Abstract
Background
The indication for minimally invasive plate osteosynthesis (MIPO) may include articular fractures depending on the fracture pattern. The goal of this study was to evaluate the feasibility of the MIPO technique for extra- and intra-articular distal humeral fractures.
Methods
The feasibility of the MIPO technique was assessed on 8 cadaveric elbows and 2 clinical cases. The four surgical approaches tested included a 20-mm ulnar incision, a 20-mm dorsoradial incision, and two incisions for olecranon osteotomy (A and B). Surgical incision A was 40 mm on the osteotomy level of the olecranon, and surgical incision B was an extension of the radial incision toward the osteotomy of the olecranon (80 mm).
The four approaches were tested on 4 extra-articular (AO 13 A3) fractures and 4 intra-articular (AO 13 C3) fractures.
Results
Reduction and plate fixation of all distal humeral fractures (8 cadaveric) with and without osteotomy was feasible. However, when using approach B, the soft tissue tension is reduced due to the wider incision. Nevertheless, both approaches A and B showed the same adequate intra-articular fracture control and reduction.
Conclusion
The MIPO technique for reduction and plate fixation in distal humeral fractures is feasible.
Level of evidence
As a feasibility study, this study cannot be clearly classified into a level of evidence. It corresponds most closely to level IV.
Similar content being viewed by others
Introduction
Minimally invasive plate osteosynthesis (MIPO) was first described for distal femoral fractures in 1997 [1]. The control of bone alignment was confirmed by fluoroscopy and rotation clinically. Furthermore, MIPO is commonly applied for fracture stabilization in long bones, resulting in good clinical outcomes in femoral and tibial fractures [2, 3]. Indirect reduction and percutaneous fixation of the plate in MIPO protect the blood supply of the bone and the fracture hematoma and therefore seem beneficial for bone healing [4, 5]. In one of the earliest trials on MIPO for intraarticular distal tibial fractures, improved results for plate osteosynthesis were reported with only minimal wound-healing complications compared to the standard open reduction and internal fixation [6]. However, as extensive detachments of soft tissues and fracture exposure are omitted, an exact preoperative imaging technique and understanding of the fracture are crucial for the application of the MIPO technique. The possibilities of modern diagnostics enable precise fracture analysis and preoperative planning for osteosynthesis; thus, the indications for MIPO are becoming increasingly broad [7, 8].
Distal humeral fractures are typically treated using the dorsal approach. Several variations of this surgical approach have been described [9], and all utilize an extensive incision on the dorsal aspect of the elbow. Increased soft tissue dissection and longer duration of surgery are the result. Hence, it is tempting to hypothesize that MIPO in distal humeral fractures is beneficial to avoid these disadvantages of the dorsal approach. At present, there are no studies on the MIPO technique on the intraarticular distal humerus.
In this respect, we tested the feasibility of the MIPO technique for distal humeral fractures. We determined its applicability for extra-articular and intra-articular distal humeral fractures and for the latter using a minimally invasive olecranon osteotomy. We investigated a suitable incision to insert the plates and to align the shaft fracture and the intraarticular fracture anatomically. Furthermore, the plate position was evaluated postoperatively. We used a perpendicular plate position and compared the correct plate position with the AO manual. After reduction and fixation, X-ray control was performed to control the result. In addition, the ulnar and radial nerves and the collateral vessels were visualized by opening the surgical area to assess their integrity.
Materials and methods
Cadavers and patients
The feasibility of the MIPO technique was assessed on 10 elbows, including eight elbows from four Thiel-fixed and Thiel-conserved [10] cadavers (two males, two females; average time of death: 76 years) and two clinical cases with an extra-articular fracture (AO 13 A3).
Four extra-articular (AO type 13-A3) and four intra-articular distal humerus fractures (AO type 13-C3) were created in the cadaveric elbows. A short skin incision was made on the flexor side, and the fractures were produced with a chisel under fluoroscopic guidance. The 4 intraarticular (AO 13-C3) distal humeral fractures were reduced using an olecranon osteotomy via two different approaches, A and B, as described below. The 2 clinical cases involves AO 13 A3 fractures from a 57-year-old male (right side) and a 64-year-old female (left side).
Cadavers were placed in the supine position. The arm was bent over the chest to the contralateral shoulder and stabilized with a roll at 90° flexion of the elbow joint. The elbow was completely mobile during the entire procedure. Bony landmarks (olecranon, radial head, medial/lateral epicondyle and cubital tunnel containing the ulnar nerve) were marked with a waterproof pencil. The 2 clinical cases were operated on in the prone position with the elbow bent over a roll at 90°. An inflatable tourniquet was used for surgery, and the anatomic landmarks, the fracture, and incisions were marked with a waterproof pencil.
Minimally invasive approaches
Four surgical approaches were developed to allow plate positioning and to control fracture reduction: an ulnar approach, a radial approach, and two approaches for olecranon osteotomy (A and B).
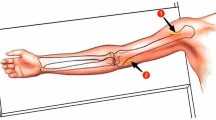
The ulnar approach involved an incision performed directly over the fracture extending to the medial epicondyle with a length of approximately 20 mm (Fig. 1a).
The radial approach (Fig. 1b) was dorsally performed over the fracture on the lateral column extending distally with the same length to provide 90-degree plate alignment of the ulnar and radial plate (Fig. 1c). The triceps muscle was mobilized to the medial side.
To reduce a C fracture correctly under visual control, an olecranon osteotomy is often necessary. For the minimally invasive olecranon osteotomy, we employed two different approaches, A and B. Approach A was located centrally over the olecranon at the level of the osteotomy (length 4 cm). Chevron-type osteotomy was performed, and the proximal fragment was reflected with a joystick K-wire at the tip of the olecranon to open the plane of the osteotomy (Fig. 2a+b).
Approach B was an extension of the radial approach, which was already directed toward the olecranon. Thus, the incision could be easily extended toward the olecranon up to the level of the osteotomy (length 8 cm). The osteotomy was performed as described above (Fig. 2c).
The reduction was controlled digitally and visually through the incisions and through the osteotomy for C3 fractures. For reduction of the extra-articular fractures, we placed two K-wires (2.0 mm) in the distal part of the humerus at the tip of the epicondyles. After fluoroscopic control of the reduction, the K-wires were advanced into the proximal part of the humerus to fix the fracture temporarily. In some cases, a reduction clamp was used over the incisions to facilitate reduction.
After temporary fixation of the fracture, the plates were inserted through the approaches on the bone. We used distal humerus locking compression plates (3.5 mm/2.7 mm LCP; DePuy Synthes, Oberdorf, Switzerland) for 90-degree double-plate osteosynthesis. Here, one plate was placed ulnarly, and one was placed posterolaterally. After temporary fixation of the plates to the bone with K-wires (1.6 mm) through drill sleeves, the position of the plates was confirmed radiologically. Then, the distal screws were inserted over the incision, and the proximal screws were inserted percutaneously through stab incisions into the plate for definitive fixation.
For intra-articular fractures, olecranon osteotomy permitted visual control of the articular surface. Reduction clamps and K-wires were inserted through the existing incisions. The osteotomy was fixed using an olecranon LCP (3.5 mm, DePuy Synthes) that was slid distally under the skin and locked percutaneously distally and through the incision proximally.
After radiological assessment of the 8 elbows with the C-arm in 2 planes, the approaches were extended, and the soft tissues were dissected to evaluate the plate positions and to detect possible injuries to the soft tissues, particularly the ulnar nerve (Fig. 3). The AO Manual was used as a reference for the plate position. Attention was given to the bone-plate distance and the correct orthograde alignment of the plate.
We evaluated the overall feasibility of the reduction and fixation of the 8 cadavers and 2 patients using the tested approaches, including the ulnar, radial, and osteotomy A and B approaches. In this respect, we assessed the reduction and plate positioning of all 8 elbows radiologically and after dissection of the 8 cadaveric elbows. Soft tissue damage of the cadaveric elbows was controlled in regard to unforeseen damage and ulnar nerve injury.
The reduction and control of the fractures and the application of percutaneous K-wires and small and large reduction clamps were tested. Osteotomy approaches A and B were compared.
In the two clinical cases with AO 13-A3 fractures, we exclusively used the ulnar and radial incisions. An olecranon osteotomy was not needed, so approaches A and B were not employed.
Results
The reduction and plate fixation of all distal humeral fractures (4 cadaveric AO 13-A3 fractures, 4 cadaveric AO 13-C3 fractures, 2 AO 13-A3 fractures in patients) with and without osteotomy was feasible.
Insertion of the plates on the humerus, temporary K-wire fixation through the ulnar and radial approaches of the plates and temporary fracture fixation percutaneously, and screw placement were possible in all 8 cadaveric distal humeral A3 and C3 fractures as well as the 2 A3 fractures in patients without obvious pitfalls (Fig. 4). The radiological control showed adequate fracture reduction, plate, and screw positioning in both planes for all ten distal humeral fractures.
The dissection of the cadaveric elbows showed adequate fracture reduction and plate positioning and did not reveal undue soft tissue injury. On the one hand, we examined the joint surface clinically. No steps or gaps were noted in any of the specimens. The fragments could be reduced anatomically with good bony contact. We also examined the fracture position with regard to the axial alignment of the humerus. Here, no clinically relevant deviations with regard to rotation or varus and valgus were found. The ulnar nerve was not injured macroscopically in all cadavers. The radial nerve also showed no injury macroscopically at the proximal incision. The 2 patients’ postoperative courses were uneventful. No neurologic deficits, vascular injuries or wound infections were noted. The range of motion was satisfactory in the last clinical controls. Both patients showed free pro- and supination at 6 months, and only one showed limited extension of 10 degrees in the elbow joint with free flexion.
Reduction and control of all fractures, including intra- and extra-articular fractures, could be performed without notable events using the ulnar and radial approaches as well as both osteotomy approaches A and B. It was possible to see the fracture landmarks sufficiently on the humeral metaphysis using both approaches (ulnar and radial) and those in the articular surface through the osteotomy (Fig. 5), thereby ensuring adequate control on the reduction of the fracture. The application of K-wires and the positioning of reduction clamps was possible using the existing approaches (ulnar, radial, osteotomy A and B).
Intraarticular fracture of the distal humerus (AO 13 C3) in a cadaveric specimen. a Approach B of the olecranon osteotomy with view on the articular surface of a fractured distal humerus. The approach is too extensive to be called MIPO. b Same as a after reduction. c,d Anteroposterior and lateral intraoperative X-ray after osteosynthesis with double plating of the humerus (3.5 mm ulnar and 3.5/2.7 mm radial LCP) and fixation of the osteotomy with olecranon LCP (3.5 mm LCP)
Both osteotomy approaches allowed safe osteotomy of the olecranon, sufficient manipulation of the fractures, and control of the articular surface of the distal humerus. Although approach A had an incision length of only 40 mm, approach B permitted easier reduction because of the lower tension of the soft tissues. If the overview of two small incisions as described in approach A is not sufficient, this can be improved via an extension to approach B. Nevertheless, the radial approach was already included in approach B. For approach A, the sum of the length of all incisions was 80 mm (20 mm ulnar, 20 mm radial, and 40 mm osteotomy) (Fig. 2b). For approach B, the sum of the lengths was 100 mm (20 mm ulnar and 80 mm radial + osteotomy) (Fig. 2c). The reduction and plate fixation of the osteotomy could be accomplished with both approaches, including screw insertion.
Although approach B provided better view and control of the articular surface, approach A was less extensive. The lengths of the two approaches were measured, revealing a difference in length of 20 mm (100 mm compared to 80 mm) (Fig. 2b/c). Nevertheless, we found no essential differences regarding control and reduction of the articular surface or the osteotomy between approaches A and B.
Discussion
The MIPO technique has gained increasing popularity for the treatment of humeral fractures [7, 11] and has already been established for use in proximal humeral fractures [12, 13]. An important prerequisite for the application of this technique is the possibility for sufficient fracture control, fracture reduction, and correct plate positioning. The results of this study show that these requirements can be fulfilled to allow the use of the MIPO technique for the treatment of extra- and intra-articular distal humeral fractures.
The standard surgical exposure for distal humeral fractures is the dorsal approach with an extensive incision and a full thickness flap. Different variations of the approach, especially for its dissection through or around the triceps muscle to the bone, exist: the paratricipital approach [14], the modification according to Newcastle [15], the triceps splitting approach and its modification [16]. To preserve muscle integrity, the triceps reflecting approach was established [17] and modified to the “triceps-reflecting-anconeus-pedicle” approach (TRAP) [18]. The most common approach for intraarticular fractures of the distal humerus is the dorsal approach with olecranon osteotomy [19]. Each approach described has its advantages and disadvantages, but there seem to be no differences in the functional outcomes [20, 21]. The many different approaches may indicate that an ideal approach for the treatment of distal humeral fractures has not yet been established. However, an extensive incision is necessary for any dorsal approach described thus far [9]. The duration of surgery and the length of the incision correlate directly with the wound infection rate [22]. In this study, the length of the incision was kept as short as we thought possible. In the two clinical cases, it was possible to minimize soft tissue damage by making smaller skin incisions.
The abovementioned reports describe the general feasibility of the MIPO technique and highlight its advantages and disadvantages. A clear advantage of small approaches used in the MIPO technique is the reduced damage to the blood supply of the bone and to the soft tissues compared to standard surgery. Our dissections of the cadaveric elbows after surgery showed no unexpected damage to the soft tissues or the ulnar nerve. Furthermore, the muscles remained macroscopically unharmed; this finding is in contrast to other studies in other anatomic regions, such as in the proximal humerus [23]. In their study, the authors described a partial lesion of the distal deltoid insertion caused by the insertion of the plate on the humeral shaft in the MIPO technique in a cadaveric study.
A possible disadvantage of the MIPO technique discussed in the literature was the fact that it is not possible to see and control the entire fracture and that its reduction can be cumbersome. Nevertheless, adequate fracture reduction can be achieved by controlling a few but crucial landmarks. For extraarticular fractures, the control of the entire fracture plane is not necessary to reduce the fracture or to place the plates. The strategically placed incisions, ulnarly and radially, right on the fracture site, made it possible to control the fracture sufficiently for reduction on both humeral edges. Furthermore, these incisions permitted the adequate positioning of plates onto the distal humerus to fix the fracture. However, plate positioning in the MIPO technique has been discussed as another disadvantage, as small incisions limit the working space and are expected to be more challenging. In our study, adequate plate positioning was confirmed radiologically in all 10 elbows and by dissection of the surrounding tissues in the 8 cadavers.
In addition to the abovementioned advantages of minimally invasive fracture treatment, disadvantages are also noted. In our subjective opinion, the overview achieved by the shorter incisions is sufficient for adequate reduction and insertion of the plates but limited compared to the open procedure. In the elbow area, a large number of vessels and nerves run within a small region. The location of these structures must be precisely known by the surgeon. In addition, due to the small number of cases and the fact that only one surgeon has performed these operations, our results of clinical cases represent a subjective assessment of the applicability of the MIPO technique. Nevertheless, the results of the experiments on the cadaver show that its implementation is feasible.
Clinical studies on the MIPO technique on the distal third of the shaft of the humerus have been reported in the literature [7, 24]. These results have demonstrated that the MIPO technique is feasible in this region of the humerus and achieves good results. However, studies on intra-articular fractures on the distal humerus have not been reported to date.
The use of the MIPO technique for articular fractures has been described only recently for distal tibial fractures [25, 26]. The approaches developed in these studies permit the sufficient control of fractures in the articular surface and plate insertion through a singular limited incision. Similar to our approaches to the distal humerus, proximal locking of the plates was performed percutaneously. Intraarticular fractures of the distal humerus, especially when comminuted, are treated best by olecranon osteotomy. In our experience, a compression screw outside the plate can also be used with this technique, as the preparation is sufficient. In our cases, reduction and stability could be achieved via k-wires and compression plates, so we did not use an additional screw. We expanded our indication for MIPO to intraarticular fractures using olecranon osteotomy with two different approaches. Although approach B was too extensive to be called minimally invasive in our opinion, approach A showed a surprisingly satisfying view and control of the articular surface of the distal humerus. The overview of the articular surface was similar to that of the conventional dorsal approach. Given the smaller incision and less soft tissue dissection, we prefer approach A for the treatment of intraarticular distal humeral fractures. However, when performing incision A, special attention must be paid to the ulnar nerve during further preparation and insertion of the plate. This nerve lies in the surgical area and represents a vulnerable structure. Both approaches A and B allowed the adequate surgical treatment of these fractures.
Limitations of the study include the fact that it was mainly a cadaver study, and only two patients were enrolled. The transferability of biomechanical studies to the in vitro model is not always accurate. Nevertheless, this study is a proof of concept and demonstrates general feasibility. A subsequent clinical study with a sufficient number of patients is necessary to recommend it for clinical application. We think that the development of further MIPO techniques for articular fractures is beneficial for the patient’s outcome and can generate equal osteosyntheses compared with open techniques.
Conclusion
In this cadaveric study, we were able to show that it is possible to reduce and fix extra- and intra-articular distal humeral fractures with locking plates using the MIPO technique in cadavers and two clinical cases.
Availability of data and materials
The data supporting the findings of this study are available upon request from the corresponding author (Valeska Hofmann, M.D., M.Sc.; Email: vhofmann@nolimitsurgery.com).
References
Krettek C, Schandelmaier P, Tscherne H. Neue Entwicklungen bei der Stabilisierung dia- und metaphysärer Frakturen der langen Röhrenknochen. Orthopade. 1997;26:408.
Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate Osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38:365–70.
Schütz M, Müller M, Krettek C, Höntzsch D, Regazzoni P, Ganz R, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study results of a clinical study with special emphasis on difficult cases. Injury. 2001;32:48–54.
Oh HK, Cho DY, Choo SK, Park JW, Park KC, Lee JI. Lessons learned from treating patients with unstable multifragmentary fractures of the proximal humerus by minimal invasive plate osteosynthesis. Arch Orthop Trauma Surg. 2015;135:235–42.
Devkota P, Khan JA, Shrestha SK, Acharya BM, Pradhan NS, Mainali LP, et al. Minimally invasive plate Osteosynthesis for distal Tibial fractures. J Orthop Surg (Hong Kong). 2014;22:299–303.
Collinge CA, Sanders RW. Percutaneous plating in the lower extremity. J Am Acad Orthop Surg. 2000;8:211–6.
Zhao W, Qu W, Fu C, Jiang H, Liu S, Cheng C. Antero-lateral minimally invasive plate osteosynthesis (MIPO) with the radial nerve exploration for extra-articular distal-third diaphyseal fractures of the humerus. Int Orthop. 2017;41:1757–62.
Samir Kassem M, Morsi E, Loutfy El-Adwar K, Motawea A, B. Minimally invasive plate Osteosynthesis versus intramedullary nailing for fixation of humeral shaft fractures in adults. J Orthop Sports Med. 2021;3:19–27.
Beeres FJP, Oehme F, Babst R. Distale Humerusfraktur – Zugänge und Erweiterungen. Oper Orthop Traumatol. 2017;29:115–24.
Thiel W. The preservation of the whole corpse with natural color. Ann Anat. 1992;174:185–95.
Apivatthakakul T. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Yearbook of hand and upper limb. Surgery. 2005;2004:9.
Acklin YP, Jenni R, Walliser M, Sommer C. Minimal invasive PHILOS®-plate Osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg Surg. 2009;35:35–9.
Gardner MJ, Griffith MH, Dines JS, Lorich DG. A minimally invasive approach for plate fixation of the proximal humerus. Bull Hosp Jt Dis. 2004;62:18–23.
Alonso-Llames M. Bilaterotricipital approach to the elbow: its application in the Osteosynthesis of supracondylar fractures of the Humerus in children. Acta Orthop Scand. 1972;43:479–90.
Amirfeyz R, Clark D, Quick T, Blewitt N. Newcastle approach to the elbow, a cadaveric study. Arch Orthop Trauma Surg. 2011;131:747–51.
Ziran BH, Smith WR, Balk ML, Manning CM, Agudelo JF. A true triceps-splitting approach for treatment of distal Humerus fractures: a preliminary report. J Trauma. 2005;58:70–5.
Bryan RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin Orthop Relat Res. 1982;(166):188–92.
O’Driscoll SW. The triceps-reflecting anconeus pedicle (trap) approach for distal humeral fractures and nonunions. Orthop Clin N Am. 2000;31:91–101.
Jupiter JB. AO manual of fracture management - Elbow & Forearm. Stuttgart: Thieme; 2009.
McKEE MD, Wilson TL, Winston L, Schemitsch EH, Richards RR. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach*. J Bone Joint Surg Am. 2000;82:1701–7.
Ljungquist KL, Beran MC, Awan H. Effects of surgical approach on functional outcomes of open reduction and internal fixation of intra-articular distal humeral fractures: a systematic review. J Shoulder Elb Surg. 2012;21:126–35.
Keshav K, Baghel A, Kumar V, Neradi D, Kaustubh K, Mishra P. Is minimally invasive plating Osteosynthesis better than conventional open plating for humeral shaft fractures? A systematic review and Meta-analysis of comparative studies. Indian J Orthop. 2021;55:283–303.
Benninger E, Meier C. Minimally invasive lateral plate placement for metadiaphyseal fractures of the humerus and its implications for the distal deltoid insertion- it is not only about the radial nerve. A cadaveric study. Injury. 2017;48:615–20.
Zogbi DR, Terrivel AM, Mouraria GG, Mongon MLD, Kikuta FK, Zoppi FA. Fracture of distal humerus: MIPO technique with visualization of the radial nerve. Acta Ortop Bras. 2014;22:300–3.
Wu D, Peng C, Ren G, Yuan B, Liu H. Novel anterior curved incision combined with MIPO for Pilon fracture treatment. BMC Musculoskelet Disord. 2020;21:176.
Kim GB, Shon O-J, Park CH. Treatment of AO/OTA type C Pilon fractures through the anterolateral approach combined with the medial MIPO technique. Foot Ankle Int. 2018;39:426–32.
Acknowledgments
Not applicable.
Informed consent
All individuals providing cadaver specimens must sign an informed consent for cadaver donation at the Institute of Anatomy and Cellular Biology, Paracelsus Medical University Salzburg, Austria. This consent includes the use for scientific research.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received to assist with the preparation of this manuscript. No funding was received to conduct this study. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
V.H., F.W., C.D., J.D. and M.B. conceived and planned the experiments. V.H., F.W., C.D. and J.D. performed the experiments. M.M. and M.B. contributed to sample preparation. V.H., F.W., M.M. and C.D. contributed to the interpretation of the results. V.H. took the lead in writing the manuscript. All authors provided critical feedback and helped shape the research, analysis and manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki and was reviewed and approved by the Ethics Commission Salzburg, Austria.
Consent for publication
All individuals providing cadaver specimens must sign an informed consent for cadaver donation at the Institute of Anatomy and Cellular Biology, Paracelsus Medical University Salzburg, Austria. This consent includes the use of the cadaver for scientific research and publication. The patients in the clinical cases were informed and provided their consent for publication.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hofmann, V., Diepold, J., Moursy, M. et al. Minimally invasive plate osteosynthesis (MIPO) for distal humeral fractures: a cadaveric study and first clinical application. BMC Musculoskelet Disord 24, 206 (2023). https://doi.org/10.1186/s12891-023-06189-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06189-0