Abstract
Objectives
The aim of this literature review was to synthesise and report current practice in evaluation and reporting of scar outcomes in hand and wrist clinical research.
Methods
A systematic search from inception to 2022 was conducted using three electronic databases. English language randomized controlled trials and observational cohort studies reporting standardised scar outcome measures and/or scar symptoms, appearance, impairment, function, or mental health outcomes in patients with hand and wrist scars were included. Two independent reviewers determined study eligibility and performed data extraction of a priori identified scar outcome domains. Data analysis included descriptive statistics and identification of discordance in taxonomy.
Results
Fifty-nine studies were included. Elective surgery cohorts were the most frequently included clinical population (n = 28; 47%) followed by burns (n = 16; 27%). Six different standardised scar outcome measures were reported by 25% of studies however only 7% of studies utilised a patient-reported measure. Scar symptoms were the most frequently reported outcome domain (81%); but taxonomy was incongruous, constructs lacked working definitions required for generalisability and outcome measurement was variable and unreported. Nineteen different measures of scar appearance and structure were reported by 30 (51%) of studies however only nine (23%) were patient-reported. Seven different hand function PROMs were reported by 25 (43%) studies. Person-centred domains including scar acceptability (12%), mental health impact (5%), and social participation (4%) were rarely reported.
Conclusions
This review highlights that evaluation and reporting of hand and wrist scar outcomes is not standardised, assessment methods and measures are under-reported and there is discordance in taxonomy. Evaluation is not person-centred, rather it is dependent on clinician assessment. Domains including scar acceptability, mental health, and social participation are rarely addressed. A stakeholder consensus derived hand and wrist scar core outcome measurement set will promote standardisation and underpin improvements in clinical research quality, transparency, and rigour.
Similar content being viewed by others
Background
Scars in the hand and wrist, whether secondary to traumatic injury or planned surgery, are common and burdensome for patients. In the United Kingdom [1] and the United States [2], approximately twenty percent of patients attending Accident & Emergency present with injuries to the hand and wrist. While not all traumatic hand injury will result in a scar, analysis of Hospital Episode Statistics (HES) in England demonstrates that more than 50% of hand trauma patients present with a wound or laceration, inevitably resulting in scar [3]. Likewise, hand scars are an unavoidable consequence of surgical treatment for pathologic or acquired hand conditions. Following planned hand surgery, up to 50% of patients report scar hyperesthesia and/or functional interference, which can persist at 2 years post-surgery [4,5,6,7]. The significant burden posed by hand scarring was recently highlighted by a British Society for Surgery of the Hand—James Lind Alliance Priority Setting Partnership, where treatment to improve scar and fibrosis formation following hand surgery or trauma was identified as a top ten research priority [8].
Scar pain and hypersensitivity, though commonly reported adverse events, have no diagnostic criteria [9, 10] and evaluation techniques are not standardised [11,12,13]. Although the physical characteristics of scar are thought to be related to hypersensitivity, there is no evidence for how the morphology of a hypersensitive scar differs from a quiescent scar [14, 15]. Persistent scar pain may be related to the extent of local tissue trauma and/or associated with psychological factors, but the underlying mechanisms are unclear and likely multifactorial [16].
While there is emerging evidence for the psychosocial impact of scars and the detrimental effect that scars may have on quality of life, this scar burden receives little attention in the literature. In “The hidden cost of skin scars; quality of life after skin scarring”, Brown et al. (2008) explored the effects of scarring. The authors report significant, multidimensional impacts of scarring; patients report feeling stigmatised, anxious, and angry because of their scars. Patients report that hand scars impact their personal and work lives and emotional well-being [17]. This work suggests the multidimensional evaluation of hand scars is crucial to capture the effects of scarring that are important to patients.
Recommendations for scar evaluation suggest a comprehensive patient-centred evaluation should assess physical characteristics, cosmetic appearance, and symptoms including the impact of scar on activity, social participation, and quality of life [18]. However, while there are numerous available scar evaluation tools, there is no universally accepted clinician-completed or patient-reported outcome measure (PROM) [12]. The first standardised scar evaluation measure, the Vancouver Scar Scale (1990) was a clinician-completed evaluation of scar physical qualities [19]. Over the past three decades, numerous scar assessment measures have been developed. In 2004, the first tool to innovatively include both the clinician and patient assessment of scar, the Patient and Observer Scar Assessment scale (POSAS), was developed [20]. Importantly, POSAS domains included patient evaluated scar physical symptoms, appearance, and global rating of scar. Further progress in patient-centred scar evaluation was made in 2009 with the development of the Patient Scar Assessment Questionnaire (PSAQ) [21], a patient completed assessment of scar appearance, symptoms, and scar consciousness. In an evaluation of scar assessment methods, Lipman et al. (2020) provide a comprehensive overview of the evolution of current scar evaluation tools. Despite advances in scar evaluation, the authors conclude that current tools fail to fully capture the impact of scarring on patients’ function, psychosocial health, and quality of life [22].
The impact of scarring is multidimensional; therefore, it may be unrealistic to expect that one scar evaluation measure can adequately capture the numerous outcome domains of importance to people with scars. However, at present, a consensus-derived core outcome set [23] for the evaluation of hand and wrist scars is lacking. Given the lack of concurrence in scar evaluation, a review exploring the evaluation and reporting of scar outcomes in the hand and wrist provides important insight and is warranted. This research aimed to explore the state-of-the-art of current practice in evaluation and reporting of scar outcomes in hand and wrist clinical research, identify discordance in taxonomy and highlight domains for inclusion in future scar reporting consensus activities [24].
Methods
A study design of ‘state-of-the-art’ literature review was used to provide a synthesis of current practice and identify priorities for future research, as opposed to identifying treatment uncertainties or making recommendations for care [25]. Systematic methods were employed, however, as the review objective was to generate a descriptive summary of current reporting practice, critical appraisal of risk of bias of the included literature would have been inappropriate and was therefore omitted. PRISMA guidelines for reporting of systematic reviews were followed [26]. The review protocol was registered on Open Science Framework https://osf.io/74an6/.
A search strategy (Supplementary data 1) was developed and piloted by the review team with the guidance of an NHS Support Librarian, Imperial College London. Medline, Embase and CINAHL databases were initially searched from inception until May 2020. The literature search was thereafter updated to locate additional reports published until 2nd December 2022. English language, full primary research reports (randomised controlled trials [RCTs] and observational studies [cohort and repeated methods]) in humans were included. There were no age exclusions. Evidence syntheses, abstracts and conference proceedings, case reports, case series, study protocols, narrative reviews, and non-English language papers were excluded.
Two reviewers (DLK; TCB) independently performed title and abstract screening and any disagreements were discussed and taken to a third reviewer (DF) if consensus was not reached. Following the initial screening, full text manuscripts were screened against review inclusion and exclusion criteria. Two reviewers independently performed data extraction using a piloted proforma (Supplementary data 2). Study participant characteristics including gender, age (child or adult), clinical condition, and procedure or intervention were recorded. Study characteristics including year of publication, timepoint of scar assessment, scar evaluation domains, and relevant outcome measures were extracted. Data synthesis included the generation of descriptive statistics and identification of variability in taxonomy pertaining to scar outcomes.
Results
Study characteristics
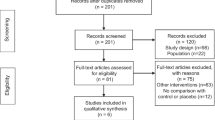
Results of the literature search and each stage of literature screening are reported in Fig. 1. A total of 424 records were identified in the initial search, of which 54 were included. An additional 56 records were identified in the search update, with five reports included for a total of 59 reports included in the amalgamated synthesis. Design parameters, reported scar outcome domains, and relevant assessment tools for included studies are reported in Supplementary data 3. Included studies were RCTs [n = 22] and cohort studies [n = 37]. Publication dates ranged from 1993 to 2022. Data collection was retrospective in ten studies and prospective in 49 studies. Study outcomes were reported at multiple time points, with 20% of studies evaluating outcomes at three months; 31% at one year and 20% at two years or longer (Fig. 2). The plan for the evaluation of scar outcomes was reported in the study methods in 51 (86%) studies. Scar evaluation was by patient report in ten (17%) studies; patient and clinician assessment in 34 (58%) studies; clinician assessment in fourteen (24%) studies and by a carer in one (2%) study.
Participants
The fifty-nine studies comprised 5972 participants: [RCTs n = 1748; cohort studies n = 4224]. Elective surgery cohorts n = 28 (47%) were the most frequently included clinical population [carpal tunnel release n = 18; Dupuytren’s excision n = 3; trigger finger/thumb n = 3; basal thumb joint osteoarthritis n = 2; ganglion excision n = 1; Dequervain’s release n = 1] followed by patients with burns n = 16 (27%). Less frequently, studies were conducted in patients following trauma or fracture (n = 8; 14%); patients undergoing treatment of scar (n = 2; 3%); patients undergoing skin grafting secondary to skin cancer (n = 2; 3%) and patients with congenital hand conditions (n = 2; 3%). One study (2%) investigated scar outcomes in a cohort comprising patients with scarring secondary to burns, traumatic injury, and surgical scarring. Six studies reported scar outcomes in children, six studies included both children and adults and forty-seven included adults. One study investigating arthroplasty for basal thumb joint arthritis included females only [27], all other studies included both males and females.
Standardized scar outcome measures
A standardised scar outcome measure was included in 15 (25%) studies (Table 1); with three (5%) studies including two standardised scar assessment tools [28,29,30]. Only five (8%) studies utilised a patient-reported standardised scar outcome measure (PROM).
Scar physical symptoms
Physical symptoms were the most frequently reported outcome domain (81% of studies); however, taxonomy and outcome measurement were variable (Table 2). Pain was reported as a physical symptom in 20 (34%) studies and quantified or qualified using PROMS or visual and verbal rating scales, however five of the 24 studies did not elaborate on the method of pain evaluation. Scar sensitivity or hypersensitivity was reported in nine studies; however, a working definition of scar hypersensitivity was not provided. Scar tenderness was reported in eight studies; again, it is unclear how tenderness was defined and whether scar tenderness is a construct independent of hypersensitivity. Seven studies reported itch as a physical symptom. Finally, one study reported scar comfort, but a working definition of the construct was not provided.
Scar appearance & physical structure
Nineteen different measures of scar appearance and structure, in various constructs, were reported by 30 (51%) studies (Table 3). Only nine of 39 (23%) physical appearance measures were patient-reported. Scar appearance was evaluated with four different standardised outcome measures which incorporated varying appearance constructs of interest; the clinician completed Vancouver Scar Scale (VSS) was the most frequently reported standardised scar appearance assessment measure (n = 11) studies. The constructs of scar appearance [57, 75, 84]; cosmesis [45, 56, 85] and aesthetic outcome [38, 75] were reported in six studies. It is unclear however, given the discordance in taxonomy, whether a common scar domain was being evaluated and reported.
Hand function assessment
Standardised patient-reported outcome measures (PROMs) of hand function were reported in 23 (39%) of studies, with three studies reporting both a disease specific and generic hand function outcome measure [48, 52, 76]. The Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH) [80], was the most frequently implemented hand function PROM, reported in 12 (20%) of studies. The Boston Carpal Tunnel Questionnaire, a disease-specific measure of self-reported symptom severity & functional status [79], was reported in six studies. The Michigan Hand Questionnaire (MHQ), evaluating unilateral & bilateral hand function, pain, work performance, aesthetics & satisfaction, was reported by four studies. The QuickDASH [91] and the Patient Evaluation Measure (PEM) [83], comprising the components of the patients’ opinion on the delivery of care, hand health profile & overall assessment, were both reported by two studies. The Patient-rated Wrist and Hand Evaluation (PRWHE) [92] was reported by one study. Finally, the Canadian Occupational Performance Measure (COPM) [93], including outcomes of self-care, productivity & leisure, was reported by one study.
In addition to patient reported measures of function, impairment measures were commonly reported. Hand grip strength, as assessed with hand dynamometry, was the most frequently reported measure of hand impairment (n = 22 [37%]). Range of motion, as assessed with goniometry, was reported by 15 (25%) studies. Range of motion assessment and reporting varied, based on the clinical cohort and research question of interest. For example, in an elective surgery cohort of patients undergoing Dupuytren’s surgery, total active motion of the affected digits was reported [88]. In contrast, in patients undergoing thumb reconstruction, range of motion of the individual thumb joints was reported [75].
Sensory function was reported by nine (15%) of studies, including the use of Semmes–Weinstein monofilaments [66,67,68, 88] and/or two-point discrimination [33, 38, 45, 63, 64, 66,67,68]. Sensory testing protocols varied, with testing conducted in the area of scarring in some cohorts [33, 38, 45] and within the sensory distribution of the affected digits in others [66, 68, 88]. Rarely, standardised measures of hand functional dexterity, including the Purdue Pegboard (Tiffin and Asher [94]) [68]; Jebsen-Taylor Hand function Test (Jebsen et al. [95]) [68] and Carroll Upper Limb Functional Evaluation (Carroll [96]) [36] were reported.
Scar acceptability / patient satisfaction
Measures of scar acceptability or satisfaction with scar outcome were included in seven (12%) studies. One study reported patient-rated acceptability using a visual analogue scale [78]. Satisfaction with outcome was assessed using willingness to pay as a surrogate measure [28]; satisfaction with appearance as a proxy measure [84]; and with patient-completed Likert scales [53, 97]. In one study, patient satisfaction was physician-rated [98] and in one study the methods for ascertaining satisfaction were not reported [33].
Mental health impact & participation restriction
The impact of scarring in the hand or wrist on patients’ mental health was included by three studies. In paediatric patients with burns, self-esteem was evaluated using the Piers-Harris Children’s Concept Scale [99] by Abdullah et al. [100]. Psychological function was evaluated [36] with the relevant scale of the abbreviated Burn Specific Health Scale [101] and psychosocial impact [46] was evaluated with the relevant SCAR-Q scale [44]. Participation restriction secondary to scarring and/or the participants underlying clinical condition was evaluated by two (3%) studies. In patients undergoing fasciectomy for Dupuytren’s disease, Engstrand et al. [88] evaluated patient-reported safety and social issues including concern about the appearance of the hand and avoiding use of the hand in social contexts with a 10-point visual analogue scale. In patients with traumatic fingertip injuries Schultz et al. [45] evaluated use of the hand in everyday life using a binary rating scale.
Discussion
This state-of-the-art literature review was undertaken to identify, synthesise and report on current methods for evaluation and reporting of scar outcomes in hand and wrist clinical research, whilst identifying discordance in taxonomy. Additionally, it was aimed to identify relevant scar associated domains for inclusion in future scar reporting consensus activities. Fifty-nine reports, published between 1993 and 2022, were included in the synthesis.
We identified that hand scar evaluation and reporting lack standardisation essential for evidence synthesis. There is limited use of standardised scar outcome measures; where standardised measures are utilised, there is variation. There is disparity and inconsistency in outcome domains included in hand scar evaluation. There is discordance in relevant taxonomy and outcome measurement of scar symptoms, appearance, and physical structure. Hand scar evaluation is not person-centred, as patient-reported outcomes are seldom utilised and domains including scar acceptability, mental health impact, and social participation are rarely reported. We identified the following scar associated domains relevant for inclusion in future scar reporting consensus activities: physical symptoms, appearance, physical structure, functional impairment, participation restriction, mental health impact, acceptability, and satisfaction.
Six different standardised scar outcome measures were utilised by fifteen of the fifty-nine included hand and wrist clinical research studies; the Vancouver Scar Scale [19], the Patient and Observer Scar Assessment Scale (POSAS) [20], the Silverberg Scar Mobility Rating Scale [40], Matching Assessment of Scars and Photographs (MAPS) [42], the University of North Carolina Scar Scale (UNC4P) [28] and SCAR-Q [44]. It is unclear why only 25% of studies included a standardised scar outcome measure; it may be that scar outcomes were not identified as a study priority or perhaps there was no available measure deemed fit for purpose at the time of the investigation.
Physical symptoms secondary to scar was the most frequently reported scar outcome domain. However, taxonomy for symptoms was variable and included pain, sensitivity, hypersensitivity, and comfort, without relevant working definitions. Furthermore, within each reported symptom parameter, this was discordance in the method of outcome evaluation. While pain was reported by one third of included studies, assessment predominantly focused on pain intensity. Important persistent pain parameters, including pain interference, frequency, nature, and quality were under-reported [102]. A more robust and uniform approach to the evaluation of scar symptoms will underpin improvements in scar clinical trials and may support the elucidation of mechanisms driving persistent scar pain.
Scar sensitivity, hypersensitivity, or tenderness, while commonly reported, lack working definitions as required to ensure conformity and consistency in assessment. The International Association for the Study of Pain (IASP [103]) define hyperesthesia as an increased sensitivity to stimulation, including touch and thermal stimuli, that may or may not be painful. As such, hyperesthesia includes both allodynia and hyperalgesia and may in fact be the working definition of scar hypersensitivity. Standardising taxonomy for the description of an individuals’ scar sensory experience, or physical symptoms secondary to scar, is required to support future evidence synthesis.
The evaluation of scar physical structure or morphology, as distinct from scar cosmetic appearance, lacks distinction. While it might be presumed that the patient is the best judge of the appearance of their scar, this review identified that only 23% of included scar appearance measures were patient-reported. The patient AND observer completed POSAS [20] was reported by three studies. However, the patient-completed POSAS domains are specific to scar structure and symptoms and do not include a patient-derived assessment of scar cosmesis. Importantly, it has also been reported for the POSAS that patient and observer ratings do not concur; patient ratings are poorer than those of clinicians, highlighting the imperative of patient reported scar outcomes [12]. SCAR-Q, developed in 2018 [44], was reported by one study [46]. The SCAR-Q appearance scale quantifies how much a patient is bothered by the appearance of their scar, including scar length, width, colour, shape, and size. The distinction between patient-rated scar appearance and the bothersomeness of appearance may be an important one, as it might be expected that those who are more bothered will possibly report lower quality of life and be more apt to seek secondary scar modification treatments.
We identified seven standardised hand function PROMs, reported by 39% of studies. In addition, impairment measures such as hand grip strength were reported by 37% of studies, range of motion (25%), sensory function (15%) and dexterity (5%). While these measures are specific to function and impairment of the hand and were not implemented to capture the functional impact of scar per se, clearly scarring in the hand and wrist can be deleterious to hand function. Whereas consensus group work to identify outcomes for the evaluation of hand function after burn injuries proposed hand function be assessed with the QuickDASH PROM [91] it is not clear how this decision was derived [104]. Furthermore, although the QuickDASH is widely used internationally, there are questions as to the robustness of the evidence supporting the measure’s psychometric properties [105,106,107]. At present, there is no evidence synthesis evaluating the clinical relevance, reliability, or responsiveness of hand function PROMs or hand impairment measures in a clinical population with hand and wrist scars; this clearly warrants further investigation.
Previous qualitative research in patients with scarring in the hand and wrist identified scar acceptability and impact on mental health and social function as important scar outcome domains [17]. However, these domains received scant attention in the literature included in the present review. Scar acceptability or satisfaction with scarring was reported by only 12% of studies. Of the 59 included studies, only three studies reported scar impact on mental health and two on social function. There is growing evidence that patients report detrimental mental health effects and impaired social participation secondary to scarring in the hand and wrist [108]. To mediate for the negative impact of scarring and improve quality of life, patients commonly seek out camouflaging treatments [109,110,111]. Whereas validated patient-self report measures of adjustment to issues of appearance, such as the Derriford Appearance Scale (DAS24) [112] are available, such measures are not widely implemented in patients with scarring in the hand and wrist. Further research is required to assess the psychometric properties, clinical feasibility, and patient-rated acceptability of such measures.
Previous reviews have evaluated the feasibility and psychometric properties [12] and clinical relevance [22] of available scar outcome measurement tools. This review adds a descriptive synthesis of current practice in scar evaluation and reporting in hand and wrist clinical research. It is anticipated this work will highlight the substantial discordance between the patient reported impact of scarring [17] and current methods of scar evaluation and reporting in hand and wrist clinical research, thereby promoting a more patient-centered approach in future studies. Importantly, the findings of this review underpin the need for a shared taxonomy and standardisation in hand and wrist scar assessment as required for future evidence synthesis.
This state-of the-art literature review took a systematic approach to reviewing the scar evaluation and reporting literature. Search strategy was developed with the support of an information specialist and double-reviewer screening and extraction were employed. For transparency, the full data set is included as supplemental data. Nonetheless, several design weaknesses require consideration. Given the broad search inclusion criteria, the review includes a vast number of clinical cohorts, as well as children and adults. Therefore, and importantly, evaluation and reporting practice in particular cohorts cannot be discerned. Comprehensive demographics including ethnicity and socioeconomic status were not reported for the included clinical cohorts, therefore the generalisability of our findings is impeded. Lastly, we did not report the country where studies were conducted, so possible geographical differences in practice cannot be detected.
Conclusion
The evaluation and reporting of hand and wrist scar outcomes is not standardised, there is under-reporting of assessment methods, and there is significant discordance in taxonomy which hinders evidence synthesis. Outcome evaluation is not patient-centred but rather is dependent on clinician assessment. Domains including scar acceptability and the impact of scarring on quality of life are rarely addressed. A consensus, stakeholder (patients, clinicians, researchers) derived hand and wrist scar core outcome measurement set will promote standardisation, underpin improvements in clinical research quality, transparency, and rigour, and provide a solid basis for advances in evidence-based treatment.
Availability of data and materials
The study data extraction sheet and all extracted data have been shared as supplementary material.
Abbreviations
- BCTQ:
-
Boston Carpal Tunnel Questionnaire
- COPM:
-
Canadian Occupational Performance Measure
- DASH:
-
Disabilities of the arm, shoulder and hand
- MAPS:
-
Matching Assessment of Scars and Photographs
- MHQ:
-
Michigan Hand Assessment Questionnaire
- PEM:
-
Patient Evaluation Measure
- PROMs:
-
Patient reported outcome measures
- POSAS:
-
Patient and Observer Scar Assessment Scale
- PRWHE:
-
Patient-rated Wrist and Hand Evaluation
- RCT:
-
Randomised controlled trial
- UNC4P:
-
University of North Carolina Scar Scale
- VAS:
-
Visual analogue scale
References
BSSH. Hand Surgery in the UK. London: Royal College of Surgeons of England; 2017.
Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand. 2012;7(1):18–22.
Manley OWG, Wormald JCR, Furniss D. The changing shape of hand trauma: an analysis of Hospital Episode Statistics in England. J Hand Surg Eur. 2019;44(5):532–6.
Citron ND, Bendall SP. Local symptoms after open carpal tunnel release. A randomized prospective trial of two incisions. J Hand Surg. 1997;22(3):317–21.
Boya H, Ozcan O, Oztekin HH. Long-term complications of open carpal tunnel release. Muscle Nerve. 2008;38(5):1443–6.
Ritchie JF, Belcher HJ. A comparison of trapeziectomy via anterior and posterior approaches. J Hand Surg Eur. 2008;33(2):137–43.
Kennedy DL, Ridout D, Lysakova L, Vollert J, Alexander CM, Rice ASC. The association of sensory phenotype and concomitant mood, sleep and functional impairment with the outcome of carpal tunnel surgery. BMC Musculoskelet Disord. 2021;22(1):962.
Karantana A, Davis T, Kennedy D, Larson D, Furniss D, Grindlay DJ, et al. Common hand and wrist conditions: creation of UK research priorities defined by a James Lind Alliance Priority Setting Partnership. BMJ Open. 2021;11(3):e044207.
Abd-Elsayed A, Pope J, Mundey DA, Slavin KV, Falowski S, Chitneni A, et al. Diagnosis, treatment, and management of painful scar: a narrative review. J Pain Res. 2022;15:925–37.
Tos P, Crosio A, Pugliese P, Adani R, Toia F, Artiaco S. Painful scar neuropathy: principles of diagnosis and treatment. Plastic Aesthetic Res. 2015;2(4):156–64.
Mundy LR, Miller HC, Klassen AF, Cano SJ, Pusic AL. Patient-reported outcome instruments for surgical and traumatic scars: a systematic review of their development, content, and psychometric validation. Aesthetic Plast Surg. 2016;40(5):792–800.
Choo AMH, Ong YS, Issa F. Scar assessment tools: how do they compare? Front Surg. 2021;8(206):1–7.
Ferriero G, Di Carlo S, Ferriero A, Salgovic L, Bravini E, Sartorio F, et al. Post-surgical scar assessment in rehabilitation: a systematic review. Phys Ther Rehabil. 2015;2(2):1–5.
Davidson JM. Wound repair. J Hand Ther. 1998;11(2):80–94.
Ireton JE, Unger JG, Rohrich RJ. The role of wound healing and its everyday application in plastic surgery: a practical perspective and systematic review. Plast Reconstr Surg Glob Open. 2013;1(1):1–10.
Bijlard E, Uiterwaal L, Kouwenberg CA, Mureau MA, Hovius SE, Huygen FJ. A systematic review on the prevalence, etiology, and pathophysiology of intrinsic pain in dermal scar tissue. Pain Phys. 2017;20(2):1–13.
Brown BC, McKenna SP, Siddhi K, McGrouther DA, Bayat A. The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg. 2008;61(9):1049–58.
Vercelli S, Ferriero G, Sartorio F, Stissi V, Franchignoni F. How to assess postsurgical scars: a review of outcome measures. Disabil Rehabil. 2009;31(25):2055–63.
Sullivan T, Smith J, Kermode J, McIver E, Courtemanche DJ. Rating the burn scar. J Burn Care Rehabil. 1990;11(3):256–60.
Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstruct Surg. 2004;113(7):1960–5. discussion 6-7.
Durani P, McGrouther DA, Ferguson MW. The patient scar assessment questionnaire: a reliable and valid patient-reported outcomes measure for linear scars. Plast Reconstr Surg. 2009;123(5):1481–9.
Lipman K, Wang M, Berthiaume E, Holloway J, Da Lio A, Ting K, et al. Evaluating current scar assessment methods. Ann Plast Surg. 2020;84(2):222–31.
Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med. 2011;8(1):e1000393.
Kennedy D, Chism-Balangue T, Furniss D. Development of a Core Outcome Measurement Set for the Evaluation of Scars in the Hand & Wrist (COSSH): Core Outcome Measures in Effectiveness Trials (COMET); 2020 [Available from: https://comet-initiative.org/Studies/Details/1503
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Vermeulen GM, Spekreijse KR, Slijper H, Feitz R, Hovius SER, Selles RW. Comparison of arthroplasties with or without bone tunnel creation for thumb basal joint arthritis: a randomized controlled trial. J Hand Surg Am. 2014;39(9):1692–8.
Hultman CS, Friedstat JS, Edkins RE, Cairns BA, Meyer AA. Laser resurfacing and remodeling of hypertrophic burn scars: the results of a large, prospective, before-after cohort study, with long-term follow-up. Ann Surg. 2014;260(3):519–32.
Schiefer JL, Arens E, Grigutsch D, Rath R, Hoffmann A, Fuchs PC, et al. A prospective intra-individual evaluation of silk compared to Biobrane for the treatment of superficial burns of the hand and face. Burns. 2017;43(3):539–48.
Schiefer JL, Rath R, Ahrens E, Grigutsch D, Gräff I, Stromps J-P, et al. Evaluation of scar quality after treatment of superficial burns of the hands and face with Dressilk or Biobrane-An intra-individual comparison. Burns. 2018;44(2):305–17.
Chan QE, Barzi F, Harvey JG, Holland AJA. Functional and cosmetic outcome of full- versus split-thickness skin grafts in pediatric palmar surface burns: a prospective, independent evaluation. J Burn Care Res. 2013;34(2):232–6.
Johnston P, Larson D, Clark IM, Chojnowski AJ. Metalloproteinase gene expression correlates with clinical outcome in Dupuytren’s disease. J Hand Surg. 2008;33(7):1160–7.
Lumenta DB, Kitzinger HB, Beck H, Frey M. Long-term outcomes of web creep, scar quality, and function after simple syndactyly surgical treatment. J Hand Surg. 2010;35(8):1323–9.
Mohammadi AA, Bakhshaeekia AR, Marzban S, Abbasi S, Ashraf AR, Mohammadi M, et al. Early excision and skin grafting versus delayed skin grafting in deep hand burns (a randomised clinical controlled trial). Burns. 2011;37(1):36–41.
Schulz A, Shoham Y, Rosenberg L, Rothermund I, Perbix W, Fuchs PC, et al. Enzymatic versus traditional surgical debridement of severely burned hands: a comparison of selectivity, efficacy, healing time, and three-month scar quality. J Burn Care Res. 2017;38(4):e745–55.
Shang F, Hou Q. Effects of allogenic acellular dermal matrix combined with autologous razor-thin graft on hand appearance and function of patients with extensive burn combined with deep hand burn. Int Wound J. 2021;18(3):279–86.
Zacharevskij E, Baranauskas G, Varkalys K, Rimdeika R, Kubilius D. Comparison of non-surgical methods for the treatment of deep partial thickness skin burns of the hand. Burns. 2018;44(2):445–52.
Zuidam JM, Coert JH, Hofer SOP. Closure of the donor site of the free radial forearm flap: a comparison of full-thickness graft and split-thickness skin graft. Ann Plast Surg. 2005;55(6):612–6.
Verhaeghe E, Ongenae K, Bostoen J, Lambert J. Nonablative fractional laser resurfacing for the treatment of hypertrophic scars: A randomized controlled trial. Dermatologic Surgery. 2013;39(3 PART 1):426–34.
Silverberg R, Johnson J, Moffat M. The effects of soft tissue mobilization on the immature burn scar: results of a pilot study. J Burn Care Rehabil. 1996;17(3):252–9.
Donnelly CJ, Wilton J. The effect of massage to scars on active range of motion and skin mobility. Brit J Hand Ther. 2002;7(1):5–11.
Masters M, McMahon M, Svens B. Reliability testing of a new scar assessment tool, Matching Assessment of Scars and Photographs (MAPS). J Burn Care Rehabil. 2005;26(3):273–84.
Jarrett M, McMahon M, Stiller K, Jarrett M, McMahon M, Stiller K. Physical outcomes of patients with burn injuries–a 12 month follow-up. J Burn Care Res. 2008;29(6):975–84.
Klassen AF, Ziolkowski N, Mundy LR, Miller HC, McIlvride A, DiLaura A, et al. Development of a new patient-reported outcome instrument to evaluate treatments for scars: The SCAR-Q. Plast Reconstr Surg Glob Open. 2018;6(4): e1672.
Ziolkowski NI, Behman R, Klassen AF, Fish JS, Mundy LR, She RW, et al. Determining the Independent risk factors for worse SCAR-Q scores and future scar revision surgery. Plast Reconstr Surg. 2021;148(1):203–12.
Forward DP, Singh AK, Lawrence TM, Sithole JS, Davis TRC, Oni JA. Preservation of the ulnar bursa within the carpal tunnel: does it improve the outcome of carpal tunnel surgery? A randomized, controlled trial. J Bone Joint Surg Am. 2006;88(11):2432–8.
Gong HS, Oh JH, Kim WS, Kim SH, Rhee SH, Baek GH. The effect of dividing muscles superficial to the transverse carpal ligament on carpal tunnel release outcomes. J Hand Surg. 2011;36(9):1475–81.
Goransson I, Cederlund R. A study of the effect of desensitization on hyperaesthesia in the hand and upper extremity after injury or surgery. Hand Ther. 2011;16:12–8.
Kim JK, Kim YK. Predictors of scar pain after open carpal tunnel release. J Hand Surg. 2011;36(6):1042–6.
Wong KC, Hung LK, Ho PC, Wong JMW. Carpal tunnel release. A prospective, randomised study of endoscopic versus limited-open methods. J Bone Joint Surg Brit Vol. 2003;85(6):863–8.
Kang HJ, Koh IH, Lee TJ, Choi YR. Endoscopic carpal tunnel release is preferred over mini-open despite similar outcome: A randomized trial hand. Clin Orthop Relat Res. 2013;471(5):1548–54.
Mohammadi AA, Foroutan A, Mohammadi S, Zardosht M. Evaluation of patients’ satisfaction and functional outcome of dorsal hand unit reconstruction in burn patients in Shiraz, Southern Iran. J Burn Care Res. 2018;39(4):572–9.
Rusciani L, Rossi G, Bono R. Use of cryotherapy in the treatment of keloids. J Dermatol Surg Oncol. 1993;19(6):529–34.
Siegmeth AW, Hopkinson-Woolley JA. Standard open decompression in carpal tunnel syndrome compared with a modified open technique preserving the superficial skin nerves: a prospective randomized study. J Hand Surg. 2006;31(9):1483–9.
Leclère FM, Kohl S, Varonier C, Unglaub F, Vögelin E. Range of motion, postoperative rehabilitation and patient satisfaction in MCP and PIP joints affected by Dupuytren Tubiana stage 1–3: collagenase enzymatic fasciotomy or limited fasciectomy? A clinical study in 52 patients. Arch Orthop Trauma Surg. 2018;138(11):1623–31.
Ben-Amotz O, Pezeshk RA, Sammer DM, Cheng J. Arthroscopic ganglionectomy in the pediatric population. Plast Reconstr Surg. 2018;142(5):718e-21e.
Schultz J, Wruck JE, Trips E, Pfeiffer R, Grahlert X, Munchow S, et al. Semi-occlusive management of fingertip injuries with finger caps: A randomized controlled trial in children and adults. Medicine (United States). 2022;101(27):E29324.
Finsen V, Andersen K, Russwurm H. No advantage from splinting the wrist after open carpal tunnel release: a randomized study of 82 wrists. Acta Orthop Scand. 1999;70(3):288–92.
Richard MJ, Wartinbee DA, Riboh J, Miller M, Leversedge FJ, Ruch DS. Analysis of the complications of palmar plating versus external fixation for fractures of the distal radius. J Hand Surg. 2011;36(10):1614–20.
Waitayawinyu T, Numnate W, Boonyasirikool C, Niempoog S. Outcomes of endoscopic carpal tunnel release with ring finger flexor digitorum superficialis opponensplasty in severe carpal tunnel syndrome. J Hand Surg. 2019;44(12):1095.
Will R, Lubahn J. Complications of open trigger finger release. J Hand Surg. 2010;35(4):594–6.
Abdullah AF, Wolber PH, Ditto IEW, Kline DG, Tindall SC, McGillicuddy JE. Sequelae of carpal tunnel surgery: rationale for the design of a surgical approach. Neurosurgery. 1995;37(5):931–6.
Weber RA, Rude MJ. Clinical outcomes of carpal tunnel release in patients 65 and older. J Hand Surg. 2005;30(1):75–80.
Weber RA, DeSalvo DJ, Rude MJ. Five-year follow-up of carpal tunnel release in patients over age 65. J Hand Surg. 2010;35(2):207–11.
Hallock GG, Lutz DA. Prospective comparison of minimal incision “open” and two-portal endoscopic carpal tunnel release. Plast Reconstr Surg. 1995;96(4):941–7.
Luria S, Waitayawinyu T, Trumble TE. Endoscopic revision of carpal tunnel release. Plast Reconstr Surg. 2008;121(6):2029–34.
Nakamichi K, Tachibana S, Yamamoto S, Ida M. Percutaneous carpal tunnel release compared with mini-open release using ultrasonographic guidance for both techniques. J Hand Surg. 2010;35(3):437–45.
Trumble TE, Diao E, Abrams RA, Gilbert-Anderson MM. Single-portal endoscopic carpal tunnel release compared with open release: A prospective, randomized trial. J Bone Joint Surg-Ser A. 2002;84(7):1107–15.
Hamed AR, Makki D, Chari R, Packer G. Double- versus single-incision technique for open carpal tunnel release. Orthopedics. 2009;32(10):733.
Koopman JE, Hundepool CA, Duraku LS, Smit JM, Zuidam JM, Selles RW, et al. Complications and functional outcomes following trigger finger release: a cohort study of 1879 patients. Plast Reconstr Surg. 2022;150(5):1015–24.
Manz S, Wolf MB, Leclre FM, Hahn P, Bruckner T, Unglaub F. Capsular imbrication for posttraumatic instability of the distal radioulnar joint. J Hand Surg. 2011;36(7):1170–5.
Davis TRC, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg. 2004;29(6):1069–77.
Dias JJ, Wildin CJ, Bhowal B, Thompson JR. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005;87(10):2160–8.
Brown RA, Gelberman RH, Seiler JG 3rd, Abrahamsson SO, Weiland AJ, Urbaniak JR, et al. Carpal tunnel release. A prospective, randomized assessment of open and endoscopic methods. J Bone Joint Surg American Vol. 1993;75(9):1265–75.
Dijkman RR, Selles RW, Hulsemann W, Mann M, Habenicht R, Hovius SER, et al. A matched comparative study of the Bilhaut procedure versus resection and reconstruction for treatment of radial polydactyly types II and IV. J Hand Surg. 2016;41(5):e73–83.
Logli AL, Bear BJ, Schwartz EG, Korcek KJ, Foster BJ. A prospective, randomized trial of splinting after minicarpal tunnel release. J Hand Surg. 2018;43(8):775.
Ebid A, Ibrahim A, Omar M, Baky A, Ebid AA, Ibrahim AR, et al. Long-term effects of pulsed high-intensity laser therapy in the treatment of post-burn pruritus: a double-blind, placebo-controlled, randomized study. Lasers Med Sci. 2017;32(3):693–701.
Kumar K. Outcome of longitudinal versus transverse incision in de Quervain’s disease and its implications in Indian population. Musculoskelet Surg. 2016;100(1):49–52.
Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–92.
Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Indust Med. 1996;29(6):602–8.
Majeski CJ, Johnson JA, Davison SN, Lauzon CJ. Itch Severity Scale: a self-report instrument for the measurement of pruritus severity. Br J Dermatol. 2007;156(4):667–73.
Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg. 1998;23(4):575–87.
Macey AC, Burke FD, Abbott K, Barton NJ, Bradbury E, Bradley A, et al. Outcomes of hand surgery. British Society for Surgery of the Hand. J Hand Surg. 1995;20(6):841–55.
Jennings TA, Keane JC, Varma R, Walsh SB, Huang CC. Observation of dog-ear regression by anatomical location. Dermatol Surg. 2017;43(11):1367–70.
Brown RL, Greenhalgh DG, Warden GD. Iron burns to the hand in the young pediatric patient: a problem in prevention. J Burn Care Rehabil. 1997;18(3):279–82.
Monstrey S, Beele H, Kettler M, Van Landuyt K, Blondeel P, Matton G, et al. Allogeneic cultured keratinocytes vs. cadaveric skin to cover wide-mesh autogenous split-thickness skin grafts. Ann Plast Surg. 1999;43(3):268–72.
Saving J, Severin Wahlgren S, Olsson K, Enocson A, Ponzer S, Skoldenberg O, et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: a randomized controlled trial. J Bone Joint Surg-Am Vol. 2019;101(11):961–9.
Engstrand C, Krevers B, Nylander G, Kvist J. Hand function and quality of life before and after fasciectomy for dupuytren contracture. J Hand Surg. 2014;39(7):1333.
Nguyen DQA, Potokar TS, Price P. An objective long-term evaluation of Integra (a dermal skin substitute) and split thickness skin grafts, in acute burns and reconstructive surgery. Burns. 2010;36(1):23–8.
Kloeters O, Ulrich D, Bloemsma G, Houdt C, Ulrich DJO, van Houdt CIA. Comparison of three different incision techniques in A1 pulley release on scar tissue formation and postoperative rehabilitation. Arch Orthop Trauma Surg. 2016;136(5):731–7.
Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative G. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am Vol. 2005;87(5):1038–46.
MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9(2):178–83.
Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther. 1990;57(2):82–7.
Tiffin J, Asher EJ. The Purdue Pegboard: norms and studies of reliability and validity. J Applied Psych. 1948;32:234–47.
Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. Objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50(6):311–9.
Carroll D. A quantitative test of upper extremity function. J Chronic Dis. 1965;18:479–91.
Abdel Fattah HAH, El-Mahy MM, Atiyya AN, Diab RA, Aly AM. Reliability of propeller flaps in post-traumatic reconstruction of wrist and hand defects. Eur. 2021;31(2):375–81.
Frame JD, Still J, Lakhel-LeCoadou A, Carstens MH, Lorenz C, Orlet H, et al. Use of dermal regeneration template in contracture release procedures: a multicenter evaluation. Plast Reconstr Surg. 2004;113(5):1330–8.
Piers EV. The Piers-Harris children’s self concept scale. Los Angeles: Western Psychological Services; 2002.
Abdullah A, Blakeney P, Hunt R, Broemeling L, Phillips L, Herndon DN, et al. Visible scars and self-esteem in pediatric patients with burns. J Burn Care Rehabil. 1994;15(2):164–8.
Munster AM, Horowitz GL, Tudahl LA. The abbreviated Burn-Specific Health Scale. J Trauma. 1987;27(4):425–8.
Fillingim RB, Loeser JD, Baron R, Edwards RR. Assessment of chronic pain: domains, methods, and mechanisms. J Pain. 2016;17(9 Suppl):T10-20.
IASP. Taxonomy Seattle: IASP Press; 2012. 2nd. Available from: https://www.iasp-pain.org/Taxonomy?navItemNumber=576.
Sizoo SJM, van Baar ME, Jelsma N, van Zuijlen PPM, Nieuwenhuis MK. Outcome measures to evaluate the function of the hand after burns; a clinical initiative. Burns Open. 2021;5(3):162–7.
MacDermid JC, Tottenham V. Responsiveness of the disability of the arm, shoulder, and hand (DASH) and patient-rated wrist/hand evaluation (PRWHE) in evaluating change after hand therapy. J Hand Ther. 2004;17(1):18–23.
Valdes K, MacDermid J, Algar L, Connors B, Cyr LM, Dickmann S, et al. Hand therapist use of patient report outcome (PRO) in practice: a survey study. J Hand Ther. 2014;27(4):299–307.
Wormald JCR, Geoghegan L, Sierakowski K, Price A, Peters M, Jain A, et al. Site-specific Patient-reported Outcome Measures for Hand Conditions: Systematic Review of Development and Psychometric Properties. Plast Reconstr Surg Glob Open. 2019;7(5): e2256.
Burke TA, Ammerman BA, Hamilton JL, Stange JP, Piccirillo M. Nonsuicidal self-injury scar concealment from the self and others. J Psychiatr Res. 2020;130:313–20.
Adamson L, Selby A. The case for skin camouflage in the management of upper limb scarring – A case series. Hand Therapy. 2021;26(3):113–9.
Guyuron B, Vaughan C. Medical-grade tattooing to camouflage depigmented scars. Plast Reconstr Surg. 1995;95(3):575–9.
Kim E, Chang T, Hong J, Koh K. Use of tattooing to camouflage various scars. Aesthetic Plast Surg. 2011;35(3):392–5.
Carr T, Moss T, Harris D. The DAS24: a short form of the Derriford Appearance Scale DAS59 to measure individual responses to living with problems of appearance. Br J Health Psychol. 2005;10(Pt 2):285–98.
Acknowledgements
The authors would like to thank Lisa Gardner, NHS Support Librarian, Imperial College London for her guidance and support with developing our review search strategy.
Disclosures
This report is independent research and the views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health.
Funding
Donna L. Kennedy is supported by the NIHR Imperial Biomedical Research Centre (BRC) and receives Imperial Postdoctoral Bridging Support Funding from the Clinical Academic Training Office, Imperial College Academic Health Science Centre. Dominic Furniss is supported by the NIHR Oxford Biomedical Research Centre (BRC).
Author information
Authors and Affiliations
Contributions
DLK conceived the idea and study design and contributed to the acquisition, analysis and interpretation of data; TCB contributed to the study design and the acquisition, analysis and interpretation of data; DF contributed to the study design, analysis and interpretation of data. All authors (DLK; TCB; DF) participated in drafting and critically revising the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kennedy, D.L., Chism-Balangue, T. & Furniss, D. Reporting of scar outcomes in the hand and wrist; a state-of-the-art literature review. BMC Musculoskelet Disord 24, 249 (2023). https://doi.org/10.1186/s12891-023-06296-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06296-y