of variance) were performed for non-normally and normally distributed data, respectively. For repeated measures ANOVA, Mauchly’s tests were conducted to check if the sphericity assumption was met, and Greenhouse–Geisser corrections were applied if the sphericity assumption was violated. Paired Wilcoxon signed-rank tests and paired T tests with Bonferroni multiple testing correction method were used as post hoc analyses for Friedman tests and repeated measures ANOVA, respectively. Data were reported as mean ± standard deviation (SD) or median (interquartile range [IQR]).
To model the change of the outcomes during the follow-up period, both linear and nonlinear mixed-effects models were used. The models with lower Akaike information criterion with correction for small sample sizes (AICc) and Bayesian information criterion (BIC) were considered to better fit the data. To further examine the factors that potentially influenced the treatment effects, covariates including age, sex, BMI, KL grade, femorotibial angle at baseline, posterior tibial slope angle at baseline, and symptoms severity at baseline were included in the models. Stepwise regressions, AICc, and BIC were used to select the optimal multivariate mixed-effects models. To validate the robustness of the multivariate models, the collinearity between the covariates were tested for significance. The values of correlation coefficient between 0 and 0.3 (0 and − 0.3) indicate a weak positive (negative) linear relationship, those between 0.3 and 0.7 (− 0.3 and − 0.7) indicate a moderate positive (negative) linear relationship, and those between 0.7 and 1.0 (− 0.7 and − 1.0) indicate a strong positive (negative) linear relationship [28]. The statistical analyses were all conducted in R (version 4.2.1), and the multivariate nonlinear mixed-effects models were performed using the “saemix” package.
Results
Baseline characteristics of the patients
Table 1 summarises the patient characteristics prior to the surgery. The patients comprised 12 men and 8 women with a mean age of 61.4 years old. The median Kellgren-Lawrence (KL) grade was 3. The patient had varus deformity with a mean anatomical femorotibial angle of 2.6° and a mean posterior tibial slope angle of 5.9°. The patients were generally overweight, with the mean BMI of 27.7 kg/m2. Regarding the symptoms at baseline, the median VAS was 62.5 mm, the median total WOMAC score was 40.2, and the mean total KOOS score was 210.9.
Radiographic outcomes
Both the anatomical femorotibial angle and posterior tibial slope angle showed significant improvement after medial opening wedge HTO (Table 2A). The varus deformities were corrected (p < 0.0001), with the mean femorotibial angle after surgery being 8.6° valgus. A slight increase of the mean posterior tibial slope from 5.9° to 7.6° was also observed (p = 0.04).
Improvement of clinical outcomes over the follow-up period
Based on the results of the Friedman tests and repeated measures ANOVA, VAS, WOMAC, KOOS, and their respective subscales all showed significant improvement over the follow-up period (Table 2B–D and Fig. 1). Furthermore, the improvement of the symptoms increased with the progress of time. According to the post hoc tests, most of the outcomes improved significantly compared to those at the previous follow-up time points. However, VAS and KOOS revealed no significant differences between the scores at 6 months and those at 12 months after the surgery (Tables 2B and D). The results indicated a possible plateau in pain reduction and function improvement after 6 months of follow-up.
The trajectory of clinical symptom improvement over the follow-up duration. Each dot represents an outcome measure. The trajectories of symptom improvement of the patients are connected by grey lines. The blue lines represent the mean ± standard deviation or median ± interquartile range. Abbreviations: VAS, visual analogue scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index; KOOS, The Knee injury and Osteoarthritis Outcome Score
Nonlinear mixed-effects model with asymptotic regression
Because a plateau was observed in symptom improvement as the follow-up duration increased, linear mixed-effects models may be unsuitable to fit the data. Nonlinear mixed-effects models with asymptotic regression were considered. The asymptotic regression can be described as the following equation:
\(t\) represents the duration of follow-up. \(\Delta (t)\) represents the differences between patients’ post-intervention scores at follow-up time \(t\) and baseline scores. \({a}_{0}\) represents the \(\Delta\) at \(t=0\) and should by definition be close to 0. \(a\) represents the asymptote, which indicates the extent of symptom reduction when the plateau was reached. \(r\) is the natural logarithm of the decline rate constant. To validate the superiority of the asymptotic regression, both the linear and nonlinear mixed-effects models were performed, and their AICc and BIC values were compared. We further considered other nonlinear models, including power regressions and polynomial regressions, for model fit. The nonlinear mixed-effects models with asymptotic regressions showed the best fit to the trajectory of the symptom improvement (Supplementary Table 1).
Factors associated with greater symptom improvement
Based on the asymptotic regression, we further consider the effect of other covariates, including age, sex, BMI, KL grade, anatomical femorotibial angle at baseline, posterior tibial slope angle at baseline, and symptoms severity at baseline, on modifying the asymptote, thereby influencing the extent of symptom reduction and the rate of symptom improvement. The multivariate nonlinear mixed-effects model can be described as the following equation:
\(C\) represents the covariates. A linear relationship was assumed between the covariates and their effects on \(a\), with \(\beta\) implicating the correlation coefficient of the linearity. Using the method of stepwise regression to construct multivariate nonlinear mixed-effects models (Supplementary Table 2–4), symptom severity at baseline and KL grade were significantly correlated with all the three outcomes (Table 3A–C). To more clearly visualise the effects of baseline symptom severity on the treatment outcomes, the regression lines of the patients with baseline symptom severity above and below the 50th percentiles were respectively constructed (Fig. 2). Patients with more severe symptoms at baseline experienced more rapid and greater symptom relief. Lower KL grades were also positively correlated with symptom improvement (Table 3A–C). In addition to baseline symptoms and KL grades, the WOMAC and KOOS questionnaire reported better global function improvement in patients with lower BMI (Table 3B and C), and those with more prominent baseline varus deformity tended to benefit more in VAS and KOOS outcomes (Table 3A and C). Furthermore, sex and age may play a role in influencing the extent of pain reduction (Table 3A) and physical function advancement (Table 3C), respectively.
The regression lines of the patients with baseline symptom severity above and below the 50th percentiles. Each dot represents an outcome measure. The trajectories of symptom improvement of the patients are connected by grey lines. The blue and red lines represent the regression lines. Abbreviations: VAS, visual analogue scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index; KOOS, The Knee injury and Osteoarthritis Outcome Score
To validate the robustness of the multivariate models, the correlation coefficients among the covariates were calculated and tested for significance (Supplementary Fig. 1). Although most of the covariates showed no significant collinearity, moderate to strong collinearity was observed between sex and WOMAC at baseline and between sex and KOOS at baseline. However, sex was removed from the final model of WOMAC and KOOS using stepwise regression. The collinearity was therefore unlikely to influence the results. Moderate collinearity was also observed among some of the structural and radiographic factors. The effects of these factors should be cautiously interpreted.
Adverse events
During the entire trial period, none of the patients reported infections, rejections, or other adverse events.
Discussion
In our study, the combination of medial opening wedge HTO and BMC significantly reduced pain and improved global function in patients with medial compartment knee osteoarthritis and varus deformity. The improvement of clinical symptoms reached a plateau 6 months after the surgery. Using multivariate nonlinear mixed-effects models with asymptomatic regressions, symptom severity at baseline and KL grades were significantly correlated with the prognosis. BMI, femorotibial angle, age, and sex may also play a role in influencing the extent of symptom relief.
Medial opening wedge HTO is indicated for medial compartment knee osteoarthritis with varus deformity [29, 30]. By adjusting the femorotibial angle, the weight bearing of the knee can be redistributed [14, 15]. Although no consensus has been reached in terms of the optimal alignment in medial opening wedge HTO, 8–10° vulgus of the post-operative anatomical femorotibial angle was often suggested [31, 32]. In our study, the mean anatomical femorotibial angle was adjusted to 8.6° vulgus postoperatively, which indicated an appropriate correction of the malalignment. Moreover, our study indicated that patients with more severe pre-operative varus deformity experienced better post-operative outcomes, which further confirmed the benefits of medial opening wedge HTO on medial compartmental knee osteoarthritis. In addition to femorotibial angle, a slight increase in posterior tibial slope angle by 1.7° was observed. The result is in line with a previous meta-analysis, where the posterior tibial slope angle averagely increased 2.02° (95% confidence interval, 1.38° to 2.66°) after opening wedge HTO [33].
Prior to our study, some clinical studies have revealed the potential benefits of the combination of HTO and orthobiologics injection [24, 25, 27, 34,35,36,37]. However, few have investigated factors that could potentially affect the clinical outcomes [27]. In a study by Kim et al. [27], the effects of several factors on Lysholm score and KOOS after HTO and BMC injection were evaluated. Patients with higher KL grades and over 70 years old were significantly correlated with unsatisfactory clinical outcomes, whereas the association between other factors and clinical outcomes were not observed. In our study, the analyses of KL grades yielded similar results to those of the study by Kim et al.[27] However, contrary to their findings, older age may be related to better KOOS improvement, but due to the small sample size and the potential overfit of the stepwise regression in this study, the result could not be definitively confirmed. Moreover, patients > 70 years old were not included in this study. The results of the two studies may therefore not be comparable. In addition to KL grade and age, higher BMI was associated with lesser WOMAC and KOOS improvement. Although prior studies of HTO in combination with orthobiologics did not report similar results of BMI [27], the negative impact of overweight and obesity on the prognosis has been revealed in some of the previous HTO studies [21, 23, 38,39,40].
In our study, clinical symptom severity at baseline was included as a covariate in the nonlinear mixed-effects models, which was not investigated in the study by Kim et al.[27] According to previous cross-sectional studies, KL grades were not significantly correlated with symptoms of pain and physical function at baseline in patients with knee osteoarthritis, indicating absence of collinearity between radiographic and clinical factors [41, 42]. The tests for collinearity in our study also showed similar results. Therefore, the treatment strategies can be planned based on the baseline clinical features and functional status in addition to radiographic findings [41]. Based on the nonlinear mixed-effects models, patients with more severe pain or more limited physical function at baseline experienced more rapid and greater symptom relief. To the best of our knowledge, this is the first study of HTO in combination with BMC to indicate baseline symptom severity as a prognostic factor. In clinical practice, baseline clinical symptoms may also be considered in addition to structural and radiographic features prior to the intervention.
One of the highlights of our study is the use of multivariate nonlinear mixed-effects models. Using asymptotic regressions to model the trajectory of symptom improvement, the results showed some differences from those reported by the study by Kim et al. [27]. In the study by Kim et al.[27], the authors set a threshold and dichotomised the continuous scores into satisfactory and unsatisfactory outcomes. To model the dichotomous outcomes, multivariate logistic regressions were performed. However, in this study, we believe that the changes of symptom severity from baseline to post-intervention were of more clinical significance. Therefore, we did not dichotomise the scores and used asymptotic regressions to more precisely model the continuous change of the outcomes.
Our study has some limitations. First, there was no control group; thus, the comparison between HTO alone and the combination of HTO and BMC could not be performed. Furthermore, the analyses in this study may suffer from limitations of observational investigations without control groups, including bias arising from regression to the mean. Regression to the mean is a statistical phenomenon where the patients with relatively lower symptom severity at baseline tend to experience greater symptom severity nearer the true mean in the follow-up period, and vice versa, thereby making natural variation in repeated data look like real change [43]. However, because the patients in this study all experienced improvement in the outcomes, it may be unlikely that the effect of regression to the mean contributed to the overall effect estimates. Second, the sample size of this study was relatively small, which may not yield enough statistical power. The patients also had various disease severity and different KL grades. However, we did not perform subgroup analyses based on KL grades because this may further hinder the statistical power of this study. Third, to construct the multivariate nonlinear mixed-effects models, stepwise regressions were adopted, but the method is prone to overfitting. Therefore, we only focused on the factors that showed significant correlations with multiple outcomes. For those that showed significant correlation with only one outcome, the results should be cautiously interpreted. Fourth, because of the non-randomisation design of this study, selection bias may occur. However, because there were no missing data due to loss to follow-up, incomplete data collection, or exclusion from analysis, the probability of the existence of selection bias was low. Fifth, patients with more than 70 years of age were not included in this study; therefore, our result may not be able to be generalised to patients > 70 years old.
In conclusion, this is the first clinical study of medial opening wedge HTO in combination with BMC injection to demonstrate the importance of baseline symptom severity on the prognosis. In clinical practice, we suggest that the evaluation of clinical features and functional status of the patients be more emphasised. Studies with larger sample size and longer follow-up duration are also warranted to validate the current evidence.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Jang S, Lee K, Ju JH. Recent updates of diagnosis, pathophysiology, and treatment on osteoarthritis of the knee. Int J Mol Sci. 2021;22:2619.
Primorac D, Molnar V, Rod E, Jeleč Ž, Čukelj F, Matišić V, et al. Knee Osteoarthritis: a review of pathogenesis and state-of-the-art non-operative therapeutic considerations. Genes. 2020;11:854.
Hunter DJ, Schofield D, Callander E. The individual and socioeconomic impact of osteoarthritis. Nat Rev Rheumatol. 2014;10:437–41.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis Lancet. 2019;393:1745–59.
Kulkarni K, Karssiens T, Kumar V, Pandit H. Obesity and osteoarthritis. Maturitas. 2016;89:22–8.
Prieto-Alhambra D, Judge A, Javaid MK, Cooper C, Diez-Perez A, Arden NK. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. 2014;73:1659–64.
Bruyère O, Honvo G, Veronese N, Arden NK, Branco J, Curtis EM, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49:337–50.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27:1578–89.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the Hand, hip, and knee. Arthritis rheumatol. 2020;72:220–33.
Gademan MGJ, Hofstede SN, Vliet Vlieland TPM, Nelissen RGHH, Marang-van de Mheen PJ. Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Musculoskelet Disord. 2016;17:463.
Li OL, Pritchett S, Giffin JR, Spouge ARI. High Tibial osteotomy: an update for radiologists. AJR Am J Roentgenol. 2022;218:701–12.
Liu X, Chen Z, Gao Y, Zhang J, Jin Z. High Tibial osteotomy: review of techniques and biomechanics. J Healthc Eng. 2019;2019:8363128.
Murray R, Winkler PW, Shaikh HS, Musahl V. High tibial osteotomy for varus deformity of the knee. J Am Acad Orthop Surg Glob Res Rev. 2021;5:e21.00141.
Bayam L, Erdem M, Gülabi D, Erdem AC, Uyar AÇ, Kochai A. Clinical and radiological outcomes of high tibial osteotomy with combined fixator-assisted nailing and subtubercle tibial osteotomy. Acta Orthop Traumatol Turc. 2020;54:89–96.
Ollivier B, Berger P, Depuydt C, Vandenneucker H. Good long-term survival and patient-reported outcomes after high tibial osteotomy for medial compartment osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2021;29:3569–84.
Chen FH, Tuan RS. Mesenchymal stem cells in arthritic diseases. Arthritis Res Ther. 2008;10:223.
Ha C-W, Park Y-B, Kim SH, Lee H-J. Intra-articular mesenchymal stem cells in osteoarthritis of the knee: a systematic review of clinical outcomes and evidence of cartilage repair. Arthroscopy. 2019;35:277-88.e2.
Shariatzadeh M, Song J, Wilson SL. The efficacy of different sources of mesenchymal stem cells for the treatment of knee osteoarthritis. Cell Tissue Res. 2019;378:399–410.
Birmingham TB, Giffin JR, Chesworth BM, Bryant DM, Litchfield RB, Willits K, et al. Medial opening wedge high tibial osteotomy: a prospective cohort study of gait, radiographic, and patient-reported outcomes. Arthritis Rheum. 2009;61:648–57.
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21:170–80.
Herbst M, Ahrend M-D, Grünwald L, Fischer C, Schröter S, Ihle C. Overweight patients benefit from high tibial osteotomy to the same extent as patients with normal weights but show inferior mid-term results. Knee Surg Sports Traumatol Arthrosc. 2022;30:907–17.
Primeau CA, Birmingham TB, Leitch KM, Willits KR, Litchfield RB, Fowler PJ, et al. Total knee replacement after high tibial osteotomy: time-to-event analysis and predictors. CMAJ. 2021;193:E158–66.
Wang F, Ma W, Chen J, Cong W, Zhang Y, Yu T, et al. Prognostic factors for medial open-wedge high tibial osteotomy with spacer implantation in patients with medial compartmental knee osteoarthritis. J Orthop Surg Res. 2022;17:50.
Betzler BK, Bin Muhammad Ridzwan Chew AH, Bin Abd Razak HR. Intra-articular injection of orthobiologics in patients undergoing high tibial osteotomy for knee osteoarthritis is safe and effective - a systematic review. J Exp Orthop. 2021;8:83.
Tan SHS, Kwan YT, Neo WJ, Chong JY, Kuek TYJ, See JZF, et al. Outcomes of high Tibial osteotomy with versus without mesenchymal stem cell augmentation: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9:23259671211014840.
Yao R-Z, Liu W-Q, Sun L-Z, Yu M-D, Wang G-L. Effectiveness of high Tibial osteotomy with or without other procedures for medial compartment osteoarthritis of knee: an update meta-analysis. J Knee Surg. 2021;34:952–61.
Kim YS, Suh DS, Tak DH, Chung PK, Kwon YB, Kim TY, et al. Factors influencing clinical and MRI outcomes of mesenchymal stem cell implantation with concomitant high Tibial osteotomy for Varus knee osteoarthritis. Orthop J Sports Med. 2021;9:2325967120979987.
Ratner B. The correlation coefficient: Its values range between +1/−1, or do they? J Target Meas Anal Mark. 2009;17:139–42.
Chahla J, Dean CS, Mitchell JJ, Moatshe G, Serra Cruz R, LaPrade RF. Medial opening wedge proximal Tibial osteotomy. Arthrosc Tech. 2016;5:e919–28.
Loia MC, Vanni S, Rosso F, Bonasia DE, Bruzzone M, Dettoni F, et al. High tibial osteotomy in varus knees: indications and limits. Joints. 2016;4:98–110.
Kang BY, Lee DK, Kim HS, Wang JH. How to achieve an optimal alignment in medial opening wedge high tibial osteotomy? Knee Surg Relat Res. 2022;34:3.
Sabzevari S, Ebrahimpour A, Roudi MK, Kachooei AR. High Tibial osteotomy: a systematic review and current concept. Arch Bone Jt Surg. 2016;4:204–12.
Nha K-W, Kim H-J, Ahn H-S, Lee D-H. Change in posterior Tibial slope after open-wedge and closed-wedge high Tibial osteotomy: a meta-analysis. Am J Sports Med. 2016;44:3006–13.
Jin Q-H, Chung Y-W, Na S-M, Ahn H-W, Jung D-M, Seon J-K. Bone marrow aspirate concentration provided better results in cartilage regeneration to microfracture in knee of osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc. 2021;29:1090–7.
Kim YS, Koh YG. Comparative matched-pair analysis of open-wedge high Tibial osteotomy with versus without an injection of adipose-derived mesenchymal stem cells for Varus knee osteoarthritis: clinical and second-look arthroscopic results. Am J Sports Med. 2018;46:2669–77.
Kim J-H, Kim K-I, Yoon WK, Song S-J, Jin W. Intra-articular injection of mesenchymal stem cells after high Tibial osteotomy in osteoarthritic knee: two-year follow-up of randomized control trial. Stem Cells Transl Med. 2022;11:572–85.
Magnanelli S, Screpis D, Di Benedetto P, Natali S, Causero A, Zorzi C. Open-wedge high Tibial osteotomy associated with Lipogems® intra-articular injection for the treatment of Varus knee osteoarthritis - retrospective study. Acta Biomed. 2020;91: e2020022.
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Does obesity and nicotine abuse influence the outcome and complication rate after open-wedge high tibial osteotomy? A retrospective evaluation of five hundred and thirty three patients. Int Orthop. 2014;38:55–60.
Gilat R, Patel S, Knapik DM, Evuarherhe A, Haunschild E, Parvaresh K, et al. Patient factors predictive of failure following high tibial osteotomy. J Cartilage Joint Preservation. 2021;1: 100012.
Tuhanioğlu Ü, Oğur HU, Seyfettinoğlu F, Çiçek H, Gültekin A. High tibial osteotomy in obese patients: Is successful surgery enough for a good outcome? J Clin Orthop Trauma. 2019;10:S168–73.
Cubukcu D, Sarsan A, Alkan H. Relationships between pain, function and radiographic findings in osteoarthritis of the knee: a cross-sectional study. Arthritis. 2012;2012: 984060.
Özden F, Nadiye Karaman Ö, Tuğay N, Yalın Kilinç C, Mihriban Kilinç R, Umut TB. The relationship of radiographic findings with pain, function, and quality of life in patients with knee osteoarthritis. J Clin Orthop Trauma. 2020;11(Suppl 4):S512–7.
Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. 2004;34:215–20.
Acknowledgements
The authors thank Shin Kong Wu Ho-Su Memorial Hospital for the support and for copyediting the manuscript.
Funding
This research was supported and funded by the Aeon Biotherapeutics Corporation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Hsiao-Yi Cheng, Chun-Wei Liang, Chen-Lun Chu, Hao-Wei Hsu, Sheng-Mou Hou, and Kao-Shang Shih. The operations were performed by Chen-Lun Chu, Hao-Wei Hsu, and Kao-Shang Shih. Data analysis was performed by Hsiao-Yi Cheng and Chun-Wei Liang. The first draft of the manuscript was written by Hsiao-Yi Cheng and Chun-Wei Liang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board (IRB) of Shin Kong Wu Ho-Su Memorial Hospital (Taipei, Taiwan; IRB number: 20181006R). The authors affirm that informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. Comparison of linear and nonlinear mixed-effects models. Supplementary Table 2. Stepwise regression in VAS. Supplementary Table 3. Stepwise regression in WOMAC. Supplementary Table 4. Stepwise regression in KOOS. Supplementary Figure 1. Demonstration of the measurement of anatomical femorotibial angle and posterior tibial slope angle. Supplementary Figure 2. Collinearity of the covariates in multivariate nonlinear mixed-effects models.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, HY., Liang, CW., Chu, CL. et al. Using multivariate nonlinear mixed-effects model to investigate factors influencing symptom improvement after high tibial osteotomy in combination with bone marrow concentrate injection for medial compartment knee osteoarthritis: a prospective, open-label study. BMC Musculoskelet Disord 24, 208 (2023). https://doi.org/10.1186/s12891-023-06314-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06314-z