Abstract
Background
Ulnar shortening osteotomy (USO) is a common surgical procedure for the treatment of ulnar impaction syndrome (UIS). The purpose of this study was to compare the results of metaphyseal and diaphyseal USO.
Methods
This retrospective study compared the clinical outcomes and complications of 32 patients who underwent diaphyseal step-cut USO (n = 10), diaphyseal oblique USO (n = 12), or metaphyseal USO (n = 10).
Results
Patient characteristics, ulnar variance, wrist range of motion, preoperative pain, grip strength, and functional scores (quick disability of the arm, shoulder, and hand and patient-rated wrist evaluation) were comparable. Both operation time (79.5 vs. 138/139 min) and incision length (7.80 vs. 9.67/13.00 cm) were shorter in the metaphyseal USO than in the diaphyseal oblique/step-cut USO. Compared with diaphyseal oblique/step-cut USO, metaphyseal osteotomies were associated with greater improvement in the pain on postoperative day 3 and shorter bone healing time. The requirements for implant removal were the same among the three groups. No complications were observed in any group.
Conclusion
Compared with diaphyseal USO, metaphyseal USO has advantages for operation time and incision length, early postoperative pain, bone healing in UIS management. The results suggested that metaphyseal USO could be widely applied to the surgical treatment of UIS. However, the long-term outcomes of these techniques still require further evaluation using more large-scale, randomized clinical trials.
Similar content being viewed by others
Introduction
Ulnar impaction syndrome (UIS) is a common degenerative wrist condition that develops as a result of force transmission across the ulnar wrist joint [1]. The root cause of UIS is progressive changes in the triquetrum, lunate, and triangular fibrocartilage complex (TFCC) caused by excessive loading on the ulnar side of the wrist joint [2]. Untreated UIS can lead to chondromalacia of the lunate, triquetral, and ulnar regions, TFCC degeneration, and ultimately osteoarthritis of the carpal ulnar or distal radioulnar joint. UIS is frequently related to positive ulnar variance, which can be acquired in various conditions such as radius malunion, radial head resection, or Essex–Lopresti injury [3].
The goal of surgery for UIS is to decrease the length of the ulna relative to the radius, thereby diminishing the amount of load that crosses the ulnocarpal joint, relieve pressure on the ulnar compartment of the carpus, and readjust TFCC tension [4]. If these issues are resolved, joint stability and normal wrist kinematics can be restored [5]. Ulnar shortening osteotomy (USO), which can reduce the ulnar load, is commonly used for the surgical treatment of patients with UIS [6]. Many types of USO and fixation techniques have been described [3, 6,7,8,9,10]. However, the effectiveness of USO has not been adequately assessed in studies with large sample sizes and reliable patient-reported outcome measures [11,12,13,14].
Thus, this retrospective study aimed to compare the three techniques of USO for UIS, including diaphyseal step-cut USO, diaphyseal USO, and metaphyseal USO.
Materials and methods
Patients
After receiving institutional review board approval from the Wuxi No. 9 People’s Hospital Affiliated with Soochow University, this retrospective study was performed to analyse data from all patients undergoing surgical intervention for UIS between 2017 and 2021.
The inclusion criteria were adult patients with UIS (aged ≥ 18 years) who underwent primary USO after 6 months of nonsurgical treatment failure. The diagnosis of UIS was confirmed by medical history and physical examination, including the use of provocative manoeuvres (e.g., ulnocarpal stress test) [15], and plain radiographs showing positive ulnar variance [16] with or without cystic change in the lunate or triquetrum [1]. Nonsurgical measures included local steroid injections, anti-inflammatory medications, and wrist immobilisation. Patients with osteoporosis (a skeletal disorder characterized by compromised bone strength predisposing a person to an increased risk of fracture, the standard criterion for the diagnosis of osteoporosis in postmenopausal women and 50 years older men is a T-score of ≤ -2.5 at the lumbar spine, femur neck, or total hip by bone mineral density testing; the standard criterion for the diagnosis of osteoporosis in premenopausal women and men under 50 years old is a Z-score of ≤ -2.0), fractures of the forearm or wrist, degenerative joint diseases, or surgeries were performed for congenital abnormalities (refers specifically to malformations of the wrist and forearm, such as Madelung malformation.) were excluded. According to the osteotomy location, patients were further stratified and underwent either diaphyseal (including step-cut and oblique osteotomy) or metaphyseal USO. These cases involving different osteotomy methods are not selected at random. Each method was confirmed by the particular patient fully aware of the merit and demerit in surgical technique after talking with the surgeon. All operations were performed by one senior hand surgeon (GZ).
Techniques
Diaphyseal USO
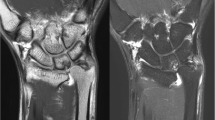
Oblique USO (Fig. 1)
The technique was verified using surgical reports. Surgery was performed under brachial plexus anaesthesia using a pneumatic tourniquet. A longitudinal ulnar forearm 8–11 cm incision was made mid-axially. The osteotomy was performed at the level of the diaphysis (usually 60 mm proximal to the ulnar styloid to preserve the soft tissues). Care was taken not to damage the dorsal sensory branch of the ulnar nerve. The ulnar diaphyseal region was exposed and passed through the space between the flexor and extensor carpi ulnaris muscles. To obtain zero or slightly negative ulnar variance, ulnar shortening was scheduled based on preoperative radiography. A procedure-specific ulnar osteotomy compression plate (TriMed; UOCP, USA) was used.
Step-cut USO (Fig. 2)
A slight volar skin incision (8–16 cm) was made along the distal 1/3 of the ulna, and the distal part of the ulna was exposed using the space between the extensor and flexor carpi ulnaris. Osteotomy was designed using a 7-hole 3.5-mm standard neutralisation plate (Synthes, GmbH, PA, USA). The osteotomy long arm was marked between the third and fifth holes, at the midportion of the plate, allowing placement of bicortical screws in these two holes. Then, the osteotomy site was reduced, and a lag screw was placed in the osteotomy centre from the dorsal to the volar and perpendicular to the osteotomy long arm to compress the steotomy arms. Finally, the osteotomy site was fixed on the volar surface of the ulna with a standard neutralisation plate, with three 6-lag screws at the proximal end and three at the distal end.
Metaphyseal USO (Fig. 3)
A longitudinal incision (6–9 cm) was made at the ulnar wrist from the tip of the ulnar styloid, and the incision was gradually made proximally. A plane was created between the flexor and extensor carpi ulnaris to expose the ulna from the subperiosteum. The dorsal cutaneous branch of the ulnar nerve was protected carefully. The locking compression distal ulnar plate (Synthes, GmbH) was placed on the surface of the exposed ulna with hooks attached to the ulnar styloid, and when reaching the desired position, we made distal drill holes in the metaphysis using a 1.5-mm drill bit to avoid the “floating” of distal bone fragment after osteotomy. Then, the plate was removed. Two transverse parallel osteotomies were performed to reach the radius–ulnar level. Before operating the osteotomy, a longitudinal line was drawn on the ulna to make the reduction more accurate and convenient. The ulna in the first osteotomy had not been wholly cut to make room for the thin plastic sheet, which was used as a reference for the second osteotomy to be cut more parallel. After locking the plate back into place, osteotomy closure was completed. Finally, proximal fixation was accomplished using one locking screw.
Data collection
Data on patient sex, age, smoking status, ulnar variance (before and after surgery), incision length, operative time, and follow-up time were collected. The visual analogue scale (VAS) for pain [17], Quick Disability of the Arm, Shoulder, and Hand (QuickDASH) score [18], Patient-Rated Wrist Evaluation (PRWE) [19], grip strength, and wrist range of motion (ROM) were analysed before and after surgery. Perioperative complications were also recorded.
Statistical analyses
Descriptive statistics were expressed as mean and median values. The Shapiro–Wilk W test was used to test whether the data were distributed normally. The differences between the various groups defined by the three techniques were compared using the nonparametric Kruskal–Wallis test (one-way analysis of variance), with the F-ratio used for determining significance. This test compares the means of multiple groups to determine whether at least one group has a different mean than the others. As an advantage, this test can be used even if the data violate the normality of the distribution. This test was used because determining the normality of data distribution was difficult in small samples. IBM SPSS Statistics, version 21 (IBM Corp., Armonk, USA) was used for statistical analysis.
Results
Thirty-two patients (11 men, 21 women) were enrolled in this study. Among them, 10 (31%), 10 (31%), and 12 (38%) patients underwent metaphyseal, step-cut, and oblique USOs, respectively. The three groups were comparable in terms of patient age, sex, smoking status, and follow-up (Table 1). Similarly, ulnar variance, wrist ROM, preoperative pain, grip strength, and functional scores (QuickDASH and PRWE) were also comparable among the groups (Table 2). Both the operation time and incision length of the metaphyseal USO were shorter than those of the diaphyseal oblique/step-cut USO (Table 1, Figs. 4 and 5). Moreover, metaphyseal USO was associated with less pain on postoperative day 3 (Table 2, Fig. 6) and shorter bone healing time (Table 2). No complications were observed. All operations were performed by one senior hand surgeon (GZ). Due to the Chinese tradition concept, all implants were removed.
Discussion
Extra-articular USO is commonly used to manage positive ulnar variance in patients with symptomatic UIS. Several USO techniques have been developed, such as those using cutting guides, special jigs, shortening systems, and different fixation forms [3, 10, 20,21,22,23,24,25]. However, a technique with great clinical superiority is uncertain. Sennwald et al. [8] reported that most patients undergoing either metaphyseal or diaphyseal USO had satisfactory outcomes, with both techniques showing equivalent clinical results. Marquez-Lara et al. [26] confirmed that pain relief and QuickDASH scores after metaphyseal USO were greater than those after diaphyseal USO. Imai et al. [27] suggested that the bone healing potential after metaphyseal USO was better than that after diaphyseal USO. Similar to the results of Marquez-Lara et al., our study confirmed greater pain relief after diaphyseal USO. Moreover, we found that metaphyseal USO generally had a shorter operative time than diaphyseal USO. The shorter operation time in the metaphyseal USO group indicated that this type of osteotomy is easier to perform, which could be related to several points, as follows: (1) the distal oblique bundle (DOB) would not hinder the reduction, (2) the proximal and distal fixation steps inherent in diaphyseal USO could be avoided, and (3) the use of a practical distal ulnar hook plate. The greater pain relief in the early stage after metaphyseal USO than after diaphyseal USO was likely determined by less soft tissue damage and shorter operative time. Owing to the abundant blood supply and less resistant to osteotomy, a metaphyseal USO is considered to provide better bone healing potential than a diaphyseal USO [28], which is consistent with our findings. Despite these theoretical advantages, bony union was achieved in all patients in this study, regardless of the surgical technique, in line with previous findings [8, 26, 27]. Theoretically, without the interference of the DOB (In a large sample of 185 forearms, reported prevalence of DOB was 29% [29]. In smaller samples of 10 to 30 forearms, reported prevalence was 40% [30,31,32,33]), metaphyseal USO may allow more shortening. In our study, none of the patients required extensive shortening osteotomy. We attempted to shorten the ulna by only a few millimetres to unload the ulnocarpal joint without having to reduce ulnar variance to the neutral position. DRUJ laxity was decreased by the increased tensioning of the distal interosseous membrane accompanying ulnar shortening. An osteotomy proximal to the ulnar attachment of the distal interosseous membrane should improve DRUJ stability, especially in the presence of a DOB [34], at the expense of increased DRUJ joint reaction force [35]. Metaphyseal USO is considered to improve DRUJ congruity and reduce the risk for arthritis [3]. There is a paucity of data on the long-term clinical effects of metaphyseal USO on DRUJ stability, but functional outcomes have appeared promising [3, 8, 36]. However, no positive ROM-related results were found among the groups, consistent with the findings of Imai et al. [27].
In terms of surgical techniques, metaphyseal USO is less difficult to perform and less expensive. With the application of a procedure-specific ulnar osteotomy compression plate, oblique USO could be more precise, but the disadvantage is its high price. Step-cut USO provides adequate bone-to-bone contact and reduces rotation control. However, the lack of guidance makes precise osteotomy challenging. Metaphyseal USO is a distal transverse osteotomy in which parallel osteotomy can be performed manually. Moreover, metaphyseal USO is less destructive to soft tissue and has a smaller stripping area. Despite the thinness of the locking compression distal ulnar plate, its strength was sufficient, there was no problem with non-weight bearing daily activities before the bone heals, and no case of plate fracture occurred. Moreover, the price of the hook plate is more acceptable to the patients. The disadvantage is that, in a few cases, there is discomfort at the place where the styloid process is hooked on the plate, which only occurs after pressing. No subsequent interventions have been necessary.
The main limitation of this comparative study was the lack of randomisation, which is inherent to any retrospective study. Female patients were dominant in the metaphyseal group, which may have introduced a potential bias for our data analysis. Based on the results of this study, the diaphyseal USO was replaced by a metaphyseal USO, and the metaphyseal USO was applied for routine ulnar shortening. The average follow-up was 15.1 months, which was sufficient to evaluate bone union. However, some complications may have occurred after this period, which were not documented in the study. Another limitation was that the cohort size was small. Further large-scale, randomised clinical trials are warranted to assess the long-term outcomes of these techniques.
In conclusion, compared with diaphyseal USO, metaphyseal USO has advantages for operation time and incision length, early postoperative pain, bone healing in UIS management. The results suggested that metaphyseal USO could be widely applied to the surgical treatment of UIS. However, the long-term outcomes of these techniques still require further evaluation using more large-scale, randomized clinical trials.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Tomaino MM, Elfar J. Ulnar impaction syndrome. Hand Clin. 2005;21(4):567–75.
Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1991;7(2):295–310.
Nunez FA Jr, Barnwell J, Li Z, Nunez FA. Sr.: Metaphyseal ulnar shortening osteotomy for the treatment of ulnocarpal abutment syndrome using distal ulna hook plate: case series. J Hand Surg. 2012;37(8):1574–9.
Sammer DM, Rizzo M. Ulnar impaction. Hand Clin. 2010;26(4):549–57.
Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. Surgical technique. J bone joint Surg Am volume. 2006;88(Suppl 1 Pt 2):212–20.
Stockton DJ, Pelletier ME, Pike JM. Operative treatment of ulnar impaction syndrome: a systematic review. J hand Surg Eur volume. 2015;40(5):470–6.
Im JH, Lee JY, Kang HV. The Combined Procedure of Ulnar Metaphyseal Shortening Osteotomy With Triangular Fibrocartilage Complex Foveal Knotless Repair. The Journal of hand surgery. 2021;46(9):822.e821-822.e827.
Sennwald G, Della Santa D, Beaulieu JY. A comparison of diaphyseal and metaphyseal techniques of ulna shortening. J hand Surg Eur volume. 2013;38(5):542–9.
Luria S, Lauder AJ, Trumble TE. Comparison of ulnar-shortening osteotomy with a new trimed dynamic compression system versus the Synthes dynamic compression system: clinical study. J Hand Surg. 2008;33(9):1493–7.
Papatheodorou LK, Baratz ME, Bougioukli S, Ruby T, Weiser RW, Sotereanos DG. Long-term outcome of step-cut Ulnar Shortening Osteotomy for Ulnar Impaction Syndrome. J bone joint Surg Am volume. 2016;98(21):1814–20.
Hassan S, Shafafy R, Mohan A, Magnussen P. Solitary ulnar shortening osteotomy for malunion of distal radius fractures: experience of a centre in the UK and review of the literature. Ann R Coll Surg Engl. 2019;101(3):203–7.
Isaacs J, Howard SB, Gulkin D. A prospective study on the initial results of a low profile ulna shortening osteotomy system. Hand (New York NY). 2010;5(2):148–54.
Schmidle G, Kastenberger T, Arora R. Time-Dependent Recovery of Outcome Parameters in Ulnar Shortening for positive Ulnar Variance: a prospective Case Series. Hand (New York NY). 2018;13(2):215–22.
Aibinder WR, Izadpanah A, Elhassan BT. Ulnar Shortening Versus Distal Radius Corrective Osteotomy in the Management of Ulnar Impaction After Distal Radius Malunion. Hand (New York, NY). 2018;13(2):194–201.
Friedman SL, Palmer AK, Short WH, Levinsohn EM, Halperin LS. The change in ulnar variance with grip. J Hand Surg. 1993;18(4):713–6.
Jung JM, Baek GH, Kim JH, Lee YH, Chung MS. Changes in ulnar variance in relation to forearm rotation and grip. J bone joint Surg Br volume. 2001;83(7):1029–33.
Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–26.
Wormdal AH, Tallaksen SH, Hagen Ø, Foss OA, Finsen V. Remembered preoperative quick disabilities of the arm, shoulder and hand (QuickDASH) scores. J hand Surg Eur volume. 2017;42(1):78–83.
MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–86.
Chennagiri R, Burge P. Pre-osteotomy plate application technique for ulnar shortening. J Hand Surg (Edinb Scotl). 2004;29(5):453–7.
Wehbé MA, Cautilli DA. Ulnar shortening using the AO small distractor. J Hand Surg. 1995;20(6):959–64.
Minami A, Kato H. Ulnar shortening for triangular fibrocartilage complex tears associated with ulnar positive variance. J Hand Surg. 1998;23(5):904–8.
Mizuseki T, Tsuge K, Ikuta Y. Precise ulna-shortening osteotomy with a new device. J Hand Surg. 2001;26(5):931–9.
Horn PC. The long ulnar sliding osteotomy. J Hand Surg. 2004;29(5):871–6.
Chen NC, Wolfe SW. Ulna shortening osteotomy using a compression device. J Hand Surg. 2003;28(1):88–93.
Marquez-Lara A, Nuñez FA Jr, Kiymaz T, Nuñez FA, Li SZ. Metaphyseal Versus Diaphyseal Ulnar Shortening Osteotomy for Treatment of Ulnar Impaction Syndrome: A Comparative Study. The Journal of hand surgery. 2017;42(6):477.e471-477.e478.
Imai H, Takahara M, Kondo M. Ulnar Shortening Osteotomy for Ulnar Abutment Syndrome: the results of Metaphyseal and Diaphyseal Osteotomies. J hand Surg Asian-Pacific volume. 2020;25(4):474–80.
Luo TD, De Gregorio M, Zuskov A, Khalil M, Li Z, Nunez FA, Sr., Nunez FA. Jr.: Distal metaphyseal osteotomy allows for Greater Ulnar Shortening compared to Diaphyseal Osteotomy for Ulnar Impaction Syndrome: a Biomechanical Study. J Wrist Surg. 2020;9(2):100–4.
Hohenberger GM, Schwarz AM, Weiglein AH, Krassnig R, Kuchling S, Plecko M. Prevalence of the distal oblique bundle of the interosseous membrane of the forearm: an anatomical study. J hand Surg Eur volume. 2018;43(4):426–30.
Noda K, Goto A, Murase T, Sugamoto K, Yoshikawa H, Moritomo H. Interosseous membrane of the forearm: an anatomical study of ligament attachment locations. J Hand Surg. 2009;34(3):415–22.
Kitamura T, Moritomo H, Arimitsu S, Berglund LJ, Zhao KD, An KN, Rizzo M. The biomechanical effect of the distal interosseous membrane on distal radioulnar joint stability: a preliminary anatomic study. J Hand Surg. 2011;36(10):1626–30.
Moritomo H. The distal interosseous membrane: current concepts in wrist anatomy and biomechanics. J Hand Surg. 2012;37(7):1501–7.
Dy CJ, Jang E, Taylor SA, Meyers KN, Wolfe SW. The impact of coronal alignment on distal radioulnar joint stability following distal radius fracture. J Hand Surg. 2014;39(7):1264–72.
Arimitsu S, Moritomo H, Kitamura T, Berglund LJ, Zhao KD, An KN, Rizzo M. The stabilizing effect of the distal interosseous membrane on the distal radioulnar joint in an ulnar shortening procedure: a biomechanical study. J bone joint Surg Am. volume 2011;93(21):2022–30.
Canham CD, Schreck MJ, Maqsoodi N, Messing S, Olles M, Elfar JC. Distal Radioulnar Joint reaction force following Ulnar Shortening: Diaphyseal Osteotomy Versus Wafer Resection. J Hand Surg. 2015;40(11):2206–12.
Nunez FA Jr, Li Z, Campbell D, Nunez FA, Sr. Distal ulna hook plate: angular stable implant for fixation of distal ulna. J Wrist Surg. 2013;2(1):87–92.
Acknowledgements
None.
Funding
Wuxi Sci&Tech Program (Grant No. 2021217), Top Talent Support Program for young and middle-aged people of Wuxi Heath Committee (No. BJ2020116), and Jiangsu Province Postdoctoral Research Funding Program (No. 2021217).
Author information
Authors and Affiliations
Contributions
All authors (HYY, WYQ, FZ, QZ, YZL, ZFL, GZ and JYM) contributed to the study conception and design. Material preparation, data collection, and analysis were performed by HYY, WYQ, FZ, QZ, YZL, ZFL and JYM. The first draft of the manuscript was written by HYY and critically revised by GZ. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Wuxi 9th People’s Hospital Affiliated to Soochow University. Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, H., Qi, W., Zhang, F. et al. Comparison of diaphyseal and metaphyseal ulnar shortening osteotomies for the treatment of ulnar impaction syndrome. BMC Musculoskelet Disord 24, 10 (2023). https://doi.org/10.1186/s12891-022-06070-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-06070-6









