Abstract
Background
Osteitis fibrosa cystica is a rare, benign and osteolytic lesion attributed to hyperparathyroidism. The high level of parathyroid hormone cause rapid bone loss.
Case presentation
The patient is a 50-year-old male complaining of severe and persistent pain in the right knee joint. Imaging studies were suspicious for a benign tumor in the right distal femur. Biopsy under CT guidance showed numerous osteoclast aggregation and hemosiderin deposition around the bone trabeculae. Blood tests disclosed significantly elevated parathyroid hormone, serum calcium, serum alkaline phosphatase. Parathyroid ultrasonography and CT scan showed a solid mass in front of the trachea at the thoracic entrance plane. After resection of the mass, the clinical symptoms were relieved and the radiological results were significantly improved, which further confirmed the diagnosis.
Conclusions
Metabolic diseases-associated bone lesions require a comprehensive diagnosis of multiple inspection items. An interprofessional team approach to the diagnosis and treatment of osteitis fibrosa cystica will provide the best outcome.
Similar content being viewed by others
Background
Osteitis fibrosa cystica (OFC) is a a rare, osteolytic and nonneoplastic metabolic bone disease [1]. The activation of osteoclast in OFC is due to increased endogenous parathyroid hormone (PTH) [2]. Hyperparathyroidism is a common endocrine disorder characterized by elevated blood concentration of parathyroid hormone (PTH) and hypercalcemia, usually due to a benign adenoma. Primary or secondary hyperparathyroidism is usually asymptomatic, however, severe forms may be diagnosed by lesions of target organs such as the skeletal system and the kidneys. Among patients with hyperparathyroidism, about 20% develop kidney stone disease [3]. Osteitis fibrosa cystica can occur as solitary or multiple lesions in any bone, most often in the mandible, pelvis, ribs and long bones [4, 5]. The most typical skeletal manifestation of hyperparathyroidism were loss of cortical bone and trabecular remodeling due to osteoclast activation. OFC can be associated clinically with bone fractures, skeletal deformities and bone pain [6]. At present, osteitis fibrosa cystica, though rare, was easily misdiagnosed. Due to its histological and radiological features, it is often misdiagnosed as a bone tumor [7]. We report a case of primary parathyroid adenoma with OFC that presented clinically and radiologically as an aggressive metabolic bone disease.
Case presentation
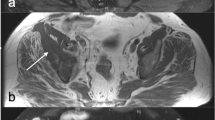
A 50-year-old male presented to our institution for pain in the right knee joint. The pain gets worse during exercise and relieved at rest. Physical examination was unremarkable. CT scan showed cyst-like bone lesion at the distal part of femur with destruction of bone cortices, soap bubble like inner structure, sclerotic rim and no periosteal reaction (Fig. 1). Other CT scans showed kidney stones in this patient (Fig. 2). Contrast-enhanced magnetic resonance imaging of the knee joint showed a heterogeneous enhancement and clear boundary (Fig. 1). There was no soft tissue mass around the lesion. Biochemical blood tests revealed high calcium concentration (3.63 mmol/L, normal values 2.11–2.52 mmol/L) and low phosphorus concentration (0.5 mmol/L, normal values 0.85–1.51 mmol/L). The result tended to be a lytic bone tumor. A bone biopsy was performed under CT scan guidance, the sample was sent for histopathologic examination. Histopathologic examination showed bone lesion composed of remodeled bone trabeculae with scattered groups of multinucleate giant cells of the osteoclast type with areas of hemorrhage and hemosiderosis. There was no evidence of malignancy in the biopsy sample (Fig. 3).
In order to verify hypercalcemia caused by hyperparathyroidism, parathyroid ultrasound and parathormone (PTH) were also performed. The concentration of PTH in serum is elevated (2034.6 pg/mL, normal values 12.0–88.0 pg/mL). Parathyroid ultrasound revealed a 3.6 × 1.6 cm solid mass in front of the trachea at the thoracic entrance plane. Contrast-enhanced CT scan of the parathyroid neoplasm showed heterogeneous enhancement and clear boundary (Fig. 2). Combined with the above results, we considered that bone lesion was related to parathyroid neoplasm.
After resection of the parathyroid adenoma, the patient no longer complained from knee joint pain and imaging performed six months later showed significant improvement, with reduction of the bone lesion dimensions and complete reconstruction of bone cortices (Fig. 4).
Discussion and conclusion
Osteitis fibrosa cystica (OFC) is a disorder involving the bone which is resulted from excessive production of parathyroid hormone (PTH) due to hyperparathyroidism. Hyperparathyroidism might be due to parathyroid adenoma (up to 85% of cases), parathyroid hyperplasia, parathyroid carcinoma and hereditary factors [8].
Biologically, PTH induces osteoclast activity which results in abnormal structural changes and bone remodeling including osteopenia, subchondral resorption, subperiosteal bone resorption and focal lytic lesion [9]. Up to 5% of hyperparathyroidism cases develop OFC. In clinical, OFC is usually diagnosed late because they are asymptomatic unless the disease reaches advanced stages and causes clinical symptoms such as pain or deformity [10]. OFC is a metabolic and non-neoplastic lesion but sometimes may also be misdiagnosed as a malignant lesion. It can also be misdiagnosed for a metastatic disease based on the radiological results, such as multiple scattered osteolytic lesions [11].
As for the imageological diagnosis, CT showed cyst-like bone destruction, monocystic or polycystic, clear boundary and no periosteal reaction.The MRI examined no soft tissue mass formation around OFC which is a relatively characteristic phenomenon. OFC also often coexist with subperiosteal bone cortical resorption, subchondral bone resorption. Based on imaging manifestations, OFC needs to be identified from giant cell tumor of bone, aneurysm-like bone cysts, plasmacytomas. Pathological manifestations of the lesions surface is brown, formed by different size of the cysts. The cystic wall is fibrous tissue. When necrosis or hemorrhage occurred in the cystic cavity, large numbers of multinucleated macrophages and hemosiderin-rich phagocytes appeared. Osteoclasts showed a sheet-like distribution. Inhomogeneous cancellous bone trabeculae was surrounded by osteoblasts.
The diagnosis of OFC may be challenging. In clinical practice, patient’s symptoms are due to bone softening and hypercalcemia, which might include bone mass or fractures, kidney stones, peptic ulcer, weight loss, nausea and loss of appetite. However, these symptoms lack the specificity. In addition to the histological and radiological findings, biochemical tests including PTH, serum calcium, alkaline phosphatase are also very important to ensure a correct OFC diagnosis.Treatment of osteitis fibrosa cystica starts with the management of hyperparathyroidism, such as parathyroid adenoma resection. After parathyroid adenoma resection, the majority of bone disorders caused by OFC will be resolved.
In summary, in current practice, skeletal manifestations of hyperparathyroidism are less common than in the past. OFC as a kind of metabolic diseases-associated bone lesion is easily misdiagnosed as bone tumor according to radiological and pathological characteristics. Serum calcium and PTH should be conventionally checked in patients with suspected metabolic bone disease. Elevated parathyroid hormone levels and hypercalcemia are indicative of OFC and complement the radiological and histological results to further confirm the diagnosis. If treated properly, OFC is reversible.
Availability of data and materials
The authors declare that data supporting the findings of this study are available within the article.
References
Shaaban ATE, Ibrahem M, Saleh A. Brown tumor due to primary hyperparathyroidism resulting in acute paraparesis: case report and literature review. Surg Neurol Int. 2020;21(11):355–9.
Jervis L, James M, Howe W, Richards S. Osteolytic lesions: osteitis fibrosa cystica in the setting ofsevere primary hyperparathyroidism. BMJ Case Rep. 2017;5(28):22–6.
Bilezikian JP, Khan A, Cusano NE. Hyperparathyroidism. Lancet. 2018;391(10116):168–78.
Lajolo C, Patini R, Limongelli L. Brown tumors of the oral cavity: presentation of 4 new cases and a systematic literature review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;129(6):575–84.
Fatma LB, Barbouch S, Fethi BH. Brown tumors in patients with chronic renal failure and secondary hyperparathyroidism: report of 12 cases. Saudi J Kidney Dis Transpl. 2010;21(4):772–7.
Colucci PG, Schweitzer AD, Saab J, et al. Imaging findings of spinal brown tumors: a rare but important cause of pathologic fracture and spinal cord compression. Clin Imaging. 2016;40(5):865–9.
Lee JH, Chung SM, Kim HS. Osteitis fibrosa cystica mistaken for malignant disease. Clin Exp Otorhinolaryngol. 2013;6(2):110–3.
De La Flor Merino JC, Domínguez JJ. Multiple brown tumors-forgotten pathology in times of calcimimetics: a case report and literature review. SAGE Open Med Case Rep. 2021;9(11):553–61.
Bandeira F, Cusano NE, Silva BC, Cassibba S, Almeida CB, Machado VC, Bilezikian JP. Bone disease in primary hyperparathyroidism. Arq Bras Endocrinol Metabol. 2014;58(5):553–61.
Nasser ML, Medawar S, Younan T. Osteitis fibrosa cystica mimicking bone tumor, a case report. 2021;22(1):479.
Khalatbari MR. Brown tumor of the spine in patients with primary hyperparathyroidism. 2014;39(18):1073-9.
Acknowledgements
The authors gratefully acknowledge the patient who agreed to participate in this study, as well as Mr Biao Hu for his assistance during the manuscript preparation.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
XLX: data acquisition, literature search, manuscript preparation. SJL and HP: data acquisition, literature search. SGC: medical management. CPY: pathological interpretation, manuscript preparation and editing. QML revised and reviewed the manuscript for the final publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Medical Ethics Committee of Jingzhou Center Hospital has approved the research. The patient agreed to participate in this study. Informed consent was obtained from the patient prior to the study. All procedures were conducted according to the Declaration of Helsinki.
Consent for publication
Written informed consent has been obtained from the patient for publication of this case report and any accompanying images.
Competing interests
All authors certify that they have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, XL., Yang, CP., Lu, SJ. et al. A patient with femoral osteitis fibrosa cystica mimicking bone neoplasm: a case report. BMC Musculoskelet Disord 23, 322 (2022). https://doi.org/10.1186/s12891-022-05274-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05274-0