Abstract
Background
Shoulder complaints are common and the recommended first-line treatment is exercise therapy. However, it remains unknown if increased shoulder pain after an exercise session is a barrier for subsequent exercise dose, particularly in people with high fear-avoidance beliefs. Such knowledge could indicate ways to optimise shoulder rehabilitation. The aim was to examine whether increased shoulder pain across an exercise session was associated with a lower subsequent exercise dose, and if high fear-avoidance beliefs exaggerated this association.
Methods
We conducted a prospective cohort study using data from a randomised controlled trial in Central Denmark Region 2017–2019. Participants were employees (n = 79) with shoulder complaints and high occupational shoulder exposures. The intervention was a home-based or partly supervised exercise programme lasting 2–3 months. Linear mixed models were used to examine the associations between change in shoulder pain and exercise dose (number of repetitions, progression level (1–3), resistance level (1–3), and time until next exercise session [days]).
Results
At baseline, the participants had a median pain intensity at rest of 2 on a numerical rating scale (0–10). For a 1-cm increase in pain on a visual analogue scale (0–10 cm) during an exercise session, the subsequent number of repetitions, progression level and resistance level were − 1.3 (95% confidence interval [CI] − 3.4 to 0.9), 0.0 (95% CI − 0.1 to 0.0) and − 0.0 (95% CI − 0.1 to 0.0), respectively. Likewise, the time until next exercise session was − 0.6 (95% CI − 2.4 to 1.3) days for a 1-cm increase. There were no interactions with fear-avoidance beliefs.
Conclusion
Increased pain across an exercise session was not associated with subsequent exercise dose, regardless of fear-avoidance beliefs, among employees with shoulder complaints and high occupational shoulder exposures.
Trial registration
The trial was registered at Clinicaltrials.gov 19/05/2017 (ID: NCT03159910).
Similar content being viewed by others
Background
Shoulder complaints are common in the adult population, with a 1-month prevalence of 19–31%, where the variation primarily depended on case definitions [1]. Exercise therapy is recommended as first-line treatment [2,3,4,5], and supervised and home-based exercise seem equally effective [5,6,7,8]. During exercise therapy, aggravation of shoulder pain should be kept to a minimum [3] and the exercise dose in the subsequent session should be reduced if pain aggravation does not subside shortly after exercising [3, 9, 10]. Two views exist regarding the accepted degree of shoulder pain aggravation during exercise therapy [3, 8]. One group argues that pain aggravation may indicate overload of stressed tissues because of too difficult exercises or too high exercise load and decrease exercise motivation [3]; another group argues that pain aggravation may guide exercise progression and increase exercise motivation [3]. Persons who exercise to reduce shoulder complaints report lower motivation if the exercise feels harmful, but higher motivation if the exercise feels beneficial [11, 12].
According to the fear-avoidance model, negative appraisals of pain may cause people to avoid physical activities, including exercise therapy, in order to reduce pain, but through a vicious circle, this may instead lead to increased pain and disability [13,14,15]. Two studies of patients with shoulder complaints treated by exercises [16, 17] showed an advantage of low fear-avoidance beliefs with respect to pain and function, whereas a third study [18] showed no prognostic role of fear-avoidance beliefs with respect to disability. The influence of fear-avoidance beliefs on exercise dose has not been investigated, but higher levels of fear-avoidance beliefs were associated with a higher probability of quitting an exercise intervention in people with non-specific chronic neck and shoulder pain [16].
We are not aware of studies that have examined whether increased shoulder pain after an exercise session is a barrier for subsequent exercise dose or adherence to exercise programmes, particularly in people with high fear-avoidance beliefs. Such knowledge could indicate ways to optimise shoulder rehabilitation.
The primary aim of this study was to examine whether increased shoulder pain across an exercise session was associated with a lower exercise dose in the subsequent session, and if this association (if any) was exaggerated by high levels of fear-avoidance beliefs. The secondary aim was to examine whether increased shoulder pain across exercise sessions together with high levels of fear-avoidance beliefs influenced adherence to the exercise programme.
Methods
Design and setting
We conducted a prospective cohort study. The study was a secondary analysis of data from a cluster-randomised controlled trial, which compared two interventions (Shoulder-Café and Shoulder-Guidance) to reduce shoulder complaints among employees with high occupational shoulder exposures (ID: NCT03159910 at Clinicaltrials.gov on 19/05/2017) [19]. Both groups were analysed as a cohort to answer the present research questions. The Danish Data Protection Agency (case number: 1–16-02–498-16) and the Committee on Health Research Ethics in Central Denmark Region approved the study (case number: 1–10-72–271-16). All participants provided written informed consent. We reported the study using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement. According to the randomisation, which was performed at company level, participants were enrolled in an intervention between August 2017 and August 2019. In-person meetings took place at six municipal health centres in Central Denmark Region. All participants completed a baseline questionnaire before the randomisation result was revealed to them. An intervention period of 12 weeks was intended, but due to work schedules of the physiotherapists and holidays, the periods varied.
Study population
Detailed in- and exclusion criteria for the randomised trial have been described previously [19]. In brief, the participants were 18–65 years of age, employed in occupations with high mechanical shoulder exposures (i.e., service, manufacturing and construction), experienced shoulder pain, were without previous shoulder surgery and had an Oxford Shoulder Score (OSS) ≤ 40. The OSS is a 12-item patient-reported tool to measure shoulder pain and function ranging from 0 (worst) to 48 (best) [20,21,22]. To be included in this study, data was required on change in pain and subsequent exercise dose.
Interventions
All participants were advised to follow a home-based shoulder exercise programme described in a pamphlet [19]. The programme was based on effect of published exercise programmes [9, 23,24,25,26], and included elements known to motivate exercise adherence (few exercises [3, 27], progression with individual adjustments [3] and elastic bands making exercise possible everywhere [12, 28]. The 15-min programme was recommended to be followed three to four times per week throughout the intervention. In addition to one posture correction exercise, the programme comprised three resistance exercises performed bilaterally with an elastic band: two exercises for the scapula stabilising muscles and one for the rotator cuff muscles. Each resistance exercise had three progression levels and three resistance levels (elastic band) (low = 1, medium = 2 and high = 3) (Additional file). Participants were recommended to start with the lowest progression and resistance levels, and to perform as many repetitions as possible until they were able to perform more than 3 sets of 15 repetitions. At this point, they were advised to progress the exercises. Progression included using an elastic band with higher resistance and to go on to the next progression level when the highest resistance level was reached. Participants were informed that pain aggravation (without further specification) during exercise could be expected, but if the aggravation did not cease within 1 h after the exercise session, they were recommended to decrease one progression or resistance level, or to decrease the number of repetitions in the next exercise session [19].
Additionally, the participants in the Shoulder-Café group were offered three supervised exercise sessions in accordance with the exercise pamphlet, and a clinical shoulder examination performed by a physiotherapist [19]. Based on the clinical shoulder examination, subacromial impingement syndrome was considered to be present if anterolateral shoulder pain was accompanied by a positive result of at least three of the following five clinical tests: Hawkins’ test, Neer’s clinical test, painful arc test, Jobe’s test and pain on resisted external rotation [29, 30].
Outcomes
Exercise dose was quantified in terms of: number of repetitions (total number of repetitions per exercise session), progression level (mean progression level per exercise session [mean across exercise sets per session]), resistance level (mean elastic band resistance per exercise session [mean across exercise sets per session]) and time until next exercise session (days between two exercise sessions). Adherence to the exercise programme was classified as high or low (≥ 2 vs < 2 weekly exercise sessions). Information on exercise dose and adherence was obtained via an exercise diary (Additional file). To describe exercise progression (as another aspect of adherence), we aggregated the number of exercises per participant during the first (1 to 7 weeks) and last (8 to 15 weeks) part of the intervention.
Predictors
Change in shoulder pain was calculated as shoulder pain at rest shortly after an exercise session minus shoulder pain at rest shortly before the exercise session using a visual analogue scale (range 0 cm [no pain] to 10 cm [worst imaginable pain]) [31]. A positive change indicated an increase in pain. For descriptive purposes, we defined decreased shoulder pain as a change of < − 1 cm, unchanged shoulder pain as a change of − 1 to 1 cm, and increased shoulder pain as a change of > 1 cm. The choice of these definitions was based on the observed distribution of changes in shoulder pain across exercise sessions. Information about pain was obtained from the exercise diary (Additional file).
Fear-avoidance beliefs were assessed using a shoulder version of the Fear-Avoidance Beliefs Questionnaire—Physical Activity (FABQ-PA) [32,33,34], which ranges from 0 [no fear-avoidance] to 24 [high fear-avoidance]. The baseline FABQ-PA was used as a dichotomised score (low ≤ 14, high > 14) [35, 36]. Information about FABQ-PA was obtained from the baseline questionnaire.
Covariates
Potential confounders comprised age, sex, body mass index (BMI), smoking status, dominant-sided pain, baseline pain at rest (measured with a numerical rating scale [NRS] ranging from 0 [no pain] to 10 [worst imaginable pain]), intervention group, days since start of intervention and session number. Age, sex, BMI and smoking status were included based on the literature [37, 38]. Apart from intervention group, days since start of intervention and session number, information on the covariates was collected through the baseline questionnaire.
Statistical analyses
Continuous variables were presented as means with standard deviations (SD) or medians with interquartile ranges (IQR) depending on their distributions, and categorical variables as numbers and percentages. In descriptive analyses, missing values for number of repetitions, progression level and resistance level were replaced by values from the most recent exercise session with non-missing values, except for the first session, where missing values were replaced by values from the subsequent session. Remaining missing values were not replaced.
The associations between change in shoulder pain (continuous) and subsequent exercise dose (continuous) were analysed using linear mixed models allowing for clustering of data according to company and repeated measurements. Participants with a minimum of one exercise session including data for change in shoulder pain and one subsequent exercise session were kept in the models. The analyses were performed using crude and adjusted models including age (continuous), sex, BMI (continuous), smoking status (never, ex, current), dominant-sided pain (yes, no), baseline pain at rest (continuous), intervention group, days since start of intervention (continuous), session number (continuous) and an interaction term between change in shoulder pain (continuous) and baseline FABQ-PA (high, low). Associations were presented as mean differences with 95% confidence intervals (CI) based on bootstrapping (with 100 replications) to allow for non-normality of the outcome.
The influence of increased shoulder pain (continuous) and baseline FABQ-PA (high, low) on adherence (high, low) was analysed using logistic regression with robust standard errors allowing for intragroup correlation at company level. The analyses were performed using crude and adjusted models including the same covariates as listed above. Adherence was presented as odds ratio (OR) with 95% CI. We applied likelihood ratio test of no interaction between change in shoulder pain and high FABQ-PA. All analyses were performed using Stata 16 (StataCorp LP, College Station, TX, USA).
Results
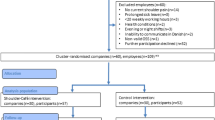
Out of the 109 participants in the randomised trial, 79 could be included (Fig. 1). Table 1 presents baseline characteristics of the participants included in the present study and those excluded due to missing data on change in pain and subsequent training dose. For the participants with a high FABQ-PA, the mean (SD) was 18.5 (2.5) for those included and 18.5 (3.0) for those with missing data. For participants with a low FABQ-PA the mean was 9.2 (4.0) for those included and 9.0 (3.8) for those with missing data. Pain duration ranged from around 1 to around 360 months. In the Shoulder-Café group, subacromial impingement syndrome was diagnosed in 38% (17/45) of the included participants and in 42% (5/12) of the participants with missing data.
The intervention period was between 7 and 15 weeks in which the home-based exercises should be followed. In the Shoulder-Café group, 96% (43/45) additionally participated in two and 67% (30/45) in three supervised exercise sessions. The total number of intervention weeks among all participants was 850, during which a total of 1401 exercise sessions was performed. This corresponds to a mean of 17.7 (range: 2 to 50) exercise sessions per participant and a mean of 1.6 (range: 0 to 7) weekly exercise sessions. Figure 2 shows the distribution of weekly exercise sessions according to intervention week. The percentage of participants performing weekly exercises decreased gradually during the intervention period while the percentage performing zero weekly exercise sessions increased likewise.
Table 2 presents characteristics of the 1401 exercise sessions according to the first (1 to 7 weeks) and last (8 to 15 weeks) part of the intervention. There were no indications of exercise progression between the two parts.
Change in shoulder pain was missing for 141 sessions, leaving 1260 exercise sessions for further analyses. The mean shoulder pain shortly before and shortly after an exercise session was 1.6 (SD 1.5) and 1.9 (SD 1.8), respectively. Figure 3 illustrates the distribution of the 1260 exercise sessions, showing that unchanged pain was most common (80%). Reduced pain was found after 2% of the exercise sessions and increased pain after 18% of the sessions.
Distribution of pain change across exercise sessions (n = 1260) performed by 79 participants according to intervention week. The 79 participants were sorted according to the number of sessions they had performed. They performed 1260 exercise sessions in total. Green dots (n = 28) represent reduced pain after an exercise session (a change of < − 1 cm), yellow dots (n = 1003) represent unchanged pain (a change of − 1 to 1 cm) and red dots (n = 229) represent increased pain (a change of > 1 cm)
Out of the 1260 exercise sessions, 59 sessions were not followed by further sessions, leaving 1201 sessions for the analyses of associations between change in shoulder pain and subsequent exercise dose. As seen in Table 3 (adjusted results), increased shoulder pain across an exercise session did not influence subsequent exercise dose, and no interaction between change in shoulder pain and high FABQ-PA was found.
Thirty-one participants had high adherence. Table 4 shows that change in shoulder pain and high FABQ-PA did not influence adherence to the exercise programme (adjusted odds ratio [95% CI]: 0.6 [0.2 to 1.4] and 1.2 [0.4 to 4.3]). The likelihood ratio test had a p-value of 0.12 for no interaction between change in shoulder pain and high FABQ-PA.
Discussion
This study demonstrated no associations between increased shoulder pain across an exercise session and lower subsequent exercise dose, regardless of the level of fear-avoidance beliefs. In addition, increased shoulder pain across exercise sessions together with high fear-avoidance beliefs did not influence adherence to the exercise programme.
Strengths of the study include the prospective design, the high participation (72%), the high data completeness and the repeated data collection. The main limitation was that the participants were informed that pain aggravation during exercise could be expected, and if the pain did not decrease within 1 h after exercise, they were advised to reduce the exercise dose in the subsequent exercise session. We did not specify the maximum tolerable pain aggravation, and it is reassuring that the exercise programme generally did not markedly aggravate shoulder pain (cf. the introduction). On the other hand, this information could have led to the low increase in pain across exercise sessions that we observed, i.e., low exposure contrast, and could have especially affected participants with a high FABQ-PA because they may be more likely to avoid exercise due to pain [13, 14]. Regarding FABQ-PA we did not observe such a pattern. High fear-avoidance beliefs might cause participants to drop out of an exercise intervention due to pain, but the mean FABQ-PA for participants included and those with missing data were comparable both in case of high and in case of low FABQ-PA. Therefore, we do not think that fear-avoidance beliefs increased the risk of attrition bias in our study. None of the main results were statistically significant, which might suggest that the study was underpowered. However, the mean differences were minimal for increase in shoulder pain, FABQ-PA and their interactions, so these factors did not seem to play any considerable role for subsequent exercise dose. Exercise dose and adherence were assessed by self-report, but we find it unlikely that under- or over-reporting of exercise efforts would be systematically related to increase in pain across an exercise session. Therefore, we do not think that the self-reported information biased our results.
Our study showed no indications of exercise progression despite all participants having a detailed description of the progression method in the exercise pamphlet. We are not aware of studies that have described progression in home-based settings, but in a study of 12 weeks’ supervised shoulder exercises, it was found that the resistance level increased by 74% [23].
Baseline FABQ-PA was comparable to previous studies of participants with shoulder complaints [32, 34]. In a study of participants with more than 6 months of neck or shoulder pain, persons with high fear-avoidance beliefs were more likely to drop out of the home-based exercise intervention [16]. In contrast, we found no association between FABQ-PA and adherence to the exercise programme. Participants in the just-mentioned study [16] had comparable baseline fear-avoidance beliefs (21 (0 to 16 scale)) and pain intensities (4 on the NRS) to our participants, but their median pain duration was 102 months (IQR 60 to 168 months), i.e. considerably longer than reported by the participants in the present study. Therefore, we think that the inclusion of patients with chronic pain in the previous study might explain why fear-avoidance beliefs played a part in that study but not in ours.
Our exercise programme was designed to support adherence. Adherence in our study was comparable with a previous study of home-based shoulder exercise [39], but higher adherence has also been reported; i.e., 88% completion of two daily sessions [40] and 96% completion of at least one daily session [41], compared with 39% completion of at least two weekly sessions in our study. A reason for our rather low adherence may be that in our participants, baseline pain was too low to motivate frequent exercise performance [12]. Our participants had not sought treatment for their complaints, whereas previous participants were in contact with the health care system [40, 41]. Another explanation could be lack of time because about 40% of the participants in one of the previous studies were on sick leave [40] compared with none of our participants. The other previous study did not inform about sick leave, but baseline pain was high (7 to 8 on the NRS) [41], indicating a probability of sick leave. Lack of time can decrease exercise motivation [12], and in line with this sick leave may enhance the motivation.
In the present study, participants with missing data seemed comparable to those included in the analyses, although they tended to be younger, more often men and more often smokers. Those with missing data seemed to have longer pain durations, but the difference only represented 10% of the total range. Due to the missing data, we were not able to tell whether these participants forgot to report their completed exercise sessions or whether they did not exercise, but we tend to assume the latter. This suggests that participants with the just-mentioned characteristics may need extra attention and guidance in relation to exercise therapy.
Employees could be included in the present study [19], if they had at least slight shoulder complaints (OSS ≤ 40), and baseline pain intensities at rest and during activity as well as changes across exercise sessions were generally low. We cannot rule out that higher increases in pain across an exercise session, depending on the severity of the shoulder disorder or the exercise programme, may lead to a subsequently reduced exercise dose. Thus, our results do not reveal whether an association exits between increases in higher pain intensities across an exercise session and subsequent exercise dose. Future studies of patients, e.g., in hospital departments of orthopaedic surgery, may examine whether this is the case.
Conclusion
Increased shoulder pain across an exercise session was not a barrier for subsequent exercise dose nor exercise adherence, regardless of fear-avoidance beliefs among persons with slight shoulder complaints.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly accessible, but are available from the corresponding author on reasonable request and under standard conditions.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FABQ-PA:
-
Fear-Avoidance Beliefs Questionnaire—Physical Activity
- IQR:
-
Interquartile range
- MD:
-
Mean difference
- NRS:
-
Numerical rating scale
- OR:
-
Odds ratio
- OSS:
-
Oxford Shoulder Score
- SD:
-
Standard deviation
- VAS:
-
Visual analogue scale
References
Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population: a systematic review. Scand J Rheumatol. 2004;33:73–81.
Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T, et al. Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 2014;85:314–22.
Klintberg IH, Cools AM, Holmgren TM, Holzhausen AC, Johansson K, Maenhout AG, et al. Consensus for physiotherapy for shoulder pain. Int Orthop. 2015;39:715–20.
Kulkarni R, Gibson J, Brownson P, Thomas M, Rangan A, Carr AJ, et al. Subacromial shoulder pain. Shoulder Elbow. 2015;7:135–43.
Sundhedsstyrelsen [Danish Health Authority]. [In Danish] Behandling af patienter med subakromielt smertesyndrom i skulderen [Treatment of patients with subacromial pain syndrome in the shoulder]. Copenhagen: Sundhedsstyrelsen; 2021.
Gutierrez-Espinoza H, Araya-Quintanilla F, Cereceda-Muriel C, Alvarez-Bueno C, Martinez-Vizcaino V, Cavero-Redondo I. Effect of supervised physiotherapy versus home exercise program in patients with subacromial impingement syndrome: a systematic review and meta-analysis. Phys Ther Sport. 2020;41:34–42.
Liaghat B, Ussing A, Petersen BH, Andersen HK, Barfod KW, Jensen MB, et al. Supervised training compared with no training or self-training in patients with subacromial pain syndrome: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2021;102:2428–3244.
Littlewood C, Malliaras P, Chance-Larsen K. Therapeutic exercise for rotator cuff tendinopathy: a systematic review of contextual factors and prescription parameters. Int J Rehabil Res. 2015;38:95–106.
Holmgren T, Hallgren HB, Öberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ. 2012;344:e787.
Littlewood C, Malliaras P, Mawson S, May S, Walters S. Development of a self-managed loaded exercise programme for rotator cuff tendinopathy. Physiotherapy. 2013;99:358–62.
Littlewood C, Malliaras P, Mawson S, May S, Walters S. Patients with rotator cuff tendinopathy can successfully self-manage, but with certain caveats: a qualitative study. Physiotherapy. 2014;100:80–5.
Sandford FM, Sanders TAB, Lewis JS. Exploring experiences, barriers, and enablers to home- and class-based exercise in rotator cuff tendinopathy: a qualitative study. J Hand Ther. 2017;30:193–9.
Turk DC, Wilson HD. Fear of pain as a prognostic factor in chronic pain: conceptual models, assessment, and treatment implications. Curr Pain Headache Rep. 2010;14:88–95.
Vlaeyen JWS, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153:1144–7.
Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–68.
Karlsson L, Gerdle B, Takala EP, Andersson G, Larsson B. Associations between psychological factors and the effect of home-based physical exercise in women with chronic neck and shoulder pain. SAGE Open Med. 2016;4:2050312116668933.
Sindhu BS, Lehman LA, Tarima S, Bishop MD, Hart DL, Klein MR, et al. Influence of fear-avoidance beliefs on functional status outcomes for people with musculoskeletal conditions of the shoulder. Phys Ther. 2012;92:992–1005.
Kromer TO, Sieben JM, de Bie RA, Bastiaenen CH. Influence of fear-avoidance beliefs on disability in patients with subacromial shoulder pain in primary care: a secondary analysis. Phys Ther. 2014;94:1775–84.
Trøstrup J, Mikkelsen LR, Frost P, Dalbøge A, Høybye MT, Casper SD, et al. Reducing shoulder complaints in employees with high occupational shoulder exposures: study protocol for a cluster-randomised controlled study (The Shoulder-Cafe Study). Trials. 2019;20:627.
Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78:593–600.
Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford Shoulder Score revisited. Arch Orthop Trauma Surg. 2009;129:119–23.
Frich LH, Noergaard PM, Brorson S. Validation of the Danish version of Oxford Shoulder Score. Dan Med Bull. 2011;58:A4335.
Christiansen DH, Frost P, Falla D, Haahr JP, Frich LH, Andrea LC, et al. Effectiveness of standardized physical therapy exercises for patients with difficulty returning to usual activities after decompression surgery for subacromial impingement syndrome: randomized controlled trial. Phys Ther. 2016;96:787–96.
Ingwersen KG, Jensen SL, Sørensen L, Jørgensen HR, Christensen R, Søgaard K, et al. Three months of progressive high-load versus traditional low-load strength training among patients with rotator cuff tendinopathy: primary results from the double-blind randomized cntrolled RoCTEx tial. Orthop J Sports Med. 2017;5:1.
Littlewood C, Bateman M, Brown K, Bury J, Mawson S, May S, et al. A self-managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: a randomised controlled trial (the SELF study). Clin Rehabil. 2016;30:686–96.
Peterson MD, Rhea MR, Alvar BA. Applications of the dose-response for muscular strength development: a review of meta-analytic efficacy and reliability for designing training prescription. J Strength Cond Res. 2005;19:950–8.
Babatunde FO, MacDermid JC, MacIntyre N. A therapist-focused knowledge translation intervention for improving patient adherence in musculoskeletal physiotherapy practice. Arch Physiother. 2017;6:1.
Andersen LL, Zebis MK. Process evaluation of workplace interventions with physical exercise to reduce musculoskeletal disorders. Int J Rheumatol. 2014;2014:761363.
Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46:964–78.
Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90:1898–903.
Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804.
Mintken PE, Cleland JA, Whitman JM, George SZ. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with shoulder pain. Arch Phys Med Rehabil. 2010;91:1128–36.
Riley SP, Tafuto V, Cote M, Brismée JM, Wright A, Cook C. Reliability and relationship of the Fear-Avoidance Beliefs Questionnaire with the Shoulder Pain And Disability Index and numeric pain rating scale in patients with shoulder pain. Physiother Theory Pract. 2019;35:464–70.
Trolle N, Christiansen DH. Measurement properties of the Fear-Avoidance Belief Questionnaire for physical activity in patients with shoulder impingement syndrome. Patient Relat Outcome Meas. 2019;10:83–7.
George SZ, Stryker SE. Fear-avoidance beliefs and clinical outcomes for patients seeking outpatient physical therapy for musculoskeletal pain conditions. J Orthop Sports Phys Ther. 2011;41:249–59.
Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine (Phila Pa 1976). 2004;29:1167–72.
da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. 2010;53:285–323.
Linaker CH, Walker-Bone K. Shoulder disorders and occupation. Best Pract Res Clin Rheumatol. 2015;29:405–23.
Roddy E, Ogollah RO, Oppong R, Zwierska I, Datta P, Hall A, et al. Optimising outcomes of exercise and corticosteroid injection in patients with subacromial pain (impingement) syndrome: a factorial randomised trial. Br J Sports Med. 2021;55:262–71.
Granviken F, Vasseljen O. Home exercises and supervised exercises are similarly effective for people with subacromial impingement: a randomised trial. J Physiother. 2015;61:135–41.
Santello G, Rossi DM, Martins J, Libardoni TC, de Oliveira AS. Effects on shoulder pain and disability of teaching patients with shoulder pain a home-based exercise program: a randomized controlled trial. Clin Rehabil. 2020;34:1245–55.
Acknowledgements
We would like to thank the physiotherapists and the participants for their contributions. We also thank the funding institution.
Funding
This work was supported by Public Health in Central Denmark Region (grant number: A911); Danish Regions; Task Force for Health Innovation in Central Denmark Region; Aarhus University; the Association of Danish Physiotherapists; the Danish Rheumatism Association (grant number: A5659); Sawmill owner Jeppe Juhl and Wife Ovita Juhl’s Foundation (personal grant to SWS); Helga and Peter Korning’s Fund. The funding sources had no role in the design, conduct or reporting of the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the planning and design of the study. JT managed the project, collected the data and drafted the manuscript. JT and PF performed the data analysis and interpreted the results supported by SWS, AD and LRM. MTH, LBJ and TMK supported throughout the process. All authors critically revised the manuscript and read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Danish Data Protection Agency on 7 September 2016 (case number: 1–16-02–498-16) and by the Committee on Health Research Ethics in Central Denmark Region on 20 March 2017 (case number: 1–10-72–271-16). Written informed consent was obtained from all participants. The study was performed in accordance with the ethical principles described in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Trøstrup, J., Svendsen, S.W., Dalbøge, A. et al. Increased shoulder pain across an exercise session and subsequent shoulder exercise: a prospective cohort study. BMC Musculoskelet Disord 23, 726 (2022). https://doi.org/10.1186/s12891-022-05674-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05674-2